Mixed-Thickness Tunnel Access (MiTT) through a Linear Vertical Mucosal Incision for a Minimally Invasive Approach for Root Coverage Procedures in Anterior and Posterior Sites: Technical Description and Case Series with 1-Year Follow-Up
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
- Healthy individuals;
- Non-smokers;
- Non-diabetics;
- Diagnosed with gingival recession type 1 or 2 (RT1 or RT2) [16].
- Patients with a poor standard of plaque control and demonstrating a lack of ability to maintain a good level of oral hygiene (full-mouth plaque score ≥ 20%);
- Bleeding on probing (BoP) > 10%;
- Questionable long-term prognosis of patient dentition;
- Any mobility;
- Pregnancy;
- Severe cardiovascular disease;
- Taking any medication that may interfere with the healing;
- Malignancy;
- Bleeding disorders.
2.2. MiTT Technique—Preparation Steps
- Systemic health condition compatible with a healthy patient or with controlled disease;
- Non-pregnant;
- If using any medication, it must not harm healing or cause excessive bleeding;
- Adequate blood pressure (lower than 140/90 mmHg recommended);
- The width of the local keratinized tissue width (KTW) remnant is suggested to be at least 1 mm;
- Whether it is a single tooth or multiple teeth with gingival recessions, evaluate the best site for the primary incision or, if necessary, more than one incision;
- Identify the type of recession (RT) [13], which can help with the prediction of the results;
- Verify if there is a step and visible cement–enamel junction (CEJ) [17];
- Verify gingival thickness;
- Verify if there is any bone or soft tissue defect close to the recession(s);
- Periodontal diagnosis;
- Verify if there is a rotated, tilted, or crowded tooth associated with the area of the recession
- BoP—recommended ≤ 10%.
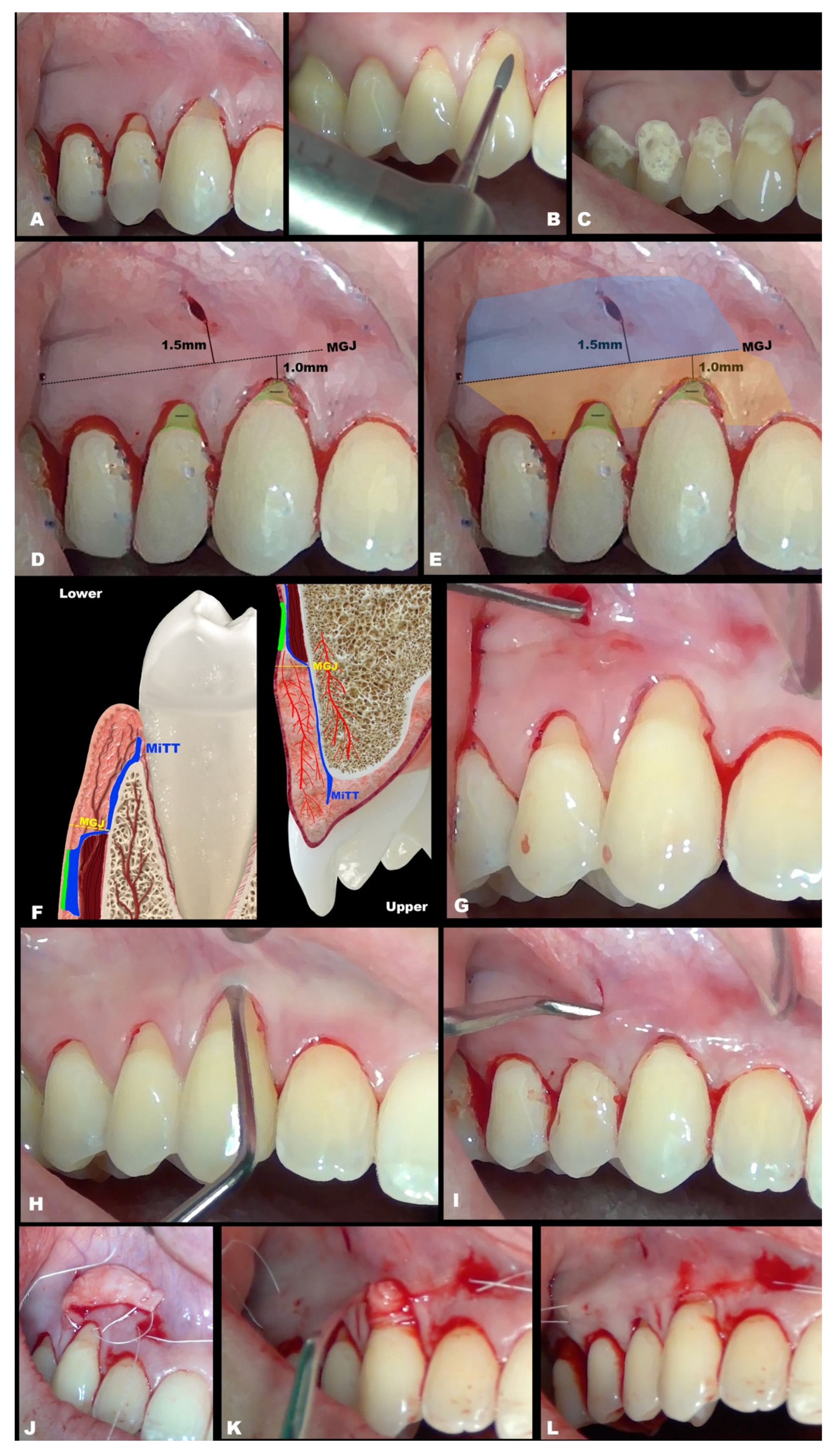
2.3. MiTT Technique—Surgical Steps
- (1)
- Vertical incision on the mucosa (around 1–2 mm apical to the MGJ), lateral to the papilla base (Figure 1D). It is mandatory not to perform this incision in the center of the papilla’s base, which might damage any vascular supply or risk damage to the papilla. In multiple recessions, it is recommended to perform two vertical incisions; and if extremely necessary, more vertical incisions can be performed, always in mucosa and lateral in the papilla’s base.
- (2)
- (3)
- It is permitted (but not mandatory) to perform intrasulcular incisions, including up to one adjacent tooth (Figure 1H), which can facilitate the procedure to connect the tunnel. Avoid causing any damage to the gingival margin.
- (4)
- From the MGJ, subperiosteal access to raise the full-thickness tunnel is performed (Figure 1I), involving one adjacent tooth, to keep the local vascularization. The access is subperiosteal, and it is essential to act gently in this stage.
- (5)
- Confirm the tissue detachment until the gingival sulcus area (free gingival margin) and also in the papilla’s base (Figure 1J), keeping the papilla’s tip intact.
- (6)
- After CTG is harvested (either subepithelial or de-epithelialized), it will be inserted in the desired site through the linear incision or intrasulcularly (Figure 1K,L).
- (7)
- The CTG will be adjusted to cover the recession (Figure 1l) and must be coronally advanced at least 1 mm coronal to the CEJ.
- (8)
- Then, MiTT should be sutured according to the personally preferred technique. It is suggested that the suture techniques slightly pull the tunnel coronal (anchored with composite or double-crossed suture [18]). The vertical incision must be sutured with one or two single sutures. It is suggested to stabilize the soft tissues using interrupted sutures, and it may be used as adjunctive material, such as a biological glue. It is suggested that the suture be removed between 7 and 14 days.
2.4. Statistical Analysis
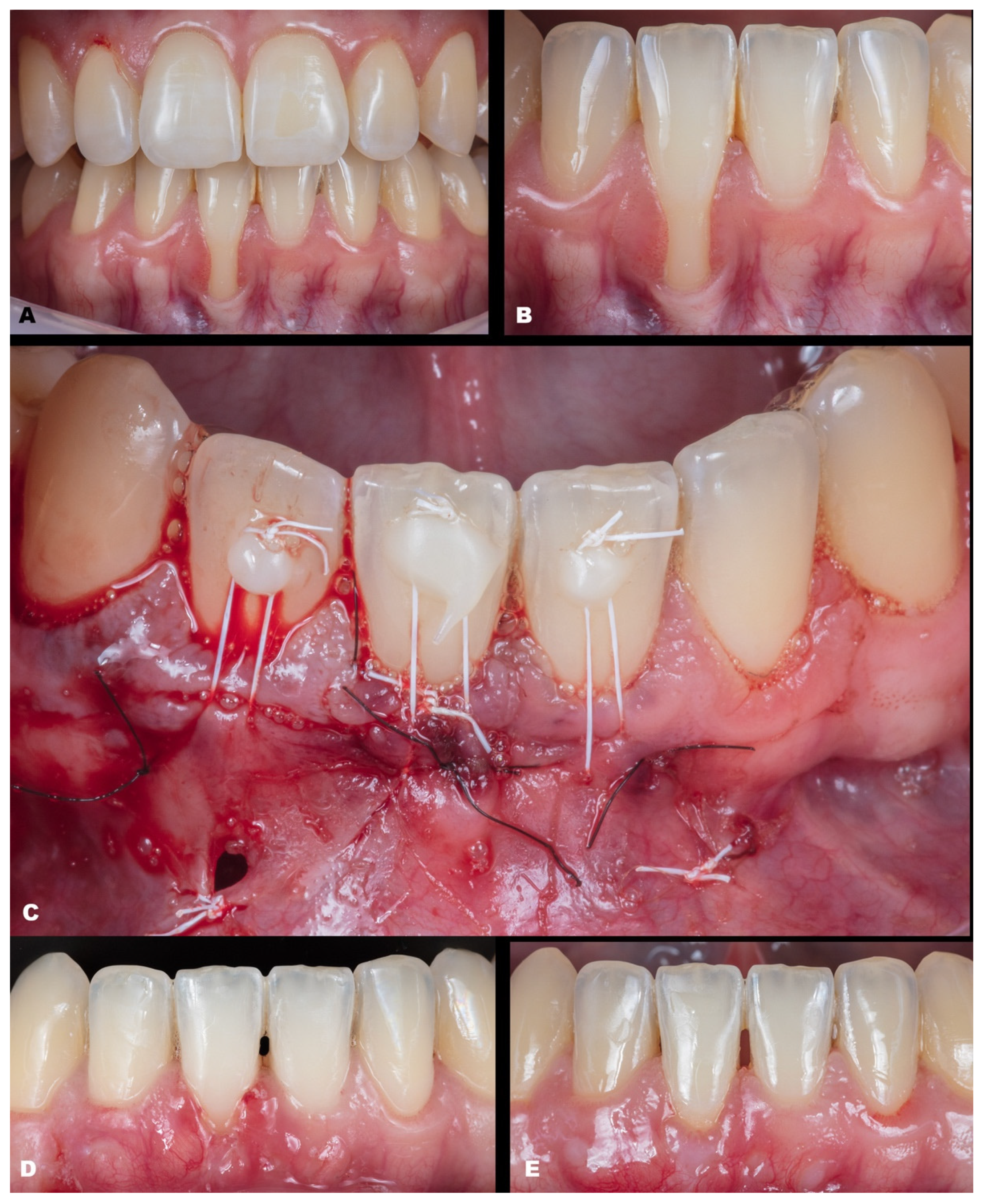
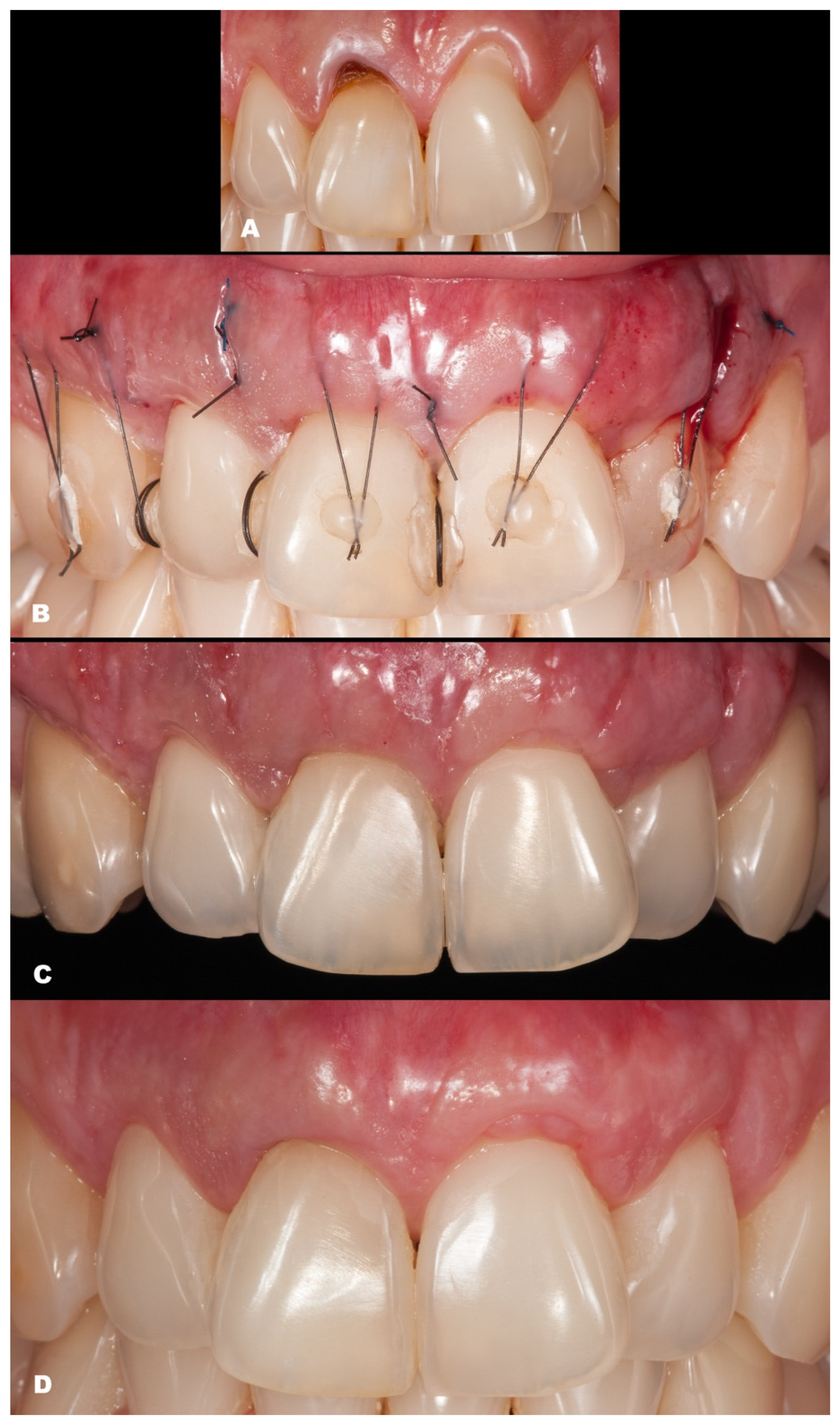
3. Results
4. Discussion
4.1. Evolution of Tunnel Techniques
4.2. Pros and Cons of the MiTT Technique and Limitations of This Study
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Chambrone, L.; Tatakis, D.N. Periodontal soft tissue root coverage procedures: A systematic review from the AAP Regeneration Workshop. J. Periodontol. 2015, 86, S8–S51. [Google Scholar] [CrossRef]
- Zabalegui, I.; Sicilia, A.; Cambra, J.; Gil, J.; Sanz, M. Treatment of multiple adjacent gingival recessions with the tunnel subepithelial connective tissue graft: A clinical report. Int. J. Periodontics Restor. Dent. 1999, 19, 199–206. [Google Scholar]
- Tözüm, T.F.; Dini, F.M. Treatment of adjacent gingival recessions with sub-epithelial connective tissue grafts and the modified tunnel technique. Quintessence Int. 2003, 34, 7–13. [Google Scholar]
- Raetzke, P.B. Covering localized areas of root exposure employing the “envelope” technique. J. Periodontol. 1985, 56, 397–402. [Google Scholar] [CrossRef]
- Zadeh, H.H. Minimally invasive treatment of maxillary anterior gingival recession defects by vestibular incision subperiosteal tunnel access and platelet-derived growth factor BB. Int. J. Periodontics Restor. Dent. 2011, 31, 653–660. [Google Scholar]
- Allen, A.L. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. I. Rationale and technique. Int. J. Periodontics Restor. Dent. 1994, 14, 216–227. [Google Scholar]
- Allen, A.L. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. II. Clinical results. Int. J. Periodontics Restor. Dent. 1994, 14, 302–315. [Google Scholar]
- Chao, J.C. A novel approach to root coverage: The pinhole surgical technique. Int. J. Periodontics Restor. Dent. 2012, 32, 521–531. [Google Scholar]
- Tuttle, D.; Kurtzman, G.; Bernotti, A.L. Gum Drop Technique: Minimally Invasive Soft-Tissue Platelet-Rich Plasma Grafting for Marginal Soft-Tissue Recession. Compend. Contin. Educ. Dent. 2018, 39, e9–e12. [Google Scholar]
- Fernandes, G.V.; Santos, N.B.; Siqueira, R.A.; Wang, H.L.; Blanco-Carrion, J.; Fernandes, J.C. Autologous platelet concentrate of 2nd and 3rd generations efficacy in the surgical treatment of gingival recession: An overview of systematic reviews. J. Indian Soc. Periodontol. 2021, 25, 463–479. [Google Scholar] [CrossRef]
- Jankovic, S.; Aleksic, Z.; Milinkovic, I.; Dimitrijevic, B. The coronally advanced flap in combination with platelet-rich fibrin (PRF) and enamel matrix derivative in the treatment of gingival recession: A comparative study. Eur. J. Esthet. Dent. 2010, 5, 260–273. [Google Scholar] [PubMed]
- Tunalι, M.; Özdemir, H.; Arabacι, T.; Gürbüzer, B.; Pikdöken, L.; Firatli, E. Clinical evaluation of autologous platelet-rich fibrin in the treatment of multiple adjacent gingival recession defects: A 12-month study. Int. J. Periodontics Restor. Dent. 2015, 35, 105–114. [Google Scholar] [CrossRef]
- Kuka, S.; Ipci, S.D.; Cakar, G.; Yılmaz, S. Clinical evaluation of coronally advanced flap with or without platelet-rich fibrin for the treatment of multiple gingival recessions. Clin. Oral Investig. 2018, 22, 1551–1558. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-T.; Hamalian, T.; Schulze-Späte, U. Minimally invasive treatment of soft tissue deficiency around an implant-supported restoration in the esthetic zone: Modified VISTA technique case report. J. Oral Implantol. 2015, 41, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Tözüm, T.F.; Keçeli, H.G.; Güncü, G.N.; Hatipoğlu, H.; Sengün, D. Treatment of gingival recession: Comparison of two techniques of subepithelial connective tissue graft. J. Periodontol. 2005, 76, 1842–1848. [Google Scholar] [CrossRef]
- Cairo, F.; Nieri, M.; Cincinelli, S.; Mervelt, J.; Pagliaro, U. The interproximal clinical attachment level to classify gingival recessions and predict root coverage outcomes: An explorative and reliability study. J. Clin. Periodontol. 2011, 38, 661–666. [Google Scholar] [CrossRef]
- Pini-Prato, G.P.; Franceschi, D.; Cairo, F.; Nieri, M.; Rotundo, R. Classification of dental surface defects in areas of gingival recession. J. Periodontol. 2010, 81, 885–890. [Google Scholar] [CrossRef]
- Zuhr, O.; Rebele, S.F.; Thalmair, T.; Fickl, S.; Hürzeler, M.B. A modified suture technique for plastic periodontal and implant surgery—The double-crossed suture. Eur. J. Esthet. Dent. 2009, 4, 338–347. [Google Scholar]
- Wennström, J. Mucogingival surgery. In Proceedings of the 1st European Workshop on Periodontology, Thurgau, Switzerland, 1–4 February 1993; Lang, N.P., Karring, T., Eds.; Quintessence: London, UK, 1994; pp. 193–209. [Google Scholar]
- Harris, R.J. The connective tissue and partial thickness double pedicle graft: A predictable method of obtaining root coverage. J. Periodontol. 1992, 63, 477–486. [Google Scholar] [CrossRef]
- Zucchelli, G.; Clauser, C.; De Sanctis, M.; Calandriello, M. Mucogingival versus guided tissue regeneration procedures in the treatment of deep recession type defects. J. Periodontol. 1998, 69, 139–145. [Google Scholar] [CrossRef]
- Roccuzzo, M.; Bunino, M.; Needleman, I.; Sanz, M. Periodontal plastic surgery for treatment of localized gingival recessions: A systematic review. J. Clin. Periodontol. 2002, 29, 178–194. [Google Scholar] [CrossRef] [PubMed]
- Zucchelli, G.; Amore, C.; Sforzal, N.M.; Montebugnoli, L.; De Sanctis, M. Bilaminar techniques for the treatment of recession-type defects. A comparative clinical study. J. Clin. Periodontol. 2003, 30, 862–870. [Google Scholar] [CrossRef] [PubMed]
- Dias, A.T.; Menezes, C.C.; Kahn, S.; Fischer, R.G.; Figueredo, C.M.S.; Fernandes, G.V.O. Gingival recession treatment with enamel matrix derivative associated with coronally advanced flap and subepithelial connective tissue graft: A split-mouth randomized controlled clinical trial with molecular evaluation. Clin. Oral Investig. 2022, 26, 1453–1463. [Google Scholar] [CrossRef]
- Allen, E.P.; Miller, P.D., Jr. Coronal positioning of existing gingiva: Short term results in the treatment of shallow marginal tissue recession. J. Periodontol. 1989, 60, 316–319. [Google Scholar] [CrossRef]
- Harris, R.J.; Harris, A.W. The coronally positioned pedicle graft with inlaid margins: A predictable method of obtaining root coverage of shallow defects. Int. J. Periodontics Restor. Dent. 1994, 14, 228–241. [Google Scholar]
- Zucchelli, G.; De Sanctis, M. Treatment of multiple recession-type defects in patients with esthetic demands. J. Periodontol. 2000, 71, 1506–1514. [Google Scholar] [CrossRef] [PubMed]
- Zuhr, O.; Rebele, S.F.; Cheung, S.L.; Hurzeler, M.B.; Research Group on Oral Soft Tissue Biology and Wound Healing. Surgery without papilla incision: Tunneling flap procedures in plastic periodontal and implant surgery. Periodontology 2000 2018, 77, 123–149. [Google Scholar] [CrossRef] [PubMed]
- Tavelli, L.; Barootchi, S.; Nguyen, T.V.N.; Tattan, M.; Ravidà, A.; Wang, H.-L. Efficacy of tunnel technique in the treatment of localized and multiple gingival recessions: A systematic review and meta-analysis. J. Periodontol. 2018, 89, 1075–1090. [Google Scholar] [CrossRef]
- Papageorgakopoulos, G.; Greenwell, H.; Hill, M.; Vidal, R.; Scheetz, J.P. Root coverage using acellular dermal matrix and comparing a coronally positioned tunnel to a coronally positioned flap approach. J. Periodontol. 2008, 79, 1022–1030. [Google Scholar] [CrossRef]
- Bherwani, C.; Kulloli, A.; Kathariya, R.; Shetty, S.; Agrawal, P.; Gujar, D.; Desai, A. Zucchelli’s technique or tunnel technique with subepithelial connective tissue graft for treatment of multiple gingival recessions. J. Int. Acad. Periodontol. 2014, 16, 34–42. [Google Scholar]
- Gobbato, L.; Nart, J.; Bressan, E.; Mazzocco, F.; Paniz, G.; Lops, D. Patient morbidity and root coverage outcomes after the application of a subepithelial connective tissue graft in combination with a coronally advanced flap or via a tunneling technique: A randomized controlled clinical trial. Clin. Oral Investig. 2016, 20, 2191–2202. [Google Scholar] [CrossRef] [PubMed]
- Azaripour, A.; Kissinger, M.; Farina, V.S.; Van Noorden, C.J.; Gerhold-Ay, A.; Willershausen, B.; Cortellini, P. Root coverage with connective tissue graft associated with coronally advanced flap or tunnel technique: A randomized, double-blind, mono-centre clinical trial. J. Clin. Periodontol. 2016, 43, 1142–1150. [Google Scholar] [CrossRef] [PubMed]
- Toledano-Osorio, M.; Muñoz-Soto, E.; Toledano, M.; Vallecillo-Rivas, M.; Vallecillo, C.; Ramos-García, P.; Osorio, R. Treating Gingival Recessions Using Coronally Advanced Flap or Tunnel Techniques with Autografts or Polymeric Substitutes: A Systematic Review and Meta-Analysis. Polymers 2022, 14, 1453. [Google Scholar] [CrossRef]
- González-Febles, J.; Romandini, M.; Laciar-Oudshoorn, F.; Noguerol, F.; Marruganti, C.; Bujaldón-Daza, A.; Zabalegui, I.; Sanz, M. Tunnel vs. coronally advanced flap in combination with a connective tissue graft for the treatment of multiple gingival recessions: A multi-center randomized clinical trial. Clin. Oral Investig. 2023, 27, 3627–3638. [Google Scholar] [CrossRef] [PubMed]
- Rebele, S.F.; Zuhr, O.; Schneider, D.; Jung, R.E.; Hürzeler, M.B. Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivative for root coverage: A RCT using 3D digital measuring methods. Part II. Volumetric studies on healing dynamics and gingival dimensions. J. Clin. Periodontol. 2014, 41, 593–603. [Google Scholar] [CrossRef]
- Quispe-López, N.; Castaño-Séiquer, A.; Pardal-Peláez, B.; Garrido-Martínez, P.; Gómez-Polo, C.; Mena-Álvarez, J.; Montero-Martín, J. Clinical Outcomes of the Double Lateral Sliding Bridge Flap Technique with Simultaneous Connective Tissue Graft in Sextant V Recessions: Three-Year Follow-Up Study. Appl. Sci. 2022, 12, 1038. [Google Scholar] [CrossRef]
- Azzi, R.; Etienne, D.; Takei, H.; Fenech, P. Surgical thickening of the existing gingiva and reconstruction of interdental papillae around implant-supported restorations. Int. J. Periodontics Restor. Dent. 2002, 22, 71–77. [Google Scholar]
- Aroca, S.; Molnar, B.; Windisch, P.; Gera, I.; Salvi, G.E.; Nikolidakis, D.; Sculean, A. Treatment of multiple adjacent Miller class I and II gingival recessions with a Modified Coronally Advanced Tunnel (MCAT) technique and a collagen matrix or palatal connective tissue graft: A randomized, controlled clinical trial. J. Clin. Periodontol. 2013, 40, 713–720. [Google Scholar] [CrossRef]
- Zuhr, O.; Fickl, S.; Wachtel, H.; Bolz, W.; Hurzeler, M.B. Covering of gingival recessions with a modified microsurgical tunnel technique: Case report. Int. J. Periodontics Restor. Dent. 2007, 27, 457–463. [Google Scholar]
- Boutros, S.; Bernard, R.W.; Galiano, R.D.; Addona, T.; Stokes, B.; McCarthy, J.G. The Temporal Sequence of Periosteal Attachment after Elevation. Plast. Reconstr. Surg. 2003, 111, 1942–1947. [Google Scholar] [CrossRef]
- Mikecs, B.; Vág, J.; Gerber, G.; Molnár, B.; Feigl, G.; Shahbazi, A. Revisiting the vascularity of the keratinized gingiva in the maxillary esthetic zone. BMC Oral Health 2021, 21, 160. [Google Scholar] [CrossRef] [PubMed]
- Salem, S.; Salhi, L.; Seidel, L.; Lecloux, G.; Rompen, E.; Lambert, F. Tunnel/Pouch versus Coronally Advanced Flap Combined with a Connective Tissue Graft for the Treatment of Maxillary Gingival Recessions: Four-Year Follow-Up of a Randomized Controlled Trial. J. Clin. Med. 2020, 9, 2641. [Google Scholar] [CrossRef] [PubMed]







| “Envelope” Technique | Modified Envelope Technique | Tunnel Technique | Modified Tunnel Technique | VISTA | PST | m-VISTA | GDT | |
|---|---|---|---|---|---|---|---|---|
| Authors/Year | Raetzke (1985) [4] | Allen (1994) [6,7] | Zabalegui et al. (1999) [2] | Tözüm & Dini (2003) [3] | Zadeh (2011) [5] | Chao (2012) [8] | Lee et al. (2015) [14] | Tuttle et al. (2018) [9] |
| Advantages | - Simple technique (without coronal displacement) with minimal trauma. - Does not detach papillae. | - Can be performed on multiple sites. - Simple technique (without coronal displacement) with minimal trauma. | - Does not detach papillae - Simple technique (without coronal displacement). - Partial dissection. | - Without vertical incisions. - Full-thickness dissection at the mucogingival area (in a coronoapical direction) to supply more blood vessels. - Does not detach papillae. | - Does not detach papillae. - Incision in mucosa facilitating the access. - Easier detachment of the soft tissue (subperiosteal). | - Does not detach papillae. - Incision in mucosa facilitating the access. - Full-thickness dissection (reduced risk of fenestration). | - Double vascular surfaces for revascularization of the graft. - Lower risk of graft necrosis and scarring. - Better capillary ingrowth. - Does not detach papillae. | - Minimally invasive. - Places holes in mucosa to permit the access. - Reduced risk of fenestration-full-thickness tunnel (subperiosteal access). - Does not detach papillae. |
| Disadvantages | - Higher risk of necrosis of the CTG (exposed). - Used in isolated areas (single tooth). - Lower level of root coverage for gingival recessions greater than 3 mm. - Supraperiosteal approach (higher risk of fenestration). | - Supraperiosteal approach—higher risk of fenestration. - Higher risk of necrosis of the CTG (exposed). | - Only intrasulcular incisions. - Supraperiosteal approach (higher risk of fenestration. - CTG has a small exposition—elevated risk of necrosis. | - Only intrasulcular incisions. - CTG has a small exposition (around 50%)—elevated risk of necrosis. | - Expensive biomaterial was used (membrane complex (β-TCP hydrated with rhPDGF-BB)). - More invasive. | - Collagen stripes placed (increase the cost due to the biomaterial). - Specific instruments to perform the technique. - More invasive. | - Access is only through the frenum area, “V-shaped” incision. - Simultaneous frenectomy. - Difficult level for thin phenotypes (risk of fenestration). - More invasive. | - Substitution of the “gold standard” (CTG) for the A-PRF and i-PRF. - Rapid resorption of the PRF compared with the CTG. - More invasive. |
| Classification | Gender | Tooth/Teeth with REC | Initial REC Height (mm) | Initial REC Width (mm) | Initial PD (mm) | Initial KTW (mm) | Final REC Height (mm) | Final PD (mm) | Final KTW (mm) | % RC | p-Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6-Month Follow-up | |||||||||||
| Case 1 | RT2 | M | 41 | 6.2 | 2.5 | 1.0 | 0.3 | 1.1 | 2.0 | 4.3 | 82.25 | REC: p < 0.0001 PD: p = 0.2771 KTW: p = 0.1013 |
| Case 2 | RT1 | F | 31 | 3.3 | 1.7 | 0.5 | 0.3 | none | 1.0 | 3.7 | 100 | |
| Case 3 | RT1 | F | 41 | 1.2 | 2.1 | 1.0 | 3.3 | none | 0.5 | 7.3 | 100 | |
| Case 4 | RT1 | F | 41 31 | 1.4 1.2 | 2.1 1.8 | 1.0 0.5 | 3.1 2.9 | none | 1.0 0.5 | 3.7 4.0 | 100 100 | |
| Case 5 | RT1 | M | 43 | 1.5 | 2.3 | 1.0 | 1.3 | none | 1.5 | 4.4 | 100 | |
| Case 6 | RT1 | F | 43 44 45 | 1.2 2.1 1.4 | 2.6 3.1 2.8 | 2.0 1.5 1.0 | 3.0 3.8 3.8 | none | 1.5 1.0 1.0 | 2.1 2.8 5.3 | 100 100 100 | |
| Case 7 | RT1 | F | 12 11 21 22 | 1.1 1.5 2.4 1.5 | 1.5 3.0 4.0 2.0 | 1.0 2.0 1.5 2.0 | 5.4 5.0 6.3 6.9 | none | 1.0 2.5 2.5 1.5 | 4.3 5.7 6.0 6.3 | 100 100 100 100 | |
| Case 8 | RT2 | F | 42 41 31 32 | 2.2 3.4 3.2 1.2 | 2.3 2.5 3.0 2.7 | 0.5 0.5 0.5 1.0 | 2.4 1.9 1.5 3.5 | 0 0.6 0.6 0.5 | 1.5 1.0 1.0 1.0 | 3.6 2.9 2.1 3.3 | 100 82.35 81.25 58.34 | |
| Case 9 | RT1 | F | 12 13 | 1.3 2.1 | 2.2 2.3 | 1.5 2.0 | 4.4 5.3 | none | 2.5 1.5 | 4.6 5.2 | 100 100 | |
| MITT | |
|---|---|
| Advantages | - Simple technique with reduced risk of fenestration. |
| - Does not detach papillae. | |
| - Easier access. | |
| - Greater mobility of the tunnel. | |
| - No exposition of the graft, reduced risk of necrosis. | |
| Disadvantages | - Reduced vascularization, complete detachment. |
| Differences | - Lower risk of necrosis for the flap and graft. |
| - Used in single or multiple recessions. | |
| - It can be used in shallow or deep recessions. | |
| - More predictable release of the tunnel. | |
| - It is not performed only in the frenum area. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marques, T.; Santos, N.B.M.d.; Sousa, M.; Fernandes, J.C.H.; Fernandes, G.V.O. Mixed-Thickness Tunnel Access (MiTT) through a Linear Vertical Mucosal Incision for a Minimally Invasive Approach for Root Coverage Procedures in Anterior and Posterior Sites: Technical Description and Case Series with 1-Year Follow-Up. Dent. J. 2023, 11, 235. https://doi.org/10.3390/dj11100235
Marques T, Santos NBMd, Sousa M, Fernandes JCH, Fernandes GVO. Mixed-Thickness Tunnel Access (MiTT) through a Linear Vertical Mucosal Incision for a Minimally Invasive Approach for Root Coverage Procedures in Anterior and Posterior Sites: Technical Description and Case Series with 1-Year Follow-Up. Dentistry Journal. 2023; 11(10):235. https://doi.org/10.3390/dj11100235
Chicago/Turabian StyleMarques, Tiago, Nuno Bernardo Malta dos Santos, Manuel Sousa, Juliana Campos Hasse Fernandes, and Gustavo Vicentis Oliveira Fernandes. 2023. "Mixed-Thickness Tunnel Access (MiTT) through a Linear Vertical Mucosal Incision for a Minimally Invasive Approach for Root Coverage Procedures in Anterior and Posterior Sites: Technical Description and Case Series with 1-Year Follow-Up" Dentistry Journal 11, no. 10: 235. https://doi.org/10.3390/dj11100235
APA StyleMarques, T., Santos, N. B. M. d., Sousa, M., Fernandes, J. C. H., & Fernandes, G. V. O. (2023). Mixed-Thickness Tunnel Access (MiTT) through a Linear Vertical Mucosal Incision for a Minimally Invasive Approach for Root Coverage Procedures in Anterior and Posterior Sites: Technical Description and Case Series with 1-Year Follow-Up. Dentistry Journal, 11(10), 235. https://doi.org/10.3390/dj11100235







