Fixed Full-Arch Implant-Supported Restorations: Techniques Review and Proposal for Improvement
Abstract
1. Introduction
2. Aim and Rationale
3. Treatment Concepts
3.1. The Fixed Denture
3.2. The Ohio State University Method
3.3. Brånemark Novum Protocol
3.4. Trefoil System
3.5. Stumpel Modular Substructure
3.6. The Malo/Toronto Bridges
3.7. The Bar with Sectioned Restorations
3.8. Complete Arch Zirconia Screwed to a Metal Bar
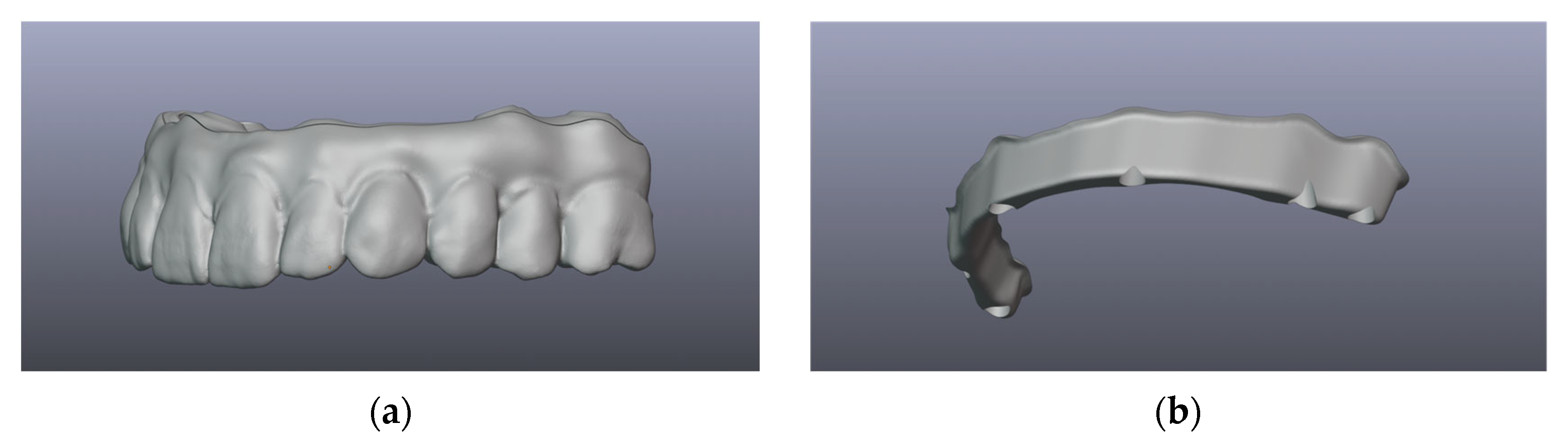
3.9. Full-Arch Zirconia
4. Proposal for Improvement
4.1. The Choice
4.2. The Proposed Novel Technique
4.2.1. Data Acquisition
- Assessment of implant positioning
- Optical registration with an intraoral scanner (IOS) or with a photogrammetry device must be carried out; photogrammetry has been shown to have better accuracy when superimposing implant positions for all-on-X-type restorations [51].
- Conventional pick-up impression with splinted impression copings, followed by model casting with implant analogs and model scanning must be carried out directly in the dental office, or the technician can provide a jig to be splinted intraorally.
- A mixed protocol may allow the use of an intraoral scan for gingiva and implant positioning, followed by a bonded jig for precision assessment, model casting and scanning and finally overlapping the first and second scans.
- Registration of gingiva can be carried out at the same time as the implant positioning assessment or it can be scanned/impression-model-scanned and digitally overlapped.
- Vertical dimension of occlusion (VDO) can be assessed using photography, facial scanning, radiographs or occlusal rims.
- Intermaxillary occlusal relations may be assessed through either static or dynamic occlusal registration.
- Static occlusion registration—through the use of occlusal rims.
- Dynamic occlusion registration—through the use of devices that capture and record real jaw motion.

4.2.2. Restoration Design and Validation
4.2.3. Manufacturing and Delivery
4.2.4. Follow-Up
5. Discussion
5.1. Passivity and Accuracy
5.2. Strength and Flexibility
5.3. Weight
5.4. Biological Aspects and Interfaces
5.5. Maintenance
5.6. Options
6. Conclusions
- Material and technology advancements:
- ○
- Modern digital workflows offer clinicians a wide range of materials and techniques that encompass both analog and digital approaches for fixed dental prostheses (FDPs), each with specific strengths and limitations.
- Proposed technique combines:
- ○
- Passivity, strength, and weight reduction via a titanium framework.
- ○
- Aesthetic benefits and durability through a zirconia superstructure.
- Reverse engineering process:
- ○
- Utilizes advanced software with a dual software approach to reverse engineer the titanium bar based on the desired restoration.
- ○
- Enhances the esthetic outcome by optimizing the design for predictability, volume, and weight reduction.
- Potential limitations:
- ○
- The presence of an additional interface could present long-term challenges.
- ○
- Evidence supporting the long-term biological and mechanical performance of hybrid restorations, such as those combining titanium and zirconia, is currently limited.
- Future directions:
- ○
- Further research is needed, including clinical follow-up and comparative studies to assess the outcomes and long-term performance of various FDP restoration options.
- ○
- Comparative research should focus on evaluating analog and digital workflows to identify best practices for specific clinical scenarios.
- ○
- Continued advancements in cost-effective, user-friendly digital solutions can help bridge gaps in accessibility and adoption, while maintaining a biologically driven treatment approach.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al-Rafee, M.A. The epidemiology of edentulism and the associated factors: A literature Review. J. Fam. Med. Prim. Care 2020, 9, 1841–1843. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Prevalence of Edentulism in People 20+ Years. 2023. Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/prevalence-of-edentulism-in-people-20--years (accessed on 16 July 2024).
- Chimbinha, Í.G.M.; Ferreira, B.N.C.; Miranda, G.P.; Guedes, R.S. Oral-health-related quality of life in adolescents: Umbrella review. BMC Public Health 2023, 23, 1603. [Google Scholar] [CrossRef]
- Kronstrom, M.; Carlsson, G.E. An International Survey among Prosthodontists of the Use of Mandibular Implant-Supported Dental Prostheses. J. Prosthodont. 2019, 28, e622–e626. [Google Scholar] [CrossRef] [PubMed]
- Peñarrocha-Diago, M.; Peñarrocha-Diago, M.; Zaragozi-Alonso, R.; Soto-Peñaloza, D.; On behalf of the Ticare Consensus Meeting. Consensus statements and clinical recommendations on treatment indications, surgical procedures, prosthetic protocols and complications following All-On-4 standard treatment. 9th Mozo-Grau Ticare Conference in Quintanilla, Spain. J. Clin. Exp. Dent. 2017, 9, e712–e715. [Google Scholar] [CrossRef]
- Galindo, D.F.; Butura, C.C. Immediately loaded mandibular fixed implant prostheses using the all-on-four protocol: A report of 183 consecutively treated patients with 1 year of function in definitive prostheses. Int. J. Oral Maxillofac. Implant. 2012, 27, 628–633. [Google Scholar]
- Soto-Penaloza, D.; Zaragozi-Alonso, R.; Penarrocha-Diago, M.; Penarrocha-Diago, M. The all-on-four treatment concept: Systematic review. J. Clin. Exp. Dent. 2017, 9, e474–e488. [Google Scholar] [CrossRef] [PubMed]
- Wakam, R.; Benoit, A.; Mawussi, K.B.; Gorin, C. Evaluation of Retention, Wear, and Maintenance of Attachment Systems for Single- or Two-Implant-Retained Mandibular Overdentures: A Systematic Review. Materials 2022, 15, 1933. [Google Scholar] [CrossRef]
- Ramanauskaite, A.; Becker, K.; Wolfart, S.; Lukman, F.; Schwarz, F. Efficacy of rehabilitation with different approaches of implant-supported full-arch prosthetic designs: A systematic review. J. Clin. Periodontol. 2022, 49 (Suppl. S24), 272–290. [Google Scholar] [CrossRef] [PubMed]
- Abou-Ayash, S.; Fonseca, M.; Pieralli, S.; Reissmann, D.R. Treatment effect of implant-supported fixed complete dentures and implant overdentures on patient-reported outcomes: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2023, 34 (Suppl. S26), 177–195. [Google Scholar] [CrossRef]
- Beresford, D.; Klineberg, I. A Within-Subject Comparison of Patient Satisfaction and Quality of Life Between a Two-Implant Overdenture and a Three-Implant-Supported Fixed Dental Prosthesis in the Mandible. Int. J. Oral Maxillofac. Implant. 2018, 33, 1374–1382. [Google Scholar] [CrossRef]
- Elsyad, M.A.; El-Asfahani, I.A.; Kortam, S.A.; Mourad, S.I. Masseter muscle activity of conventional denture, fixed prosthesis, and milled bar overdenture used for All-on-4 implant rehabilitation: A within-subject study. Clin. Implant. Dent. Relat. Res. 2021, 23, 408–416. [Google Scholar] [CrossRef]
- Delucchi, F.; De Giovanni, E.; Pesce, P.; Bagnasco, F.; Pera, F.; Baldi, D.; Menini, M. Framework Materials for Full-Arch Implant-Supported Rehabilitations: A Systematic Review of Clinical Studies. Materials 2021, 14, 3251. [Google Scholar] [CrossRef]
- Wang, J.; Wu, P.; Liu, H.L.; Zhang, L.; Liu, L.P.; Ma, C.F.; Chen, J.H. Polyetheretherketone versus titanium CAD-CAM framework for implant-supported fixed complete dentures: A retrospective study with up to 5-year follow-up. J. Prosthodont. Res. 2022, 66, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Desai, S.R.; Koulgikar, K.D.; Alqhtani, N.R.; Alqahtani, A.R.; Alqahtani, A.S.; Alenazi, A.; Heboyan, A.; Fernandes, G.V.O.; Mustafa, M. Three-Dimensional FEA Analysis of the Stress Distribution on Titanium and Graphene Frameworks Supported by 3 or 6-Implant Models. Biomimetics 2023, 8, 15. [Google Scholar] [CrossRef]
- Jemt, T.; Lindén, B. Fixed implant-supported prostheses with welded titanium frameworks. Int. J. Periodontics Restor. Dent. 1992, 12, 177–184. [Google Scholar]
- Jemt, T. Three-dimensional distortion of gold alloy castings and welded titanium frameworks. Measurements of the precision of fit between completed implant prostheses and the master casts in routine edentulous situations. J. Oral Rehabil. 1995, 22, 557–564. [Google Scholar] [CrossRef] [PubMed]
- Jemt, T.; Henry, P.; Linden, B.; Naert, I.; Weber, H.; Bergstrom, C. A comparison of laser-welded titanium and conventional cast frameworks supported by implants in the partially edentulous jaw: A 3-year prospective multicenter study. Int. J. Prosthodont. 2000, 13, 282–288. [Google Scholar]
- Jemt, T.; Henry, P.; Lindén, B.; Naert, I.; Weber, H.; Wendelhag, I. Implant-supported laser-welded titanium and conventional cast frameworks in the partially edentulous jaw: A 5-year prospective multicenter study. Int. J. Prosthodont. 2003, 16, 415–421. [Google Scholar]
- Degidi, M.; Nardi, D.; Piattelli, A. Immediate loading of the edentulous maxilla with a final restoration supported by an intraoral welded titanium bar: A case series of 20 consecutive cases. J. Periodontol. 2008, 79, 2207–2213. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Nardi, D.; Piattelli, A. Immediate rehabilitation of the edentulous mandible with a definitive prosthesis supported by an intraorally welded titanium bar. Int. J. Oral Maxillofac. Implant. 2009, 24, 342–347. [Google Scholar]
- Degidi, M.; Nardi, D.; Piattelli, A. Prospective study with a 2-year follow-up on immediate implant loading in the edentulous mandible with a definitive restoration using intra-oral welding. Clin. Oral Implant. Res. 2010, 21, 379–385. [Google Scholar] [CrossRef]
- Degidi, M.; Nardi, D.; Piattelli, A. Immediate loading of the edentulous maxilla with a definitive restoration supported by an intraorally welded titanium bar and tilted implants. Int. J. Oral Maxillofac. Implant. 2010, 25, 1175–1182. [Google Scholar]
- Degidi, M.; Nardi, D.; Piattelli, A. Immediate definitive rehabilitation of the edentulous patient using an intraorally welded titanium framework: A 3-year prospective study. Quintessence Int. 2010, 41, 651–659. [Google Scholar] [PubMed]
- Avvanzo, P.; Fabrocini, L.A.; Ciavarella, D.; Avvanzo, A.; Lo Muzio, L.; De Maio, R.A. Use of intraoral welding to stabilize dental implants in augmented sites for immediate provisionalization: A case report. J. Oral Implantol. 2012, 38, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Nardi, D.; Piattelli, A.; Malevez, C. Immediate loading of zygomatic implants using the intraoral welding technique: A 12-month case series. Int. J. Periodontics Restor. Dent. 2012, 32, e154–e161. [Google Scholar]
- Al-Fadda, S.A.; Zarb, G.A.; Finer, Y. A comparison of the accuracy of fit of 2 methods for fabricating implant-prosthodontic frameworks. Int. J. Prosthodont. 2007, 20, 125–131. [Google Scholar]
- Svanborg, P.; Stenport, V.; Eliasson, A. Fit of cobalt-chromium implant frameworks before and after ceramic veneering in comparison with CNC-milled titanium frameworks. Clin. Exp. Dent. Res. 2015, 1, 49–56. [Google Scholar] [CrossRef]
- Agliardi, E.L.; Pozzi, A.; Romeo, D.; Del Fabbro, M. Clinical outcomes of full-arch immediate fixed prostheses supported by two axial and two tilted implants: A retrospective cohort study with 12–15 years of follow-up. Clin. Oral Implant. Res. 2023, 34, 351–366. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Labrador, L.; Molinero-Mourelle, P.; Cortes-Breton Brinkmann, J.; Prados-Frutos, J.C.; Gomez-Polo, M.; Martinez-Gonzalez, J.M. Clinical Behavior and Complications of Mandibular Full-Arch Fixed Dental Prostheses Supported by Three Dental Implants. A Systematic Review and Meta-Analysis. Biology 2021, 10, 308. [Google Scholar] [CrossRef] [PubMed]
- Mackert, J.; El-Shewy, M.; Pannu, D.; Schoenbaum, T. Prosthetic complications and survival rates of metal-acrylic implant fixed complete dental prostheses: A retrospective study up to 10 years. J. Prosthet Dent. 2022, 132, 766–771. [Google Scholar] [CrossRef]
- Bozini, T.; Petridis, H.; Garefis, K.; Garefis, P. A meta-analysis of prosthodontic complication rates of implant-supported fixed dental prostheses in edentulous patients after an observation period of at least 5 years. Int. J. Oral Maxillofac. Implant. 2011, 26, 304–318. [Google Scholar]
- Turkyilmaz, I.; Suarez, J.C.; Company, A.M.; McGlumphy, E.A. Early load mandibular hybrid prosthesis using the Ohio State University acrylic frame requiring no final impression. Aust Dent. J. 2009, 54, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Engstrand, P.; Nannmark, U.; Martensson, L.; Galeus, I.; Branemark, P.I. Branemark Novum: Prosthodontic and dental laboratory procedures for fabrication of a fixed prosthesis on the day of surgery. Int. J. Prosthodont. 2001, 14, 303–309. [Google Scholar]
- Henry, P.J.; van Steenberghe, D.; Blomback, U.; Polizzi, G.; Rosenberg, R.; Urgell, J.P.; Wendelhag, I. Prospective multicenter study on immediate rehabilitation of edentulous lower jaws according to the Branemark Novum protocol. Clin. Implant. Dent. Relat. Res. 2003, 5, 137–142. [Google Scholar] [CrossRef]
- Higuchi, K.; Liddelow, G. An Innovative Implant-Supported Treatment for the Edentulous Mandible: Case Report. Int. J. Oral Maxillofac. Implant. 2019, 34, e13–e16. [Google Scholar] [CrossRef] [PubMed]
- Jokstad, A.; Shokati, B. New 3D technologies applied to assess the long-term clinical effects of misfit of the full jaw fixed prosthesis on dental implants. Clin. Oral Implant. Res. 2015, 26, 1129–1134. [Google Scholar] [CrossRef] [PubMed]
- Karl, M.; Taylor, T.D. Bone Adaptation Induced by Non-Passively Fitting Implant Superstructures: A Randomized Clinical Trial. Int. J. Oral Maxillofac. Implant. 2016, 31, 369–375. [Google Scholar] [CrossRef]
- Stumpel, L.J. A prefabricated modular substructure for a 4-implant-supported fixed complete denture: A dental technique. J. Prosthet. Dent. 2020, 124, 637–641. [Google Scholar] [CrossRef] [PubMed]
- Kodama, T. Implant-supported full-mouth reconstruction Malo Implant Bridge. J. Calif. Dent. Assoc. 2012, 40, 497–508. [Google Scholar] [CrossRef]
- Grande, F.; Cesare, P.M.; Mochi Zamperoli, E.; Gianoli, C.M.; Mollica, F.; Catapano, S. Evaluation of Tension and Deformation in a Mandibular Toronto Bridge Anchored on Three Fixtures Using Different Framework Materials, Abutment Systems, and Loading Conditions: A FEM Analysis. Eur. J. Dent. 2023, 17, 1097–1105. [Google Scholar] [CrossRef]
- Scarano, A.; Stoppaccioli, M.; Casolino, T. Zirconia crowns cemented on titanium bars using CAD/CAM: A five-year follow-up prospective clinical study of 9 patients. BMC Oral Health 2019, 19, 286. [Google Scholar] [CrossRef]
- Ayna, M.; Gulses, A.; Acil, Y. A comparative study on 7-year results of “All-on-Four” immediate-function concept for completely edentulous mandibles: Metal-ceramic vs. bar-retained superstructures. Odontology 2018, 106, 73–82. [Google Scholar] [CrossRef]
- Piermatti, J. Using CAD-CAM technology for the full-mouth, fixed, retrievable implant restoration: A clinical report. J. Oral Implantol. 2007, 33, 23–27. [Google Scholar] [CrossRef]
- Bidra, A.S. Complete Arch Monolithic Zirconia Prosthesis Supported By Cobalt Chromium Metal Bar: A Clinical Report. J. Prosthodont. 2020, 29, 558–563. [Google Scholar] [CrossRef] [PubMed]
- Cinquini, C.; Alfonsi, F.; Marchio, V.; Gallo, F.; Zingari, F.; Bolzoni, A.R.; Romeggio, S.; Barone, A. The Use of Zirconia for Implant-Supported Fixed Complete Dental Prostheses: A Narrative Review. Dent. J. 2023, 11, 144. [Google Scholar] [CrossRef] [PubMed]
- Al-Tarawneh, S.; Thalji, G.; Shonberg, D.; Fayz, L.; Cooper, L. Retrospective Cohort Evaluation of Full-Arch Zirconia Implant-Supported Fixed Prostheses. Int. J. Oral Maxillofac. Implant. 2023, 38, 381–390. [Google Scholar] [CrossRef]
- Tirone, F.; Salzano, S.; Rolando, E.; Pozzatti, L.; Rodi, D. Framework Fracture of Zirconia Supported Full Arch Implant Rehabilitation: A Retrospective Evaluation of Cantilever Length and Distal Cross-Sectional Connection Area in 140 Patients Over an Up-To-7 Year Follow-Up Period. J. Prosthodont. 2022, 31, 121–129. [Google Scholar] [CrossRef]
- Acampora, R.; Montanari, M.; Scrascia, R.; Ferrari, E.; Pasi, M.; Cervino, G.; Meloni, S.M.; Lumbau, A.I.; Xhanari, E.; Koshovari, A.; et al. 1-Year Evaluation of OT Bridge Abutments for Immediately Loaded Maxillary Fixed Restorations: A Multicenter Study. Eur. J. Dent. 2021, 15, 290–294. [Google Scholar] [CrossRef] [PubMed]
- Pelekanos, S.; Ntovas, P.; Rizou, V.; Pozzi, A. Translucent monolithic zirconia titanium-supported FP1 full-arch prosthesis: A novel proof of concept to address esthetic, functional, and biologic challenges. J. Esthet. Restor. Dent. 2023, 36, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Revilla-Leon, M.; Barmak, A.B.; Lanis, A.; Kois, J.C. Influence of connected and nonconnected calibrated frameworks on the accuracy of complete arch implant scans obtained by using four intraoral scanners, a desktop scanner, and a photogrammetry system. J. Prosthet. Dent. 2024. [Google Scholar] [CrossRef] [PubMed]
- Mitha, T.; Owen, C.P.; Howes, D.G. The three-dimensional casting distortion of five implant-supported frameworks. Int. J. Prosthodont. 2009, 22, 248–250. [Google Scholar]
- Jemt, T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Brånemark implants in edentulous jaws: A study of treatment from the time of prosthesis placement to the first annual checkup. Int. J. Oral Maxillofac. Implant. 1991, 6, 270–276. [Google Scholar]
- Cappare, P.; Sannino, G.; Minoli, M.; Montemezzi, P.; Ferrini, F. Conventional versus Digital Impressions for Full Arch Screw-Retained Maxillary Rehabilitations: A Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2019, 16, 829. [Google Scholar] [CrossRef]
- Oteiza-Galdón, B.; Martínez-González, A.; Escuder, Á. Analysis of fit on implants of chrome cobalt versus titanium frameworks made by cad/cam milling. J. Clin. Exp. Dent. 2020, 12, e951–e957. [Google Scholar] [CrossRef] [PubMed]
- Dmd, C.S.; Bidra, A.S. Management of Fractured Zirconia Complete Arch Fixed Implant-Supported Prosthesis Caused by Misfit Due to Diverse Implant Components: A Case Report. J. Prosthodont. 2021, 30, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Araújo, G.M.D.; França, D.G.B.D.; Silva Neto, J.P.; Barbosa, G.A.S. Passivity of Conventional and CAD/CAM Fabricated Implant Frameworks. Braz. Dent. J. 2015, 26, 277–283. [Google Scholar] [CrossRef]
- Jemt, T.; Back, T.; Petersson, A. Precision of CNC-milled titanium frameworks for implant treatment in the edentulous jaw. Int. J. Prosthodont. 1999, 12, 209–215. [Google Scholar]
- Tribst, J.P.M.; Dal Piva, A.M.O.; Lo Giudice, R.; Borges, A.L.S.; Bottino, M.A.; Epifania, E.; Ausiello, P. The Influence of Custom-Milled Framework Design for an Implant-Supported Full-Arch Fixed Dental Prosthesis: 3D-FEA Sudy. Int. J. Environ. Res. Public Health 2020, 17, 4040. [Google Scholar] [CrossRef]
- Villefort, R.F.; Tribst, J.P.M.; Dal Piva, A.M.O.; Borges, A.L.; Binda, N.C.; Ferreira, C.E.A.; Bottino, M.A.; von Zeidler, S.L.V. Stress distribution on different bar materials in implant-retained palatal obturator. PLoS ONE 2020, 15, e0241589. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; Dal Piva, A.M.D.O.; Borges, A.L.S.; Rodrigues, V.A.; Bottino, M.A.; Kleverlaan, C.J. Does the prosthesis weight matter? 3D finite element analysis of a fixed implant-supported prosthesis at different weights and implant numbers. J. Adv. Prosthodont. 2020, 12, 67. [Google Scholar] [CrossRef]
- Alwade, F.H.; Ismail, I.J.; Ibrahim, F.J. Zirconia in dental and other biomedical applications: An overview. Int. J. Med. Res. Health Sci. 2019, 8, 30–37. [Google Scholar]
- Hoque, M.E.; Showva, N.N.; Ahmed, M.; Rashid, A.B.; Sadique, S.E.; El-Bialy, T.; Xu, H. Titanium and titanium alloys in dentistry: Current trends, recent developments, and future prospects. Heliyon 2022, 8, e11300. [Google Scholar] [CrossRef]
- Bhaskaran, E.; Azhagarasan, N.S.; Miglani, S.; Ilango, T.; Krishna, G.P.; Gajapathi, B. Comparative Evaluation of Marginal and Internal Gap of Co-Cr Copings Fabricated from Conventional Wax Pattern, 3D Printed Resin Pattern and DMLS Tech: An In Vitro Study. J. Indian Prosthodont. Soc. 2013, 13, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Limmer, B.; Sanders, A.E.; Reside, G.; Cooper, L.F. Complications and patient-centered outcomes with an implant-supported monolithic zirconia fixed dental prosthesis: 1 year results. J. Prosthodont. 2014, 23, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, J.; Triplett, R.G. Complications and Clinical Considerations of the Implant-Retained Zirconia Complete-Arch Prosthesis with Various Opposing Dentitions. Int. J. Oral Maxillofac. Implant. 2017, 32, 864–869. [Google Scholar] [CrossRef]
- Mesquita, A.M.M.; Al-Haj Husain, N.; Molinero-Mourelle, P.; Ozcan, M. An Intraoral Repair Method for Chipping Fracture of a Multi-unit Fixed Zirconia Reconstruction: A Direct Dental Technique. Eur. J. Dent. 2021, 15, 174–178. [Google Scholar] [CrossRef] [PubMed]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Froimovici, F.-O.; Butnărașu, C.C.; Montanari, M.; Săndulescu, M. Fixed Full-Arch Implant-Supported Restorations: Techniques Review and Proposal for Improvement. Dent. J. 2024, 12, 408. https://doi.org/10.3390/dj12120408
Froimovici F-O, Butnărașu CC, Montanari M, Săndulescu M. Fixed Full-Arch Implant-Supported Restorations: Techniques Review and Proposal for Improvement. Dentistry Journal. 2024; 12(12):408. https://doi.org/10.3390/dj12120408
Chicago/Turabian StyleFroimovici, Florin-Octavian, Cristian Corneliu Butnărașu, Marco Montanari, and Mihai Săndulescu. 2024. "Fixed Full-Arch Implant-Supported Restorations: Techniques Review and Proposal for Improvement" Dentistry Journal 12, no. 12: 408. https://doi.org/10.3390/dj12120408
APA StyleFroimovici, F.-O., Butnărașu, C. C., Montanari, M., & Săndulescu, M. (2024). Fixed Full-Arch Implant-Supported Restorations: Techniques Review and Proposal for Improvement. Dentistry Journal, 12(12), 408. https://doi.org/10.3390/dj12120408




