Effectiveness of Lidocaine with Epinephrine Irrigation in Reducing Acute Pain from Surgical Removal of Mesioangular-Impacted Third Molars
Abstract
1. Introduction
2. Materials and Methods
2.1. Drugs
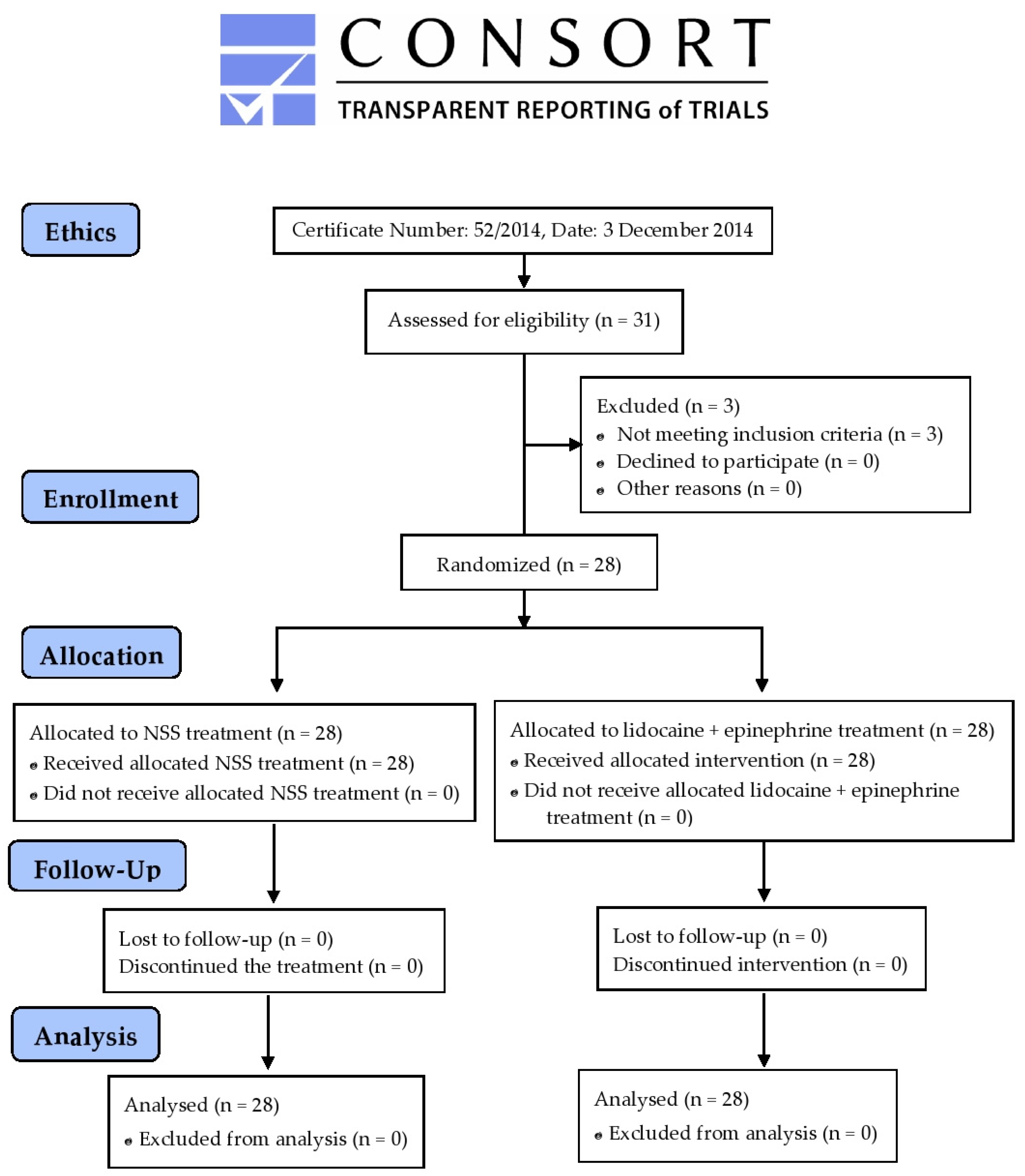
2.2. Ethics
2.3. Clinical Trial Registry
2.4. Patients’ History
2.5. Patient Preparation
2.6. Sample Size Calculation
2.7. Study Design and Clinical Evaluation
2.8. Study Variables
2.9. Subject Allocation and Randomization
2.10. Surgical Intervention
2.11. VAS Assessment
2.12. Postoperative Medication
2.13. Statistical Analysis
3. Results
3.1. Participant Information
3.2. VAS Scores
3.3. Analgesic Effect Associated with Paracetamol
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Santosh, P. Impacted mandibular third molars: Review of literature and a proposal of a combined clinical and radiological classification. Ann. Med. Health Sci. Res. 2015, 5, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Unwerawattana, W. Common symptoms and type of impacted molar tooth in King Chulalongkorn Memorial Hospital. J. Med. Assoc. Thai 2006, 89 (Suppl. S3), S134–S139. Available online: https://www.ncbi.nlm.nih.gov/pubmed/17718279 (accessed on 5 October 2024). [PubMed]
- Osunde, O.; Saheeb, B.; Bassey, G. Indications and risk factors for complications of lower third molar surgery in a nigerian teaching hospital. Ann. Med. Health Sci. Res. 2014, 4, 938–942. [Google Scholar] [CrossRef]
- Jerjes, W.; Upile, T.; Nhembe, F.; Gudka, D.; Shah, P.; Abbas, S.; McCarthy, E.; Patel, S.; Mahil, J.; Hopper, C. Experience in third molar surgery: An update. Br. Dent. J. 2010, 209, E1. [Google Scholar] [CrossRef]
- Thorat, S.D.; Nilesh, K. Efficacy of low-level laser therapy in the management of postoperative surgical sequelae after surgical removal of impacted mandibular third molars. Natl. J. Maxillofac. Surg. 2022, 13, S52–S56. [Google Scholar] [CrossRef]
- Sreesha, S.; Ummar, M.; Sooraj, S.; Aslam, S.; Roshni, A.; Jabir, K. Postoperative pain, edema and trismus following third molar surgery—A comparitive study between submucosal and intravenous dexamethasone. J. Fam. Med. Prim. Care 2020, 9, 2454–2459. [Google Scholar] [CrossRef]
- Kasapoglu, M.B.; Cebi, A.T. Randomized split-mouth study for evaluating the efficacy of nimesulide and nimesulide + Thiocolchicoside combination following impacted mandibular third molar surgery. Niger. J. Clin. Pract. 2022, 25, 641–646. [Google Scholar] [CrossRef]
- Yang, M.; Li, T.; Wang, H.; Zhang, Q.; Yang, H.; Chi, Y.; Hou, J. Effect of a thermosensitive hydroxybutyl chitosan hydrogel on postoperative sequalae and quality of life after impacted mandibular third molar extraction. J. Oral. Maxillofac. Surg. 2024, 82, 1246–1256. [Google Scholar] [CrossRef] [PubMed]
- Givens, V.A.; Lipscomb, G.H.; Meyer, N.L. A randomized trial of postoperative wound irrigation with local anesthetic for pain after cesarean delivery. Am. J. Obstet. Gynecol. 2002, 186, 1188–1191. [Google Scholar] [CrossRef] [PubMed]
- Mc Loughlin, S.; Bianco, J.C.; Marenchino, R.G. Anesthetic and perioperative considerations for combined heart-kidney transplantation. J. Cardiothorac. Vasc. Anesth. 2018, 32, 44–49. [Google Scholar] [CrossRef]
- Manaa, E. Local anesthetic irrigation and postoperative pain in patients undergoing breast augmentation. J. Anesth. Clin. Res. 2011, 2, 1000151. [Google Scholar] [CrossRef]
- Khalil, H. A basic review on the inferior alveolar nerve block techniques. Anesth. Essays Res. 2014, 8, 3–8. [Google Scholar] [CrossRef]
- Nazeer, J.; Kumari, S.; Haidry, N.; Kulkarni, P.; Aastha; Gautam, A.; Gupta, P. Comparison of efficacy of lignocaine, ropivacaine, and bupivacaine in pain control during extraction of mandibular posterior teeth. Natl. J. Maxillofac. Surg. 2021, 12, 238–243. [Google Scholar] [CrossRef]
- Drucker, M.; Cardenas, E.; Arizti, P.; Valenzuela, A.; Gamboa, A. Experimental studies on the effect of lidocaine on wound healing. World J. Surg. 1998, 22, 394–397. [Google Scholar] [CrossRef]
- Bahar, E.; Yoon, H. Lidocaine: A local anesthetic, its adverse effects and management. Medicina 2021, 57, 782. [Google Scholar] [CrossRef]
- Khorshidi Khiavi, R.; Pourallahverdi, M.; Pourallahverdi, A.; Ghorani Khiavi, S.; Ghertasi Oskouei, S.; Mokhtari, H. Pain control following impacted third molar surgery with bupivacaine irrigation of tooth socket: A prospective study. J. Dent. Res. Dent. Clin. Dent. Prospect. 2010, 4, 105–109. [Google Scholar] [CrossRef]
- Karns, J.L. Epinephrine-induced potentially lethal arrhythmia during arthroscopic shoulder surgery: A case report. AANA J. 1999, 67, 419–421. Available online: https://www.ncbi.nlm.nih.gov/pubmed/10876433 (accessed on 27 July 2024). [PubMed]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef]
- Synan, W.; Stein, K. Management of impacted third molars. Oral. Maxillofac. Surg. Clin. N. Am. 2020, 32, 519–559. [Google Scholar] [CrossRef] [PubMed]
- Abouleish, A.E.; Leib, M.L.; Cohen, N.H. ASA provides examples to each ASA physical status class. ASA Newsl. 2015, 79, 38–49. [Google Scholar]
- Rauten, A.M.; Surlin, P.; Oprea, B.; Silosi, I.; Moisa, M.; Caramizaru, D.; Vatu, M. Matrix metalloproteinase 9 levels in gingival crevicular fluid in patients after periodontal microsurgery for orthodontic induced gingival hypertrophy. Rom. J. Morphol. Embryol. 2011, 52, 431–433. Available online: https://www.ncbi.nlm.nih.gov/pubmed/21424088 (accessed on 1 May 2024).
- Yamano, S.; Kuo, W.P.; Sukotjo, C. Downregulated gene expression of TGF-betas in diabetic oral wound healing. J. Craniomaxillofac Surg. 2013, 41, e42–e48. [Google Scholar] [CrossRef]
- Surin, W.; Chatiketu, P.; Hutachok, N.; Srichairatanakool, S.; Chatupos, V. Pain intensity and salivary alpha-amylase activity in patients following mandibular third molar surgery. Clin. Exp. Dent. Res. 2022, 8, 1082–1091. [Google Scholar] [CrossRef]
- Rodrigues, F.V.; Hochman, B.; Wood, V.T.; Simoes, M.J.; Juliano, Y.; Ferreira, L.M. Effects of lidocaine with epinephrine or with buffer on wound healing in rat skin. Wound Repair Regen. 2011, 19, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Graefe, S.; Mohiuddin, S.S. Biochemistry, Substance P. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Eshghpour, M.; Nejat, A.H. Dry socket following surgical removal of impacted third molar in an Iranian population: Incidence and risk factors. Niger. J. Clin. Pract. 2013, 16, 496–500. [Google Scholar] [CrossRef]
- Sisk, A.L. Vasoconstrictors in local anesthesia for dentistry. Anesth. Prog. 1992, 39, 187–193. Available online: https://www.ncbi.nlm.nih.gov/pubmed/8250339 (accessed on 1 May 2024). [PubMed]
- Grouselle, M.; Tueux, O.; Dabadie, P.; Georgescaud, D.; Mazat, J.P. Effect of local anaesthetics on mitochondrial membrane potential in living cells. Biochem. J. 1990, 271, 269–272. [Google Scholar] [CrossRef] [PubMed]
- Karpie, J.C.; Chu, C.R. Lidocaine exhibits dose- and time-dependent cytotoxic effects on bovine articular chondrocytes in vitro. Am. J. Sports Med. 2007, 35, 1621–1627. [Google Scholar] [CrossRef]
- Waite, A.; Gilliver, S.C.; Masterson, G.R.; Hardman, M.J.; Ashcroft, G.S. Clinically relevant doses of lidocaine and bupivacaine do not impair cutaneous wound healing in mice. Br. J. Anaesth. 2010, 104, 768–773. [Google Scholar] [CrossRef]
- Tappeiner, C.; Flueckiger, F.; Boehnke, M.; Goldblum, D.; Garweg, J.G. Effect of topical anesthetic agents and ethanol on corneoepithelial wound healing in an ex vivo whole-globe porcine model. J. Cataract. Refract. Surg. 2012, 38, 519–524. [Google Scholar] [CrossRef]
- Castagna, V.; Pardo, A.; Lanaro, L.; Signoriello, A.; Albanese, M. Periodontal healing after lower third molars extraction: A clinical evaluation of different flap designs. Healthcare 2022, 10, 1587. [Google Scholar] [CrossRef]
- Nourwali, I. The effects of platelet-rich fibrin on post-surgical complications following removal of impacted wisdom teeth: A pilot study. J. Taibah Univ. Med. Sci. 2021, 16, 521–528. [Google Scholar] [CrossRef] [PubMed]
| Rinsing Solution | Factors | |
|---|---|---|
| Volume of Local Anesthetic (mL) | Duration of Surgery (min) | |
| NSS | 2.03 ± 0.38 | 43.21 ± 7.34 |
| Lidocaine with epinephrine | 1.96 ± 0.33 NS | 41.87 ± 6.85 NS |
| Treatment | Postoperative VAS Scores | ||
|---|---|---|---|
| 3 h | 4 h | 5 h | |
| NSS | 44.25 ± 27.16 | 48.67 ± 21.43 | 42.63 ± 23.08 |
| Lidocaine with epinephrine | 19.44 ± 18.03 * | 27.63 ± 19.26 *,# | 39.74 ± 19.73 |
| Treatment | Postoperative Paracetamol Consumption (Tablet/Person) | ||||||
|---|---|---|---|---|---|---|---|
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | |
| NSS | 3.17 ± 0.78 | 2.27 ± 0.66 | 1.03 ± 0.59 | 0.93 ± 0.47 ** | 0.32 ± 0.29 * | 0.09 ± 0.15 | 0.02 ± 0.15 |
| Lidocaine + epinephrine | 2.34 ± 0.41 ** | 1.81 ± 0.69 ** | 0.65 ± 0.49 ** | 0.37 ± 0.21 | 0 | 0 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chatupos, V.; Apiphathanamontri, M.; Yuthavong, S.; Chatiketu, P.; Hutachok, N.; Srichairatanakool, S. Effectiveness of Lidocaine with Epinephrine Irrigation in Reducing Acute Pain from Surgical Removal of Mesioangular-Impacted Third Molars. Dent. J. 2024, 12, 412. https://doi.org/10.3390/dj12120412
Chatupos V, Apiphathanamontri M, Yuthavong S, Chatiketu P, Hutachok N, Srichairatanakool S. Effectiveness of Lidocaine with Epinephrine Irrigation in Reducing Acute Pain from Surgical Removal of Mesioangular-Impacted Third Molars. Dentistry Journal. 2024; 12(12):412. https://doi.org/10.3390/dj12120412
Chicago/Turabian StyleChatupos, Vuttinun, Molee Apiphathanamontri, Sumatee Yuthavong, Piyanart Chatiketu, Nuntouchaporn Hutachok, and Somdet Srichairatanakool. 2024. "Effectiveness of Lidocaine with Epinephrine Irrigation in Reducing Acute Pain from Surgical Removal of Mesioangular-Impacted Third Molars" Dentistry Journal 12, no. 12: 412. https://doi.org/10.3390/dj12120412
APA StyleChatupos, V., Apiphathanamontri, M., Yuthavong, S., Chatiketu, P., Hutachok, N., & Srichairatanakool, S. (2024). Effectiveness of Lidocaine with Epinephrine Irrigation in Reducing Acute Pain from Surgical Removal of Mesioangular-Impacted Third Molars. Dentistry Journal, 12(12), 412. https://doi.org/10.3390/dj12120412







