Clinicoradiopathologic Analysis of Odontomas: A Retrospective Study of 242 Cases
Abstract
:1. Introduction
2. Materials and Methods
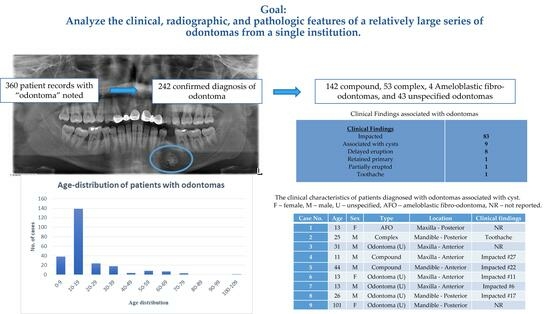
3. Results
3.1. Clinical, Radiographic, and Pathologic Characteristics
3.2. Types of Odontoma
3.2.1. Compound Odontoma
3.2.2. Complex Odontoma
3.2.3. Ameloblastic Fibro-Odontoma
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Regezi, J.A.; Kerr, D.A.; Courtney, R.M. Odontogenic tumors: Analysis of 706 cases. J. Oral Surg. 1978, 36, 771–778. [Google Scholar] [PubMed]
- Buchner, A.; Merrell, P.W.; Carpenter, W.M. Relative frequency of central odontogenic tumors: A study of 1088 cases from Northern California and comparison to studies from other parts of the world. J. Oral Maxillofac. Surg. 2006, 64, 1343–1352. [Google Scholar] [CrossRef] [PubMed]
- Daley, T.D.; Wysocki, G.P.; Pringle, G.A. Relative incidence of odontogenic tumors and oral and jaw cysts in a Canadian population. Oral Surg. Oral Med. Oral Pathol. 1994, 77, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Chrysomali, E.; Leventis, M.; Titsinides, S.; Kyriakopoulos, V.; Sklavounou, A. Odontogenic tumors. J. Craniofac. Surg. 2013, 24, 1521–1525. [Google Scholar] [CrossRef]
- Kokubun, K.; Yamamoto, K.; Nakajima, K.; Akashi, Y.; Chujo, T.; Takano, M.; Katakura, A.; Matsuzaka, K. Frequency of Odontogenic Tumors: A Single Center Study of 1089 Cases in Japan and Literature Review. Head Neck Pathol. 2022, 16, 494–502. [Google Scholar] [CrossRef]
- Aregbesola, B.; Soyele, O.; Effiom, O.; Gbotolorun, O.; Taiwo, O.; Amole, I. Odontogenic tumours in Nigeria: A multicentre study of 582 cases and review of the literature. Med. Oral Patol. Oral Cir. Bucal 2018, 23, e761–e766. [Google Scholar] [CrossRef]
- Nalabolu, G.R.K.; Mohiddin, A.; Hiremath, S.K.S.; Manyam, R.; Bharath, T.S.; Raju, P.R. Epidemiological study of odontogenic tumours: An institutional experience. J. Infect. Public Health 2017, 10, 324–330. [Google Scholar] [CrossRef]
- Ismail, S.; Saw, C.L. A clinicopathologic study of 173 odontogenic tumours in Northern Peninsular Malaysia (2007–2014). Malays. J. Pathol. 2018, 40, 129–135. [Google Scholar]
- Siriwardena, B.S.; Tennakoon, T.M.; Tilakaratne, W.M. Relative frequency of odontogenic tumors in Sri Lanka: Analysis of 1677 cases. Pathol. Res. Pract. 2012, 208, 225–230. [Google Scholar] [CrossRef]
- Soluk-Tekkesin, M.; Cakarer, S.; Aksakalli, N.; Alatli, C.; Olgac, V. New World Health Organization classification of odontogenic tumours: Impact on the prevalence of odontogenic tumours and analysis of 1231 cases from Turkey. Br. J. Oral Maxillofac. Surg. 2020, 58, 1017–1022. [Google Scholar] [CrossRef]
- Vered, M.; Wright, J.M. Update from the 5th Edition of the World Health Organization Classification of Head and Neck Tumors: Odontogenic and Maxillofacial Bone Tumours. Head Neck Pathol. 2022, 16, 63–75. [Google Scholar] [CrossRef] [PubMed]
- Fujii, S.; Nagata, K.; Matsumoto, S.; Kohashi, K.I.; Kikuchi, A.; Oda, Y.; Kiyoshima, T.; Wada, N. Wnt/beta-catenin signaling, which is activated in odontomas, reduces Sema3A expression to regulate odontogenic epithelial cell proliferation and tooth germ development. Sci. Rep. 2019, 9, 4257. [Google Scholar] [CrossRef] [PubMed]
- Wolf, J.; Jarvinen, H.J.; Hietanen, J. Gardner’s dento-maxillary stigmas in patients with familial adenomatosis coli. Br. J. Oral Maxillofac. Surg. 1986, 24, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Lutz, J.C.; Nicot, R.; Schlund, M.; Schaefer, E.; Bornert, F.; Fioretti, F.; Ferri, J. Dental and maxillofacial features of Noonan Syndrome: Case series of ten patients. J. Craniomaxillofac. Surg. 2020, 48, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.M.; Vered, M. Update from the 4th Edition of the World Health Organization Classification of Head and Neck Tumours: Odontogenic and Maxillofacial Bone Tumors. Head Neck Pathol. 2017, 11, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Soluk Tekkesin, M.; Pehlivan, S.; Olgac, V.; Aksakalli, N.; Alatli, C. Clinical and histopathological investigation of odontomas: Review of the literature and presentation of 160 cases. J. Oral Maxillofac. Surg. 2012, 70, 1358–1361. [Google Scholar] [CrossRef] [PubMed]
- Owens, B.M.; Schuman, N.J.; Mincer, H.H.; Turner, J.E.; Oliver, F.M. Dental odontomas: A retrospective study of 104 cases. J. Clin. Pediatr. Dent. 1997, 21, 261–264. [Google Scholar] [PubMed]
- Chang, J.Y.; Wang, J.T.; Wang, Y.P.; Liu, B.Y.; Sun, A.; Chiang, C.P. Odontoma: A clinicopathologic study of 81 cases. J. Formos. Med. Assoc. 2003, 102, 876–882. [Google Scholar] [PubMed]
- An, S.Y.; An, C.H.; Choi, K.S. Odontoma: A retrospective study of 73 cases. Imaging Sci. Dent. 2012, 42, 77–81. [Google Scholar] [CrossRef]
- Toretti, E.F.; Miller, A.S.; Peezick, B. Odontomas: An analysis of 167 cases. J. Pedod. 1984, 8, 282–284. [Google Scholar]
- Kaugars, G.E.; Miller, M.E.; Abbey, L.M. Odontomas. Oral Surg. Oral Med. Oral Pathol. 1989, 67, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, L.F.; David, L.; Ribeiro, D.; Felino, A. Odontomas: A clinicopathologic study in a Portuguese population. Quintessence Int. 2009, 40, 61–72. [Google Scholar] [PubMed]
- Pereira de Carvalho, C.H.; Costa, D.d.A.; Guedes Queiroz, L.M.; do Amaral, J.I.Q.; Germano, A.R. Extensive complex odontoma in the maxillary sinus: An uncommon presentation as a cause of chronic sinusitis. Rev. Odonto Cienc. 2011, 26, 92–95. [Google Scholar] [CrossRef]
- Frame, J.W. Surgical excision of a large complex composite odontome of the mandible. Br. J. Oral Maxillofac. Surg. 1986, 24, 47–51. [Google Scholar] [CrossRef]
- Blinder, D.; Peleg, M.; Taicher, S. Surgical considerations in cases of large mandibular odontomas located in the mandibular angle. Int. J. Oral Maxillofac. Surg. 1993, 22, 163–165. [Google Scholar] [CrossRef]
- Casap, N.; Zeltser, R.; Abu-Tair, J.; Shteyer, A. Removal of a large odontoma by sagittal split osteotomy. J. Oral Maxillofac. Surg. 2006, 64, 1833–1836. [Google Scholar] [CrossRef] [PubMed]
- Ram, H.; Sundaram, E.; Katrolia, R.; Gupta, R. Huge complex composite odontoma of mandible. BMJ Case Rep. 2023, 16, e254948. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.K.; Van Huynh, D. Clinical and radiological characteristics of odontomas: A retrospective study of 90 cases. Imaging Sci. Dent. 2023, 53, 117–126. [Google Scholar] [CrossRef]
- Katz, R.W. An analysis of compound and complex odontomas. ASDC J. Dent. Child. 1989, 56, 445–449. [Google Scholar]
- Bereket, C.; Cakir-Ozkan, N.; Sener, I.; Bulut, E.; Tek, M. Complex and compound odontomas: Analysis of 69 cases and a rare case of erupted compound odontoma. Niger. J. Clin. Pract. 2015, 18, 726–730. [Google Scholar] [CrossRef]
- Vizuete-Bolanos, M.X.; Salgado-Chavarria, F.; Ramirez-Martinez, C.M.; Ramos-Nieto, J.J.; Vazquez-Davalos, N.M. Compound odontoma associated with a calcifying odontogenic cyst. Case report and systematic review. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, e97–e105. [Google Scholar] [CrossRef] [PubMed]
- Gwartzman, B.; Trinh, K.; Hassan, A.; Philipone, E. Dentinogenic ghost cell tumor associated with odontoma: Report of a rare case and review of literature. Quintessence Int. 2023, 54, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Siriwardena, B.; Crane, H.; O’Neill, N.; Abdelkarim, R.; Brierley, D.J.; Franklin, C.D.; Farthing, P.M.; Speight, P.M.; Hunter, K.D. Odontogenic tumors and lesions treated in a single specialist oral and maxillofacial pathology unit in the United Kingdom in 1992–2016. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 127, 151–166. [Google Scholar] [CrossRef]
- Coura, B.P.; Bernardes, V.F.; de Sousa, S.F.; Diniz, M.G.; Moreira, R.G.; de Andrade, B.A.B.; Romanach, M.J.; Pontes, H.A.R.; Gomez, R.S.; Odell, E.W.; et al. Targeted Next-Generation Sequencing and Allele-Specific Quantitative PCR of Laser Capture Microdissected Samples Uncover Molecular Differences in Mixed Odontogenic Tumors. J. Mol. Diagn. 2020, 22, 1393–1399. [Google Scholar] [CrossRef]
- Kirjavainen, A.; Tuovinen, V.; Sandor, G.K. Large ameloblastic fibro-odontoma in a 7-year-old girl with analysis of 108 cases. Ann. Maxillofac. Surg. 2016, 6, 15–20. [Google Scholar] [CrossRef]
- Piette, E.M.; Tideman, H.; Wu, P.C. Massive maxillary ameloblastic fibro-odontoma: Case report with surgical management. J. Oral Maxillofac. Surg. 1990, 48, 526–530. [Google Scholar] [CrossRef]
- Servato, J.P.; de Souza, P.E.; Horta, M.C.; Ribeiro, D.C.; de Aguiar, M.C.; de Faria, P.R.; Cardoso, S.V.; Loyola, A.M. Odontogenic tumours in children and adolescents: A collaborative study of 431 cases. Int. J. Oral Maxillofac. Surg. 2012, 41, 768–773. [Google Scholar] [CrossRef]
- Fernandes, A.M.; Duarte, E.C.; Pimenta, F.J.; Souza, L.N.; Santos, V.R.; Mesquita, R.A.; de Aguiar, M.C. Odontogenic tumors: A study of 340 cases in a Brazilian population. J. Oral Pathol. Med. 2005, 34, 583–587. [Google Scholar] [CrossRef]
- Ochsenius, G.; Ortega, A.; Godoy, L.; Penafiel, C.; Escobar, E. Odontogenic tumors in Chile: A study of 362 cases. J. Oral Pathol. Med. 2002, 31, 415–420. [Google Scholar] [CrossRef]
- Tamme, T.; Soots, M.; Kulla, A.; Karu, K.; Hanstein, S.M.; Sokk, A.; Joeste, E.; Leibur, E. Odontogenic tumours, a collaborative retrospective study of 75 cases covering more than 25 years from Estonia. J. Craniomaxillofac. Surg. 2004, 32, 161–165. [Google Scholar] [CrossRef]
- Tawfik, M.A.; Zyada, M.M. Odontogenic tumors in Dakahlia, Egypt: Analysis of 82 cases. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2010, 109, e67–e73. [Google Scholar] [CrossRef] [PubMed]





| Number of Cases | 242 |
|---|---|
| Gender | |
| Male | 126 |
| Female | 116 |
| Age (Years) | |
| Range | 3–101 |
| Mean | 19.5 |
| Median | 14 |
| Adult/Pediatric | |
| Pediatric (<18 years) | 169 |
| Adult (>18 years) | 73 |
| Type of Dentition | |
| Primary (<6 years) | 2 |
| Mixed (6–13 years) | 118 |
| Permanent (>13 years) | 122 |
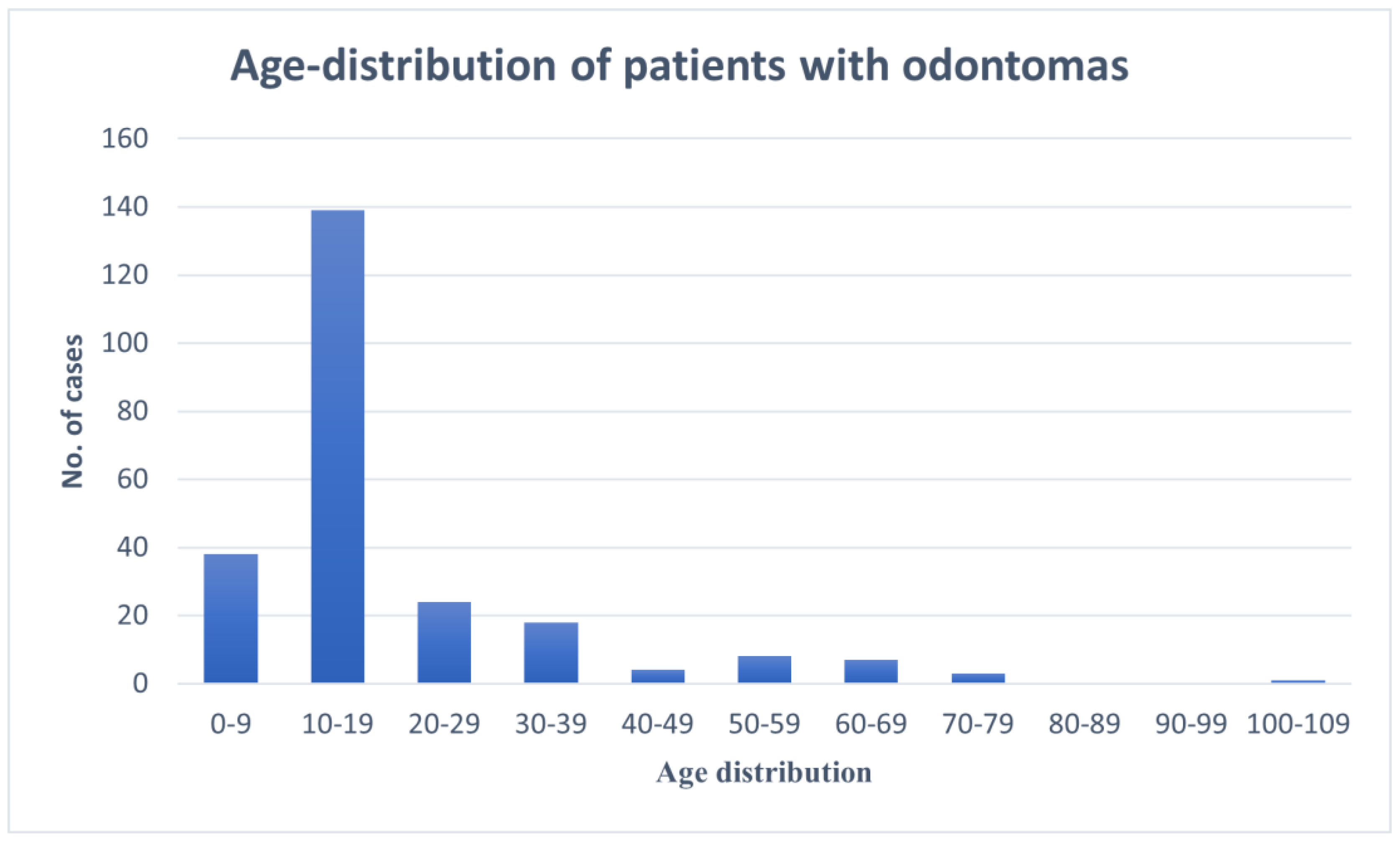
| Age Distribution (Years) | |
| 0–9 | 38 |
| 10–19 | 139 |
| 20–29 | 24 |
| 30–39 | 18 |
| 40–49 | 4 |
| 50–59 | 8 |
| 60–69 | 7 |
| 70–79 | 3 |
| 80–89 | 0 |
| 90–99 | 0 |
| 100–109 | 1 |
| Jaw | |
| Maxilla | 117 |
| Mandible | 122 |
| Unspecified | 3 |
| Location | |
| Anterior | 137 |
| Posterior | 95 |
| Unspecified | 10 |
| Type | |
| Compound | 142 |
| Complex | 53 |
| AFO | 4 |
| Unspecified (odontoma) | 43 |
| Pathologic/radiographic confirmation | |
| Pathologic alone | 197 |
| Radiographic alone | 42 |
| Both | 3 |
| Associated Cyst | |
| Dentigerous | 8 |
| Nasopalatine duct cyst | 1 |
| Clinical Findings | |
| Impacted | 83 |
| Delayed eruption | 8 |
| Retained primary | 1 |
| Partially erupted | 1 |
| Toothache | 1 |
| Case No. | Age | Sex | Type | Location | Clinical Findings |
|---|---|---|---|---|---|
| 1 | 13 | F | AFO | Maxilla—Posterior | NR |
| 2 | 25 | M | Complex | Mandible—Posterior | Toothache |
| 3 | 31 | M | Odontoma (U) | Maxilla—Anterior | NR |
| 4 | 11 | M | Compound | Maxilla—Anterior | Impacted #27 |
| 5 | 44 | M | Compound | Mandible—Anterior | Impacted #22 |
| 6 | 13 | F | Odontoma (U) | Maxilla—Anterior | Impacted #11 |
| 7 | 13 | M | Odontoma (U) | Maxilla—Anterior | Impacted #6 |
| 8 | 26 | M | Odontoma (U) | Mandible—Posterior | Impacted #17 |
| 9 | 101 | F | Odontoma (U) | Mandible—Posterior | NR |
| Type | Compound | Complex | AFO |
|---|---|---|---|
| No. of cases | 142 | 53 | 4 |
| Gender | |||
| Male | 76 | 22 | 3 |
| Female | 66 | 31 | 1 |
| Jaw | |||
| Maxilla | 62 | 29 | |
| Anterior | 44 | 13 | 3 |
| Posterior | 15 | 16 | - |
| Unspecified | 3 | 3 | |
| Mandible | 78 | 23 | |
| Anterior | 53 | 7 | 1 |
| Posterior | 23 | 15 | - |
| Unspecified | 2 | 1 | 1 |
| Unspecified | 2 | 1 | |
| Age (Years) | |||
| Range | 3–78 | 7–68 | 10–13 |
| Mean | 17.7 | 23.7 | 11.75 |
| Median | 13 | 16 | 12 |
| Pathologic/radiographic | |||
| Pathologic alone | 120 | 36 | 4 |
| Radiographic alone | 20 | 17 | - |
| Both | 2 | - | - |
| Clinical Findings | 55 impacted | 14 impacted | 1 impacted |
| 1 retained | |||
| 5 delayed eruptions | 2 delayed eruptions | ||
| 1 partially erupted |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
DeColibus, K.A.; Rasner, D.S.; Okhuaihesuyi, O.; Owosho, A.A. Clinicoradiopathologic Analysis of Odontomas: A Retrospective Study of 242 Cases. Dent. J. 2023, 11, 253. https://doi.org/10.3390/dj11110253
DeColibus KA, Rasner DS, Okhuaihesuyi O, Owosho AA. Clinicoradiopathologic Analysis of Odontomas: A Retrospective Study of 242 Cases. Dentistry Journal. 2023; 11(11):253. https://doi.org/10.3390/dj11110253
Chicago/Turabian StyleDeColibus, Katherine A., D. Shane Rasner, Osariemen Okhuaihesuyi, and Adepitan A. Owosho. 2023. "Clinicoradiopathologic Analysis of Odontomas: A Retrospective Study of 242 Cases" Dentistry Journal 11, no. 11: 253. https://doi.org/10.3390/dj11110253
APA StyleDeColibus, K. A., Rasner, D. S., Okhuaihesuyi, O., & Owosho, A. A. (2023). Clinicoradiopathologic Analysis of Odontomas: A Retrospective Study of 242 Cases. Dentistry Journal, 11(11), 253. https://doi.org/10.3390/dj11110253