40-Year Outcome of Old-School, Non-Surgical Endodontic Treatment: Practice-Based Retrospective Evaluation
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Clinical Outcomes for Practitioner A
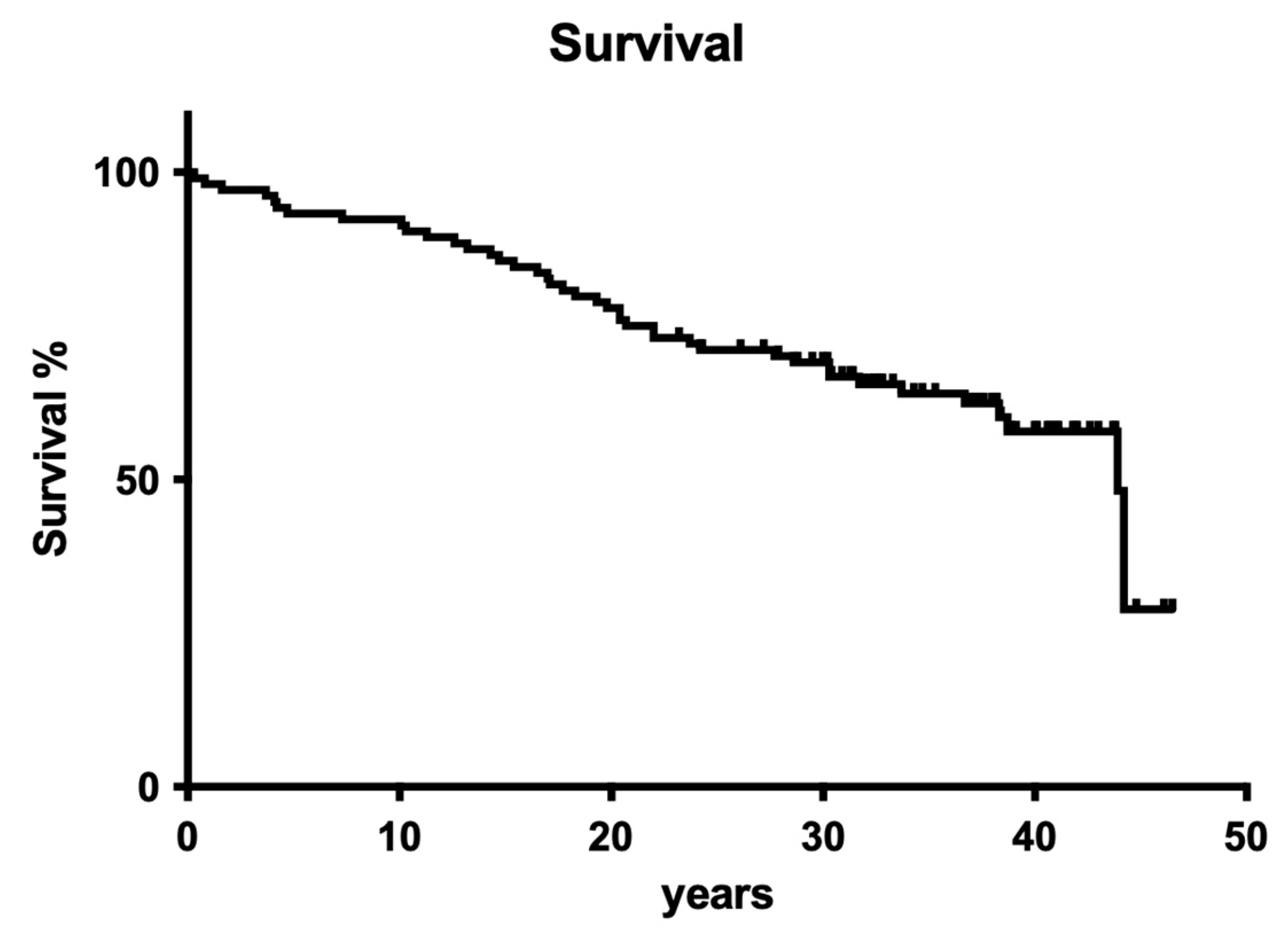
3.1.1. Overall Tooth Survival
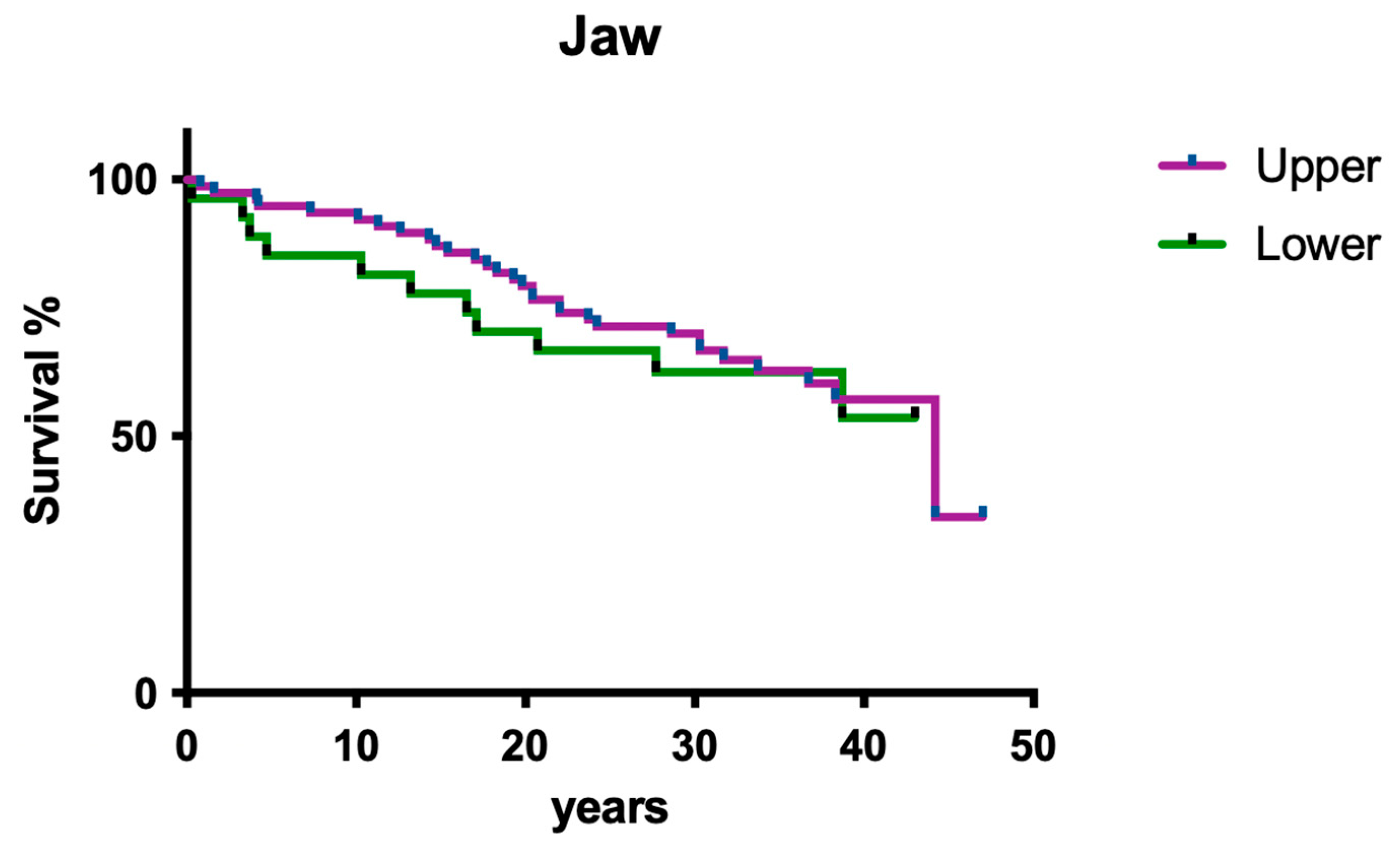
3.1.2. Influence of Jaw
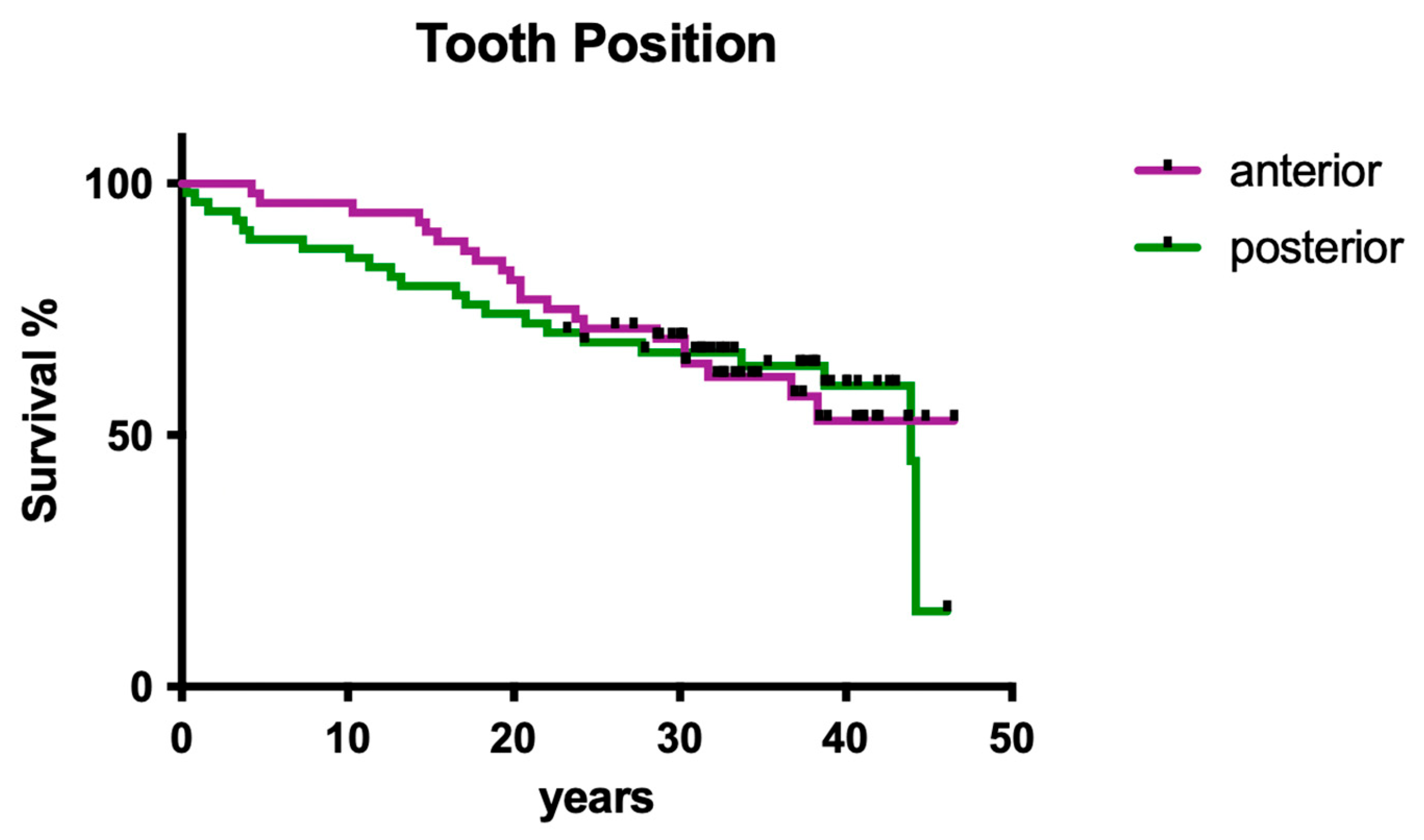
3.1.3. Influence of Tooth Position
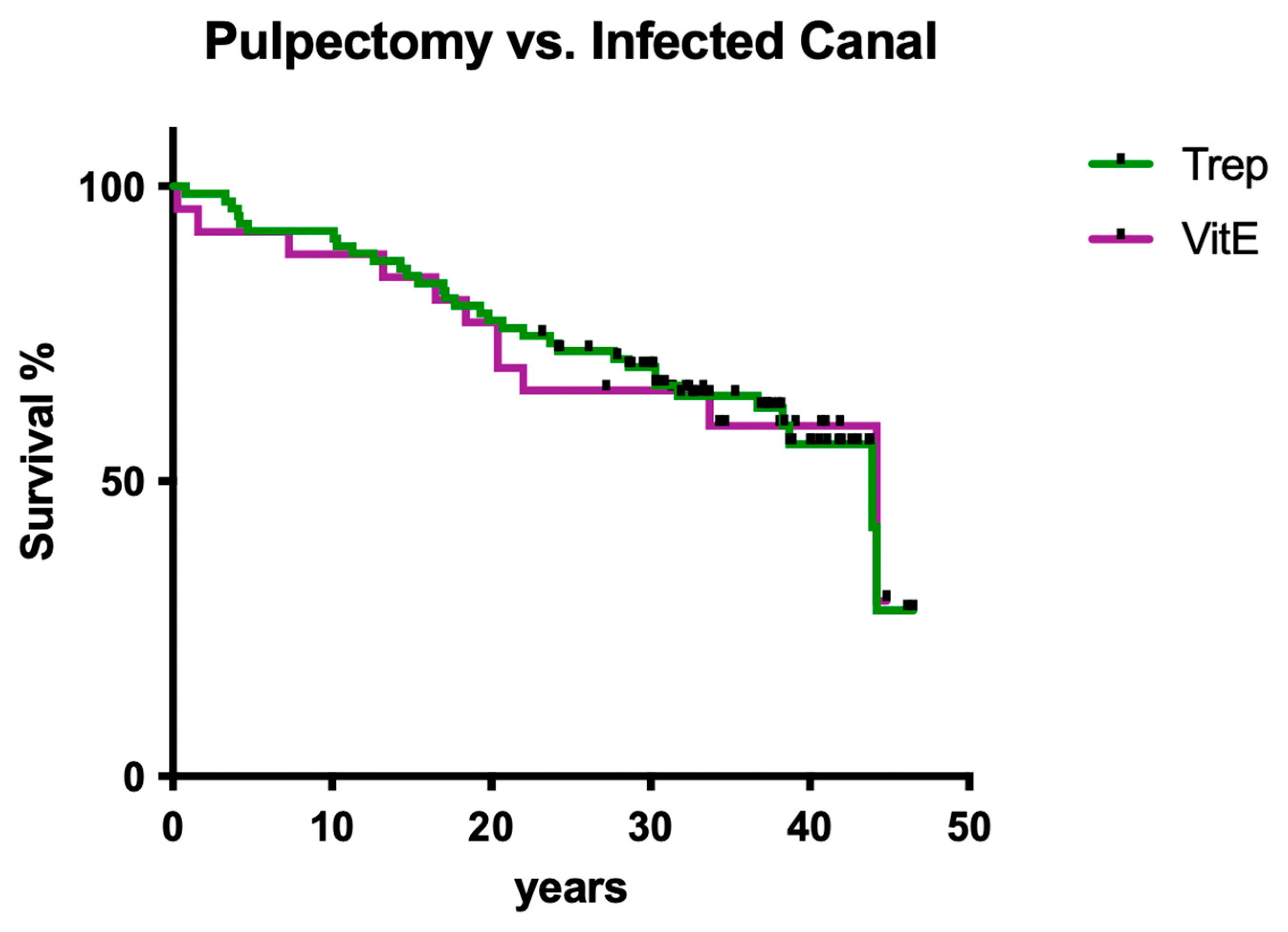
3.1.4. Influence of Root Canal Infection
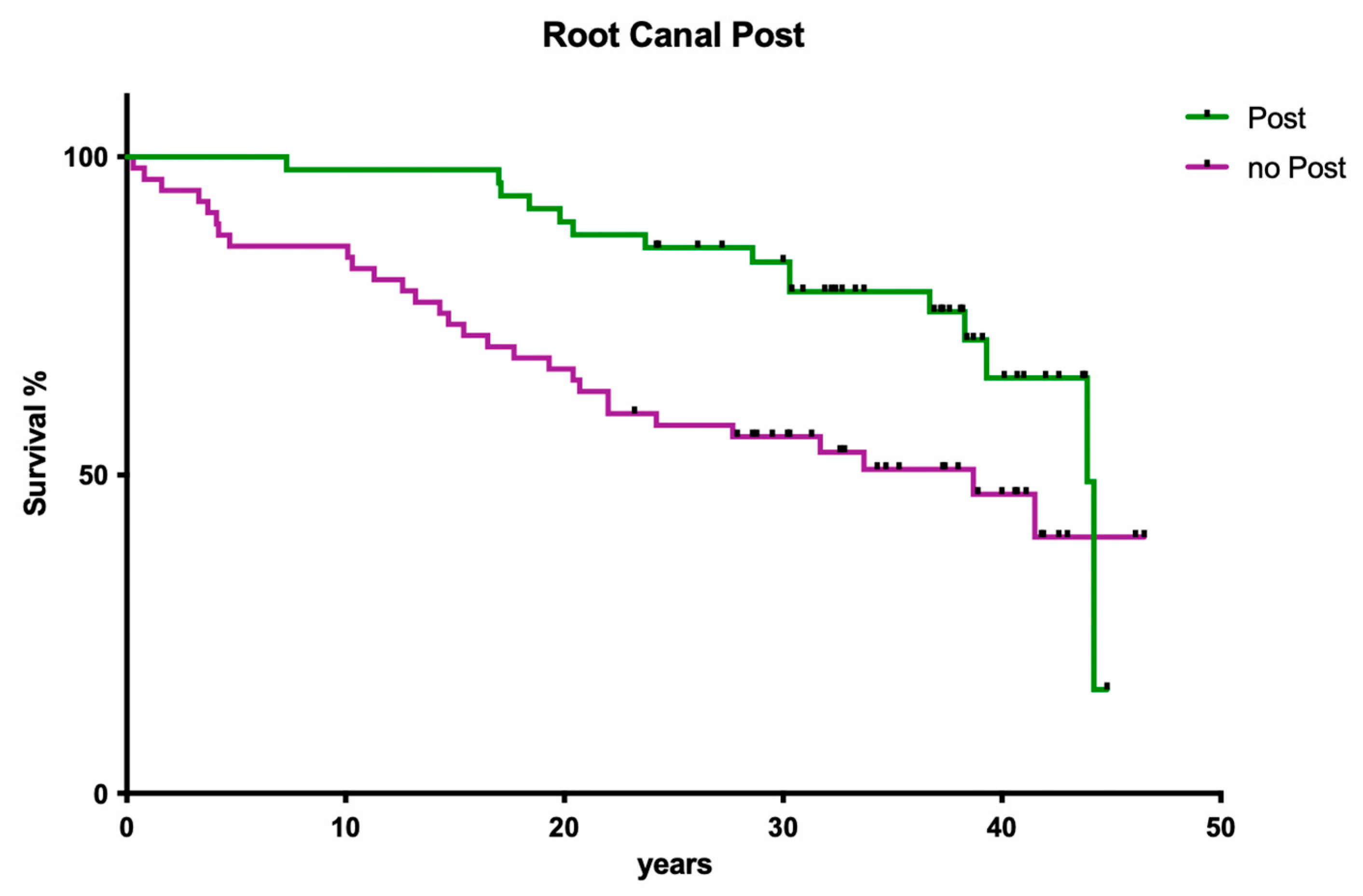
3.1.5. Influence of Post Insertion
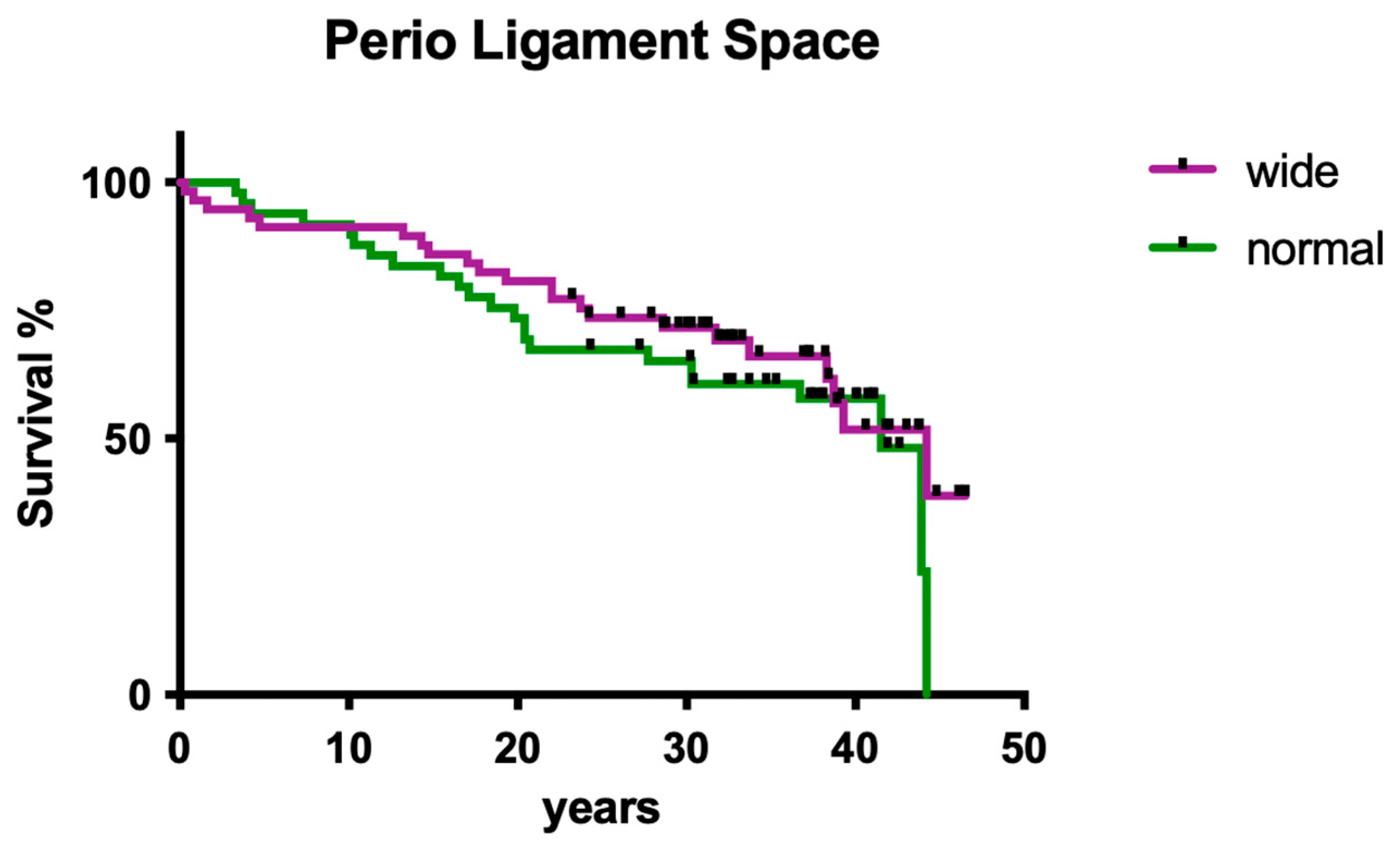
3.1.6. Influence of Periodontal Ligament Space
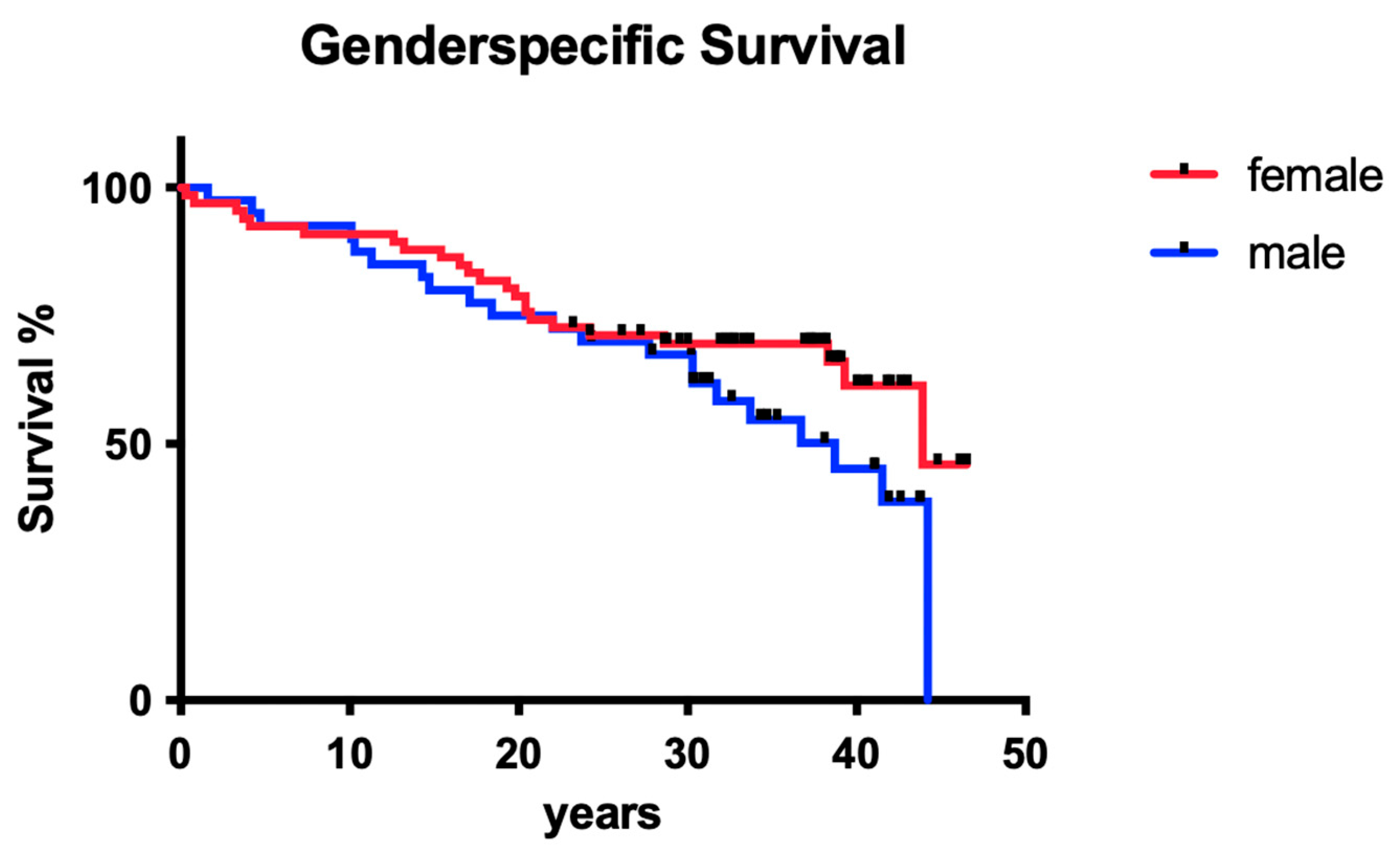
3.1.7. Influence of Gender
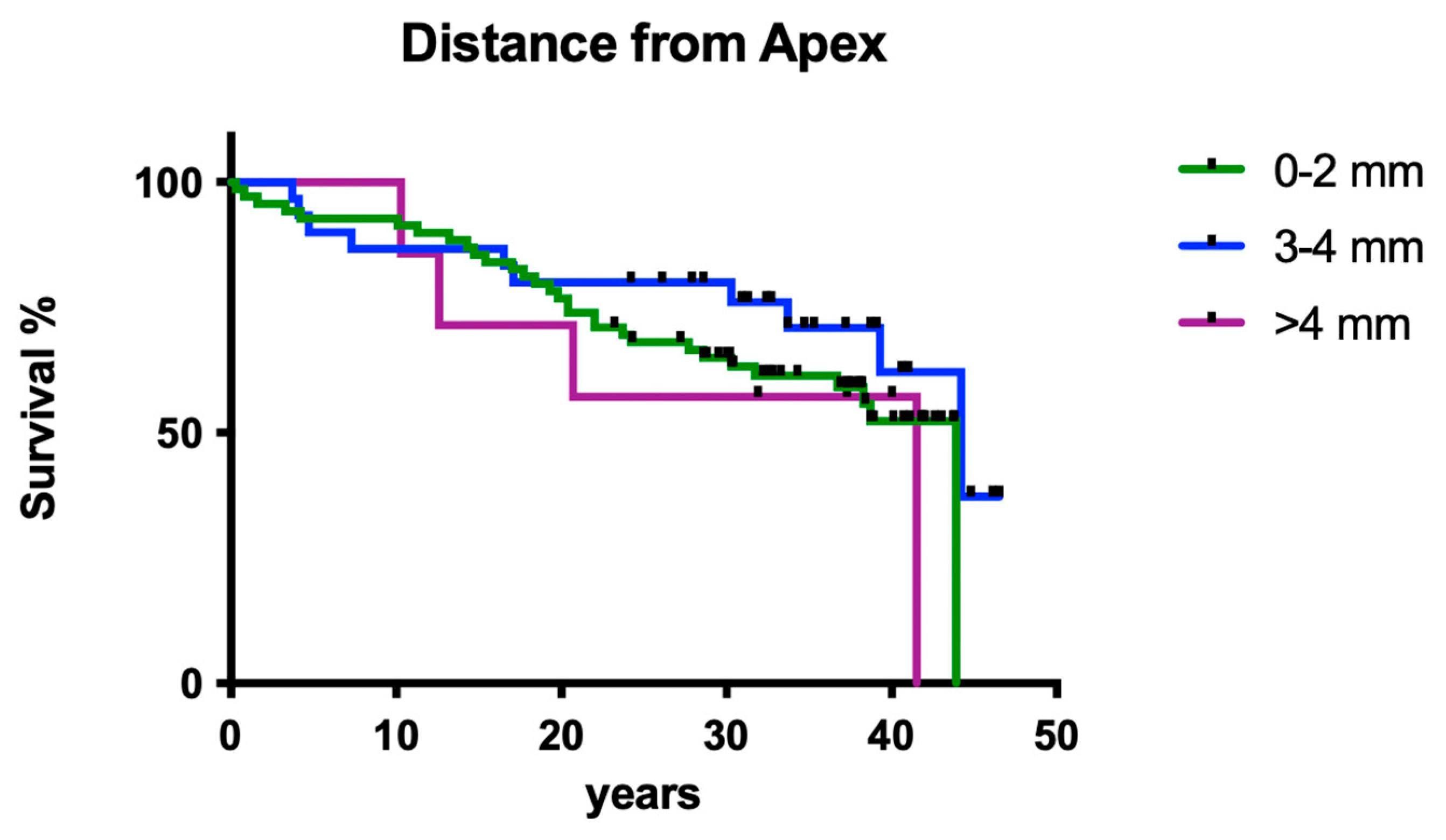
3.1.8. Influence of Working Length
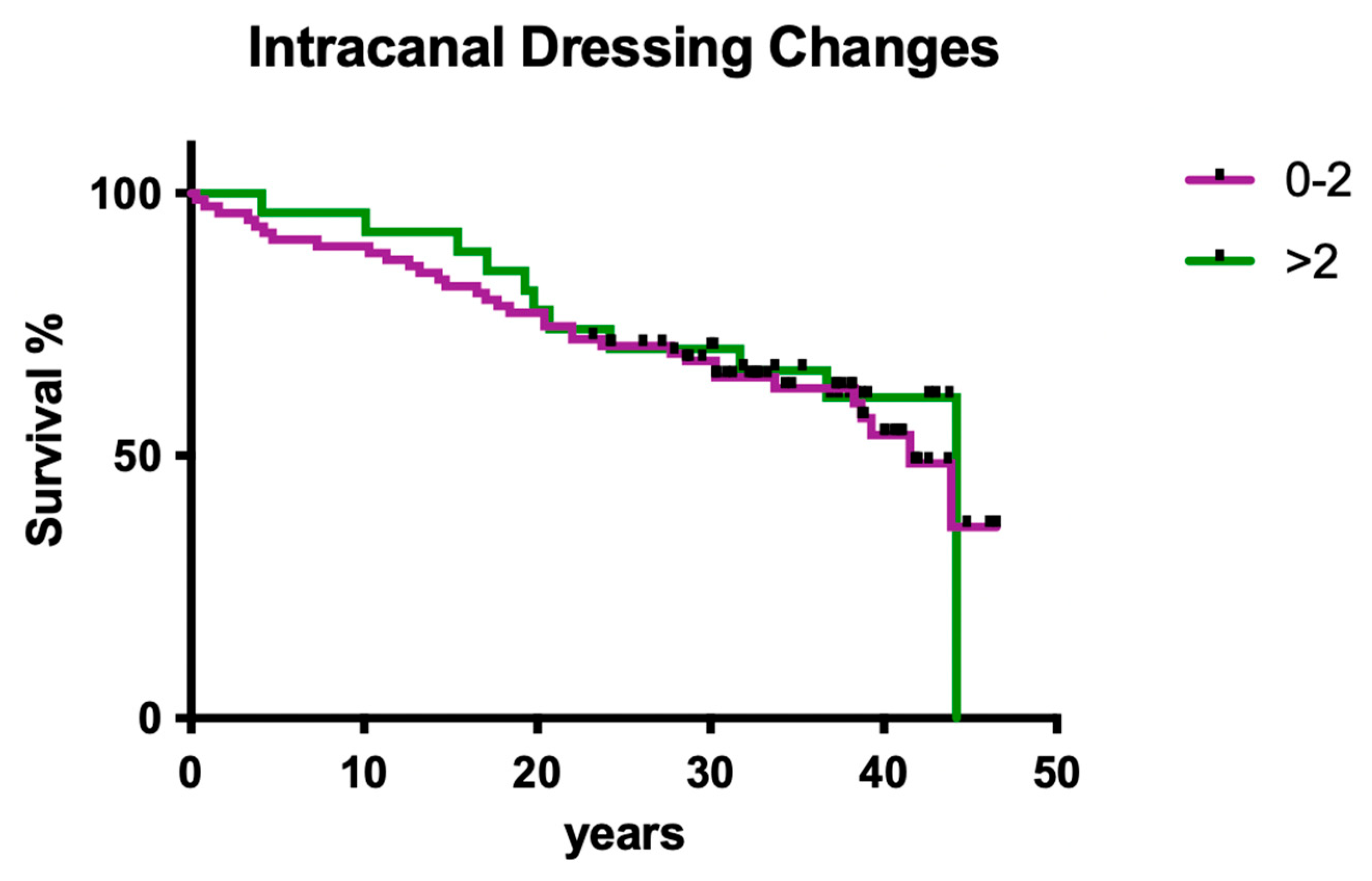
3.1.9. Influence of Intracanal Dressing Changes
3.2. Clinical Outcome Practitioner B
3.2.1. Overall Survival
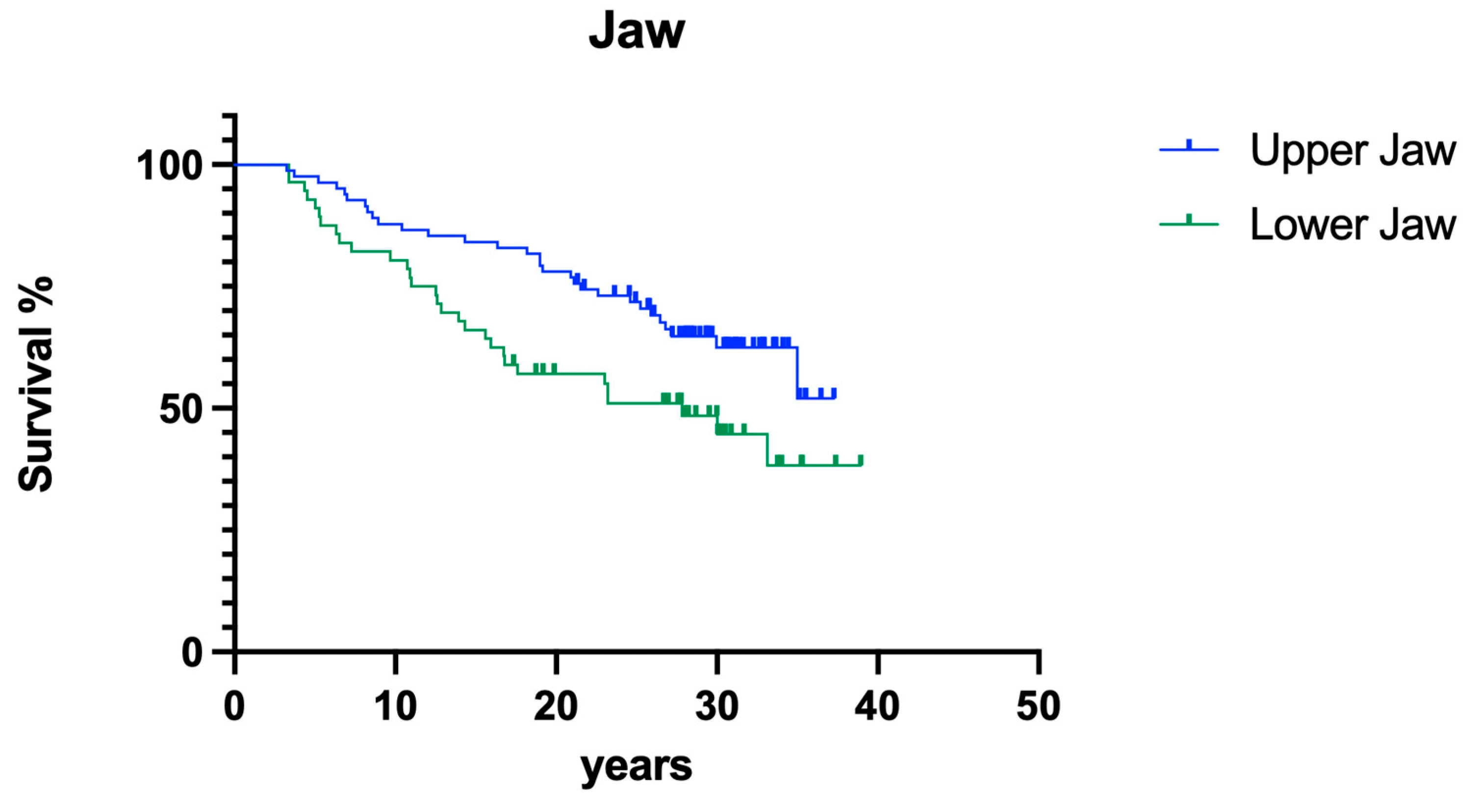
3.2.2. Jaw
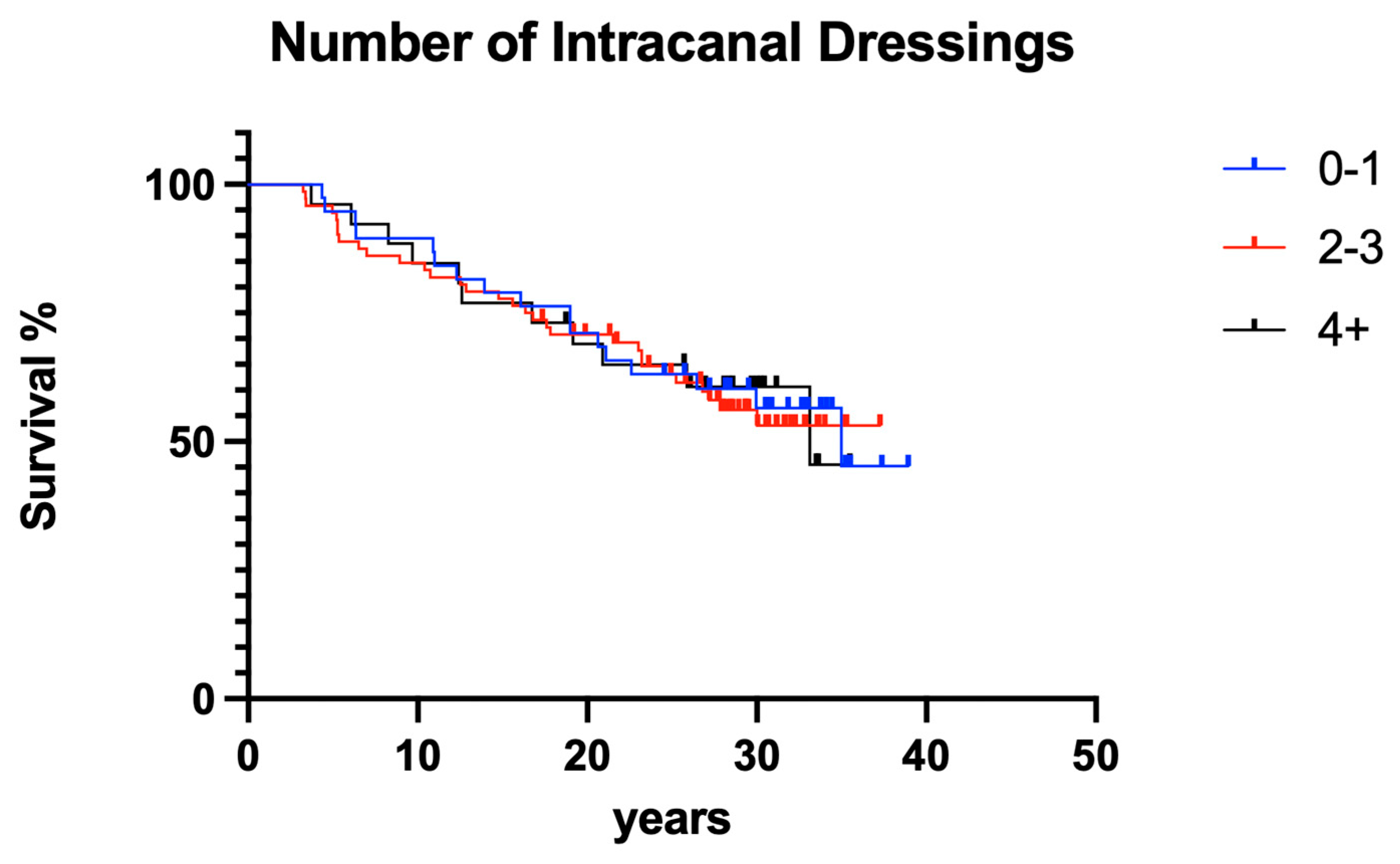
3.2.3. Number of Intracanal Dressing Changes
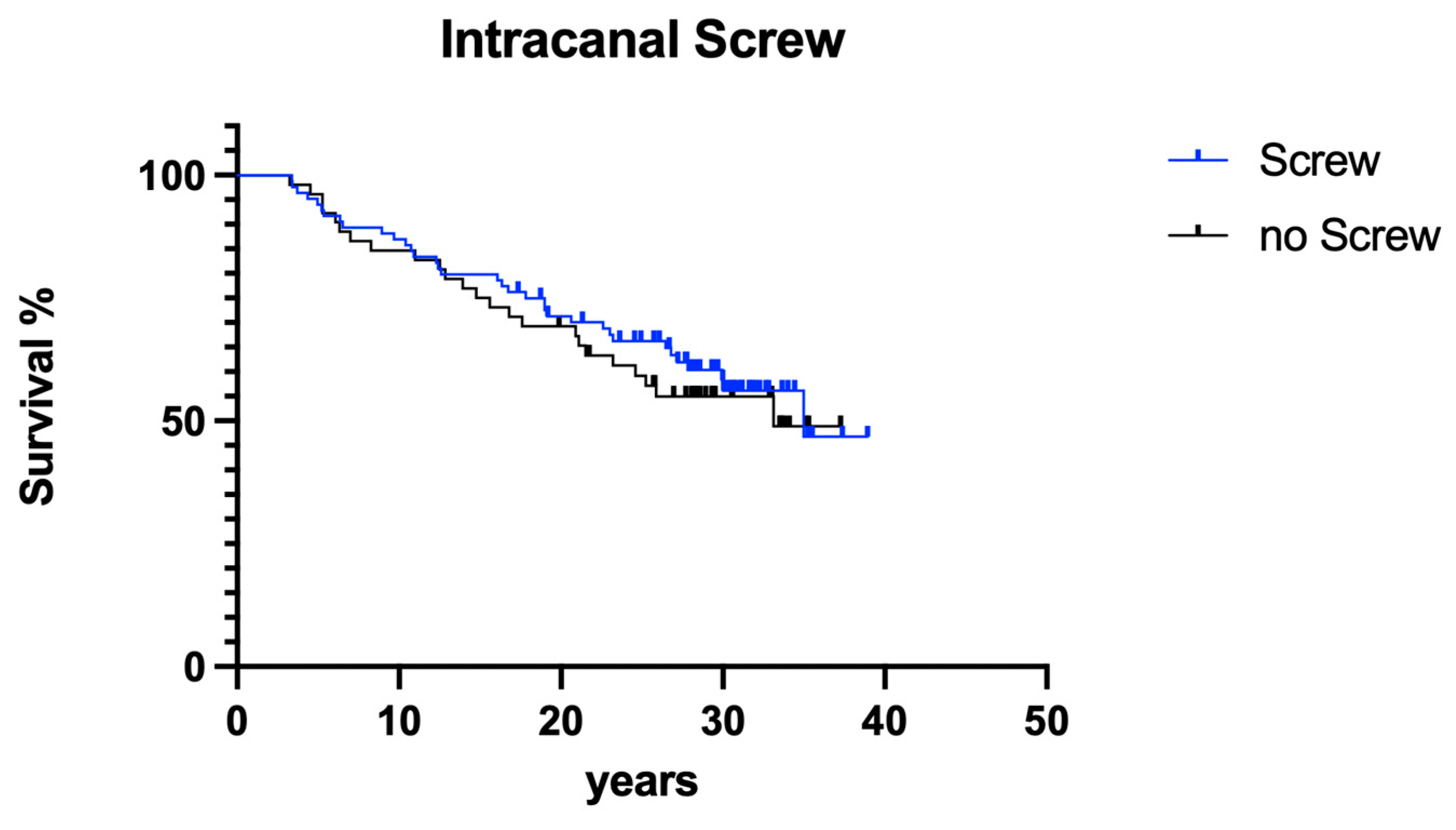
3.2.4. Screws
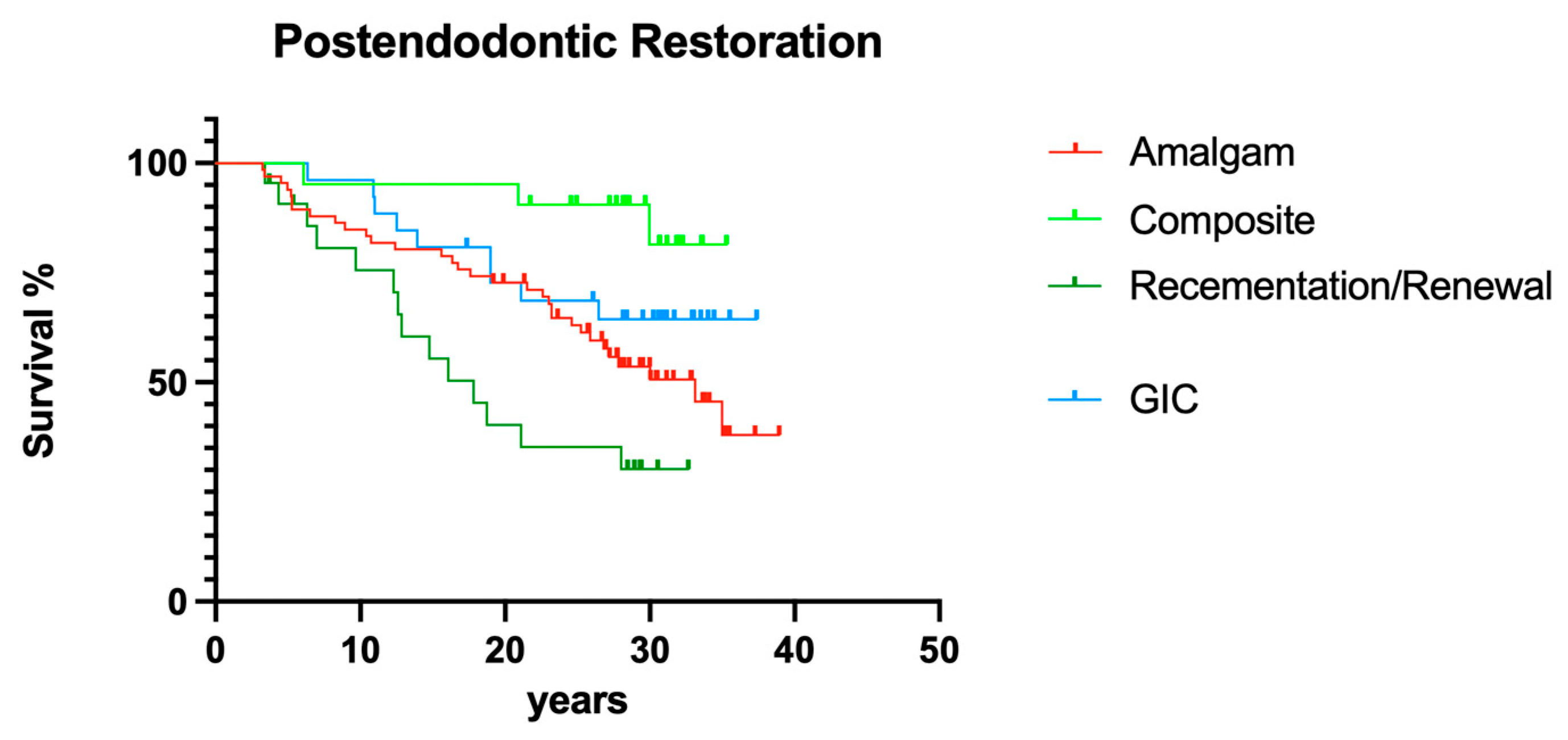
3.2.5. Post-endodontic Restoration
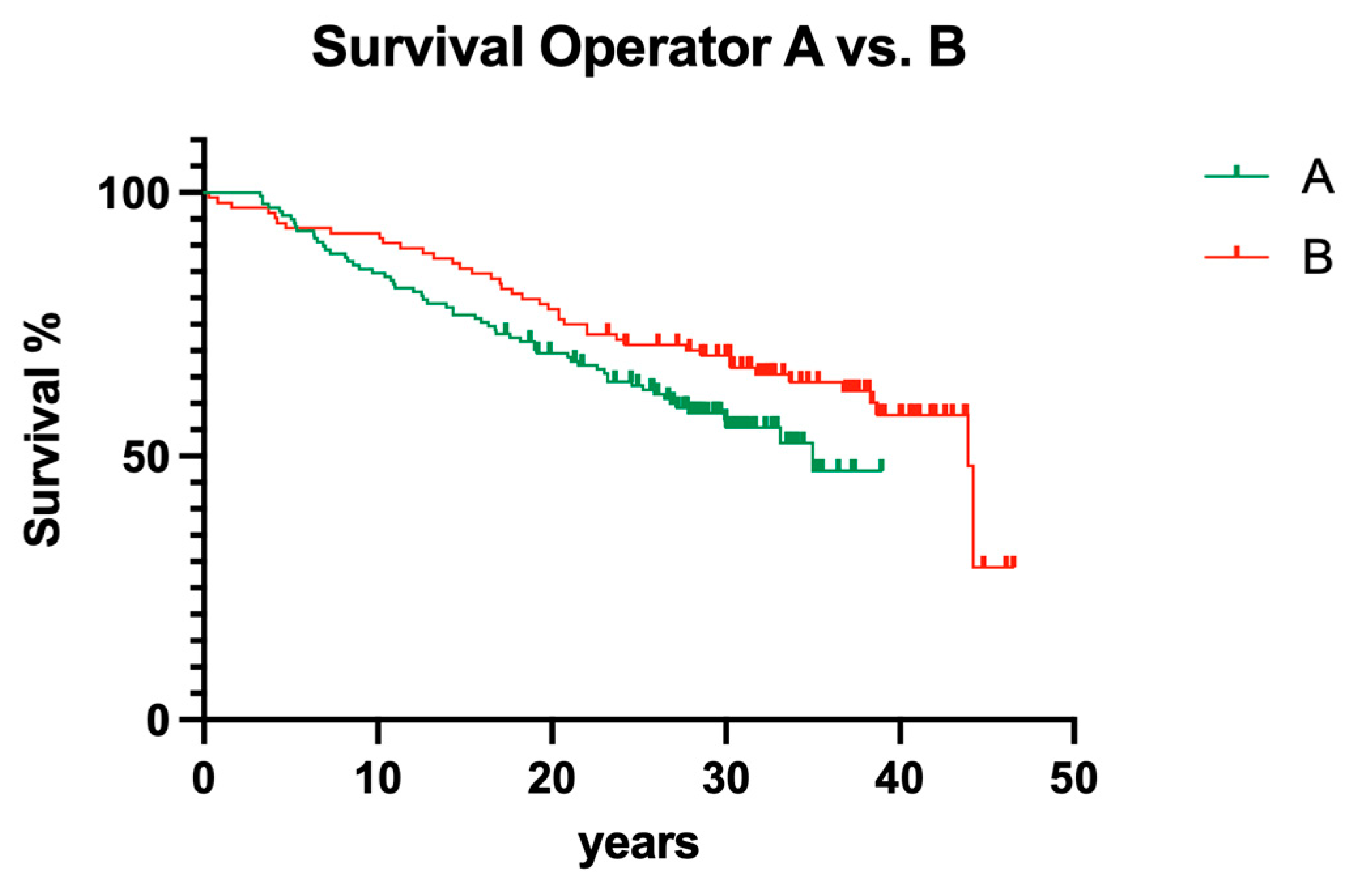
3.3. Interoperator Comparison
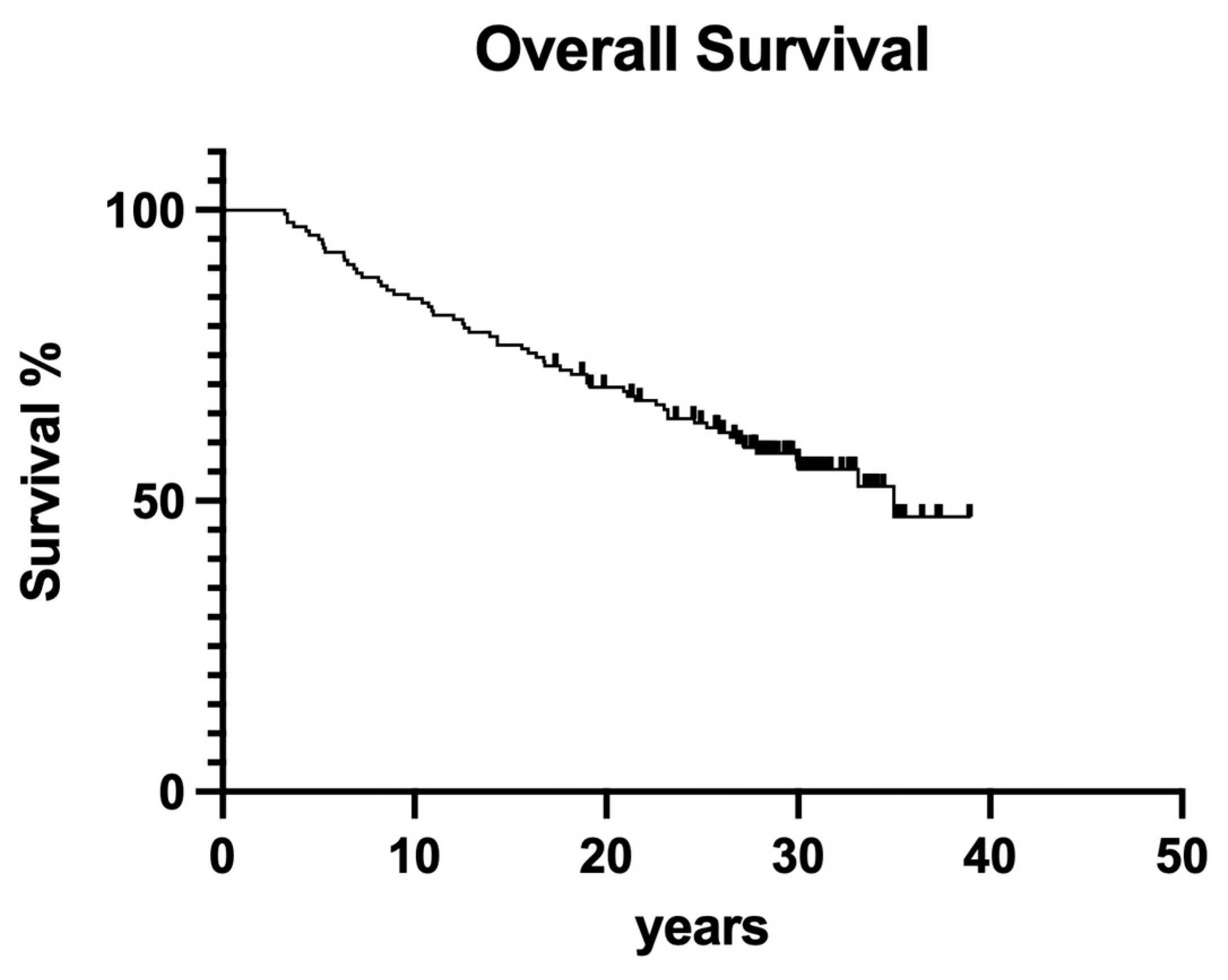
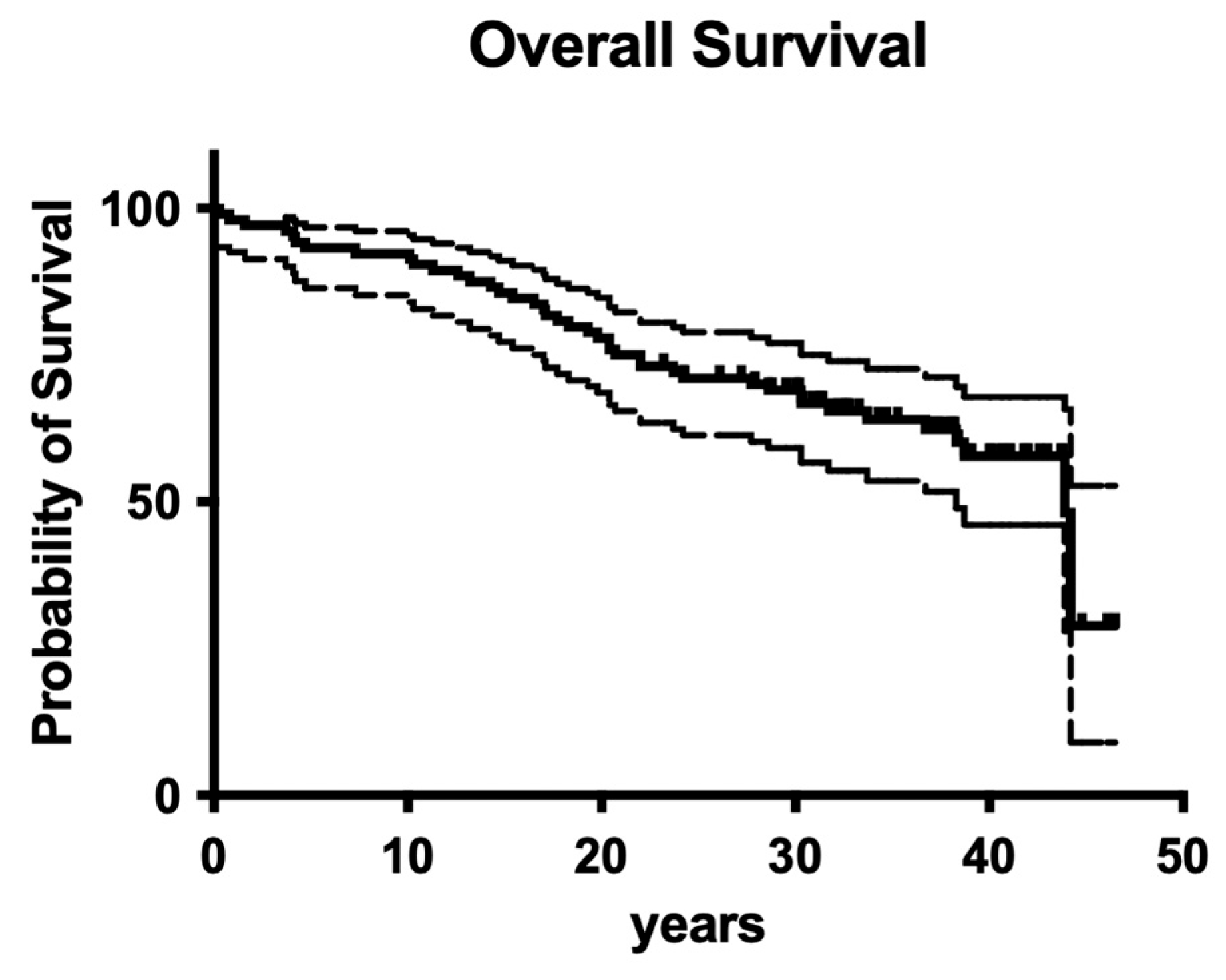
3.4. Overall Survival
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Banerjee, A.; Splieth, C.; Breschi, L.; Fontana, M.; Paris, S.; Burrow, M.; Crombie, F.; Foster Page, L.; Gaton-Hernandez, P.; Giacaman, R.A.; et al. When to intervene in the caries process? A Delphi consensus statement. Br. Dent. J. 2020, 229, 474–482. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Splieth, C.H.; Bottenberg, P.; Breschi, L.; Campus, G.; Domejean, S.; Ekstrand, K.; Giacaman, R.A.; Haak, R.; Hannig, M.; et al. How to intervene in the caries process in adults: Proximal and secondary caries? An EFCD-ORCA-DGZ expert Delphi consensus statement. Clin. Oral. Investig. 2020, 24, 3315–3321. [Google Scholar] [CrossRef] [PubMed]
- European Society of Endodontology (ESE); Duncan, H.F.; Galler, K.M.; Tomson, P.L.; Simon, S.; El-Karim, I.; Kundzina, R.; Krastl, G.; Dammaschke, T.; Fransson, H.; et al. European Society of Endodontology position statement: Management of deep caries and the exposed pulp. Int. Endod. J. 2019, 52, 923–934. [Google Scholar] [CrossRef] [PubMed]
- Chopra, V.; Davis, G.; Baysan, A. Clinical and Radiographic Outcome of Non-Surgical Endodontic Treatment Using Calcium Silicate-Based Versus Resin-Based Sealers-A Systematic Review and Meta-Analysis of Clinical Studies. J. Funct. Biomater. 2022, 13, 38. [Google Scholar] [CrossRef]
- Van Nieuwenhuysen, J.P.; D’Hoore, W.; Leprince, J.G. What ultimately matters in root canal treatment success and tooth preservation: A 25-year cohort study. Int. Endod. J. 2023, 56, 544–557. [Google Scholar] [CrossRef] [PubMed]
- Frankenberger, R.; Van Meerbeek, B. Editorial: Citations in Science–Original Research vs Review Papers. J. Adhes. Dent. 2020, 22, 231. [Google Scholar] [CrossRef]
- Cornish, F. Evidence synthesis in international development: A critique of systematic reviews and a pragmatist alternative. Anthropol. Med. 2015, 22, 263–277. [Google Scholar] [CrossRef] [PubMed]
- Duncan, H.F.; Kirkevang, L.L.; Orstavik, D.; Sequeira-Byron, P. Research that matters–clinical studies. Int. Endod. J. 2016, 49, 224–226. [Google Scholar] [CrossRef] [PubMed]
- Greener, M. The good, the bad and the ugly red tape of biomedical research. How could regulators lower bureaucratic hurdles in clinical research without compromising the safety of patients? EMBO Rep. 2009, 10, 17–20. [Google Scholar] [CrossRef]
- Osanto, S.; van Poppel, H.; Burggraaf, J.; Hall, R.R. Hurdles in modern trial management: As overbureaucracy and commercialization of clinical trials suffocate independent academic research, it’s time for a change. Eur. Urol. 2009, 56, 622–624. [Google Scholar] [CrossRef]
- Dugas, N.N.; Lawrence, H.P.; Teplitsky, P.; Friedman, S. Quality of life and satisfaction outcomes of endodontic treatment. J. Endod. 2002, 28, 819–827. [Google Scholar] [CrossRef] [PubMed]
- Leong, D.J.X.; Yap, A.U. Quality of life of patients with endodontically treated teeth: A systematic review. Aust. Endod. J. 2020, 46, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Neelakantan, P.; Liu, P.; Dummer, P.M.H.; McGrath, C. Oral health-related quality of life (OHRQoL) before and after endodontic treatment: A systematic review. Clin. Oral. Investig. 2020, 24, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Hatipoglu, O.; Hatipoglu, F.P.; Javed, M.Q.; Nijakowski, K.; Taha, N.; El-Saaidi, C.; Sugumaran, S.; Elhamouly, Y.; Drobac, M.; Machado, R.; et al. Factors Affecting the Decision-making of Direct Pulp Capping Procedures among Dental Practitioners: A Multinational Survey from 16 Countries with Meta-analysis. J. Endod. 2023, 49, 675–685. [Google Scholar] [CrossRef] [PubMed]
- Bergenholtz, G.; Kvist, T. Call for improved research efforts on clinical procedures in endodontics. Int. Endod. J. 2013, 46, 697–699. [Google Scholar] [CrossRef] [PubMed]
- Leprince, J.G.; Van Nieuwenhuysen, J.P. The missed root canal story: Aren’t we missing the point? Int. Endod. J. 2020, 53, 1162–1166. [Google Scholar] [CrossRef] [PubMed]
- Ricucci, D.; Russo, J.; Rutberg, M.; Burleson, J.A.; Spangberg, L.S. A prospective cohort study of endodontic treatments of 1,369 root canals: Results after 5 years. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2011, 112, 825–842. [Google Scholar] [CrossRef] [PubMed]
- Ng, Y.L.; Mann, V.; Gulabivala, K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 1: Periapical health. Int. Endod. J. 2011, 44, 583–609. [Google Scholar] [CrossRef]
- Friedman, S.; Abitbol, S.; Lawrence, H.P. Treatment outcome in endodontics: The Toronto Study. Phase 1: Initial treatment. J. Endod. 2003, 29, 787–793. [Google Scholar] [CrossRef]
- Ray, H.A.; Trope, M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int. Endod. J. 1995, 28, 12–18. [Google Scholar] [CrossRef]
- European Society of Endodontology developed, b.; Mannocci, F.; Bhuva, B.; Roig, M.; Zarow, M.; Bitter, K. European Society of Endodontology position statement: The restoration of root filled teeth. Int. Endod. J. 2021, 54, 1974–1981. [Google Scholar] [CrossRef] [PubMed]
- Bruhnke, M.; Naumann, M.; Beuer, F.; Bose, M.W.H.; von Stein-Lausnitz, M.; Schwendicke, F. Implant or tooth?–A cost-time analysis of managing “unrestorable” teeth(✰). J. Dent. 2023, 136, 104646. [Google Scholar] [CrossRef] [PubMed]
- Mannocci, F.; Bitter, K.; Sauro, S.; Ferrari, P.; Austin, R.; Bhuva, B. Present status and future directions: The restoration of root filled teeth. Int. Endod. J. 2022, 55 (Suppl. 4), 1059–1084. [Google Scholar] [CrossRef] [PubMed]
- Naumann, M.; Schmitter, M.; Krastl, G. Postendodontic Restoration: Endodontic Post-and-Core or No Post At All? J. Adhes. Dent. 2018, 20, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Naumann, M.; Schmitter, M.; Frankenberger, R.; Krastl, G. “Ferrule Comes First. Post Is Second!” Fake News and Alternative Facts? A Systematic Review. J. Endod. 2018, 44, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Schafer, E.; Zapke, K. A comparative scanning electron microscopic investigation of the efficacy of manual and automated instrumentation of root canals. J. Endod. 2000, 26, 660–664. [Google Scholar] [CrossRef] [PubMed]
- Pantaleo, G.; Amato, A.; Iandolo, A.; Abdellatif, D.; Di Spirito, F.; Caggiano, M.; Pisano, M.; Blasi, A.; Fornara, R.; Amato, M. Two-Year Healing Success Rates after Endodontic Treatment Using 3D Cleaning Technique: A Prospective Multicenter Clinical Study. J. Clin. Med. 2022, 11, 6213. [Google Scholar] [CrossRef] [PubMed]
- Stueland, H.; Orstavik, D.; Handal, T. Treatment outcome of surgical and non-surgical endodontic retreatment of teeth with apical periodontitis. Int. Endod. J. 2023, 56, 686–696. [Google Scholar] [CrossRef]
- Winkler, A.; Adler, P.; Ludwig, J.; Hofmann, N.; Soliman, S.; Krastl, G.; Krug, R. Endodontic Outcome of Root Canal Treatment Using Different Obturation Techniques: A Clinical Study. Dent. J. 2023, 11, 200. [Google Scholar] [CrossRef]
- Frankenberger, R.; Reinelt, C.; Petschelt, A.; Kramer, N. Operator vs. material influence on clinical outcome of bonded ceramic inlays. Dent. Mater. 2009, 25, 960–968. [Google Scholar] [CrossRef]
- Schmitter, M.; Hamadi, K.; Rammelsberg, P. Survival of two post systems--five-year results of a randomized clinical trial. Quintessence Int. 2011, 42, 843–850. [Google Scholar] [PubMed]
| Variables (P1) | Endodontically Treated Teeth | Extractions | |
|---|---|---|---|
| Preoperative | |||
| n = 107 | n = 46 | ||
| Gender | Male (29) | 66 | |
| Female (44) | |||
| Tooth location | Upper jaw | 77 | |
| Lower Jaw | 27 | ||
| Anterior | 52 | ||
| Posterior | 54 | ||
| Coronal caries | 63 | 31 | |
| Root caries | 4 | 2 | |
| Sensitivity to percussion | Yes | 75 | 30 |
| No | 32 | 16 | |
| Vitality status | Vital | 29 | 16 |
| Non-vital | 75 | 30 | |
| Presence of apical radiolucency | Yes | 45 | 27 |
| No | 62 | 19 | |
| Periapical space | Normal | 49 | 23 |
| Enlarged | 58 | 23 | |
| Tooth function | Distal tooth in quadrant | 13 | 4 |
| Bridge in abutment | 10 | 9 | |
| Double proximal contact | 84 | 33 | |
| Distance of root canal filling to apex | 0–2 mm | 59 | 27 |
| 2–3 mm | 31 | 12 | |
| ≥4 mm | 16 | 7 | |
| Number of intracanal medications | 0 | 35 | 14 |
| 1 | 21 | 11 | |
| 2 | 24 | 9 | |
| 3 | 19 | 10 | |
| 4 or more | 8 | 2 | |
| Post | Yes | 49 | 17 |
| No | 58 | 29 | |
| Variables (P2) | Endodontically Treated Teeth | Extraction | |
|---|---|---|---|
| Pre-operative | |||
| n = 138 | n = 61 | ||
| Gender | Male | ||
| Female | |||
| Deep caries | 11 | 6 | |
| Vitality status | Vital | 46 | 23 |
| Non-vital | 60 | 23 | |
| No data | 32 | 15 | |
| Pain symptoms | Yes | 11 | 5 |
| No data | 127 | 56 | |
| Sensitivity to percussion | Yes | 137 | 61 |
| No | 1 | 0 | |
| Operator | P1 | 104 | 42 |
| P2 | 138 | 60 | |
| P1 anterior | 52 | 21 | |
| P1 posterior | 54 | 22 | |
| P2 anterior | 30 | 9 | |
| P2 posterior | 108 | 51 | |
| Tooth location | Upper jaw | 82 | 30 |
| Lower Jaw | 56 | 30 | |
| Anterior upper jaw | 30 | 9 | |
| Posterior upper jaw | 52 | 21 | |
| Posterior lower jaw | 56 | 30 | |
| Number of intracanal medications | 0–1 | 38 | 17 |
| 2–3 | 72 | 31 | |
| ≥4 | 26 | 11 | |
| Duration from trepanation to root canal filling | 0 | 18 | 10 |
| 1–14 days | 10 | 4 | |
| 15–28 days | 33 | 12 | |
| >28 days | 75 | 34 | |
| Post | Yes | 86 | 37 |
| No | 52 | 24 | |
| Restoration | Amalgam | 66 | 33 |
| Composite | 21 | 3 | |
| Recementation/renewal of prosthetic restoration | 22 | 14 | |
| Glass ionomer cement | 26 | 9 | |
| Periodontal therapy | Yes | 30 | 13 |
| No | 108 | 47 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frankenberger, R.; Becker, S.; Beck-Broichsitter, B.; Albrecht-Hass, S.; Behrens, C.J.; Roggendorf, M.J.; Koch, A. 40-Year Outcome of Old-School, Non-Surgical Endodontic Treatment: Practice-Based Retrospective Evaluation. Dent. J. 2024, 12, 90. https://doi.org/10.3390/dj12040090
Frankenberger R, Becker S, Beck-Broichsitter B, Albrecht-Hass S, Behrens CJ, Roggendorf MJ, Koch A. 40-Year Outcome of Old-School, Non-Surgical Endodontic Treatment: Practice-Based Retrospective Evaluation. Dentistry Journal. 2024; 12(4):90. https://doi.org/10.3390/dj12040090
Chicago/Turabian StyleFrankenberger, Roland, Stephan Becker, Benedicta Beck-Broichsitter, Susanne Albrecht-Hass, Charlotte J. Behrens, Matthias J. Roggendorf, and Andreas Koch. 2024. "40-Year Outcome of Old-School, Non-Surgical Endodontic Treatment: Practice-Based Retrospective Evaluation" Dentistry Journal 12, no. 4: 90. https://doi.org/10.3390/dj12040090
APA StyleFrankenberger, R., Becker, S., Beck-Broichsitter, B., Albrecht-Hass, S., Behrens, C. J., Roggendorf, M. J., & Koch, A. (2024). 40-Year Outcome of Old-School, Non-Surgical Endodontic Treatment: Practice-Based Retrospective Evaluation. Dentistry Journal, 12(4), 90. https://doi.org/10.3390/dj12040090








