Can a Novel Device with Pure Dry Air Increase the Shear Bond Strength of Dental Composites to Dentin? An Experimental Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Specimen Fabrication
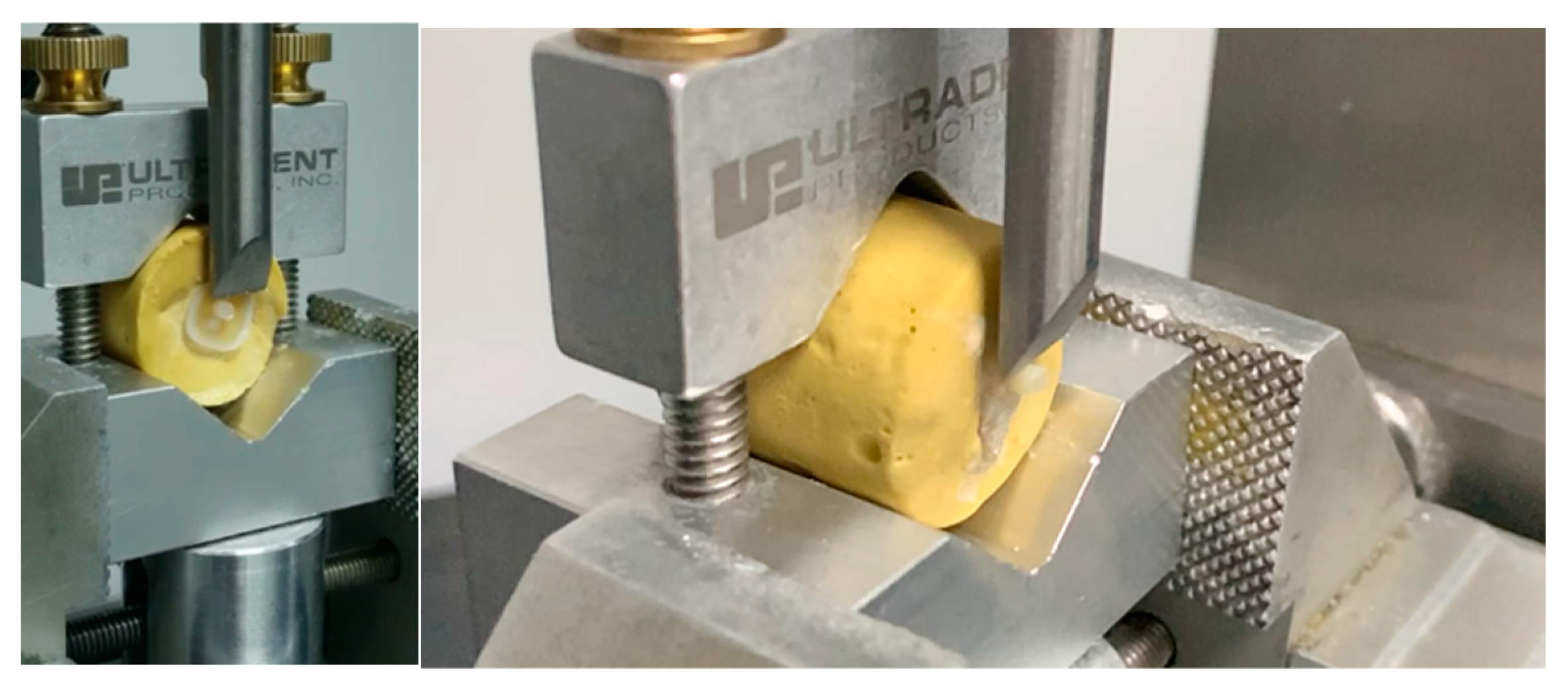
2.2. Bond Strength Test
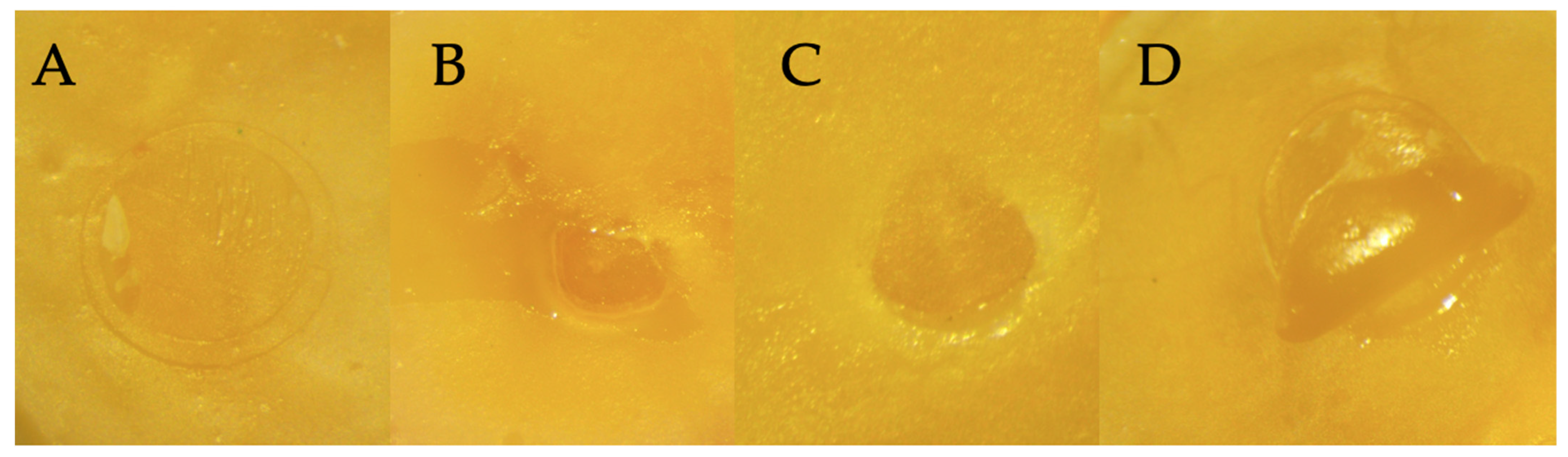
2.3. Failure Mode Analysis
2.4. Statistical Analyses
3. Results
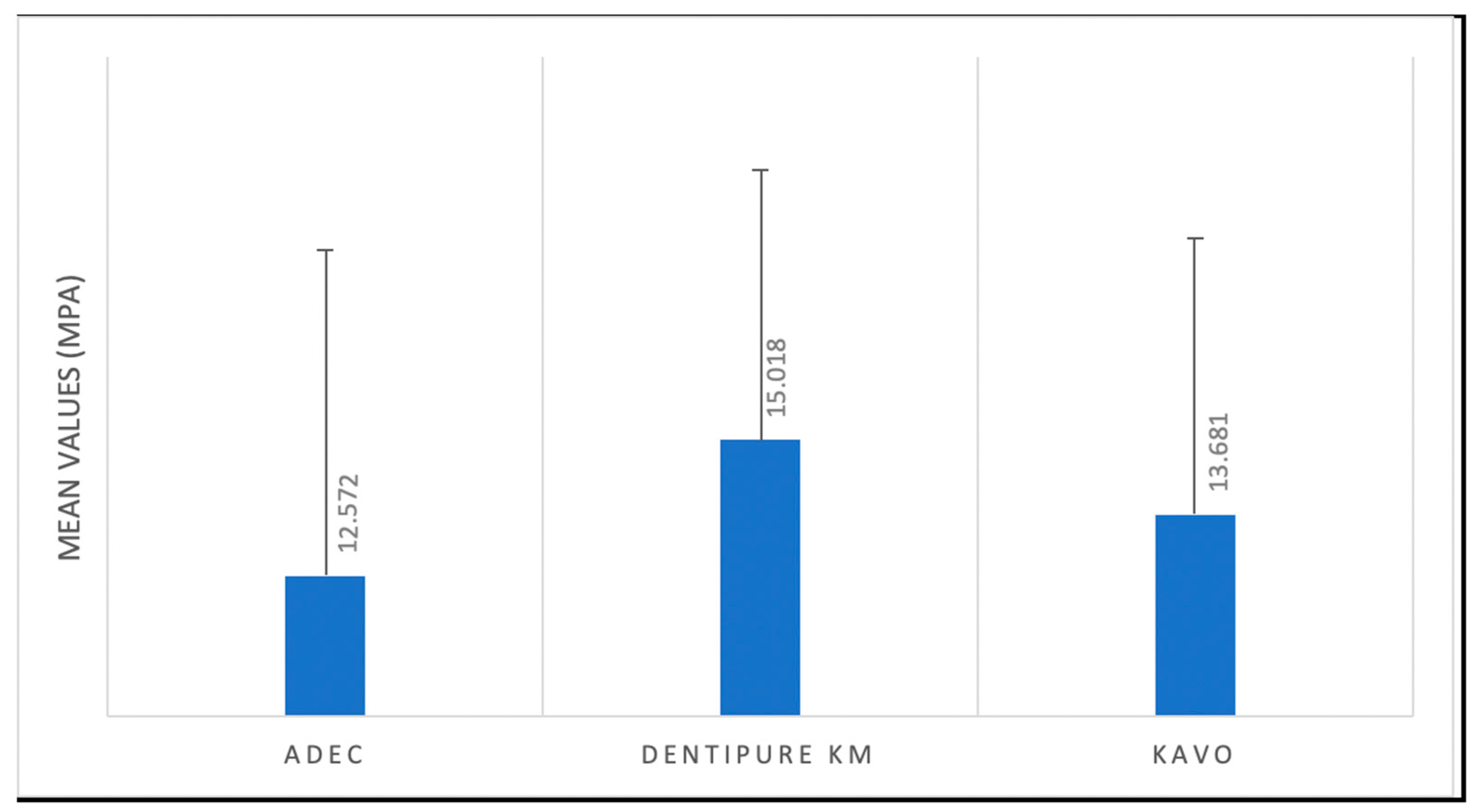
3.1. Bond Strength Test
3.2. Failure Mode Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Masarwa, N.; Mohamed, A.; Abou-Rabii, I.; Abu Zaghlan, R.; Steier, L. Longevity of Self-etch Dentin Bonding Adhesives Compared to Etch-and-rinse Dentin Bonding Adhesives: A Systematic Review. J. Evid. Based. Dent. Pract. 2016, 16, 96–106. [Google Scholar] [CrossRef]
- Geng Vivanco, R.; Cardoso, R.S.; Sousa, A.B.S.; Chinelatti, M.A.; Vincenti, S.A.F.; Tonani-Torrieri, R.; Pires-de-Souza, F.C.P. Effect of thermo-mechanical cycling and chlorhexidine on the bond strength of universal adhesive system to dentin. Heliyon 2020, 6, e03871. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; Yoshihara, K.; Yoshida, Y.; Mine, A.; De Munck, J.; Van Landuyt, K.L. State of the art of self-etch adhesives. Dent. Mater. 2011, 27, 17–28. [Google Scholar] [CrossRef]
- Papadogiannis, D.; Dimitriadi, M.; Zafiropoulou, M.; Gaintantzopoulou, M.D.; Eliades, G. Universal Adhesives: Setting Characteristics and Reactivity with Dentin. Materials 2019, 12, 1720. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; Yoshihara, K.; Van Landuyt, K.; Yoshida, Y.; Peumans, M. From Buonocore’s Pioneering Acid-Etch Technique to Self-Adhering Restoratives. A Status Perspective of Rapidly Advancing Dental Adhesive Technology. J. Adhes. Dent. 2020, 22, 7–34. [Google Scholar] [PubMed]
- Tay, F.R.; Gwinnett, A.J.; Pang, K.M.; Wei, S.H. Variability in microleakage observed in a total-etch wet-bonding technique under different handling conditions. J. Dent. Res. 1995, 74, 1168–1178. [Google Scholar] [CrossRef] [PubMed]
- Nunes, T.G.; Garcia, F.C.; Osorio, R.; Carvalho, R.; Toledano, M. Polymerization efficacy of simplified adhesive systems studied by NMR and MRI techniques. Dent. Mater. 2006, 22, 963–972. [Google Scholar] [CrossRef]
- de Carvalho Cardoso, P.; Loguercio, A.D.; Vieira, L.C.C.; Baratieri LN, B.; Reis, A. Effect of prolonged application times on resin-dentin bond strengths. J. Adhes. Dent. 2005, 7, 143–149. [Google Scholar]
- Luque-Martinez, I.V.; Perdigão, J.; Muñoz, M.A.; Sezinando, A.; Reis, A.; Loguercio, A.D. Effects of solvent evaporation time on immediate adhesive properties of universal adhesives to dentin. Dent. Mater. 2014, 30, 1126–1135. [Google Scholar] [CrossRef] [PubMed]
- Bourgi, R.; Hardan, L.; Rivera-Gonzaga, A.; Cuevas-Suárez, C.E. Effect of Warm-Air Stream for Solvent Evaporation on Bond Strength of Adhesive Systems: A Systematic Review and Meta-Analysis of in Vitro Studies. Int. J. Adhes. Adhes. 2021, 105, 102794. [Google Scholar] [CrossRef]
- Rodríguez, E.; Vicente, M.A. A copper-sulfate-based inorganic chemistry laboratory for first-year university students that teaches basic operations and concepts. J. Chem. Educ. 2002, 79, 486. [Google Scholar] [CrossRef]
- Saraiva, L.O.; Aguiar, T.R.; Costa, L.; Cavalcanti, A.N.; Giannini, M.; Mathias, P. Influence of intraoral temperature and relative humidity on the dentin bond strength: An in situ study. J. Esthet. Restor. Dent. 2015, 27, 2–9. [Google Scholar] [CrossRef]
- Shalini, S.; Jha, A.; Kashyap, P.; Gupta, P.; Rajbhoj, S.; Bhandari, S. A Comparison of the Shear Bond Strength of Orthodontic Brackets Bonded with Different Orthodontic Adhesives. Cureus 2023, 15, 5. [Google Scholar] [CrossRef]
- ISO/TS 11405:2015; Dentistry-Testing of Adhesion to Tooth Structure. International Organizazion for Standardization: Geneva, Switzerland, 2015.
- Edelhoff, D.; Güth, J.F.; Erdelt, K.; Brix, O.; Liebermann, A. Clinical performance of occlusal onlays made of lithium disilicate ceramic in patients with severe tooth wear up to 11 years. Dent. Mater. 2019, 35, 1319–1330. [Google Scholar] [CrossRef] [PubMed]
- Emam, Z.N.; A Aleem, N.A. Influence of different materials and preparation designs on marginal adaptation and fracture resistance of CAD/CAM fabricated occlusal veneers. Egypt. Dent. J. 2020, 66, 439–452. [Google Scholar] [CrossRef]
- Dabbagh, S.; Hardan, L.; Kassis, C.; Bourgi, R.; Devoto, W.; Zarow, M.; Jakubowicz, N.; Ghaleb, M.; Kharouf, N.; Dabbagh, M.; et al. Effect of intraoral humidity on dentin bond strength of two universal adhesives: An in vitro preliminary study. Coatings 2022, 12, 712. [Google Scholar] [CrossRef]
- Erickson, R.L.; Barkmeier, W.W.; Kimmes, N.S. Fatigue of enamel bonds with self-etch adhesives. Dent. Mater. 2009, 25, 716–720. [Google Scholar] [CrossRef]
- Erickson, R.L.; Barkmeier, W.W.; Latta, M.A. The role of etching in bonding to enamel: A comparison of self-etching and etch-and-rinse adhesive systems. Dent. Mater. 2009, 25, 1459–1467. [Google Scholar] [CrossRef]
- Marchesi, G.; Frassetto, A.; Visintini, E.; Diolosà, M.; Turco, G.; Salgarello, S.; Di Lenarda, R.; Cadenaro, M.; Breschi, L. Influence of ageing on self-etch adhesives: One-step vs. two-step systems. Eur. J. Oral Sci. 2013, 121, 43–49. [Google Scholar] [CrossRef]
- Takamizawa, T.; Barkmeier, W.W.; Tsujimoto, A.; Scheidel, D.D.; Erickson, R.L.; Latta, M.A.; Miyazaki, M. Effect of Phosphoric Acid Pre-etching on Fatigue Limits of Self-etching Adhesives. Oper. Dent. 2015, 40, 379–395. [Google Scholar] [CrossRef] [PubMed]
- Tay, F.R.; Pashley, D.H.; Suh, B.I.; Carvalho, R.M.; Itthagarun, A. Single-step adhesives are permeable membranes. J. Dent. 2002, 30, 371–382. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, M.; Nakajima, M.; Hosaka, K.; Ikeda, M.; Foxton, R.M.; Tagami, J. Long-term evaluation of water sorption and ultimate tensile strength of HEMA-containing/-free one-step self-etch adhesives. J. Dent. 2011, 39, 506–512. [Google Scholar] [CrossRef] [PubMed]
- Van Landuyt, K.L.; Peumans, M.; De Munck, J.; Lambrechts, P.; Van Meerbeek, B. Extension of a one-step self-etch adhesive into a multi-step adhesive. Dent. Mater. 2006, 22, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Yamada, M.; Miyazaki, M.; Moore, B.K. Influence of interchanging adhesive resins and self-etching primers on the mechanical properties of adhesive resins. Oper. Dent. 2004, 29, 532–537. [Google Scholar] [PubMed]
- Tay, F.R.; Pashley, D.H.; Suh, B.; Carvalho, R.; Miller, M. Single-step, self-etch adhesives behave as permeable membranes after polymerization. Part I. Bond strength and morphologic evidence. Am. J. Dent. 2004, 17, 271–278. [Google Scholar]
- Chiba, Y.; Yamaguchi, K.; Miyazaki, M.; Tsubota, K.; Takamizawa, T.; Moore, B.K. Effect of air-drying time of single-application self-etch adhesives on dentin bond strength. Oper. Dent. 2006, 31, 233–239. [Google Scholar] [CrossRef]
- Ogura, Y.; Shimizu, Y.; Shiratsuchi, K.; Tsujimoto, A.; Takamizawa, T.; Ando, S.; Miyazaki, M. Effect of warm air-drying on dentin bond strength of single-step self-etch adhesives. Dent. Mater. J. 2012, 31, 507–513. [Google Scholar] [CrossRef]
- Shiratsuchi, K.; Tsujimoto, A.; Takamizawa, T.; Furuichi, T.; Tsubota, K.; Kurokawa, H.; Miyazaki, M. Influence of warm air-drying on enamel bond strength and surface free-energy of self-etch adhesives. Eur. J. Oral Sci. 2013, 121, 370–376. [Google Scholar] [CrossRef]
- Muñoz, M.A.; Sezinando, A.; Luque-Martinez, I.; Szesz, A.L.; Reis, A.; Loguercio, A.D.; Bombarda, N.H.; Perdigão, J. Influence of a hydrophobic resin coating on the bonding efficacy of three universal adhesives. J. Dent. 2014, 42, 595–602. [Google Scholar] [CrossRef]
- Perdigão, J.; Muñoz, M.A.; Sezinando, A.; Luque-Martinez, I.V.; Staichak, R.; Reis, A.; Loguercio, A.D. Immediate adhesive properties to dentin and enamel of a universal adhesive associated with a hydrophobic resin coat. Oper. Dent. 2014, 39, 489–499. [Google Scholar] [CrossRef][Green Version]
- Fujiwara, S.; Takamizawa, T.; Barkmeier, W.W.; Tsujimoto, A.; Imai, A.; Watanabe, H.; Erickson, R.L.; Latta, M.A.; Nakatsuka, T.; Miyazaki, M. Effect of double-layer application on bond quality of adhesive systems. J. Mech. Behav. Biomed. Mater. 2018, 77, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Reis, A.; Albuquerque, M.; Pegoraro, M.; Mattei, G.; Bauer, J.R.; Grande, R.H.; Klein-Junior, C.A.; Baumhardt-Neto, R.; Loguercio, A.D. Can the durability of one-step self-etch adhesives be improved by double application or by an extra layer of hydrophobic resin? J. Dent. 2008, 36, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Sezinando, A.; Luque-Martinez, I.; Muñoz, M.A.; Reis, A.; Loguercio, A.D.; Perdigão, J. Influence of a hydrophobic resin coating on the immediate and 6-month dentin bonding of three universal adhesives. Dent. Mater. 2015, 31, 236–246. [Google Scholar] [CrossRef]
- Cardenas, A.M.; Siqueira, F.; Rocha, J.; Szesz, A.L.; Anwar, M.; El-Askary, F.; Reis, A.; Loguercio, A. Influence of Conditioning Time of Universal Adhesives on Adhesive Properties and Enamel-Etching Pattern. Oper. Dent. 2016, 41, 481–490. [Google Scholar] [CrossRef] [PubMed]
- Ito, S.; Tay, F.R.; Hashimoto, M.; Yoshiyama, M.; Saito, T.; Brackett, W.W.; Waller, J.L.; Pashley, D.H. Effects of multiple coatings of two all-in-one adhesives on dentin bonding. J. Adhes. Dent. 2005, 7, 133–141. [Google Scholar] [PubMed]
- Loguercio, A.D.; Muñoz, M.A.; Luque-Martinez, I.; Hass, V.; Reis, A.; Perdigão, J. Does active application of universal adhesives to enamel in self-etch mode improve their performance? J. Dent. 2015, 43, 1060–1070. [Google Scholar] [CrossRef]
- Takahashi, R.; Nikaido, T.; Ariyoshi, M.; Kitayama, S.; Sadr, A.; Foxton, R.M.; Tagami, J. Thin resin coating by dual-application of all-in-one adhesives improves dentin bond strength of resin cements for indirect restorations. Dent. Mater. J. 2010, 29, 615–622. [Google Scholar] [CrossRef] [PubMed]
- Sherlin, H.J.; Jayaraj, G.; Don, K.R.; Santhanam, A. Efficacy of Anhydrous Copper Sulfate as a Solid Dehydrant in Tissue Processing Procedure. J. Evol. Med. Dent. Sci. 2020, 9, 3004–3009. [Google Scholar]
- Juneja, R.; Duhan, J.; Tewari, S.; Sangwan, P.; Bhatnagar, N. Effect of blood contamination and decontamination protocols on acetone-based and ethanol-based total etch adhesive systems. J. Esthet. Restor. Dent. 2014, 26, 403–416. [Google Scholar] [CrossRef]
- Bourgi, R.; Cuevas-Suarez, C.E.; Devoto, W.; Monjarás-Ávila, A.J.; Monteiro, P.; Kharma, K.; Lukomska-Szymanska, M.; Hardan, L. Effect of contamination and decontamination methods on the bond strength of adhesive systems to dentin: A systematic review. J. Esthet. Rest. Dent. 2023, 35, 1218–1238. [Google Scholar] [CrossRef]
- Santschi, K.; Peutzfeldt, A.; Lussi, A.; Flury, S. Effect of salivary contamination and decontamination on bond strength of two one-step self-etching adhesives to dentin of primary and permanent teeth. J. Adhes. Dent. 2015, 17, 51–57. [Google Scholar] [PubMed]
- Jacquot, B.; Durand, J.C.; Farge, P.; Valcarcel, J.; Deville de Périère, D.; Cuisinier, F. Influence of temperature and relative humidity on dentin and enamel bonding: A critical review of the literature. Part 1. Laboratory studies. J. Adhes. Dent. 2012, 14, 433–446. [Google Scholar] [PubMed]
- Amsler, F.; Peutzfeldt, A.; Lussi, A.; Flury, S. Bond Strength of Resin Composite to Dentin with Different Adhesive Systems: Influence of Relative Humidity and Application Time. J. Adhes. Dent. 2015, 17, 249–256. [Google Scholar] [PubMed]
- Chiba, Y.; Miyazaki, M.; Rikuta, A.; Moore, B.K. Influence of environmental conditions on dentin bond strengths of one-application adhesive systems. Oper. Dent. 2004, 29, 554–559. [Google Scholar] [PubMed]
- Tay, F.R.; Sano, H.; Carvalho, R.; Pashley, E.L.; Pashley, D.H. An ultrastructural study of the influence of acidity of self-etching primers and smear layer thickness on bonding to intact dentin. J. Adhes. Dent. 2000, 2, 83–98. [Google Scholar]
- Sabatini, C. Effect of phosphoric acid etching on the shear bond strength of two self-etch adhesives. J. Appl. Oral Sci. 2013, 21, 56–62. [Google Scholar] [CrossRef][Green Version]
- Taschner, M.; Nato, F.; Mazzoni, A.; Frankenberger, R.; Krämer, N.; Di Lenarda, R.; Petschelt, A.; Breschi, L. Role of preliminary etching for one-step self-etch adhesives. Eur. J. Oral Sci. 2010, 118, 517–524. [Google Scholar] [CrossRef]
- Ikeda, M.; Kurokawa, H.; Sunada, N.; Tamura, Y.; Takimoto, M.; Murayama, R.; Ando, S.; Miyazaki, M. Influence of previous acid etching on dentin bond strength of self-etch adhesives. J. Oral Sci. 2009, 51, 527–534. [Google Scholar] [CrossRef]
- Wagner, A.; Wendler, M.; Petschelt, A.; Belli, R.; Lohbauer, U. Bonding performance of universal adhesives in different etching modes. J. Dent. 2014, 42, 800–807. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Niu, L.N.; Xie, H.; Zhang, Z.Y.; Zhou, L.Q.; Jiao, K.; Chen, J.H.; Pashley, D.H.; Tay, F.R. Bonding of universal adhesives to dentine--Old wine in new bottles? J. Dent. 2015, 43, 525–536. [Google Scholar] [CrossRef]
- Alqahtani, M.Q. Influence of acid-etching or double-curing time on dentin bond strength of one-step self-etch adhesive. Saudi J. Dent. Res. 2015, 6, 110–116. [Google Scholar] [CrossRef][Green Version]
- Fukegawa, D.; Hayakawa, S.; Yoshida, Y.; Suzuki, K.; Osaka, A.; Van Meerbeek, B. Chemical interaction of phosphoric acid ester with hydroxyapatite. J. Dent. Res. 2006, 85, 941–944. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.M.; Tay, F.R.; King, N.M.; Imazato, S.; Pashley, D.H. Bonding of mild self-etching primers/adhesives to dentin with thick smear layers. Am. J. Dent. 2003, 16, 340–346. [Google Scholar]
- Ayar, M.K.; Yesilyurt, C.; Yildirim, T. Effect of Different Composite Placement Molds on Resin-Enamel/Dentin Shear Bond Strength. J. Res. Med. Dent. Sci. 2016, 4, 141. [Google Scholar] [CrossRef]
- Harouny, R.; Hardan, L.; Harouny, E.; Kassis, C.; Bourgi, R.; Lukomska-Szymanska, M.; Kharouf, N.; Ball, V.; Khairallah, C. Adhesion of Resin to Lithium Disilicate with Different Surface Treatments before and after Salivary Contamination—An In-Vitro Study. Bioengineering 2022, 9, 286. [Google Scholar] [CrossRef]
- Beloica, M.; Goracci, C.; Carvalho, C.-A.; Radovic, I.; Margvelashvili, M.; Vulicevic, Z.-R.; Ferrari, M. Microtensile vs microshear bond strength of all-in-one adhesives to unground enamel. J. Adhes. Dent. 2010, 12, 427–433. [Google Scholar] [PubMed]
- Sano, H.; Chowdhury, A.F.-M.A.; Saikaew, P.; Matsumoto, M.; Hoshika, S.; Yamauti, M. The microtensile bond strength test: Its historical background and application to bond testing. Jpn. Dent. Sci. Rev. 2020, 56, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Sahadi, B.O.; Sebold, M.; André, C.B.; Nima, G.; Dos Santos, A.; Nascimento, F.D.; dos Santos Tersariol, I.L.; Giannini, M. Effect of experimental dentin etchants on dentin bond strength, metalloproteinase inhibition, and antibiofilm activity. Dent. Mater. 2024, 40, e12–e23. [Google Scholar] [CrossRef]
- Saikaew, P.; Sattabanasuk, V.; Harnirattisai, C.; Chowdhury, A.F.M.A.; Carvalho, R.; Sano, H. Role of the smear layer in adhesive dentistry and the clinical applications to improve bonding performance. Jpn. Dent. Sci. Rev. 2022, 58, 59–66. [Google Scholar] [CrossRef]


| Devices | Manufacturer |
|---|---|
| DENTIPURE KM™ | KM, Beirut, Lebanon |
| KAVO™ ESTETICA E30/E70/E80 Vision | KAVO, Biberach, Germany |
| ADEC™ A-dec Performer 200 | ADEC, Newberg, OR, USA |
| Material | Manufacturer | Main Components |
|---|---|---|
| Adhesive: Prime & Bond | DENTSPLY Charlotte, NC, USA | Dipentaerythritol penta acrylate monophosphate, polymerizeable dimethacrylate resin, polymerizeable PE trimethacrylate resin, diketon, organic phosphine oxide, stabilizers, cetylamine hydrofluoride, water. |
| Etching: Onyx | CENTRIX, Shelton, CT, USA | Phosphoric acid concentration: 40% |
| Bulk fill composite: SDR plus | DENTSPLY Charlotte, NC, USA | Urethane dimethacrylate resin, dimethacrylate resin, di-functional diluents barium and strontium, aluminofluorosilicate glasses, photo initiating system colorants. |
| Devices | PBU |
|---|---|
| ADEC | 12.572 (5.901) a |
| DENTIPURE KM | 15.018 (4.895) b |
| KAVO | 13.681 (5.011) a,b |
| Grups | N | 1 | 2 |
|---|---|---|---|
| ADEC | 60 | 12.57211 | |
| KAVO | 60 | 13.68098 | 13.68098 |
| DENTIPURE KM | 60 | 15.01836 | |
| p | 0.486 | 0.351 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kharma, K.; Hardan, L.; Kassis, C.; Dimitriu, B.; Harouny, R.; Baba, N.Z.; Bourgi, R.; Zogheib, C.M. Can a Novel Device with Pure Dry Air Increase the Shear Bond Strength of Dental Composites to Dentin? An Experimental Study. Dent. J. 2024, 12, 160. https://doi.org/10.3390/dj12060160
Kharma K, Hardan L, Kassis C, Dimitriu B, Harouny R, Baba NZ, Bourgi R, Zogheib CM. Can a Novel Device with Pure Dry Air Increase the Shear Bond Strength of Dental Composites to Dentin? An Experimental Study. Dentistry Journal. 2024; 12(6):160. https://doi.org/10.3390/dj12060160
Chicago/Turabian StyleKharma, Khalil, Louis Hardan, Cynthia Kassis, Bogdan Dimitriu, Ryan Harouny, Nadim Z. Baba, Rim Bourgi, and Carina Mehanna Zogheib. 2024. "Can a Novel Device with Pure Dry Air Increase the Shear Bond Strength of Dental Composites to Dentin? An Experimental Study" Dentistry Journal 12, no. 6: 160. https://doi.org/10.3390/dj12060160
APA StyleKharma, K., Hardan, L., Kassis, C., Dimitriu, B., Harouny, R., Baba, N. Z., Bourgi, R., & Zogheib, C. M. (2024). Can a Novel Device with Pure Dry Air Increase the Shear Bond Strength of Dental Composites to Dentin? An Experimental Study. Dentistry Journal, 12(6), 160. https://doi.org/10.3390/dj12060160








