Health Coaching-Based Interventions for Oral Health Promotion: A Scoping Review
Abstract
1. Introduction
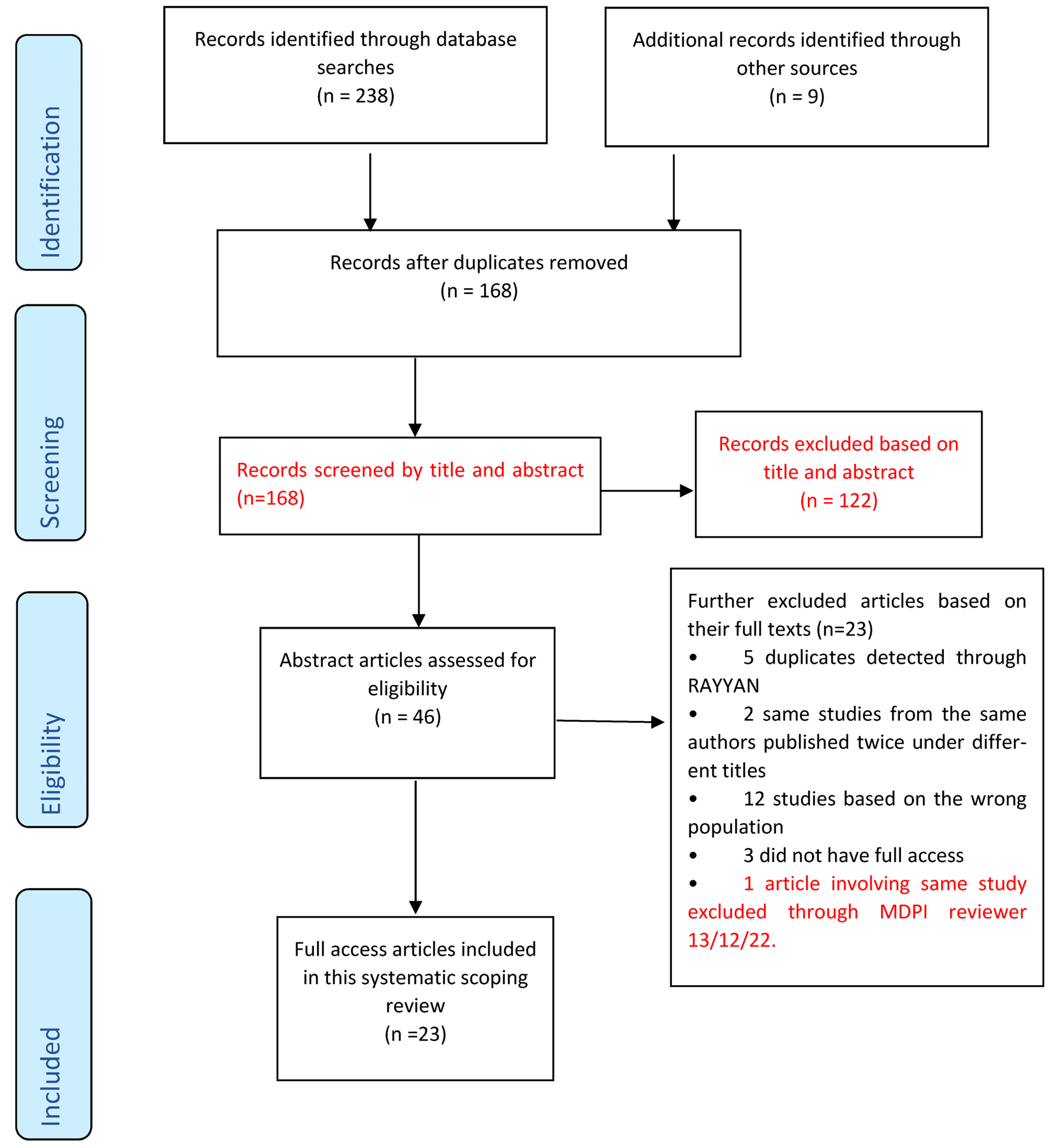
2. Materials and Methods
- Population: Adult patients aged 18 years or over.
- Concept: Health coaching-based interventions for oral health promotion
- Context: Community and clinical settings
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Data Selection
2.4. Quality Assessment, Data Charting and Synthesis
| Type of Study | JBI Critical Appraisal Checklist Questions Used |
|---|---|
| Systematic reviews and research syntheses |
|
| Randomised Control Trials |
|
| Quasi-experimental/Interventional Studies |
|
| Type of Study | Study | Quality |
|---|---|---|
| RCT | Godard et al. [30] | Medium |
| RCT | Stenman et al. [31] | High |
| RCT | López-Jornet et al. [32] | High |
| Systematic Review and Research Syntheses | Cascaes et al. [33] | Medium |
| RCT | Brand et al. [34] | High |
| Quasi-experimental/Interventional study | Johansson et al. [35] | High |
| Quasi-experimental/Interventional study | Saengtipbovorn and Taneepanichskul [36] | High |
| Systematic Review and Research Syntheses | Yevlahova and Satur [37] | High |
| Quasi-experimental/Interventional study | Tellez et al. [38] | Medium |
| Systematic Review and Research Syntheses | Kay et al. [1] | High |
| Systematic Review and Research Syntheses | Gao et al. [39] | High |
| RCT | Naidu et al. [40] | High |
| Quasi-experimental/Interventional study | Cinar et al. [13] | High |
| Quasi-experimental/Interventional study | Dermen et al. [41] | High |
| Systematic Review and Research Syntheses | Werner et al. [2] | High |
| RCT | Tellez et al. [42] | High |
| RCT | Stenman et al. [43] | High |
| RCT | Jönsson et al. [44] | High |
| RCT | Alrashdi et al. [45] | High |
| Systematic Review and Research Syntheses | Watt [46] | Low |
| Quasi-experimental/Interventional study | Cinar et al. [47] | High |
| RCT | Rigau-Gay et al. [48] | High |
| Systematic Review and Research Syntheses | Antoniadou and Varzakas [49] | Low |
| Author(s) | Year | Country of Origin | Aim | Study Sample | Method | Intervention | Key Finding |
|---|---|---|---|---|---|---|---|
| Godard, Dufour, Jeanne [30] | 2011 | France | To assess the effectiveness of MI vs. Conventional basic instruction on compliance with plaque control and periodontitis | N = 51 patients | Quantitative | MI on OH improvement | MI can be used to target and modify inappropriate behaviour and can be implemented into a periodontal treatment plan |
| Stenman, Wennström, Abrahamsson [31] | 2018 | Sweden | To evaluate whether a single MI session can influence periodontal therapy. Evaluate retention of OH behaviours | N = 26 patients | Quantitative | Single session MI on periodontal health | A single MI session could not be proven to be of the long-term beneficial additive effect regarding prevention of relapse in oral hygiene behaviour |
| Naidu, Nunn, Irwin, [40] | 2015 | Trinidad | To compare MI to oral health education on oral health knowledge, attitudes, beliefs and behaviours | N = 79 parents and caregivers | Quantitative | Compare MI to traditional HE, behaviours | Use of MI during oral health information giving session had positive effect on parent/caregiver oral health knowledge, attitudes and behaviours compared to traditional oral health education. |
| Alrashdi, Hameed, Mendez, Farokhi [45] | 2020 | USA | To assess the effectiveness of oral health education and behavioural intervention on improving knowledge, attitudes and behaviours of refugee families using MI. | N = 66 parents | Quantitative | Behaviour change, MI oral health improvement | Behavioural intervention with oral health education did not improve oral health-related knowledge, attitudes, or behaviours in a diverse group of recent refugee families. |
| López-Jornet, Fabio, Consuelo, Paz [32] | 2014 | Spain | To assess the effectiveness of MI-behavioral skills for plaque control in patients with hyposalivation | N = 60 patients | Quantitative | Oral hygiene practices, MI, OH improvement | In patients with hyposalivation, application of OHI based on cognitive principles and MI offers benefits for periodontal health |
| Cascaes, Bielemann, Clark, Barros [33] | 2014 | Brazil | To analyse the effectiveness of MI at improving oral hygiene habits | N = 78 articles | Systematic Review | MI, OH improvement | More research needed to fully understand the impact of MI on oral health and understand counselling interventions. |
| Cinar, Oktay, Schou [47] | 2014 | Turkey | To evaluate the impact of HC compared to health education on oral health and diabetes management among patients with type 2 Diabetes | N = 186 patients | Quantitative | Compare health education to health coaching on oral health improvement and behaviour change | HC has a significantly higher impact on better management of diabetes and oral health when compared to formal health education. |
| Brand, Bray, MacNeill, Catley, Williams [34] | 2013 | USA | To evaluate whether brief MI is effective in improving internal motivation for oral hygiene behaviour. | N = 56 patients | Quantitative | Single session MI on oral hygiene behaviour change and internal motivation | One-time MI session is insufficient for improving oral hygiene in long-standing maintenance patients. |
| Johansson, Torge, Lindmark [35] | 2020 | Sweden | To examine the feasibility of HC in a nursing home to improve oral health care | N = 106 nursing home staff and residents | Quantitative | HC on oral health improvement | HC can support nursing staff in maintaining a high level of oral health among residents. |
| Saengtipbovorn, Taneepanichskul [36] | 2015 | Thailand | To assess if Lifestyle Change plus Dental Care can improve oral health knowledge, attitude and practice in diabetic patients | N = 132 patients | Quantitative | Oral hygiene practices, MI, behaviour change and oral health improvement | A combination of lifestyle change with dental care improves knowledge, attitude and practice toward oral health and diabetes mellitus in the elderly with Type 2 Diabetes |
| Yevlahova, Satur [37] | 2009 | Australia | To identify and assess the effectiveness of behaviour models as a basis for individual oral health promotion | N = 32 studies | Systematic Review | MI, behaviour change and oral health improvement | There is a need to develop an effective model for chairside oral health promotion. MI has the potential to be developed within the oral health field |
| Tellez, Virtue, Neckritz, Bhoopathi, Hernández, Shearer [38] | 2019 | USA | To examine fidelity of individual MI intervention and assess baseline characteristics related to older adults’ self-efficacy oral health-related quality of life | N = 60 patients | Quantitative | Tailored MI and OHWs | Findings from the study support the reliability of one-on-one MI intervention for conducting oral health education |
| Kay, Vascott, Hocking, Nield [1] | 2016 | UK | To review evidence regarding the use of MI in general dental practice so practitioners can decide whether it might be an important skill to develop within their practices. | N = 20 studies | Systematic Review | oral health workers, MI as a skill for professionals | MI based on the concept of autonomy support has potential for helping patients with poor oral health. MI training for dental personnel could be a beneficial skill. |
| Gao, Lo, Kot, Chan [39] | 2014 | China | To synthesise the evidence on the effectiveness of MI compared with conventional (health) education (CE) in improving oral health | N = 221 records | Systematic Review | MI vs. standard HE in oral health improvement | MI shows varied success in improving oral health. Potential of MI in dental health care, like improving periodontal health, remains controversial. Additional studies are needed to understand the role of dental practice on a bigger scale. |
| Watt [46] | 2010 | UK | To identify models for health behaviour, change and to evaluate evidence for their effectiveness | N = 32 studies | Narrative Review | MI and Dental Setting | MI interventions were found to be the most effective method for altering health behaviours in a clinical setting. |
| Cinar, Freeman and Schou [13] | 2018 | Turkey & Denmark | To assess the effectiveness of HC vs. health education using clinical and type 2 diabetes patients in Turkey and Denmark. | 302 patients N = 186 participants Turkey N = 116 participants Denmark | Quantitative | HC on Behaviour change | HC has a greater impact on type 2 diabetes management |
| Dermen, Ciancio, Fabiano [41] | 2014 | USA | To provide initial evidence that, compared with a didactic control intervention, a brief MI-based intervention (BMI) delivered by dental practitioners can yield greater oral health improvements | N = 60 in-patients | Quantitative | Brief MI on OH | A brief intervention using MI methods can be delivered by dental professionals and has potential utility for promoting improved oral hygiene. |
| Werner, Hakeberg, Dahlström, Eriksson, Sjögren, Strandell, Svanberg, Svensson, Boman [2] | 2016 | Sweden | To study the effectiveness of psychological interventions in adults and adolescents with poor oral health | N = 843 articles in 2013 N = 378 articles in 2015 | Systematic review | MI on oral hygiene practices | Statistically significant differences reported in favour of psychological interventions in oral health behaviour and self-efficacy in toothbrushing. |
| Tellez, Myers Virtue, Neckritz, Lim, Bhoopathi, Hernandez, Ismail [42] | 2020 | USA | To assess the treatment fidelity of an individual-based oral health education intervention using MI compared to group-based oral health education | N = 180 patients | Quantitative | Tailored MI compared to HE | This study supports the fidelity of this intervention and the improvement of all non-clinical outcomes after 12 months amongst the MI group |
| Stenman, Lundgren, Wennström, Ericsson, Abrahamsson, [43] | 2012 | Sweden | To evaluate the effect of a single session of MI on self-performed periodontal infection control. | N = 44 patients | Quantitative | Single session MI on improving periodontal infection control | A single freestanding MI session had no significant effect on the individuals’ standard of self-performed periodontal infection control in a short-term perspective. |
| Jönsson, Öhrn, Lindberg, Oscarson [44] | 2010 | Sweden | To evaluate the effectiveness of individually tailored oral health education compared with standard oral health education on periodontal health. | N = 113 patients | Quantitative | Individually tailored oral health education using MI on periodontal health improvement | An individually tailored oral health educational program intervention, in combination with scaling is preferable to the standard oral hygiene education in non-surgical periodontal treatment. |
| Rigau-Gay, Claver-Garrido, Benet, Lusilla-Palacios, Ustrell-Torrent [48] | 2020 | Spain | To evaluate the effectiveness of a single session of MI on enhancing oral hygiene among orthodontic patients compared with conventional education alone | N = 130 patients | Quantitative | Single session MI with orthodontic patients | Short time-MI combined with conventional education is useful to improve oral hygiene, since it decreases plaque and gingival indexes, in adolescents and young adults wearing fixed appliances. |
| Antoniadou, Varzakas [49] | 2020 | Greece | To identify diet and oral health coaching methods and models for the independent elderly | N/A | Narrative Review | HC on diet and oral health/dietary habits | Dental and other medical professionals should re-evaluate their roles as health coaches to improve dietary habits and nutritional intake of their patients |
| Study | Recommendations | Themes/Characteristics |
|---|---|---|
| Werner et al. [2] | Interventions may be used if benefits and risks, cost-effectiveness and ethical aspects are considered |
|
| Tellez et al. [42] | Training, dental personnel on MI approach would make it a powerful alternative particularly in settings where there are no dentists. |
|
| Stenman et al. [43] | Dental professionals should learn how to motivate the patients. MI should be added to traditional health education methods. |
|
| Jönsson et al. [44] | Non-surgical periodontal treatment is achieved through individually tailored oral health communication. The treatment programme is possible for special trained dental hygienists to perform in their treatment of patients with chronic periodontitis. |
|
| Alrashdi et al. [45] | Health education should be supplemented with other interventions to achieve positive oral health outcomes |
|
| Cinar et al. [47] | Training of health professionals Engagement of health workers and their patients on the behaviour change journey |
|
| Rigau-Gay et al. [48] | Training dental hygienists as part of the working team to become experts in MI focused on dental settings could be useful, for self-empowerment and motivation. |
|
| Antoniadou & Varzakas [49] | Quick health education sessions followed by tailored feedback using empathy is important in terms of helping elderly adults in improving their oral health. Health professionals should re-evaluate their role as health coaches. |
|
| Dermen et al. [41] | A brief MI intervention delivered by dental professionals is feasible and efficacious than didactic methods. |
|
| Cinar et al. [13] | There is a need for health promotion strategies with health coaching for the management of type 2 diabetes that focus on multidisciplinary approaches including oral health. The study highlights the importance of (i) training of health professionals on HC and (ii) patient-health professional collaboration. |
|
| Watt [46] | There is potential to further develop the MI approach within the oral health field. |
|
| Gao et al. [39] | A growing interest of dental professionals in MI and suggests some the potential of applying MI in oral health |
|
| Kay et al. [1] | Build relationships between OHPs and patients. Training of OHPs in MI techniques. Avoidance of negative judgements |
|
| Tellez et al. [38] | MI is reliable for HE. Engaging patients with a menu of options rather than a prescribed checklist |
|
| Yevlahova & Satur [37] | MI has the potential to be developed within the oral health field. |
|
| Saruta Saengtipbovorn & Taneepanichskul [36] | Knowledge and education are essential for engaging clients in making behaviour or lifestyle change |
|
| Johansson et al. [35] | Extended support from dental care, including practical training and feedback on an individual basis, could benefit nursing staff in providing oral health care |
|
| Brand et al. [34] | Adoption of MI in dental and dental hygiene education. Adopt evidence-based patient-engagement strategies. |
|
| Cascaes et al. [33] | Beneficial effects of MI conducted individually in clinical settings. MI appears to be a promising approach for changing individual behaviour |
|
| López-Jornet et al. [32] | Dental professionals must provide instructions on oral hygiene, education and information and identify obstacles to behavioural improvement |
|
| Naidu et al. [40] | MI approach had a positive effect compared to traditional health education. Development of the person-centred counselling approach |
|
| Stenman et al. [31] | A single MI session does not add beneficial effects to standard periodontal therapy for efficient oral hygiene behaviour |
|
| Godard et al. [30] | Dentists are recommended to start using MI. This procedure could be applied in similar clinical settings when the patient’s active role is crucial to treatment success. |
|
3. Results
3.1. Study Characteristics
3.2. Key Findings in Relation to Characteristics/Themes
3.2.1. Engage Clients or Patients and Avoid Negative Feedback and Criticism
3.2.2. Supplement Traditional Health Education Methods with Tailored Communication
3.2.3. Introduce Brief Routine MI/HC Sessions
3.2.4. Train Health Professionals to Provide MI/HC in Clinical Settings
3.2.5. Cost-Effectiveness of MI/HC Strategies
4. Discussion
4.1. Engage Clients or Patients and Avoid Negative Feedback and Criticism
4.2. Supplement Traditional Health Education Methods with Tailored Communication
4.3. Introduce Brief Routine MI/HC Sessions
4.4. Train Health Professionals to Provide MI/HC in Clinical Settings
4.5. Cost-Effectiveness for MI/HC Strategies
4.6. Research Gaps
- I.
- No paper or article included in this review addressed the role of organisational, regulatory, fiscal, or legislation as factors directly influencing interventions and oral health delivery and outcomes.
- II.
- There is a limited number of studies using the design of randomised controlled trials [30,31,32,34,40,42,43,44,45,48] showing varied success of the interventions in improving oral health. However, more studies with methodological rigor targeting at various age groups and behaviours are required to better understand their roles in oral disease management.
- III.
- IV.
- Only two studies addressed the role of plaque control measures, such as toothbrushing in improving oral health outcomes and oral health behaviour change [32,47]. López-Jornet et al. [32] showed how the frequency and use of interproximal brushing affect plaque and bleeding indices, while Cinar et al. [47] explored how toothbrushing efficacy and frequency affect oral health and quality of life among patients with type 2 diabetes.
4.7. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kay, E.J.; Vascott, D.; Hocking, A.; Nield, H. Motivational interviewing in general dental practice: A review of the evidence. Br. Dent. J. 2016, 221, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Werner, H.; Hakeberg, M.; Dahlström, L.; Eriksson, M.; Sjögren, P.; Strandell, A.; Svanberg, T.; Svensson, L.; Wide Boman, U. Psychological interventions for poor oral health: A systematic review. J. Dent. Res. 2016, 95, 506–514. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. Motivational Interviewing: Helping People Change; Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Nakre, P.D.; Harikiran, A.G. Effectiveness of oral health education programs: A systematic review. J. Int. Soc. Prev. Community Dent. 2013, 3, 103. [Google Scholar] [CrossRef] [PubMed]
- Vernon, L.T.; Howard, A.R. Advancing health promotion in dentistry: Articulating an integrative approach to coaching oral health behavior change in the dental setting. Curr. Oral Health Rep. 2015, 2, 111–122. [Google Scholar] [CrossRef] [PubMed]
- NHS Health Coaching Implementation and Quality Summary Guide. Available online: https://www.england.nhs.uk/wp-content/uploads/2020/03/health-coaching-implementation-and-quality-summary-guide.pdf (accessed on 11 November 2022).
- Olsen, J.M. Health coaching: A concept analysis. In Nursing Forum; Wiley: Hoboken, NJ, USA, 2014; Volume 49, pp. 18–29. [Google Scholar]
- Croffoot, C.; Bray, K.K.; Black, M.A.; Koerber, A. Evaluating the effects of coaching to improve motivational interviewing skills of dental hygiene students. Am. Dent. Hyg. Assoc. 2010, 84, 57–64. [Google Scholar]
- Sharon, C.; Trace, A.; Ziada, H. Motivational Interviewing for Dental Clinicians; Irish Dental Association: Dublin, Ireland, 2014. [Google Scholar]
- Miller, W.R.; Moyers, T.B. Motivational interviewing and the clinical science of Carl Rogers. J. Consult. Clin. Psychol. 2017, 85, 757. [Google Scholar] [CrossRef]
- Watson, M.C.; Ferguson, J.; Barton, G.R.; Maskrey, V.; Blyth, A.; Paudyal, V.; Bond, C.M.; Holland, R.; Porteous, T.; Sach, T.H.; et al. A cohort study of influences, health outcomes and costs of patients’ health-seeking behaviour for minor ailments from primary and emergency care settings. BMJ Open 2015, 5, e006261. [Google Scholar] [CrossRef]
- Shrivastava, R.; Couturier, Y.; Kadoch, N.; Girard, F.; Bedos, C.; Macdonald, M.E.; Torrie, J.; Emami, E. Patients’ perspectives on integrated oral healthcare in a northern Quebec Indigenous primary health care organisation: A qualitative study. BMJ Open 2019, 9, e030005. [Google Scholar] [CrossRef]
- Cinar, A.B.; Freeman, R.; Schou, L. A new complementary approach for oral health and diabetes management: Health coaching. Int. Dent. J. 2018, 68, 54–64. [Google Scholar] [CrossRef]
- Scott, R.E.; Mars, M. Behaviour change and e-health–Looking broadly: A scoping narrative review. Stud. Health Technol. Inform. 2020, 268, 123–138. [Google Scholar]
- Linden, A.; Butterworth, S.W.; Prochaska, J.O. Motivational interviewing-based health coaching as a chronic care intervention. J. Eval. Clin. Pract. 2010, 16, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Oksman, E.; Linna, M.; Hörhammer, I.; Lammintakanen, J.; Talja, M. Cost-effectiveness analysis for a tele-based health coaching program for chronic disease in primary care. BMC Health Serv. Res. 2017, 17, 138. [Google Scholar] [CrossRef] [PubMed]
- Neuner-Jehle, S.; Schmid, M.; Grüninger, U. The “Health Coaching” programme: A new patient-centred and visually supported approach for health behaviour change in primary care. BMC Fam. Pract. 2013, 14, 100. [Google Scholar] [CrossRef] [PubMed]
- Gillam, D.G.; Yusuf, H. Brief motivational interviewing in dental practice. Dent. J. 2019, 7, 51. [Google Scholar] [CrossRef] [PubMed]
- Randall, C.L. On motivational interviewing for oral health promotion: State of the field and future directions. JDR Clin. Transl. Res. 2018, 3, 376–377. [Google Scholar] [CrossRef]
- Harrison, R. Motivational interviewing (MI) compared to conventional education (CE) has potential to improving oral health behaviors. J. Evid. Based Dent. Pract. 2014, 14, 124–126. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- JBI Manual for Evidence Synthesis. Available online: https://jbi-global-wiki.refined.site/space/MANUAL/4687579/Appendix+11.1+JBI+template+source+of+evidence+details%2C+characteristics+and+results+extraction+instrument (accessed on 12 November 2022).
- Pham, M.T.; Rajić, A.; Greig, J.D.; Sargeant, J.M.; Papadopoulos, A.; McEwen, S.A. A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Res. Synth. Methods 2014, 5, 371–385. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.; Colquhoun, H.; Kastner, M.; Levac, D.; Ng, C.; Sharpe, J.P.; Wilson, K.; et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med. Res. Methodol. 2016, 16, 15. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Anderson, S.; Allen, P.; Peckham, S.; Goodwin, N. Asking the right questions: Scoping studies in the commissioning of research on the organisation and delivery of health services. Health Res. Policy Syst. 2008, 6, 7. [Google Scholar] [CrossRef]
- JBI Critical Appraisal Tools. Available online: https://jbi.global/critical-appraisal-tools (accessed on 30 December 2022).
- Godard, A.; Dufour, T.; Jeanne, S. Application of self-regulation theory and motivational interview for improving oral hygiene: A randomized controlled trial. J. Clin. Periodontol. 2011, 38, 1099–1105. [Google Scholar] [CrossRef]
- Stenman, J.; Wennström, J.L.; Abrahamsson, K.H. A brief motivational interviewing as an adjunct to periodontal therapy—A potential tool to reduce relapse in oral hygiene behaviours. A three-year study. Int. J. Dent. Hyg. 2018, 16, 298–304. [Google Scholar] [CrossRef]
- López-Jornet, P.; Fabio, C.A.; Consuelo, R.A.; Paz, A.M. Effectiveness of a motivational–behavioural skills protocol for oral hygiene among patients with hyposalivation. Gerodontology 2014, 31, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Cascaes, A.M.; Bielemann, R.M.; Clark, V.L.; Barros, A.J. Effectiveness of motivational interviewing at improving oral health: A systematic review. Rev. Saude Publica 2014, 48, 142–153. [Google Scholar] [CrossRef] [PubMed]
- Brand, V.S.; Bray, K.K.; MacNeill, S.; Catley, D.; Williams, K. Impact of single-session motivational interviewing on clinical outcomes following periodontal maintenance therapy. Int. J. Dent. Hyg. 2013, 11, 134–141. [Google Scholar] [CrossRef]
- Johansson, I.; Torgé, C.J.; Lindmark, U. Is an oral health coaching programme a way to sustain oral health for elderly people in nursing homes? A feasibility study. Int. J. Dent. Hyg. 2020, 18, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Saruta Saengtipbovorn, D.D.; Taneepanichskul, S. Lifestyle Change Plus Dental Care (LCDC) program improves knowledge, attitude, and practice (KAP) toward oral health and diabetes mellitus among the elderly with type 2 diabetes. J. Med. Assoc. Thail. 2015, 98, 279–290. [Google Scholar]
- Yevlahova, D.; Satur, J. Models for individual oral health promotion and their effectiveness: A systematic review. Aust. Dent. J. 2009, 54, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Tellez, M.; Myers Virtue, S.; Neckritz, S.; Bhoopathi, V.; Hernández, M.; Shearer, B. Motivational interviewing, and oral health education: Experiences from a sample of elderly individuals in North and Northeast Philadelphia. Spec. Care Dent. 2019, 39, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Lo, E.C.; Kot, S.C.; Chan, K.C. Motivational interviewing in improving oral health: A systematic review of randomized controlled trials. J. Periodontol. 2014, 85, 426–437. [Google Scholar] [CrossRef] [PubMed]
- Naidu, R.; Nunn, J.; Irwin, J.D. The effect of motivational interviewing on oral healthcare knowledge, attitudes and behaviour of parents and caregivers of preschool children: An exploratory cluster randomised controlled study. BMC Oral Health 2015, 15, 101. [Google Scholar] [CrossRef]
- Dermen, K.H.; Ciancio, S.G.; Fabiano, J.A. A pilot test of motivational oral health promotion with alcohol-dependent inpatients. Health Psychol. 2014, 33, 392. [Google Scholar] [CrossRef]
- Tellez, M.; Myers Virtue, S.; Neckritz, S.; Lim, S.; Bhoopathi, V.; Hernandez, M.; Shearer, B.; Ismail, A. Randomised clinical trial of a motivational interviewing intervention to improve oral health education amongst older adults in Philadelphia: 12-month evaluation of non-clinical outcomes. Gerodontology 2020, 37, 279–287. [Google Scholar] [CrossRef]
- Stenman, J.; Lundgren, J.; Wennström, J.L.; Ericsson, J.S.; Abrahamsson, K.H. A single session of motivational interviewing as an additive means to improve adherence in periodontal infection control: A randomized controlled trial. J. Clin. Periodontol. 2012, 39, 947–954. [Google Scholar] [CrossRef]
- Jönsson, B.; Öhrn, K.; Lindberg, P.; Oscarson, N. Evaluation of an individually tailored oral health educational programme on periodontal health. J. Clin. Periodontol. 2010, 37, 912–919. [Google Scholar] [CrossRef]
- Alrashdi, M.; Hameed, A.; Cervantes Mendez, M.J.; Farokhi, M. Education intervention with respect to the oral health knowledge, attitude, and behaviours of refugee families: A randomized clinical trial of effectiveness. J. Public Health Dent. 2021, 81, 90–99. [Google Scholar] [CrossRef]
- Watt, R.G. Motivational interviewing may be effective in dental setting. Evid.-Based Dent. 2010, 11, 13. [Google Scholar] [CrossRef]
- Cinar, A.B.; Oktay, I.; Schou, L. “Smile healthy to your diabetes”: Health coaching-based intervention for oral health and diabetes management. Clin. Oral Investig. 2014, 18, 1793–1801. [Google Scholar] [CrossRef]
- Rigau-Gay, M.M.; Claver-Garrido, E.; Benet, M.; Lusilla-Palacios, P.; Ustrell-Torrent, J.M. Effectiveness of motivational interviewing to improve oral hygiene in orthodontic patients: A randomized controlled trial. J. Health Psychol. 2020, 25, 2362–2373. [Google Scholar] [CrossRef] [PubMed]
- Antoniadou, M.; Varzakas, T. Diet and Oral Health Coaching Methods and Models for the Independent Elderly. Appl. Sci. 2020, 10, 4021. [Google Scholar] [CrossRef]
- Wong-Rieger, D.; Rieger, F.P. Health coaching in diabetes: Empowering patients to self-manage. Can. J. Diabetes 2013, 37, 41–44. [Google Scholar] [CrossRef]
- Freeman, R. Strategies for motivating the non-compliant patient. Br. Dent. J. 1999, 187, 307–312. [Google Scholar] [CrossRef]
- Carter, A.; Tamkin, P.; Wilson, S.; Miller, L. The Case for Health Coaching. Lessons Learned from Implementing a Training and Development Intervention for Clinicians across the East of England; Institute for Employment Studies: Brighton, UK, 2015. [Google Scholar]
- Wanyonyi, K.L.; Themessl-Huber, M.; Humphris, G.; Freeman, R. A systematic review and meta-analysis of face-to-face communication of tailored health messages: Implications for practice. Patient Educ. Couns. 2011, 85, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Williams, K. Motivational interviewing: Application to oral health behaviours. Am. Dent. Hyg. Assoc. 2010, 84, 6–10. [Google Scholar]
- Kopp, S.L.; Ramseier, C.A.; Ratka-Krüger, P.; Woelber, J.P. Motivational interviewing as an adjunct to periodontal therapy—A systematic review. Front. Psychol. 2017, 8, 279. [Google Scholar] [CrossRef]
- Olsen, J.M.; Nesbitt, B.J. Health coaching to improve healthy lifestyle behaviours: An integrative review. Am. J. Health Promot. 2010, 25, e1–e12. [Google Scholar] [CrossRef]
- Kivelä, K.; Elo, S.; Kyngäs, H.; Kääriäinen, M. The effects of health coaching on adult patients with chronic diseases: A systematic review. Patient Educ. Couns. 2014, 97, 147–157. [Google Scholar] [CrossRef]
- Söderlund, L.L.; Madson, M.B.; Rubak, S.; Nilsen, P. A systematic review of motivational interviewing training for general health care practitioners. Patient Educ. Couns. 2011, 84, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Hale, R.; Giese, J. Cost-effectiveness of health coaching. Prof. Case Manag. 2017, 22, 228–238. [Google Scholar] [CrossRef] [PubMed]
- Satre, D.D.; Parthasarathy, S.; Young-Wolff, K.C.; Meacham, M.C.; Borsari, B.; Hirschtritt, M.E.; Van Dyke, L.; Sterling, S.A. Cost-effectiveness of motivational interviewing to reduce alcohol and cannabis use among patients with depression. J. Stud. Alcohol Drugs 2022, 83, 662–671. [Google Scholar] [CrossRef] [PubMed]
| PCC Framework | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Participants | Adult patients aged 18 years or over | Studies including children, or those with cognitive impairments. |
| Concept | Interventions that have a component of oral health improvement using health coaching (HC) or motivational interviewing (MI) techniques to encourage participants’ oral health behaviour or lifestyle change. | Interventions with no oral health promotion elements or no communication techniques to support participants in oral health-related behaviour change. |
| Context | Community and clinical settings | Studies not based on community/clinical settings |
| Language | English | Non-English |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chunda, R.; Mossey, P.; Freeman, R.; Yuan, S. Health Coaching-Based Interventions for Oral Health Promotion: A Scoping Review. Dent. J. 2023, 11, 73. https://doi.org/10.3390/dj11030073
Chunda R, Mossey P, Freeman R, Yuan S. Health Coaching-Based Interventions for Oral Health Promotion: A Scoping Review. Dentistry Journal. 2023; 11(3):73. https://doi.org/10.3390/dj11030073
Chicago/Turabian StyleChunda, Remus, Peter Mossey, Ruth Freeman, and Siyang Yuan. 2023. "Health Coaching-Based Interventions for Oral Health Promotion: A Scoping Review" Dentistry Journal 11, no. 3: 73. https://doi.org/10.3390/dj11030073
APA StyleChunda, R., Mossey, P., Freeman, R., & Yuan, S. (2023). Health Coaching-Based Interventions for Oral Health Promotion: A Scoping Review. Dentistry Journal, 11(3), 73. https://doi.org/10.3390/dj11030073







