Smoking as a Risk Factor for Dry Socket: A Systematic Review
Abstract
:1. Introduction
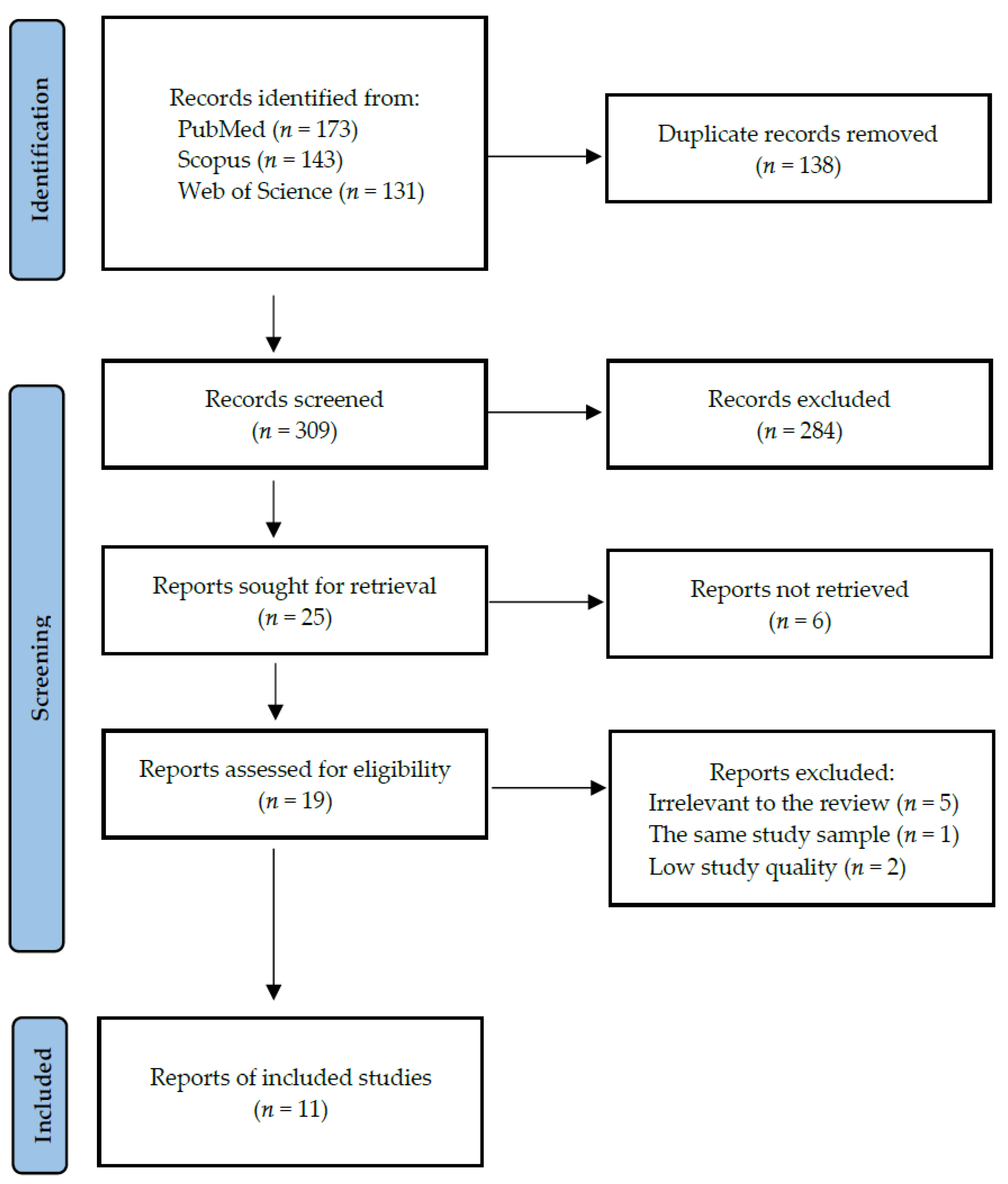
2. Materials and Methods
2.1. Search Strategy and Data Extraction
- -
- For PubMed: ((dry socket) OR (dry alveol*) OR (alveolar osteitis) OR (alveolitis osteitis) OR (fibrynolitic alveolitis)) AND ((smoker*) OR (alcoholic*) OR (smoking) OR (alcohol consumption) OR (cigarette) OR (nicotine) OR (tobacco) OR (alcohol) OR (alcohol addiction) OR (cigarette addiction))
- -
- For Scopus: TITLE-ABS-KEY ((“dry socket”) OR (“dry alveol*”) OR (“alveolar osteitis”) OR (“alveolitis osteitis”) OR (“fibrynolitic alveolitis”)) AND ((smoker*) OR (alcoholic*) OR (smoking) OR (“alcohol consumption”) OR (cigarette) OR (nicotine) OR (tobacco) OR (alcohol) OR (“alcohol addiction”) OR (“cigarette addiction”))
- -
- For Web of Science: TS = (dry socket OR dry alveol* OR alveolar osteitis OR alveolitis osteitis OR fibrynolitic alveolitis) AND TS = (smoker* OR alcoholic* OR smoking OR alcohol consumption OR cigarette OR nicotine OR tobacco OR alcohol OR alcohol addiction OR cigarette addiction).
2.2. Quality Assessment and Critical Appraisal for the Systematic Review of Included Studies
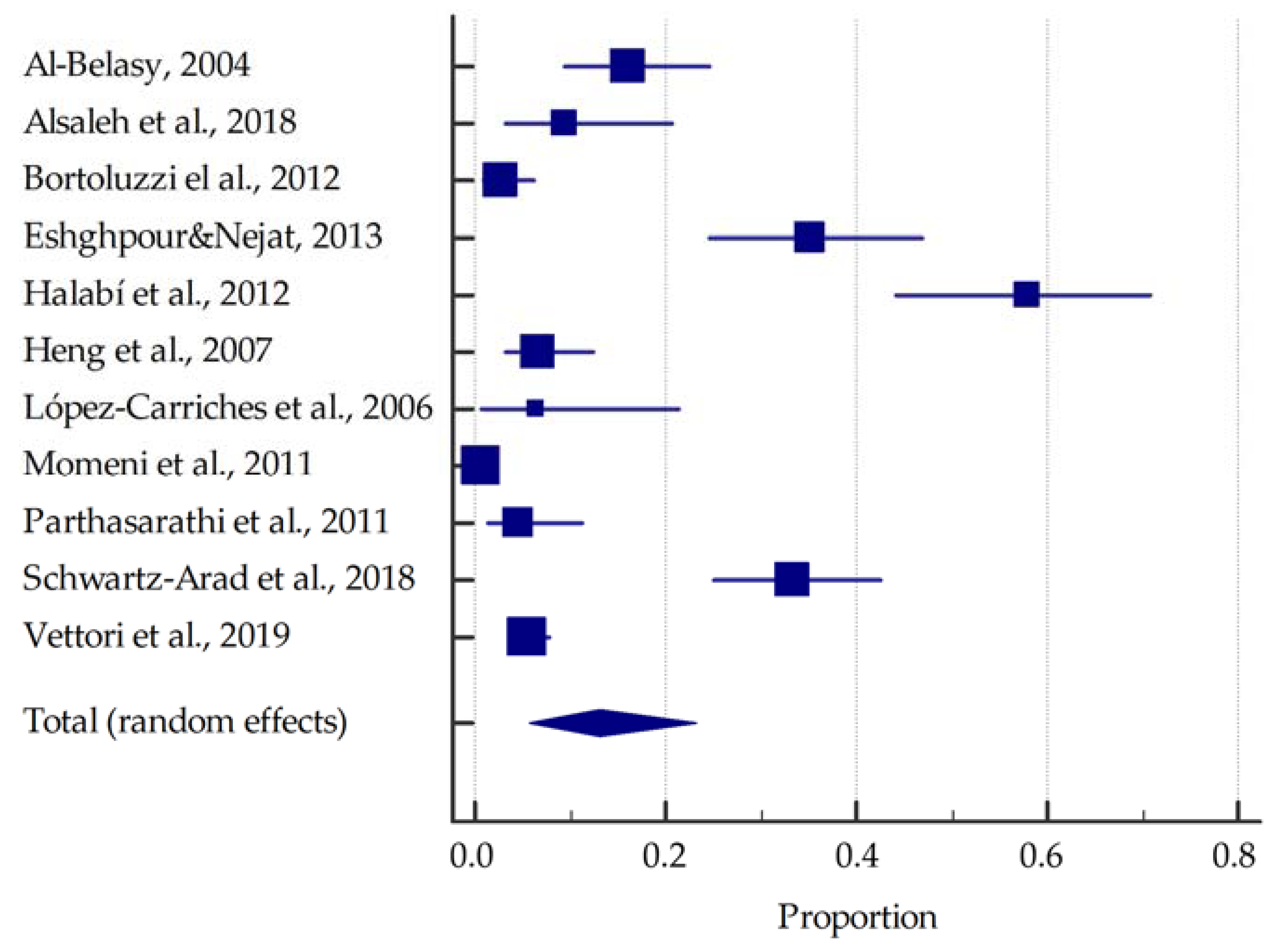
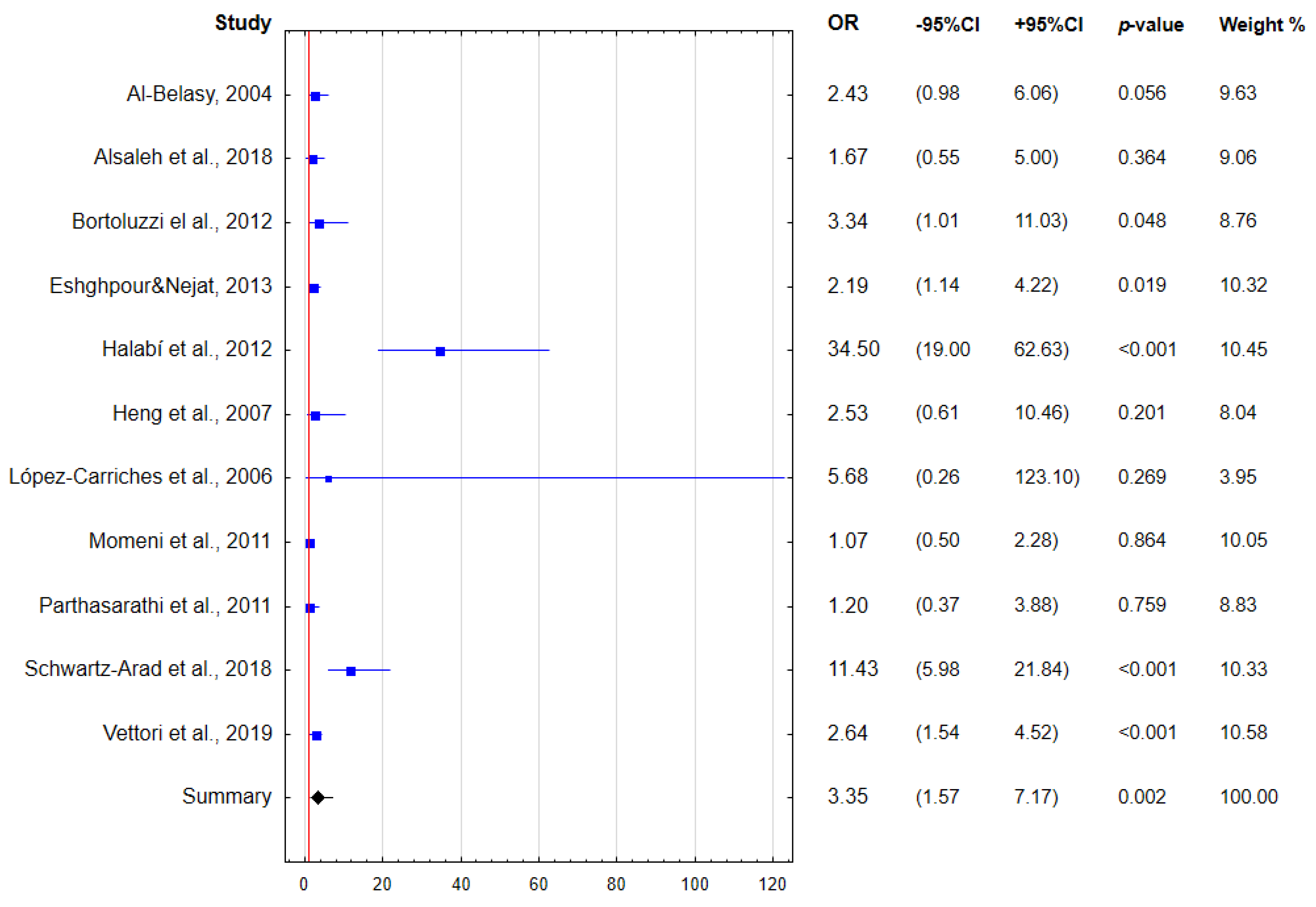
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nijakowski, K.; Cieślik, K.; Łaganowski, K.; Gruszczyński, D.; Surdacka, A. The Impact of the COVID-19 Pandemic on the Spectrum of Performed Dental Procedures. Int. J. Environ. Res. Public Health 2021, 18, 3421. [Google Scholar] [CrossRef] [PubMed]
- Cagetti, M.G.; Balian, A.; Camoni, N.; Campus, G. Influence of the COVID-19 Pandemic on Dental Emergency Admissions in an Urgent Dental Care Service in North Italy. Int. J. Environ. Res. Public Health 2021, 18, 1812. [Google Scholar] [CrossRef] [PubMed]
- Farooq, Z.; Waqar, A.; Saeed, A. Incidence and Treatment of Complications in Patients Who Had Third Molars or Other Teeth Extracted. Indoam. J. Pharm. Sci. 2018, 5, 8540–8545. [Google Scholar] [CrossRef]
- Cahen, P.M.; Frank, R.M.; Turlot, J.C. A Survey of the Reasons for Dental Extractions in France. J. Dent. Res. 1985, 64, 1087–1093. [Google Scholar] [CrossRef] [PubMed]
- Nusair, Y.M.; Younis, M.H.A. Prevalence, Clinical Picture, and Risk Factors of Dry Socket in a Jordanian Dental Teaching Center. J. Contemp. Dent. Pract. 2007, 8, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Abu Younis, M.H.; Abu Hantash, R.O. Dry Socket: Frequency, Clinical Picture, and Risk Factors in a Palestinian Dental Teaching Center. Open Dent. J. 2011, 5, 7–12. [Google Scholar] [CrossRef] [Green Version]
- Grossi, G.B.; Maiorana, C.; Garramone, R.A.; Borgonovo, A.; Creminelli, L.; Santoro, F. Assessing Postoperative Discomfort after Third Molar Surgery: A Prospective Study. J. Oral Maxillofac. Surg. 2007, 65, 901–917. [Google Scholar] [CrossRef]
- Bouloux, G.F.; Steed, M.B.; Perciaccante, V.J. Complications of Third Molar Surgery. Oral Maxillofac. Surg. Clin. N. Am. 2007, 19, 117–128. [Google Scholar] [CrossRef]
- Saravanan, K.; Santhosh Kumar, M.P. Assessment of Post Extraction Complications in Indians. Bioinformation 2021, 17, 1120–1125. [Google Scholar] [CrossRef]
- Akinbami, B.O.; Godspower, T. Dry Socket: Incidence, Clinical Features, and Predisposing Factors. Int. J. Dent. 2014, 2014, 796102. [Google Scholar] [CrossRef]
- Ghosh, A.; Aggarwal, V.R.; Moore, R. Aetiology, Prevention and Management of Alveolar Osteitis-A Scoping Review. J. Oral Rehabil. 2022, 49, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Bortoluzzi, M.C.; Manfro, R.; De Déa, B.E.; Dutra, T.C. Incidence of Dry Socket, Alveolar Infection, and Postoperative Pain Following the Extraction of Erupted Teeth. J. Contemp. Dent. Pract. 2010, 11, 33–40. [Google Scholar] [CrossRef]
- Giorgetti, A.P.O.; César Neto, J.B.; Casati, M.Z.; Sallum, E.A.; Nociti Júnior, F.H. Cigarette Smoke Inhalation Influences Bone Healing of Post-Extraction Tooth Socket: A Histometric Study in Rats. Braz. Dent. J. 2012, 23, 228–234. [Google Scholar] [CrossRef] [Green Version]
- Jiang, Y.; Zhou, X.; Cheng, L.; Li, M. The Impact of Smoking on Subgingival Microflora: From Periodontal Health to Disease. Front. Microbiol. 2020, 11, 66. [Google Scholar] [CrossRef] [PubMed]
- Chou, H.-H.; Lu, S.-L.; Wang, S.-T.; Huang, T.-H.; Chen, S.L.-S. The Association between Bone Mineral Density and Periodontal Disease in Middle-Aged Adults. Int. J. Environ. Res. Public Health 2021, 18, 3321. [Google Scholar] [CrossRef] [PubMed]
- Ramôa, C.P.; Eissenberg, T.; Sahingur, S.E. Increasing Popularity of Waterpipe Tobacco Smoking and Electronic Cigarette Use: Implications for Oral Healthcare. J. Periodontal. Res. 2017, 52, 813–823. [Google Scholar] [CrossRef]
- Ralho, A.; Coelho, A.; Ribeiro, M.; Paula, A.; Amaro, I.; Sousa, J.; Marto, C.; Ferreira, M.; Carrilho, E. Effects of Electronic Cigarettes on Oral Cavity: A Systematic Review. J. Evid.-Based Dent. Pract. 2019, 19, 101318. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- National Heart, Lung, and Blood Institute, National Institutes of Health. Study Quality Assessment Tools. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 22 August 2020).
- Oxford Centre for Evidence-Based Medicine. Levels of Evidence. Available online: https://www.cebm.net/2016/05/ocebm-levels-of-evidence (accessed on 22 August 2020).
- Al-Belasy, F.A. The Relationship of “Shisha” (Water Pipe) Smoking to Postextraction Dry Socket. J. Oral Maxillofac. Surg. 2004, 62, 10–14. [Google Scholar] [CrossRef]
- Alsaleh, M.K.; Alajlan, S.S.; Alateeq, N.F.; Alamer, N.S.; Alshammary, F.; Alhobeira, H.A.; Khan, S.; Siddiqui, A.A. Alveolar Osteitis: Patient’s Compliance with Post-Extraction Instructions Following Permanent Teeth Extraction. J. Contemp. Dent. Pract. 2018, 19, 1518–1525. [Google Scholar] [CrossRef]
- Bortoluzzi, M.C.; Capella, D.L.; Barbieri, T.; Marchetti, S.; Dresch, C.P.; Tirello, C. Does Smoking Increase the Incidence of Postoperative Complications in Simple Exodontia? Int. Dent. J. 2012, 62, 106–108. [Google Scholar] [CrossRef] [PubMed]
- Eshghpour, M.; Nejat, A.H. Dry Socket Following Surgical Removal of Impacted Third Molar in an Iranian Population: Incidence and Risk Factors. Niger. J. Clin. Pract. 2013, 16, 496–500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Halabí, D.; Escobar, J.; Muñoz, C.; Uribe, S. Logistic Regression Analysis of Risk Factors for the Development of Alveolar Osteitis. J. Oral Maxillofac. Surg. 2012, 70, 1040–1044. [Google Scholar] [CrossRef] [PubMed]
- Heng, C.K.; Badner, V.M.; Clemens, D.L.; Mercer, L.T.; Mercer, D.W. The Relationship of Cigarette Smoking to Postoperative Complications from Dental Extractions among Female Inmates. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 104, 757–762. [Google Scholar] [CrossRef] [PubMed]
- López-Carriches, C.; Gómez-Font, R.; Martínez-González, J.M.; Donado-Rodríguez, M. Influence of Smoking upon the Postoperative Course of Lower Third Molar Surgery. Med. Oral Patol. Oral Cir. Bucal 2006, 11, 56–60. [Google Scholar]
- Momeni, H.; Shahnaseri, S.; Hamzeheil, Z. Evaluation of Relative Distribution and Risk Factors in Patients with Dry Socket Referring to Yazd Dental Clinics. Dent. Res. J. 2011, 8, S84–S87. [Google Scholar]
- Parthasarathi, K.; Smith, A.; Chandu, A. Factors Affecting Incidence of Dry Socket: A Prospective Community-Based Study. J. Oral Maxillofac. Surg. 2011, 69, 1880–1884. [Google Scholar] [CrossRef]
- Schwartz-Arad, D.; Lipovsky, A.; Pardo, M.; Adut, O.; Dolev, E. Interpretations of Complications Following Third Molar Extraction. Quintessence Int. 2018, 49, 33–39. [Google Scholar] [CrossRef]
- Vettori, E.; Costantinides, F.; Nicolin, V.; Rizzo, R.; Perinetti, G.; Maglione, M.; Di Lenarda, R. Factors Influencing the Onset of Intra- and Post-Operative Complications Following Tooth Exodontia: Retrospective Survey on 1701 Patients. Antibiotics 2019, 8, 264. [Google Scholar] [CrossRef] [Green Version]

| Parameter | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | patients with dry socket—both genders, regardless of age | patients with other complications after tooth extraction |
| Intervention | smoking | |
| Comparison | non-smoking | |
| Outcomes | prevalence of dry socket | prevalence of dry socket with other predisposing factors, such as alcohol, contraceptives, or water pipe |
| Study design | case-control, cohort and cross-sectional studies | literature reviews, case reports, expert opinion, conference reports |
| published after 2000 | not published in English |
| Author, Year, Setting | Participants (F/M) | Age (Years) | Smoking Status (% of Smokers) | Inclusion Criteria | Exclusion Criteria | Comorbidities | Oral Hygiene Status |
|---|---|---|---|---|---|---|---|
| Al-Belasy, 2004, Egypt [21] | 200 (0/100) | mean 27 (range: 20–38) | 50.0 | patients who were treated at the Oral Surgery Department, Faculty of Dentistry, Mansoura University between January 2000 and February 2002, healthy patients required to have unilateral high mesioangular impactions of a mandibular third molar with an exposed occlusal surface | women, former smokers, men who smoked both cigarettes and shisha, patients with recent antibiotic use, and patients with medical need for prophylactic antibiotics | 100% no systemic disease | NR |
| Alsaleh et al., 2018 Kingdom of Saudi Arabia [22] | 201 (79/122) | NR | 26.4 | patients classified as ASA I (healthy patients) and ASA II (patients with mild, controlled systemic disease without functional limitation), patients with a history of nonsurgical extraction of a permanent tooth | patients who required treatment under general anaesthesia, children under 6 years of age who have not yet grown permanent teeth, and all patients with exodontia of primary teeth and retained teeth | 90.1% no systemic disease | NR |
| Bortoluzzi et al., 2012, Brazil [23] | 793 (337/456) | 41.6 ± 16.0 (range: 9–85) | 23.3 | simple and erupted teeth exodontia, procedures conducted by undergraduate students under similar conditions between March 2007 and December 2011 | extractions of third molars that had not fully erupted and/or were classified as difficult for undergraduate students to remove and extractions of deciduous teeth | NR | NR |
| Eshghpour & Nejat, 2013, Iran [24] | 189 (91/98) | 18–48 | 40.7 | extraction of impacted third mandibular molar teeth performed between April 2009 and August 2010 in Dental Clinic of Oral and Maxillofacial Surgery | NR | 86.0% no systemic disease | prior to surgery, all the patients underwent a thorough scaling and oral prophylaxis |
| Halabí et al., 2012, Chile [25] | 1302 (90/1212) | 39.7 ± 16 | 4.4 | patients who underwent dental extraction from March to June 2011 in dental clinic in Valdiva, Chile | extraction in the operating theatre necessary, residents of rural areas who did not present themselves for the follow-up, patients undergoing antimicrobial therapy | 96.8% no systemic disease | 8% poor oral hygiene |
| Heng et al., 2007 USA [26] | 219 (219/0) | mean 37.7 | 61.1 | inmates who had tooth extractions in the 8 months before the smoking ban (January 2004–August 2004) and 8 months after the ban (September 2004–April 2005) | inmates whose tooth extractions were performed at different times | NR | NR |
| López-Carriches et al., 2006, Spain [27] | 64 (46/18) | mean 23.5 (range: 18–53) | 48.4 | patients subjected to lower third molar extraction in the Unit of Oral and Maxillofacial Surgery (Madrid Complutense University, Spain), healthy volunteers over age 18 years and requiring surgical lower third molar extraction, absence of systemic disease, absence of any habitual medication | pregnant or nursing women, allergy to local anaesthetics, antibiotics, or analgesics, patients with cardiovascular disease or any other systemic pathology | 100% no systemic disease | 68.8% of the patients claimed not to have brushed in the zone at the time of suture removal |
| Momeni et al., 2011 Iran [28] | 4779 (2197/2581) | with dry socket 36.61 ± 13.59, without dry socket 42.86 ± 15.49 | 34.7 | patients referred to dental clinics in Yazd for tooth extraction between May 2010 and June 2010 | patients referred to dental clinics in Yazd for tooth extraction in another time period | 63.7% no systemic disease | 64% poor oral hygiene |
| Parthasarathi et al., 2011, Australia [29] | 284 (142/142) | NR | 30.8 | patients having an exodontia procedure at 4 comparable public dental clinics in Victoria between June and September 2008 | patients who underwent an exodontic procedure at 4 comparable public dental clinics in Victoria during a different time period | 47.0% no systemic disease | 85.3% poor oral hygiene |
| Schwartz-Arad et al., 2018, Israel [30] | 463 (257/206) | mean 29 (range: 13–75) | 26.0 | patients having third molar extractions at Schwartz Arad Surgical Center between 2001 and 2011 | patients having extractions of a tooth other than a third molar | NR | NR |
| Vettori et al., 2019, Italy [31] | 1701 (845/876) | 55.3 ± 19.9 | 29.7 | patients who underwent single or multiple tooth extractions between June 2015 and February 2016 at the University of Trieste | patients subjected to periodontal surgery or major oral surgery, patients without specification of which antibiotic was prescribed after extraction | 40.0% no systemic disease | caries was the reason of 57% extractions and periodontitis was of 31% |
| Study | Prevalence of Dry Socket in All Patients [%] | Prevalence of Dry Socket in Smokers [%] | Tooth Extracted | Extraction Technique | Symptoms Recognised as the Onset of Dry Socket | Provided Prophylaxis or Treatment |
|---|---|---|---|---|---|---|
| Al-Belasy, 2004 [21] | 11.5 | 16.0 | 100% impacted mandibular third molars | 100% atraumatic extractions | constant radiating pain not relieved by the analgesic, accompanied by a denuded socket or necrotic clot and a fetid smell | postoperative medications given orally for analgesia were naproxen or diflunisal at a dose of 500 mg twice daily; if dry socket was diagnosed, sockets were irrigated with saline and packed with a eugenol-iodoform dressing |
| Alsaleh et al., 2018 [22] | 7.0 | 9.4 | all teeth except retained third molars | single tooth extractions | severe pain at the extraction site within 3 days, no blood clot at the extraction site, visible bone at the extraction site, bad breath, bad taste in mouth | patients were given post-extraction instructions verbally after the extraction |
| Bortoluzzi et al., 2012 [23] | 1.3 | 2.7 | all kinds of fully erupted teeth | 12% traumatic extractions, 88% simple extractions | NR | NR |
| Eshghpour & Nejat, 2013 [24] | 25.9 | 35.1 | 100% impacted mandibular third molars | 100% traumatic extractions | 1 to 3 days after extraction with severe pain, halitosis, foul taste, and regional lymphadenitis; no blood clot in the socket and the bone is exposed | flap sutured using 3-0 silk suture; regimen of amoxicillin (500 mg) and Gelofen (400 mg cap, TID, for maximum 3 days) was prescribed |
| Halabí et al., 2012 [25] | 6.1 | 57.9 | 93.6% maxillary, 6.4% mandibular | 4.9% traumatic extractions, 95.1% simple extractions | increasing postoperative pain intensity for 4 days within and around the socket and/or total or partial breakdown of the blood clot in the socket with or without bone exposure | reported measures for alleviating alveolar osteitis in high-risk patients include local treatment with tetracycline or preoperative and 7-day postoperative rinsing with 0.12% chlorhexidine |
| Heng et al., 2007 [26] | 5.0 | 6.7 | 83.1% maxillary, 16.9% mandibular | 27.9% traumatic extractions, 72.1% simple extractions | alveolar osteitis, pain, swelling, bleeding | patients received a verbal and written postoperative recommendation, usually ibuprofen as an analgesic; for postoperative complaints, patients had open access to the clinic |
| López-Carriches et al., 2006 [27] | 3.1 | 6.5 | 100% lower third molar | NR | wound appearance and condition were assessed in terms of colour, marginal swelling, ulceration, the presence of plaque | no antibiotic treatment was prescribed postoperatively, and the patients received only metamizole as analgesic treatment, diclofenac was also prescribed as antiinflammatory treatment |
| Momeni et al., 2011 [28] | 0.6 | 0.6 | 36.3% maxillary, 63.7% mandibular | NR | throbbing pain, oral malodour, and unpleasant taste; onset of symptoms 42–72 h after tooth extraction and there is no redness or purulent discharge at the affected sites | palliative intervention with prescribing anti-inflammatory drugs |
| Parthasarathi et al., 2011 [29] | 4.2 | 4.6 | 38.8% maxillary, 61.2% mandibular | 17% traumatic extractions, 83% simple extractions | the patient’s history of pain and the presence of exposed bone, intraorally | NR |
| Schwartz-Arad et al., 2018 [30] | 11.7 | 33.3 | 100% third molar extraction | NR | NR | all patients were prescribed oral antibiotics (amoxicillin 1.5 g for 5 days) or clindamycin (1.2 mg for 4 days), and dexamethasone (4 mg for 2 days); rinsing with 0.25% chlorohexidine continued twice a day for 10 days after extraction; naproxen was provided as a nonsteroidal anti-inflammatory drug twice a day |
| Vettori et al., 2019 [31] | 3.2 | 5.5 | 51% maxillary, 49% mandibular | 15.7% traumatic extractions, 84.3% simple extractions | NR | almost all surgical sites had been sutured, in 10.47% of cases the patient had started an antibiotic therapy before the intervention; after the intervention, the surgeon prescribed antibiotic therapy to 9.23% of patients, steroids to 0.24% of patients, NSAIDs to 3% of patients |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuśnierek, W.; Brzezińska, K.; Nijakowski, K.; Surdacka, A. Smoking as a Risk Factor for Dry Socket: A Systematic Review. Dent. J. 2022, 10, 121. https://doi.org/10.3390/dj10070121
Kuśnierek W, Brzezińska K, Nijakowski K, Surdacka A. Smoking as a Risk Factor for Dry Socket: A Systematic Review. Dentistry Journal. 2022; 10(7):121. https://doi.org/10.3390/dj10070121
Chicago/Turabian StyleKuśnierek, Weronika, Kaja Brzezińska, Kacper Nijakowski, and Anna Surdacka. 2022. "Smoking as a Risk Factor for Dry Socket: A Systematic Review" Dentistry Journal 10, no. 7: 121. https://doi.org/10.3390/dj10070121
APA StyleKuśnierek, W., Brzezińska, K., Nijakowski, K., & Surdacka, A. (2022). Smoking as a Risk Factor for Dry Socket: A Systematic Review. Dentistry Journal, 10(7), 121. https://doi.org/10.3390/dj10070121









