Effectiveness of Elastodontic Devices for Correcting Sagittal Malocclusions in Mixed Dentition Patients: A Scoping Review
Abstract
1. Introduction
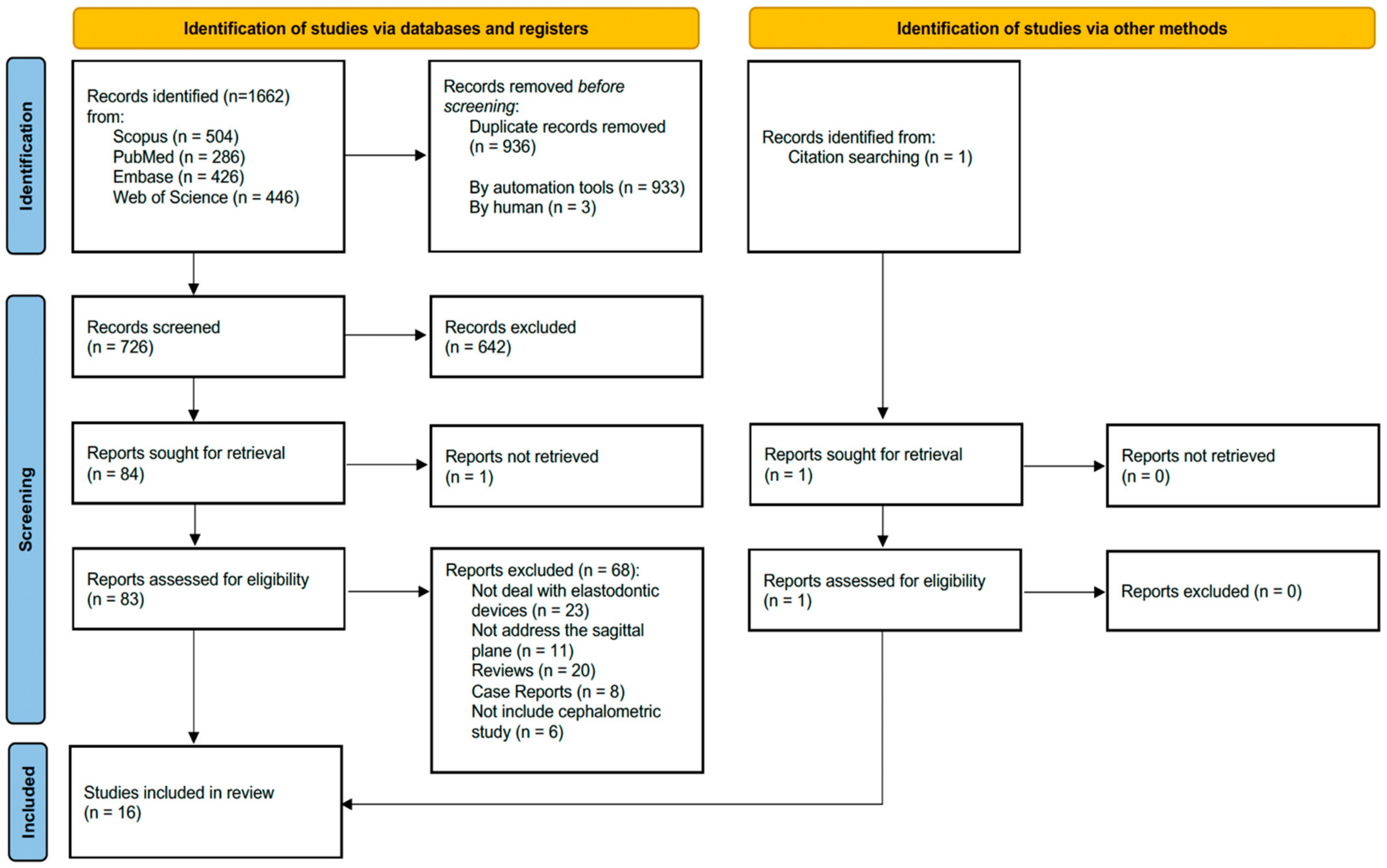
2. Materials and Methods
- Patients in mixed dentition
- Randomized controlled trials
- Retrospective and prospective studies
- Patients with permanent or full deciduous dentition
- Studies without radiographic records
- Review studies
3. Results
3.1. Study Characteristics
| Author (Year) [Reference] | Setting/Country | Study Design | Conclusions |
|---|---|---|---|
| Chen LR et al. (2022) [23] | Taichung Veterans General Hospital/Taiwan | Retrospective Case–Control Study | EF group: UI angle decrease, LI angle increase, and LI tip to Mb plane distance decrease in comparison to the control group UI angle changes were statistically significant One-year follow-up was not sufficient to determine the skeletal effect of the EF appliance |
| Ciavarella D et al. (2021) [16] | Orthodontic Department, University of Foggia/Italy | Retrospective Case–Control Study | EA treatment produces the following: No significant dental or aesthetic changes Minor skeletal effects Mb length and LFH increased after EA treatment compared with untreated patients |
| Ciftci V et al. (2021) [26] | Department of Orthodontics, Faculty of Dentistry, Cukurova University/Turkey | Prospective Study | Multi-P functional appliance: Reduction in OVJ, OVB, and convexity in the mixed dentition stage Follow-up data are needed to evaluate the long-term benefits of this appliance |
| Çoban Büyükbayraktar Z et al. (2023) [27] | Orthodontic Department of Sivas Cumhuriyet University Dentistry Faculty/Turkey | Retrospective Case–Control Study | TB and myobrace can be used for Mb advancement Twin-block appliance was more effective The long-term effects of myobrace on Mb advancement are unknown |
| Fichera G et al. (2021) [12] | Department of Orthodontics, University of Catania/Italy | Retrospective Case–Control Study | EA showed: Improvement of OVJ, OVB, crowding, and the sagittal molar relationship EA is a simple, natural, and less invasive therapeutic option for treating malocclusion |
| Galluccio G et al. (2021) [17] | Italy | Retrospective Case–Control Study | Occlus-o-Guide®, FR-2, TB increase in Mb length FR-2 and TB are more effective in increasing the Mb length The reduction in the ANB angle was similar in the three groups, but the increase in the SNB angle was significant only for FR-2 and TB Occlus-o-Guide®, FR-2, and TB produce the following: Reduction in OVJ and OVB in relation to the control group The reduction produced by TB was significant compared to that for the other two devices The IMPA angle increased more in the O-o-G® group The esthetic analysis shows the following: TB group: More reduction in facial convexity More reduction in the thickness of LL O-o-G® group: More retrusion of UL followed by that in the TB group FR-2 group: Increase in the thickness of the UL compared to the control group |
| Inchingolo AD et al. (2022) [18] | Italy | Retrospective Study | The AMCOP® Integral with a flat mastication plane is sufficient to correct mild hyperdivergency The AMCOP® Open is more indicated in severe hyperdivergent. This device also contributes to the functional re-education of the tongue The AMCOP® SC allows the correction of class II dysmorphism favoring a mandibular advancement The long-term stability of the results obtained is still to be evaluated |
| Johnson JS et al. (2021) [29] | KVG Dental College and Hospital, Sullia, Karnataka/India | Randomized Control Prospective Study | TB and myobrace appliances: Not effective in restricting the forward growth of the maxilla TB produced the following: Significant skeletal and dentoalveolar changes Better improvement of mandibular growth (Go–Ar, Go–Me, Ar–Gn) than the myobrace system Myobrace induced the following: Reduction in OVJ, forward rotation of the mandible, and forward positioning of the mandible TB appliances demonstrated the following: Correction of full Class II molar relationship Better correction of molar relation than myobrace TB and myobrace showed the following: Improvement in the profile TB showed the following: Increase in the anterior and posterior facial heights Myobrace group showed the following: Better bite closure effect Myobrace and TB groups exhibited the following: Flaring of the lower incisors, such as unfavorable treatment outcome More prominent in the myobrace group than the twin-block group |
| Lanteri V et al. (2022B) [19] | Department of Biomedical, Surgical and Dental Sciences, University of Milan/Italy | Randomized Control Retrospective Study | Customized and preformed EGAs showed the following: Improvement of Class II malocclusion and anterior crowding Reduction in OVJ and OVB Significant changes regarding the sagittal and vertical cephalometric relationship Customized EGA was as follows: More effective in correcting anterior crowding, dento-skeletal vertical relationship, and the position of the permanent incisor compared to the preformed appliance |
| Lo Giudice A et al. (2022) [20] | Department of Orthodontics, Pediatric Unit, University of Catania/Italy | Prospective Control Study | EAs showed the following: Improvement in OVJ, OVB, crowding, and the sagittal molar relationship compared to controls EAs determined the following: Correction of early signs of malocclusion in Class II subjects Harmonious development of the palate |
| Madian AM et al. (2023) [30] | Orthodontic Department, Faculty of Dentistry, Alexandria University/Egypt | Randomized Control Prospective Study | TB was as follows: More effective than myobrace in improving the upper and middle airways No difference was detected regarding the lower airway TB and myobrace produced the following: Reduction in the severity of developing skeletal Class II due to mandibular retrognathism by forward posturing of the mandible |
| Patano A et al. (2023) [21] | Department of Orthodontics at the Policlinico of Bari/Italy | Retrospective Case–Control Study | AMCOP® SC permitted the following: Correction of skeletal Class II malocclusion Improvement of Mb advancement Functional elastodontic device therapy determined the following: Significant airway changes in skeletal Class II subjects compared with an untreated control group Improvement of deglutition, phonation, and respiratory function The hyoid bone shifted inferiorly at the end of treatment in the treated group with respect to the control group |
| Ronsivalle V et al. (2023) [22] | Section of Orthodontics, School of Dentistry, University of Catania/Italy | Retrospective Case–Control Study | EAs permitted the following: Correction of Class III malocclusions in children Improvement of morphology of the palate in the transverse and anteroposterior directions Correction of anterior crossbite by promoting harmonious restoration of maxillary growth |
| Usumez S et al. (2004) [28] | Department of Orthodontics, School of Dentistry, Selcuk University, Konya/Turkey | Retrospective Case–Control Study | Preorthodontic trainer appliance caused the following: Better reduction in LI proinclination and OVJ than in the control group Increase in total facial height |
| Yang X et al. (2022) [24] | Pediatric Dentistry Department of Shanghai Ninth People’s Hospital/China | Retrospective Case–Control Study | Orofacial myofunctional therapy resulted in the following: Improvement of the patient’s lip strength A good option for mixed dentition patients with lip incompetence Preformed appliances determined the following: Improvement in lip strength and forward movement of the mandible LI protrusion had a negative effect |
| Zhang X et al. (2021) [25] | Department of Stomatology, The Second Affiliated Hospital of Jiaxing University, Jiaxing, Zhejiang Province/China | Retrospective Case–Control Study | Prefabricated myofunctional appliance and RME are as follows: The best option for the treatment of mouth breathers with Class II malocclusion in the mixed dentition period T4K showed the following: Optimal sagittal correction of maxilla and mandible Greater dental compensation with inhibition of skeletal remodeling Further studies with larger sample sizes are needed |
Cephalometric Outcomes
Elastodontic Appliances vs. Other Functional Appliances
Elastodontic Appliances vs. Untreated Patients (Control)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Spinas, E.; Savasta, A. Prevention of traumatic dental lesions: Cognitive research on the role of mouthguards during sport activities in paediatric age. Eur. J. Paediatr. Dent. 2007, 8, 193–198. [Google Scholar] [PubMed]
- Tausche, E.; Luck, O.; Harzer, W. Prevalence of malocclusions in the early mixed dentition and orthodontic treatment need. Eur. J. Orthod. 2004, 26, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Keski-Nisula, K.; Lehto, R.; Lusa, V.; Keski-Nisula, L.; Varrela, J. Occurrence of malocclusion and need of orthodontic treatment in early mixed dentition. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Ingelsson-Dahlström, M.; Hagberg, C. The longitudinal development of malocclusion in postnormal children with little respectively urgent need for orthodontic treatment. Swed. Dent. J. 1994, 18, 49–57. [Google Scholar] [PubMed]
- Al Nimri, K.; Richardson, A. Interceptive orthodontics in the real world of community dentistry. Int. J. Paediatr. Dent. 2008, 10, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Pavlow, S.S.; McGorray, S.P.; Taylor, M.G.; Dolce, C.; King, G.J.; Wheeler, T.T. Effect of early treatment on stability of occlusion in patients with Class II malocclusion. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Spinas, E.; Aresu, M.; Giannetti, L. Use of Mouth Guard in Basketball: Observational Study of a Group of Teenagers with and without Motivational Reinforcement. Eur. J. Paediatr. Dent. 2014, 15, 392–396. [Google Scholar] [PubMed]
- Corbett, M.C. Class II treatment with elastodontics. J. Clin. Orthod. 1992, 26, 419–424. [Google Scholar] [PubMed]
- Methenitou, S.; Shein, B.; Ramanathan, G.; Bergersen, E.O. Prevention of overbite and overjet development in the 3 to 8 year old by controlled nighttime guidance of incisal eruption: A study of 43 individuals. J. Pedod. 1990, 14, 219–230. [Google Scholar] [PubMed]
- Massaro, C.; Garib, D.; Cevidanes, L.; Janson, G.; Yatabe, M.; Lauris, J.R.P.; Ruellas, A.C. Maxillary dentoskeletal outcomes of the expander with differential opening and the fan-type expander: A randomized controlled trial. Clin. Oral Investig. 2021, 25, 5247–5256. [Google Scholar] [CrossRef] [PubMed]
- Ortu, E.; Barrucci, G.; Aprile, G.; Guerrini, L.; Pietropaoli, D.; Monaco, A. Electro-myographic evaluation during orthodontic therapy: Comparison of two elastodontic devices. J. Biol. Regul. Homeost. Agents 2020, 34, 1935–1939. [Google Scholar] [CrossRef] [PubMed]
- Fichera, G.; Martina, S.; Palazzo, G.; Musumeci, R.; Leonardi, R.; Isola, G.; Lo Giudice, A. New Materials for Orthodontic Interceptive Treatment in Primary to Late Mixed Dentition. A Retrospective Study Using Elastodontic Devices. Materials 2021, 4, 1695. [Google Scholar] [CrossRef] [PubMed]
- Ortu, E.; Pietropaoli, D.; Cova, S.; Marci, M.C.; Monaco, A. Efficacy of elastodontic devices in overjet and overbite reduction assessed by computer-aid evaluation. BMC Oral Health 2021, 21, 269. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Ciavarella, D.; Campobasso, A.; Campa, R.; Suriano, C.; Illuzzi, G.; Cazzolla, A.P.; Tepedino, M. Cephalometric effects of the elastodontic appliance in managing skeletal class ii division 1 cases. Aust. Orthod. J. 2021, 37, 251–258. [Google Scholar] [CrossRef]
- Galluccio, G.; Guarnieri, R.; Jamshir, D.; Impellizzeri, A.; Ierardo, G.; Barbato, E. Comparative Evaluation of Esthetic and Structural Aspects in Class II Functional Therapy. A Case–Control Retrospective Study. Int. J. Environ. Res. Public Health 2021, 18, 6978. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Ceci, S.; Patano, A.; Inchingolo, A.M.; Montenegro, V.; Di Pede, C.; Malcangi, G.; Marinelli, G.; Coloccia, G.; Garibaldi, M.; et al. Elastodontic Therapy of Hyperdivergent Class II Patients Using AMCOP® Devices: A Retrospective Study. Appl. Sci. 2022, 12, 3259. [Google Scholar] [CrossRef]
- Lanteri, V.; Cagetti, M.G.; Ugolini, A.; Gaffuri, F.; Maspero, C.; Abate, A. Skeletal and dento-alveolar changes obtained with customised and preformed eruption guidance appliances after 1-year treatment in early mixed dentition. Eur. J. Paediatr. Dent. 2023, 24, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, A.; Ronsivalle, V.; Santonocito, S.; Lucchese, A.; Venezia, P.; Marzo, G.; Leonardi, R.; Quinzi, V. Digital analysis of the occlusal changes and palatal morphology using elastodontic devices. A prospective clinical study including Class II subjects in mixed dentition. Eur. J. Paediatr. Dent. 2022, 23, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Patano, A.; Inchingolo, A.M.; Cardarelli, F.; Inchingolo, A.D.; Viapiano, F.; Giotta, M.; Bartolomeo, N.; Di Venere, D.; Malcangi, G.; Minetti, E.; et al. Effects of Elastodontic Appliance on the Pharyngeal Airway Space in Class II Malocclusion. J. Clin. Med. 2023, 12, 4280. [Google Scholar] [CrossRef]
- Ronsivalle, V.; Quinzi, V.; La Rosa, S.; Leonardi, R.; Lo Giudice, A. Comparative Analysis of Skeletal Changes, Occlusal Changes, and Palatal Morphology in Children with Mild Class III Malocclusion Treated with Elastodontic Appliances and Bimaxillary Plates. Children 2023, 1, 1219. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.R.; Lai, C.L.; Chang, I.T.; Hsu, C.L.; Liu, J.F.; Kao, C.T. Evaluation of skeletal and dentoalveolar changes in class II division I pediatric patients receiving myofunctional appliance therapy: A preliminary study. J. Formos. Med. Assoc. 2022, 121, 2028–2034. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Lai, G.; Wang, J. Effect of orofacial myofunctional therapy along with preformed appliances on patients with mixed dentition and lip incompetence. BMC Oral Health 2022, 22, 586. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; He, J.M.; Zheng, W.Y. Comparison of rapid maxillary expansion and pre-fabricated myofunctional appliance for the management of mouth breathers with Class II malocclusion. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Ciftci, V.; Uzel, A. Dento-skeletal effects of myofunctional appliance on patients with class II div 1 in mixed dentition stage: A cephalometric study. Pediatr. Dent. J. 2021, 31, 235–241. [Google Scholar] [CrossRef]
- Çoban Büyükbayraktar, Z.; Camcı, H. Dentoalveolar, skeletal, pharyngeal airway, cervical posture, hyoid bone position, and soft palate changes with Myobrace and Twin-block: A retrospective study. BMC Oral Health 2023, 23, 53. [Google Scholar] [CrossRef]
- Usumez, S.; Uysal, T.; Sari, Z.; Basciftci, F.A.; Karaman, A.I.; Guray, E. The effects of early preorthodontic trainer treatment on class II, division 1 patients. Angle Orthod. 2004, 74, 605–609. [Google Scholar] [PubMed]
- Johnson, J.S.; Satyaprasad, S.; Sharath Chandra, H.; Havaldar, K.S.; Raj, A.; Suresh, N. A Comparative Evaluation of the Dentoskeletal Treatment Effects Using Twin Block Appliance and Myobrace System on Class II Division I Malocclusion. Int. J. Clin. Pediatr. Dent. 2021, 14, S10–S17. [Google Scholar] [CrossRef] [PubMed]
- Madian, A.M.; Elfouly, D. Cephalometric changes in pharyngeal airway dimensions after functional treatment with twin block versus myobrace appliances in developing skeletal class II patients: A randomized clinical trial. BMC Oral Health 2023, 23, 998. [Google Scholar] [CrossRef] [PubMed]
- Farronato, G.; Giannini, L.; Galbiati, G.; Grillo, E.; Maspero, C. Occlus-o-Guide® versus Andresen activator appliance: Neuromuscular evaluation. Prog. Orthod. 2013, 14, 4. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hanoun, A.A.; Rao, G.K.; Khamis, M.F.; Mokhtar, N. Efficacy of the Prefabricated Myofunctional Appliance T4FTM in Comparison to Twin Block Appliance for Class II Division 1 Malocclusion Treatment: A Randomized Clinical Trial. Malays. J. Med. Health Sci. 2020, 16, 307–316. [Google Scholar]
- Papageorgiou, S.N.; Koletsi, D.; Eliades, T. What evidence exists for myofunctional therapy with prefabricated appliances? A systematic review with meta-analyses of randomised trials. J. Orthod. 2019, 46, 297–310. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, H.; Čirgić, E.; Rizk, M.Z.; Vandevska-Radunovic, V. Effectiveness of prefabricated myofunctional appliances in the treatment of Class II division 1 malocclusion: A systematic review. Eur. J. Orthod. 2020, 42, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Rusli, R.O.; Achmad, H.; Kuandinata, W.; Fatimah, I.; Nurwahidah, A.; Halid, S.; La Mente, N.H. Myobrace versus twin block in the treatment of class II malocclusion in Children: A systematic review. Saudi Dent. J. 2024, 36, 661–664. [Google Scholar] [CrossRef] [PubMed]
- Idris, G.; Hajeer, M.Y.; Al-Jundi, A. Soft- and hard-tissue changes following treatment of Class II division 1 malocclusion with Activator versus Trainer: A randomized controlled trial. Eur. J. Orthod. 2019, 41, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Frilund, E.; Sonesson, M.; Magnusson, A. Patient compliance with Twin Block appliance during treatment of Class II malocclusion: A randomized controlled trial on two check-up prescriptions. Eur. J. Orthod. 2023, 45, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Marra, P.M.; Fiorillo, L.; Cervino, G.; Cardarelli, F.; Cicciù, M.; Laino, L. Elastodontic treatment with oral bio-activators in young children. Minerva Dent. Oral Sci. 2022, 71, 270–276. [Google Scholar] [CrossRef] [PubMed]
| Database | Search Strategy | Number of Results |
|---|---|---|
| Scopus | (TITLE-ABS-KEY ((“children” OR “mixed dentition” OR “deciduous dentition” OR “primary dentition” OR “deciduous teeth” OR “primary teeth”)) AND TITLE-ABS-KEY ((“elastodontic” OR “myofunctional” OR “prefabricated functional appliance” OR “myobrace”))) | 504 |
| Web of Science | (“children” OR “mixed dentition” OR “deciduous dentition” OR “primary dentition” OR “deciduous teeth” OR “primary teeth”) (Topic) and (“elastodontic” OR “myofunctional” OR “prefabricated functional appliance” OR “myobrace”) (Topic) | 446 |
| Embase | (‘children’/exp OR ‘children’ OR ‘mixed dentition’/exp OR ‘mixed dentition’ OR ‘deciduous dentition’/exp OR ‘deciduous dentition’ OR ‘primary dentition’/exp OR ‘primary dentition’ OR ‘deciduous teeth’/exp OR ‘deciduous teeth’ OR ‘primary teeth’/exp OR ‘primary teeth’) AND (‘elastodontic’ OR ‘myofunctional’ OR ‘prefabricated functional appliance’ OR ‘myobrace’) | 426 |
| PubMed | (“children” OR “mixed dentition” OR “deciduous dentition” OR “primary dentition” OR “deciduous teeth” OR “primary teeth”) AND (“elastodontic” OR “myofunctional” OR “prefabricated functional appliance” OR “myobrace”) | 286 |
| Author (Year) [Reference] | Sample: M/F (Age) | Sample Size Calculation | Malocclusion | Intervention (Device and Wear Instructions) | Comparison | Compliance | Follow-Up |
|---|---|---|---|---|---|---|---|
| Chen LR et al. (2022) [23] | Test group: 13: 9M/4F (9.3 years) Control group: 13: 9M/4F (9.9 years) | No | Class II div 1 | PMA 2 h/daytime + all night Breathing exercise Lip exercise Tongue exercise | Untreated patients | NA | 1 year |
| Ciavarella D et al. (2021) [16] | Test group: 20: 9M/11F (9.4 ± 0.3 years) Control group: 20: 7M/13F (9.7 ± 0.4 years) | No | Class II | PMA AMCOP 4 h/daytime + all night myofunctional exercises | Untreated patients | NA | 2 years |
| Ciftci V et al. (2021) [26] | Test group: 18: 8M/10F (9.97 ± 1.36 years) Control group: NA | Yes | Class II div 1 | Multi-P myofunctional appliance 4 h/daytime + all night | No | Yes | 2.94 ± 0.70 years |
| Çoban Büyükbayraktar Z et al. (2023) [27] | Test group: 18: NR (12.14 ± 1.23 years) Control group: 18: NR (12.14 ± 1.23 years) | Yes | Class II | Myobrace N/R | Twin-block N/R | NA | 6 months |
| Fichera G et al. (2021) [12] | Test group: 20: 8M/12F (8.4 ± 0.6years) Control group: 20: 9M/11F (8.1 ± 0.8 years) | No | Class II | AMCOP second class 1 h/daytime + all night | Untreated patients | NA | 1 year |
| Galluccio G et al. (2021) [17] | Test group 3 (Oclusoguide): 24: 13M/11F (9.05 ± 0.39 years) Control group 1 (Frankel): 23: 14M/9F (10.3 ± 1.08 years) Control group 2 (twin-block): 18: 10M/8F (10.7 ± 1.05 years) Control group 3 (untreated): 20: 11M/9F (12.17 ± 1.7 years) | No | Class II div 1 | PMA Occlus-o-Guide N/R | Control group 1: Fränkel-2 appliance N/R Control group 2: Twin-block N/R Control group 3: Untreated patients | NA | 12 months |
| Inchingolo AD et al. (2022) [18] | Test group: 21: 10M/11F (8.22 ± 1.17 years) Control group: NA | No | Class II | AMCOP Integral AMCOP second class AMCOP Open 1 h/daytime + all night for 6–8 months, and then only at night | N/R | NA | 16–18 months |
| Johnson JS et al. (2021) [29] | Test group 1 (myobrace) 10: N/R (10.40 ± 1.89 years) Control group 1 (twin-block): 10: N/R (10.850 ± 1.37 years) Control group 2 (untreated): 10: N/R (10.60 ± 1.77 years) | No | Class II div 1 | Myobrace 1–2 h/daytime + 10–12 h/night | Control Group 1: Twin-block 24 h/day Control group 2: untreated patients | N/R | 18–24 months |
| Lanteri V et al. (2022B) [19] | Test group: 36: 17M/19F (7.9 ± 0.7 years) Control group: 33: 15M/18F (7.7 ± 0.5 years) | Yes | Class I Class II | Customized eruption guide appliance 2 h/daytime + all night | Preformatted eruption guide appliance 2 h/daytime + all night | NA | 1 year |
| Lo Giudice A et al. (2022) [20] | Test group: 19: 9M/10F (9.1 ± 0.7 years) Control group: 17: 7M/10F (8.8 ± 0.8 years) | Yes | Class II | AMCOP second class 1 h/daytime + all night Lip exercises | Untreated patients | N/R | 1 year |
| Madian AM et al. (2023) [30] | Test group: 13 (9–12 years) Control group: 13 (9–12 years) | Yes | Class II | Myobrace A minimum of 1–2 h per day and overnight | Twin-block All times except for eating | Yes | 6 months |
| Patano A et al. (2023) [21] | Test group: 33: 14M/19F (8.9 ± 1.6 years) Control: 35: 18M/17F (8.9 ± 0.4 years) | No | Class II | AMCOP bioactivators 1 h during the day and throughout the night for 6–8 months, and then only at night | Untreated patients | NA | 3 years (including treatment) |
| Ronsivalle V et al. (2023) [22] | Test group: 10: 5M/5F (7.5 ± 0.9 years) Control: 10 (7M/3F) (6.9 ± 1 years) | Yes | Class III | Class III elastodontic mono-block appliance AMCOP Class III activator At night and for two hours during the day | Bi-maxillary plates with class III elastics At night and for two hours during the day | NA | 1 year |
| Usumez S et al. (2004) [28] | Test group: 20: 10M/10F (9.6 ± 1.3 years) Control: 20: 10M/10F (10.2 ± 0.8 years) | No | Class II div 1 | Preorthodontic trainer appliance (Myofunctional Research Co., Queensland, Australia) Every day for one hour and overnight | Untreated patients | NA | - |
| Yang X et al. (2022) [24] | Test group: 56: 30/26 (8.1 ± 1.1 years) Control: 53: 25/28 (8.2 ± 1.0 years) | No | Class I or II | Preformed appliances (MRC Myofunctional Research Co. Queensland, Australia) At night (≥ 8 h) during sleep and continuously for 2 h during the day | Conventional early orthodontic appliances (arch expansion devices along with “2 × 4” local fixed appliances) | NA | 2 years |
| Zhang X et al. (2021) [25] | Test group: 14 (9.2 years) Control: 14 (10 years) | No | Class II div 1 | T4K At least 14 h per day (overnight use and at least two hours during the day) | Hyrax appliance | NA | 1 year |
| Author (Year) [Reference] | Intragroup Meas. Difference (T1 − T0)/p Value | Intergroup Meas. Difference (Elastomeric Appliance − Control) p Value | |
|---|---|---|---|
| Elastomeric Appliance Group | Control Group | ||
| Chen LR et al. (2022) [23] | SNA: 0.80 (1.71)/0.106 SNB: 1.87 (1.89)/0.004 ANB: −1.15 (1.15)/0.011 Ar-B: 3.61 (2.33)/0.002 OVB: NR OVJ: NR FMA: −0.25 (2.31)/0.664 SN-Go-Gn: −0.85 (3.11)/0.305 | SNA: 0.91 (2.20)/0.150 SNB: 0.95 (1.10)/0.013 ANB: −0.12 (2.11)/0.325 Ar-B: 3.68 (4.07)/0.003 OVB: NR OVJ: NR FMA: 0.82 (3.40)/0.477 SN-Go-Gn: −0.60 (1.94)/0.154 | SNA: 0.917 SNB: 0.143 ANB: 0.164 Ar-B: 0.606 OVB: NR OVJ: NR FMA: 0.680 SN-Go-Gn: 0.408 |
| Ciavarella D et al. (2021) [16] | SNA: NR SNB: NR ANB: NR Co-Gn: 9.3/≤0.05 OVB: NR OVJ: NR FMA: NR SN-Go-Me: −1/NS | SNA: NR SNB: NR ANB: NR Co-Gn: −0.5/NS OVB: NR OVJ: NR FMA: NR SN-Go-Me: −0.85/≤0.01 | SNA: NR SNB: NR ANB: NR Co-Gn: 0.0173 OVB: NR OVJ: NR FMA: NR SN-Go-Me: 0.3378 |
| Ciftci V et al. (2021) [26] | SNA: −0.96/0.346 SNB: 1.3/0.236 ANB: −1.6/0.001 Go-Gn: 3.66/0.030 Co-Gn: 1.51/0.833 OVB: 1.12/0.261 OVJ: −4.58/0.000 FMA: −1.9/0.082 SN-Go-Gn: −0.91/0.451 | NR | NR |
| Çoban Büyükbayraktar Z et al. (2023) [27] | SNA: 0.20 (1.04)/0.415 SNB: 0.61 (0.80)/0.004 ANB: −0.38 (1.19)/0.178 Go-Pg: 1.61 (5.14)/0.188 Co-Gn: 2.31 (8.4)/0.248 OVB: −0.10 (2.27)/0.407 OVJ: −2.92 (3.47)/0.001 FMA: 0.66 (3.07)/0.360 SN-Go-Gn: 0.66 (1.84)1/0.429 | SNA: −0.44 (0.97)/0.001 SNB: 1.31 (1.42)/0.001 ANB: −1.75 (1.08)/0.001 Go-Pg: 2.68 (3.70)/0.01 Co-Gn: 4.77 (4.60)/0.003 OVB: −0.21 (1.94)/0.255 OVJ: −2.99 (1.93)/0.216 FMA: 1.65 (2.95)/0.001 SN-Go-Gn: 0.96 (1.44)/0.001 | SNA: 0.554 SNB: 0.52 ANB: 0.608 Go-Pg: 0.861 Co-Gn: 0.310 OVB: 0.502 OVJ: 0.331 FMA: 0.703 SN-Go-Gn: 0.409 |
| Fichera G et al. (2021) [12] | SNA: 0.66/NS SNB: 2.7/<0.05 ANB: −1.94/<0.05 OVB: −2.6/<0.05 OVJ: −2.6/<0.05 FMA: NR SN-Go-Gn: NR | SNA: NR SNB: NR ANB: NR OVJ: 0.3/NS OVB: 0.7/<0.05 FMA: NR SN-Go-Gn: NR | SNA: NR SNB: NR ANB: NR OVJ: NR OVB: NR FMA: NR SN-Go-Gn: NR |
| Galluccio G et al. (2021) [17] | SNA: −0.58 (1.89)/0.178 SNB: 1.42 (2.08)/0.002 ANB: −1.96 (1.12)/<0.001 Ar-Pg: 6.13 (3.11)/<0.001 OVB: −1.04 (1.27)/0.002 OVJ: −3.13 (1.85)/<0.001 FMA: NR SN-Go-Gn: −0.38 (2.81)/0.531 | Control Group 1 (FR-2): SNA: −0.09 (0.996)/0.68 SNB: 2.13 (0.97)/<0.001 ANB: −2.17 (0.78)/<0.001 Ar-Pg: 6.74 (2.68)/<0.001 OVB: −1.65 (1.87)/0.001 OVJ: −3.17 (1.92)/<0.001 FMA: NR SN-Go-Gn: −0.57 (2.86)/0.28 Control Group 2 (TB): SNA: −0.17 (0.86)/0.298 SNB: 2.28 (1.07)/<0.001 ANB: −2.33 (1.03)/<0.001 Art-Pg: 6.78 (1.55)/<0.001 OVB: −2.22 (1.06)/<0.001 OVJ: −4.28 (0.89)/<0.001 FMA: NR SN-Go-Gn: 0.33 (3.03)/0.428 Control Group 3 (Untreated): SNA: 0.41 (0.4) SNB: 0.7 (0.5) ANB: −0.2 (0.1) Art-Pg: 4.1 (3.2) OVB: 0.3 (0.6) OVJ: 0.1 (0.1) FMA: NR SN-Go-Gn: −0.7 (0.6) | Occlus-o-Guide vs. Control group SNA 0.017 SNB: 0.105 ANB: <0.001 Ar-Pg: 0.004 OVB: <0.001 OVJ: <0.001 FMA: NR SN-Go-Gn: 0.576 Occlus-o-Guide vs. TB SNA: NR SNB: NR ANB: NR Art-Pg: NR OVB: 0.041 OVJ: 0.02 FMA: NR SN-Go-Gn: NR |
| Inchingolo AD et al. (2022) [18] | SNA: −0.04/0.9484 SNB: 2.17/0.0015 ANB: −2.28/0.0001 OVB: 2.12/0.1245 OVJ: −2.64/0.0002 FMA: NR SN-Go-Gn: −2.87/0.0014 | NR | NR |
| Johnson JS et al. (2021) [29] | SNA: −0.09 (0.62)/0.661 SNB: 1.35 (0.97)/0.002 ANB: −1.14 (1.33)/0.024 Go-Me: 1.75 (0.97)/0.000 Ar-Gn: 1.55 (0.76)/0.000 OVB: −0.08 (1.17)/0.834 OVJ: −3.55 (2.59)/0.002 FMA: NR SN-Go-Gn: −0.70 (0.88)/0.034 | Control group 1 (TB): SNA: −0.30 (0.48)/0.081 SNB: 2.00 (1.33)/<0.001 ANB: −2.20 (1.22)/0.000 Go-Me: 3.90 (2.95)/0.002 Ar-Gn: 4.60 (4.56)/0.011 OVB: −1.25 (1.03)/0.004 OVJ: −5.10 (3.07)/0.001 FMA: NR SN-Go-Gn: 0.18 (0.49)/0.281 Control group 2 (Untreated): SNA: −0.01 (0.63)/0.961 SNB: 0.30 (0.35)/<0.001 ANB: −0.21 (0.72)/0.386 Go-Me: 0.50 (0.70)/0.052 Ar-Gn: 0.20 (0.34)/0.104 OVB: 0.34 (0.47)/0.049 OVJ: 0.19 (1.15)/0.616 FMA: NR SN-Go-Gn: −0.34 (0.73)/0.178 | Myobrace vs. TB: SNA: 0.489 SNB: 0.176 ANB: 0.053 Go-Me: 0.107 Ar-Gn: 0.037 OVB: 0.039 OVJ: 0.148 FMA: NR SN-Go-Gn: 0.026 Myobrace vs. control: SNA: 0.875 SNB: 0.001 ANB: 0.101 Go-Me: 0.005 Ar-Gn: <0.001 OVB: 0.314 OVJ: <0.001 FMA: NR SN-Go-Gn: 0.421 |
| Lanteri V et al. (2022B) [19] | SNA: 0.79/0.14 SNB: 2.42/<0.05 ANB: −1.43/<0.05 OVB: −1.86/<0.01 OVJ: −2.36/<0.01 FMA: NR SN-Go-Gn: 2.23/<0.05 | SNA: 0.83/0.12 SNB: 1.75/<0.05 ANB: 0.97/<0.05 OVB: −1.24/<0.05 OVJ: −2.22/<0.01 FMA: NR SN-Go-Gn: 0.98/0.083 | SNA: 0.33 SNB: 0.09 ANB: 0.17 OVB: <0.05 OVJ: 0.08 FMA: NR SN-Go-Gn: <0.05 |
| Lo Giudice A et al. (2022) [20] | SNA: 0.4/NS SNB: 2.4/<0.05 ANB: −2.1/<0.05 OVB: −2.2/<0.05 OVJ: −2.8/<0.05 FMA: NR SN-Go-Gn: NR | SNA: NR SNB: NR ANB: NR OVB: 0.5/NS OVJ: 0.6/NS FMA: NR SN-Go-Gn: NR | Matching Percentage (<0.05) |
| Madian AM et al. (2023) [30] | SNA: 0.64 (1.08)/0.06 SNB: 2.82 (3.32)/0.01 ANB: −2.42 (2.70)/0.007 OVB: NR OVJ: NR FMA: 0.80 (4.00)/0.49 SN-Go-Gn: NR | SNA: −0.03 (0.47)/0.82 SNB: 3.79 (3.06)/0.001 ANB: −3.06 (1.14)/<0.001 OVB: NR OVJ: NR FMA: −2.69 (5.96)/0.13 SN-Go-Gn: NR | SNA: 0.06 SNB: 0.45 ANB: 0.43 OVB: NR OVJ: NR FMA: 0.09 SN-Go-Gn: NR |
| Patano A et al. (2023) [21] | SNA: −1/0.0053 SNB: 1.3/<0.0001 ANB: −2.2/<0.0001 Co-Me: 8.5/<0.0001 OVB: 0.3/0.5079 OVJ: −2.1/<0.0001 FMA: −0.8/0.0773 SN-Go-Gn: −0.2/0.5227 | SNA: 0.4/0.2515 SNB: 0.6/0.0617 ANB: −0.2/0.5204 Co-Me: 5.4/<0.0001 OVB: 1.4/0.0001 OVJ: 0.2/0.2132 FMA: −0.9/0.0221 SN-Go-Gn: −0.4/0.2062 | SNA: 0.008 SNB: 0.102 ANB: <0.001 Co-Me: 0.102 OVB: 0.01 OVJ: <0.001 FMA: 0.915 SN-Go-Gn: 0.8 |
| Ronsivalle V et al. (2023) [22] | SNA: 0.8/0.071 SNB: −1.8/<0.05 ANB: 2.6/<0.05 OVB: NR OVJ: 3.1/<0.05 FMA: NR SN-Go-Gn: NR | SNA: 1/0.084 SNB: −2.1/<0.05 ANB: 3.1/<0.05 OVB: NR OVJ: 2.9/<0.05 FMA: NR SN-Go-Gn: NR | SNA: 0.168 SNB: 0.211 ANB: 0.114 OVB: NR OVJ: 0.163 FMA: NR SN-Go-Gn: NR |
| Usumez S et al. (2004) [28] | SNA: 0.13 (1.02)/NS SNB: 1.31 (1.35)/0.001 ANB: −1.19 (1.18)/0.001 Co-Gn: 2.88 (4.53)/0.023 OVB: −0.22 (1.76)/NS OVJ: −3.75 (1.60)/0.000 FMA: NR SN-Go-Gn: −1.50 (1.76)/0.003 | SNA: −0.11 (1.70)/NS SNB: 0.41 (1.64)/NS ANB: −0.50 (1.24)/NS Co-Gn: 1.47 (2.60)/0.021 OVB: 0.06 (0.39)/NS OVJ: −0.13 (0.78)/NS FMA: NR SN-Go-Gn: −0.34 (1.90)/NS | SNA: NS SNB: NS ANB: NS Co-Gn: NS OVB: NS OVJ: 0.000 FMA: NR SN-Go-Gn: NS |
| Yang X et al. (2022) [24] | SNA: 0.32 (1.98)/0.23 SNB: 1.06 (1.58)/0.00 ANB: NR OVB: NR OVJ: NR FMA: 0.18 (2.12)/0.53 SN-Go-Gn: NR | SNA: −0.02 (1.82)/0.94 SNB: 0.43 (1.55)/0.05 ANB: NR OVB: NR OVJ: NR FMA: −0.02 (2.64)/0.96 SN-Go-Gn: NR | SNA: 0.35 SNB: 0.04 ANB: NR OVB: NR OVJ: NR FMA: 0.67 SN-Go-Gn: NR |
| Zhang X et al. (2021) [25] | SNA: 1.39 (1.11)/0.022 SNB: 2.48 (1.27)/0.003 ANB: −1.06 (1.10)/0.055 Go-Me: 3.50 (2.07)/0.006 Pg/OLP: 3.41 (2.04)/0.006 OVB: NR OVJ: 0.81 (3.54)/0.594 FMA: NR SN-Go-Gn: NR | SNA: 0.05 (1.39)/0.906 SNB: 0.39 (1.50)/0.39 ANB: −0.34 (1.17)/0.337 Go-Me: 1.00 (2.09)/0.124 Pg/OLP: 2.33 (3.19)/0.039 OVB: NR OVJ: −0.92 (2.28)/0.186 FMA: NR SN-Go-Gn: NR | SNA: 0.013 SNB: 0.001 ANB: 0.123 Go-Me: 0.006 Pg/OLP: 0.239 OVB: NR OVJ: 0.161 FMA: NR SN-Go-Gn: NR |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ureni, R.; Verdecchia, A.; Suárez-Fernández, C.; Mereu, M.; Schirru, R.; Spinas, E. Effectiveness of Elastodontic Devices for Correcting Sagittal Malocclusions in Mixed Dentition Patients: A Scoping Review. Dent. J. 2024, 12, 247. https://doi.org/10.3390/dj12080247
Ureni R, Verdecchia A, Suárez-Fernández C, Mereu M, Schirru R, Spinas E. Effectiveness of Elastodontic Devices for Correcting Sagittal Malocclusions in Mixed Dentition Patients: A Scoping Review. Dentistry Journal. 2024; 12(8):247. https://doi.org/10.3390/dj12080247
Chicago/Turabian StyleUreni, Rebecca, Alessio Verdecchia, Carlota Suárez-Fernández, Manuela Mereu, Roberto Schirru, and Enrico Spinas. 2024. "Effectiveness of Elastodontic Devices for Correcting Sagittal Malocclusions in Mixed Dentition Patients: A Scoping Review" Dentistry Journal 12, no. 8: 247. https://doi.org/10.3390/dj12080247
APA StyleUreni, R., Verdecchia, A., Suárez-Fernández, C., Mereu, M., Schirru, R., & Spinas, E. (2024). Effectiveness of Elastodontic Devices for Correcting Sagittal Malocclusions in Mixed Dentition Patients: A Scoping Review. Dentistry Journal, 12(8), 247. https://doi.org/10.3390/dj12080247







