Investigating the Relationship between Oral Health and Severe Mental Illness: Analysis of NHANES 1999–2016
Abstract
1. Introduction
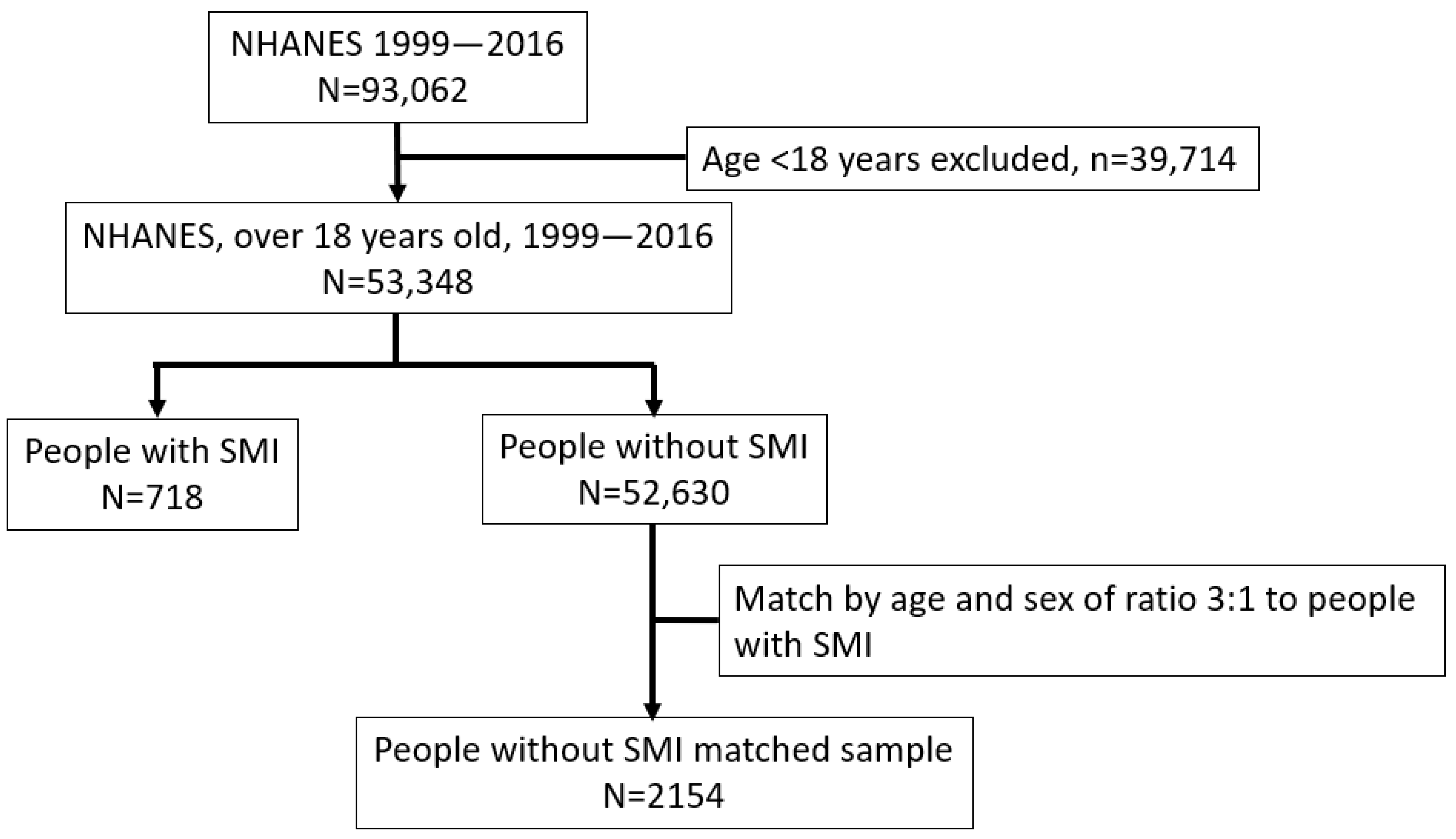
2. Methods
3. Results
3.1. Characteristics between People with and without SMI
3.2. Oral Health in People with and without SMI
3.3. Risk Factors of Poor Oral Health in People with SMI
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Firth, J.; Siddiqi, N.; Koyanagi, A.; Siskind, D.; Rosenbaum, S.; Galletly, C.; Allan, S.; Caneo, C.; Carney, R.; Carvalho, A.F.; et al. The Lancet Psychiatry Commission: A blueprint for protecting physical health in people with mental illness. Lancet Psychiatry 2019, 6, 675–712. [Google Scholar] [CrossRef] [PubMed]
- Ruggeri, M.; Leese, M.; Thornicroft, G.; Bisoffi, G.; Tansella, M. Definition and prevalence of severe and persistent mental illness. Br. J. Psychiatry 2000, 177, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Palmier-Claus, J.E.; Shiers, D.; French, P.; Harris, R.; Laverty, L. Oral health in psychosis: An unmet need. Schizophr. Res. 2019, 204, 442. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.; Palmier-Claus, J.; Wu, J.; Shiers, D.; Larvin, H.; Doran, T.; Aggarwal, V.R. Periodontal disease in people with a history of psychosis: Results from the UK biobank population-based study. Community Dent. Oral Epidemiol. 2023, 51, 985–996. [Google Scholar] [CrossRef] [PubMed]
- Joury, E.; Kisely, S.; Watt, R.G.; Ahmed, N.; Morris, A.J.; Fortune, F.; Bhui, K. Mental Disorders and Oral Diseases: Future Research Directions. J. Dent. Res. 2023, 102, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Kisely, S.; Quek, L.H.; Pais, J.; Lalloo, R.; Johnson, N.W.; Lawrence, D. Advanced dental disease in people with severe mental illness: Systematic review and meta-analysis. Br. J. Psychiatry 2011, 199, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Chen, P.; He, M.X.; Lu, M.; Wang, H.M.; Soares, J.C.; Zhang, X.Y. Poor oral health in patients with schizophrenia: A systematic review and meta-analysis. Schizophr. Res. 2018, 201, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Kilbourne, A.M.; Horvitz-Lennon, M.; Post, E.P.; McCarthy, J.F.; Cruz, M.; Welsh, D.; Blow, F.C. Oral health in Veterans Affairs patients diagnosed with serious mental illness. J. Public Health Dent. 2007, 67, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Hugo, F.N.; Hilgert, J.B.; de Sousa Mda, L.; Cury, J.A. Oral status and its association with general quality of life in older independent-living south-Brazilians. Community Dent. Oral Epidemiol. 2009, 37, 231–240. [Google Scholar] [CrossRef]
- Yamamoto, T.; Kondo, K.; Aida, J.; Fuchida, S.; Hirata, Y.; JAGES Group. Association between the longest job and oral health: Japan Gerontological Evaluation Study project cross-sectional study. BMC Oral Health 2014, 14, 130. [Google Scholar] [CrossRef]
- Hede, B. Dental health behavior and self-reported dental health problems among hospitalized psychiatric patients in Denmark. Acta Odontol. Scand. 1995, 53, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Cook, B.L.; Wayne, G.F.; Kafali, E.N.; Liu, Z.; Shu, C.; Flores, M. Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. JAMA 2014, 311, 172–182. [Google Scholar] [CrossRef] [PubMed]
- Bahorik, A.L.; Newhill, C.E.; Queen, C.C.; Eack, S.M. Under-reporting of drug use among individuals with schizophrenia: Prevalence and predictors. Psychol. Med. 2014, 44, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Teasdale, S.B.; Ward, P.B.; Samaras, K.; Firth, J.; Stubbs, B.; Tripodi, E.; Burrows, T.L. Dietary intake of people with severe mental illness: Systematic review and meta-analysis. Br. J. Psychiatry 2019, 214, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Scully, C. Drug effects on salivary glands: Dry mouth. Oral Dis. 2003, 9, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Plemons, J.M.; Al-Hashimi, I.; Marek, C.L.; American Dental Association Council on Scientific Affairs. Managing xerostomia and salivary gland hypofunction: Executive summary of a report from the American Dental Association Council on Scientific Affairs. J. Am. Dent. Assoc. 2014, 145, 867–873. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, J.; Munk-Jorgensen, P.; Skadhede, S.; Correll, C.U. Determinants of poor dental care in patients with schizophrenia: A historical, prospective database study. J. Clin. Psychiatry 2011, 72, 140–143. [Google Scholar] [CrossRef]
- Turner, E.; Berry, K.; Aggarwal, V.R.; Quinlivan, L.; Villanueva, T.; Palmier-Claus, J. Oral health self-care behaviours in serious mental illness: A systematic review and meta-analysis. Acta Psychiatr. Scand. 2022, 145, 29–41. [Google Scholar] [CrossRef] [PubMed]
- Leite, R.S.; Marlow, N.M.; Fernandes, J.K.; Hermayer, K. Oral health and type 2 diabetes. Am. J. Med. Sci. 2013, 345, 271–273. [Google Scholar] [CrossRef]
- Vancampfort, D.; Correll, C.U.; Galling, B.; Probst, M.; De Hert, M.; Ward, P.B.; Rosenbaum, S.; Gaughran, F.; Lally, J.; Stubbs, B. Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: A systematic review and large scale meta-analysis. World Psychiatry 2016, 15, 166–174. [Google Scholar] [CrossRef]
- Kisely, S.; Baghaie, H.; Lalloo, R.; Siskind, D.; Johnson, N.W. A systematic review and meta-analysis of the association between poor oral health and severe mental illness. Psychosom. Med. 2015, 77, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Wey, M.C.; Loh, S.; Doss, J.G.; Abu Bakar, A.K.; Kisely, S. The oral health of people with chronic schizophrenia: A neglected public health burden. Aust. N. Z. J. Psychiatry 2016, 50, 685–694. [Google Scholar] [CrossRef] [PubMed]
- National Health and Nutrition Examination Survey. National Center for Health Statistics. 2015. Available online: https://www.cdc.gov/nchs/index.htm (accessed on 1 October 2020).
- Hong, J.; Whelton, H.; Douglas, G.; Kang, J. Consumption frequency of added sugars and UK children’s dental caries. Community Dent. Oral Epidemiol. 2018, 46, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Rubin, D.B.; Schenker, N. Multiple imputation in health-care databases: An overview and some applications. Stat. Med. 1991, 10, 585–598. [Google Scholar] [CrossRef] [PubMed]
- Lamster, I.B.; DePaola, D.P.; Oppermann, R.V.; Papapanou, P.N.; Wilder, R.S. The relationship of periodontal disease to diseases and disorders at distant sites: Communication to health care professionals and patients. J. Am. Dent. Assoc. 2008, 139, 1389–1397. [Google Scholar] [CrossRef] [PubMed]
- Saintrain, M.V.; de Souza, E.H. Impact of tooth loss on the quality of life. Gerodontology 2012, 29, e632–e636. [Google Scholar] [CrossRef] [PubMed]
- Sheiham, A. Oral health, general health and quality of life. Bull. World Health Organ. 2005, 83, 644. [Google Scholar] [PubMed]
- FDI World Dental Federation. Access to oral healthcare for vulnerable and underserved populations: Adopted by the General Assembly: September 2019, San Francisco, United States of America. Int. Dent. J. 2020, 70, 15–16. [Google Scholar] [CrossRef]
- Waisel, D.B. Vulnerable populations in healthcare. Curr. Opin. Anaesthesiol. 2013, 26, 186–192. [Google Scholar] [CrossRef]
- Elaine Muirhead, V.; Milner, A.; Freeman, R.; Doughty, J.; Macdonald, M.E. What is intersectionality and why is it important in oral health research? Community Dent. Oral Epidemiol. 2020, 48, 464–470. [Google Scholar] [CrossRef]
- Kapilashrami, A.; Hankivsky, O. Intersectionality and why it matters to global health. Lancet 2018, 391, 2589–2591. [Google Scholar] [CrossRef] [PubMed]
- Gilbody, S.; Peckham, E.; Bailey, D.; Arundel, C.; Heron, P.; Crosland, S.; Fairhurst, C.; Hewitt, C.; Li, J.; Members of the SCIMITAR+ Collaborative. Smoking cessation in severe mental illness: Combined long-term quit rates from the UK SCIMITAR trials programme. Br. J. Psychiatry 2021, 218, 95–97. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Khalid, T.; Awan, K.H. Chronic periodontitis and smoking. Prevalence and dose-response relationship. Saudi Med. J. 2016, 37, 889–894. [Google Scholar] [CrossRef] [PubMed]
- Jang, A.Y.; Lee, J.K.; Shin, J.Y.; Lee, H.Y. Association between Smoking and Periodontal Disease in Korean Adults: The Fifth Korea National Health and Nutrition Examination Survey (2010 and 2012). Korean J. Fam. Med. 2016, 37, 117–122. [Google Scholar] [CrossRef]
- Exercise benefits dental health. Br. Dent. J. 2005, 199, 629. [CrossRef]
- Sanchez, G.F.L.; Smith, L.; Koyanagi, A.; Grabovac, I.; Yang, L.; Veronese, N.; Shin, J.I.; Loosemore, M.; Jacob, L. Associations between self-reported physical activity and oral health: A cross-sectional analysis in 17,777 Spanish adults. Br. Dent. J. 2020, 228, 361–365. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, J.I.; Muikku, T.; Simila, T.; Cinar, A.B.; Pohjola, V. Physical activity, BMI and oral health behaviour among adolescents: Finnish School Health Promotion Study. Eur. J. Public Health 2019, 29, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.Y.; Chen, P.C.; Kuo, H.K.; Lin, L.Y.; Lin, J.W.; Hwang, J.J. Effects of obesity, physical activity, and cardiorespiratory fitness on blood pressure, inflammation, and insulin resistance in the National Health and Nutrition Survey 1999–2002. Nutr. Metab. Cardiovasc. Dis. 2010, 20, 713–719. [Google Scholar] [CrossRef] [PubMed]
- Cepeda, M.S.; Weinstein, R.; Blacketer, C.; Lynch, M.C. Association of flossing/inter-dental cleaning and periodontitis in adults. J. Clin. Periodontol. 2017, 44, 866–871. [Google Scholar] [CrossRef] [PubMed]
- Sambunjak, D.; Nickerson, J.W.; Poklepovic, T.; Johnson, T.M.; Imai, P.; Tugwell, P.; Worthington, H.V. Flossing for the management of periodontal diseases and dental caries in adults. Cochrane Database Syst. Rev. 2011, 12, CD008829. [Google Scholar] [CrossRef]
- Rohani, B. Oral manifestations in patients with diabetes mellitus. World J. Diabetes 2019, 10, 485–489. [Google Scholar] [CrossRef]
- Kinane, D.F.; Chestnutt, I.G. Relationship of diabetes to periodontitis. Curr. Opin. Periodontol. 1997, 4, 29–34. [Google Scholar] [PubMed]
- Preshaw, P.M.; Alba, A.L.; Herrera, D.; Jepsen, S.; Konstantinidis, A.; Makrilakis, K.; Taylor, R. Periodontitis and diabetes: A two-way relationship. Diabetologia 2012, 55, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Davis, K.A.S.; Cullen, B.; Adams, M.; Brailean, A.; Breen, G.; Coleman, J.R.I.; Dregan, A.; Gaspar, H.A.; Hübel, C.; Lee, W.; et al. Indicators of mental disorders in UK Biobank-A comparison of approaches. Int. J. Methods Psychiatr. Res. 2019, 28, e1796. [Google Scholar] [CrossRef] [PubMed]
- Laverty, L.; Harris, R. Can conditional health policies be justified? A policy analysis of the new NHS dental contract reforms. Soc. Sci. Med. 2018, 207, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Adams, C.E.; Wells, N.C.; Clifton, A.; Jones, H.; Simpson, J.; Tosh, G.; Callaghan, P.; Liddle, P.; Guo, B.; Furtado, V.; et al. Monitoring oral health of people in Early Intervention for Psychosis (EIP) teams: The extended Three Shires randomised trial. Int. J. Nurs. Stud. 2018, 77, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Kuo, M.W.; Yeh, S.H.; Chang, H.M.; Teng, P.R. Effectiveness of oral health promotion program for persons with severe mental illness: A cluster randomized controlled study. BMC Oral Health 2020, 20, 290. [Google Scholar] [CrossRef] [PubMed]
- Grossi, S.G.; Zambon, J.J.; Ho, A.W.; Koch, G.; Dunford, R.G.; Machtei, E.E.; Norderyd, O.M.; Genco, R.J. Assessment of risk for periodontal disease. I. Risk indicators for attachment loss. J. Periodontol. 1994, 65, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Persson, G.R.; Persson, R.E.; Hollender, L.G.; Kiyak, H.A. The impact of ethnicity, gender, and marital status on periodontal and systemic health of older subjects in the Trials to Enhance Elders’ Teeth and Oral Health (TEETH). J. Periodontol. 2004, 75, 817–823. [Google Scholar] [CrossRef]
- Weatherspoon, D.J.; Borrell, L.N.; Johnson, C.W.; Mujahid, M.S.; Neighbors, H.W.; Adar, S.D. Racial and Ethnic Differences in Self-Reported Periodontal Disease in the Multi-Ethnic Study of Atherosclerosis (MESA). Oral Health Prev. Dent. 2016, 14, 249–257. [Google Scholar]
- Paulander, J.; Axelsson, P.; Lindhe, J. Association between level of education and oral health status in 35-, 50-, 65- and 75-year-olds. J. Clin. Periodontol. 2003, 30, 697–704. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Dental Research (U.S.), Epidemiology and Oral Disease Prevention Program. Oral Health of United States Adults: The National Survey of Oral Health in U.S. Employed Adults and Seniors, 1985–1986: National Findings; University of Michigan Library: Ann Arbor, MI, USA, 1987. [Google Scholar]
- Martinez-Herrera, M.; Silvestre-Rangil, J.; Silvestre, F.J. Association between obesity and periodontal disease. A systematic review of epidemiological studies and controlled clinical trials. Med. Oral Patol. Oral Cir. Bucal. 2017, 22, e708–e715. [Google Scholar] [CrossRef] [PubMed]
- Albandar, J.M.; Streckfus, C.F.; Adesanya, M.R.; Winn, D.M. Cigar, pipe, and cigarette smoking as risk factors for periodontal disease and tooth loss. J. Periodontol. 2000, 71, 1874–1881. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, S. Alcohol consumption a risk factor for periodontal disease. Evid. Based Dent. 2011, 12, 76. [Google Scholar] [CrossRef] [PubMed]
- Arora, G.F.R. Oral Health and Addiction: Consequences of Substance Use. In Textbook of Addiction Treatment; Springer: Berlin, Germany, 2021. [Google Scholar]
- Moynihan, P.J. The relationship between diet, nutrition and dental health: An overview and update for the 90s. Nutr. Res. Rev. 1995, 8, 193–224. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; Del Castillo, A.M.; Jepsen, S.; Gonzalez-Juanatey, J.R.; D’Aiuto, F.; Bouchard, P.; Chapple, I.; Dietrich, T.; Gotsman, I.; Graziani, F.; et al. Periodontitis and Cardiovascular Diseases. Consensus Report. J. Clin. Periodontol. 2020, 47, 268–288. [Google Scholar] [CrossRef] [PubMed]
- Thomson, W.M.; Williams, S.M.; Broadbent, J.M.; Poulton, R.; Locker, D. Long-term dental visiting patterns and adult oral health. J. Dent. Res. 2010, 89, 307–311. [Google Scholar] [CrossRef]
- Kumar, S.; Tadakamadla, J.; Johnson, N.W. Effect of Toothbrushing Frequency on Incidence and Increment of Dental Caries: A Systematic Review and Meta-Analysis. J. Dent. Res. 2016, 95, 1230–1236. [Google Scholar] [CrossRef]
| Characteristic | Total | Without SMI | With SMI | p-Value |
|---|---|---|---|---|
| n | 53,348 | 52,630 | 718 | |
| Age in years, mean (SD) | 47.5 (19.6) | 47.4 (19.6) | 51.1 (16.8) | <0.001 |
| Men | 25,709 (48.2) | 25,378 (48.2) | 331 (46.1) | 0.275 |
| Ethnicity, white | 23,388 (43.8) | 23,013 (43.7) | 375 (52.2) | <0.001 |
| Education, college or above | 23,974 (48.5) | 23,691 (48.6) | 283 (41.3) | <0.001 |
| Marital status, not married | 25,418 (49.6) | 24,923 (49.3) | 495 (70.6) | <0.001 |
| Ratio of family income to poverty, mean (SD) | 2.5 (1.6) | 2.5 (1.6) | 1.8 (1.4) | <0.001 |
| BMI (kg/m2), mean (SD) | 28.6 (6.8) | 28.6 (6.7) | 30.5 (7.6) | <0.001 |
| Waist circumference a | <0.001 | |||
| Low | 13,215 (27.5) | 13,112 (27.7) | 103 (17.3) | |
| High | 9291 (19.4) | 9204 (19.4) | 87 (14.6) | |
| Very high | 25,473 (53.1) | 25,066 (52.9) | 407 (68.2) | |
| Had at least 12 alcohol drink in one year | 30,261 (69.4) | 29,865 (69.4) | 396 (67.9) | 0.454 |
| Smoking status | <0.001 | |||
| Non-smoker | 30,575 (57.3) | 30,305 (57.6) | 270 (37.6) | |
| Ex-smoker | 12,278 (23.0) | 12,105 (23.0) | 173 (24.1) | |
| Current smoker | 10,495 (19.7) | 10,220 (19.4) | 275 (38.3) | |
| Cig number in past 30 days, mean (SD) | 12.6 (10.6) | 12.5 (10.5) | 16.4 (12.8) | <0.001 |
| Substance Misuse (cocain/herion) | 5766 (17.6) | 5602 (17.4) | 164 (35.7) | <0.001 |
| Had moderate Physical activity over past 30 days | 22,558 (43.0) | 22,353 (43.2) | 205 (30.1) | <0.001 |
| Sugar intake (g), mean (SD) | 115.0 (69.7) | 114.7 (69.4) | 137.6 (87.1) | <0.001 |
| Carbohydrate intake (g), mean (SD) | 255.1 (115.5) | 254.9 (115.4) | 273.8 (124.1) | <0.001 |
| Energy intake (KCAL), mean (SD) | 2060.7 (883.4) | 2059.8 (883.2) | 2132.0 (890.4) | 0.060 |
| Diabetes | 5821 (11.1) | 5695 (11.0) | 126 (18.2) | <0.001 |
| Cardiovascular disease b | 4869 (9.1) | 4749 (9.0) | 120 (16.7) | <0.001 |
| Oral Characteristic | Total | Without SMI | With SMI | p-Value |
|---|---|---|---|---|
| n | 53,348 | 52,630 | 718 | |
| Oral hygiene behaviour | ||||
| Last dental visit | 0.250 | |||
| Less than a year | 15,736 (54.1) | 15,536 (54.1) | 200 (54.2) | |
| Over 1 year | 12,648 (43.5) | 12,483 (43.5) | 165 (44.7) | |
| Never | 693 (2.4) | 689 (2.4) | 4 (1.1) | |
| Toothbrush, twice or more | 457 (76.2) | 454 (76.4) | 3 (50.0) | 0.303 |
| Use dental floss in the past 7 days | <0.001 | |||
| No | 6866 (36.3) | 6666 (35.9) | 200 (58.0) | |
| Not everyday | 6107 (32.3) | 6026 (32.4) | 81 (23.5) | |
| Everyday | 5953 (31.5) | 5889 (31.7) | 64 (18.6) | |
| Oral health status | ||||
| Self-rated oral health | <0.001 | |||
| Excellent or very good | 13,255 (28.9) | 13,121 (29.0) | 134 (21.0) | |
| Good | 16,348 (35.6) | 16,160 (35.7) | 188 (29.5) | |
| Fair | 10,665 (23.2) | 10,497 (23.2) | 168 (26.4) | |
| Poor | 5665 (12.3) | 5518 (12.2) | 147 (23.1) | |
| Ache in mouth | <0.001 | |||
| Very often | 900 (3.5) | 863 (3.4) | 37 (8.8) | |
| Fairly often | 1118 (4.3) | 1081 (4.2) | 37 (8.8) | |
| Occasionally | 3971 (15.3) | 3901 (15.3) | 70 (16.6) | |
| Hardly ever | 5617 (21.7) | 5535 (21.7) | 82 (19.4) | |
| Never | 14,291 (55.2) | 14,095 (55.3) | 196 (46.4) | |
| Tooth loss | <0.001 | |||
| No loss | 28,522 (53.5) | 28,247 (53.7) | 275 (38.3) | |
| 1–10 | 12,854 (24.1) | 12,661 (24.1) | 193 (26.9) | |
| 11–20 | 5319 (10.0) | 5238 (10.0) | 81 (11.3) | |
| 21–31 | 3020 (5.7) | 2955 (5.6) | 65 (9.1) | |
| Edentulus | 3633 (6.8) | 3529 (6.7) | 104 (14.5) | |
| DMFT, median [IQR] | 1.0 [0.0, 11.0] | 1.0 [0.0, 11.0] | 1.5 [0.0, 16.0] | 0.001 |
| DT, median [IQR] | 0.0 [0.0, 5.0] | 0.0 [0.0, 5.0] | 0.0 [0.0, 3.8] | 0.005 |
| MT, median [IQR] | 0.0 [0.0, 2.0] | 0.0 [0.0, 2.0] | 0.0 [0.0, 5.0] | <0.001 |
| Periodontal diseases | 0.093 | |||
| None | 12,487 (53.5) | 12,342 (53.5) | 145 (50.9) | |
| Mild | 1913 (8.2) | 1891 (8.2) | 22 (7.7) | |
| Moderate | 4486 (19.2) | 4415 (19.1) | 71 (24.9) | |
| Severe | 4476 (19.2) | 4429 (19.2) | 47 (16.5) |
| Ordinal Oral Health Outcomes (OR, 95% CI) a | Numeric Oral Health Outcomes (95% CI) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| DMFT | DT | MT | ||||||||
| Models | Self-Rated Oral Health d | Ache in Mouth e | Tooth Loss f | Periodontal Disease Severity g | Zero-Inflated Model, OR | Count Model, RR | Zero-Inflated Model, OR | Count Model, RR | Zero-Inflated Model, OR | Count Model, RR |
| Sample size n | 2514 | 1533 | 2872 | 1302 | 2872 | 2872 | 2872 | |||
| Unadjusted | 1.84 *** (1.58–2.16) | 1.75 *** (1.43–2.15) | 1.93 *** (1.69–2.21) | 1.11 (0.89–1.39) | 0.89 (0.70–1.13) | 1.28 *** (1.18–1.38) | 1.45 *** (1.17–1.78) | 1.02 (0.93–1.12) | 0.49 *** (0.33–0.71) | 1.37 *** (1.17–1.60) |
| Adjusted for b,c | ||||||||||
| +demographics | 1.61 *** (1.37–1.90) | 1.53 *** (1.24–1.88) | 1.69 *** (1.46–1.94) | 1.02 (0.81–1.29) | 0.97 (0.77–1.23) | 1.22 *** (1.15–1.29) | 1.27 * (1.03–1.56) | 1.05 (0.96–1.14) | 0.64 (0.38–1.05) | 1.41 *** (1.23–1.62) |
| +lifestyles | 1.19 (0.97–1.47) | 1.46 ** (1.14–1.87) | 1.66 *** (1.39–1.99) | 0.77 (0.59–1.01) | 1.08 (0.74–1.58) | 1.16 *** (1.08–1.26) | 1.60 *** (1.19–2.15) | 1.02 (0.93–1.13) | 0.99 (0.59–1.67) | 1.39 *** (1.18–1.64) |
| +comorbidities | 1.18 (0.96–1.45) | 1.43 ** (1.12–1.83) | 1.63 *** (1.36–1.95) | 0.77 (0.58–1.01) | 1.09 (0.74–1.60) | 1.16 ** (1.07–1.25) | 1.57 ** (1.17–2.11) | 1.03 (0.93–1.13) | 1.01 (0.60–1.71) | 1.37 ** (1.16–1.61) |
| +oral hygiene behaviour | 1.19 (0.97–1.47) | 1.42 ** (1.11–1.82) | 1.60 *** (1.34–1.92) | 0.76 (0.58–1.01) | 1.10 (0.75–1.61) | 1.14 * (1.05–1.23) | 1.54 (1.14–2.07) | 1.02 (0.92–1.12) | 0.99 (0.59–1.65) | 1.30 ** (1.10–1.52) |
| Ordinal Oral Health Outcomes, OR (95% CI) | Numeric Oral Health Outcomes, OR and RR (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|
| Self-Rated Oral Health | Ache in Mouth | Tooth Loss Number (Grouped) | Periodontal Disease Severity | DMFT | MT | |||
| OR (95% CI) | RR (95% CI) | OR (95% CI) | RR (95% CI) | |||||
| n | 637 | 422 | 718 | 285 | 718 | 718 | ||
| Demographics | ||||||||
| Age | 1.01 (0.99–1.03) | 1.00 (0.97–1.03) | 1.08 *** (1.06–1.09) | 1.09 *** (1.05–1.13) | 0.95 * (0.91–0.98) | 1.03 *** (1.02–1.04) | 0.96 *** (0.94–0.98) | 1.04 *** (1.03–1.06) |
| Ethnicity, white | 1.13 (0.74–1.73) | 1.35 (0.79–2.30) | 1.38 (0.96–1.98) | 0.61 (0.32–1.17) | 1.17 (0.49–2.78) | 1.20 ** (1.03–1.40) | 1.76 ** (1.09–2.77) | 1.57 ** (1.15–2.16) |
| Ratio of family income to poverty | 0.84 * (0.72–0.98) | 0.74 ** (0.59–0.92) | 0.76 *** (0.65–0.88) | 0.70 * (0.53–0.94) | 1.22 (0.88–1.68) | 0.91 * (0.86–0.97) | 1.31 * (1.08–1.58) | 0.82 (0.72–0.93) |
| Lifestyles | ||||||||
| Smoking status, ever smoker | 1.37 (0.85–2.21) | 0.68 (0.38–1.22) | 2.70 *** (1.76–4.13) | 1.31 (0.61–2.82) | 0.50 (0.20–1.25) | 1.25 * (1.05–1.49) | 0.72 (0.42–1.24) | 1.79 ** (1.24–2.58) |
| Physical activity, yes | 0.51 ** (0.31–0.82) | 1.33 (0.74–2.38) | 0.60 * (0.39–0.94) | 0.79 (0.35–1.77) | 1.02 (0.40–2.59) | 0.99 (0.82–1.18) | 0.85 (0.51–1.43) | 0.93 (0.66–1.33) |
| Comorbidities | ||||||||
| Diabetes, yes | 1.69 (0.90–3.17) | 1.12 (0.55–2.28) | 1.86 * (1.07–3.26) | 1.42 (0.57–3.49) | 1.85 (0.57–5.98) | 1.15 (0.93–1.44) | 0.79 (0.41–1.51) | 1.52 * (1.03–2.24) |
| Dental hygiene behaviour | ||||||||
| Use dental floss in the past 7 days | ||||||||
| No (ref) | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Everyday | 0.82 (0.39–1.72) | 0.71 (0.31–1.63) | 0.51 * (0.28–0.91) | 2.26 (0.86–5.95) | 0.49 (0.03–7.47) | 0.67 * (0.50–0.89) | 0.95 (0.37–2.43) | 0.52 ** (0.34–0.79) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, J.; Wu, J.; Aggarwal, V.R.; Shiers, D.; Doran, T.; Palmier-Claus, J. Investigating the Relationship between Oral Health and Severe Mental Illness: Analysis of NHANES 1999–2016. Dent. J. 2024, 12, 191. https://doi.org/10.3390/dj12070191
Kang J, Wu J, Aggarwal VR, Shiers D, Doran T, Palmier-Claus J. Investigating the Relationship between Oral Health and Severe Mental Illness: Analysis of NHANES 1999–2016. Dentistry Journal. 2024; 12(7):191. https://doi.org/10.3390/dj12070191
Chicago/Turabian StyleKang, Jing, Jianhua Wu, Vishal. R. Aggarwal, David Shiers, Tim Doran, and Jasper Palmier-Claus. 2024. "Investigating the Relationship between Oral Health and Severe Mental Illness: Analysis of NHANES 1999–2016" Dentistry Journal 12, no. 7: 191. https://doi.org/10.3390/dj12070191
APA StyleKang, J., Wu, J., Aggarwal, V. R., Shiers, D., Doran, T., & Palmier-Claus, J. (2024). Investigating the Relationship between Oral Health and Severe Mental Illness: Analysis of NHANES 1999–2016. Dentistry Journal, 12(7), 191. https://doi.org/10.3390/dj12070191








