Development of a Clinically Relevant Index for Tooth Wear Treatment Needs
Abstract
1. Introduction
| Year | Author | Aim of the Index |
|---|---|---|
| Erosion classification systems | ||
| 1978 | Eccles | Early classification of erosion TSL of industrial origin [10]. |
| 1979 | Eccles | Modified erosional TSL index of nonindustrial origin [10]. |
| 1983 | Xhonga and Valdmanis | Considering extent of erosion in addition to severity [6]. |
| Indices based on Tooth Wear Index (TWI) | ||
| 1984 | Smith and Knight | Evaluate TSL severity regardless of the etiology [9]. |
| 1994 | Millward et al. | Adopt TWI criteria to measure erosion TSL in children [17] |
| 2004 | Bardsley et al. | Simplified version of TWI to evaluate erosion TSL in children [12]. |
| TSL indices concentrating on treatment needs | ||
| 1987 | Oil et al. | Tried to provide reliable method to determine the treatment needs for each case [18]. |
| 1989 | Dahl et al. | Modification of Oilo et al.’s criteria [19]. |
| 2000 | Larsen et al. | First use of photograph as supplementary tool, with clinical examination [20]. |
| 2008 | Bartlett et al. | (BEWE) index to provide easy and reproducible diagnostic criteria [13]. |
| 2014 | Sawai | Simplified indices for cervical lesions [21]. |
| 2016 | Wetselaar and Lobbezoo | Aimed to provide comprehensive tooth wear evaluation system (TWES) [22]. |
| Use of casts and Three-dimensional methods to classify TSL | ||
| 2010 | Al-Omiri et al. | Use three-dimensional tools to classify TSL [23]. |
| 2015 | Lee et al. | Compared the change in tooth volume in a longitudinal comparison of the change in line angles on the occlusal surface of each tooth [15]. |
| 2018 | Soo-Hyun Kim et al. | New tooth wear index (NTWI) describing methods for quantitative measurement of tooth wear using the area and volume of virtual model cusps [15]. |
2. Materials and Methods
2.1. Study Design
2.2. Ethical Considerations
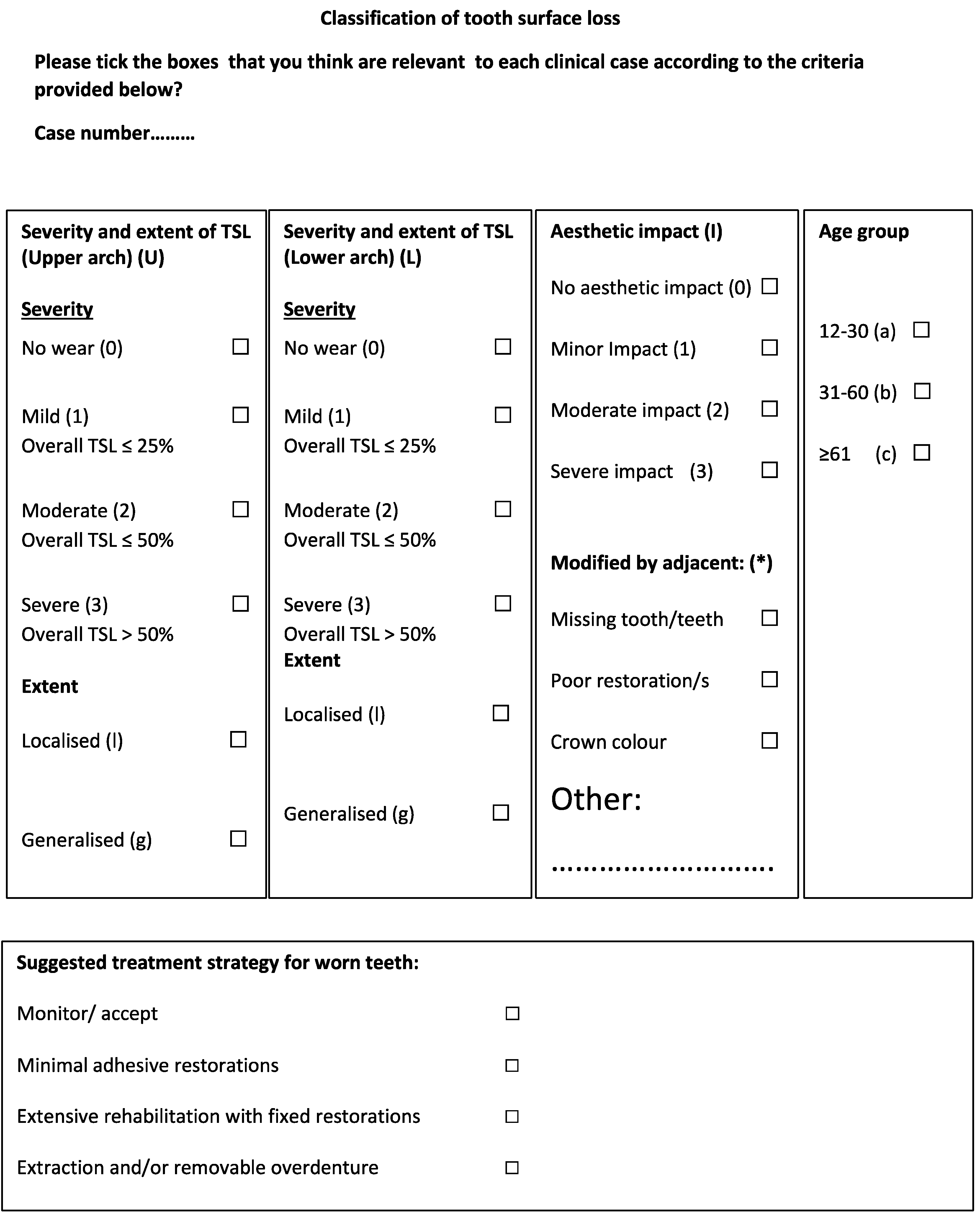
2.3. Developing the Classification System Tools
- No aesthetic impact when the TSL did not cause a noticeable aesthetic impact.
- Minor when there was noticeable TSL on the labial surface or incisal edge, but this did not affect the facial profile and aesthetic appearance.
- Moderate when there was a slight loss of OVD and the facial profile appearance had a noticeable TSL but was not severe.
- Severe aesthetic impact when the TSL was severe and the patient had a severe reduction in OVD with a severely unacceptable appearance due to The TSL itself.
2.4. Testing the Validity of the Tools
2.5. Analysis
3. Results
3.1. Severity Classification of Anterior Teeth of Maxillary Arch
3.2. Severity Classification of Posterior Teeth of Maxillary Arch
3.3. Severity Classification of Anterior Teeth of Mandibular Arch
3.4. Severity Classification of Posterior Teeth of Mandibular Arch
3.5. Aesthetic Impact Classification
3.6. Treatment Option Results
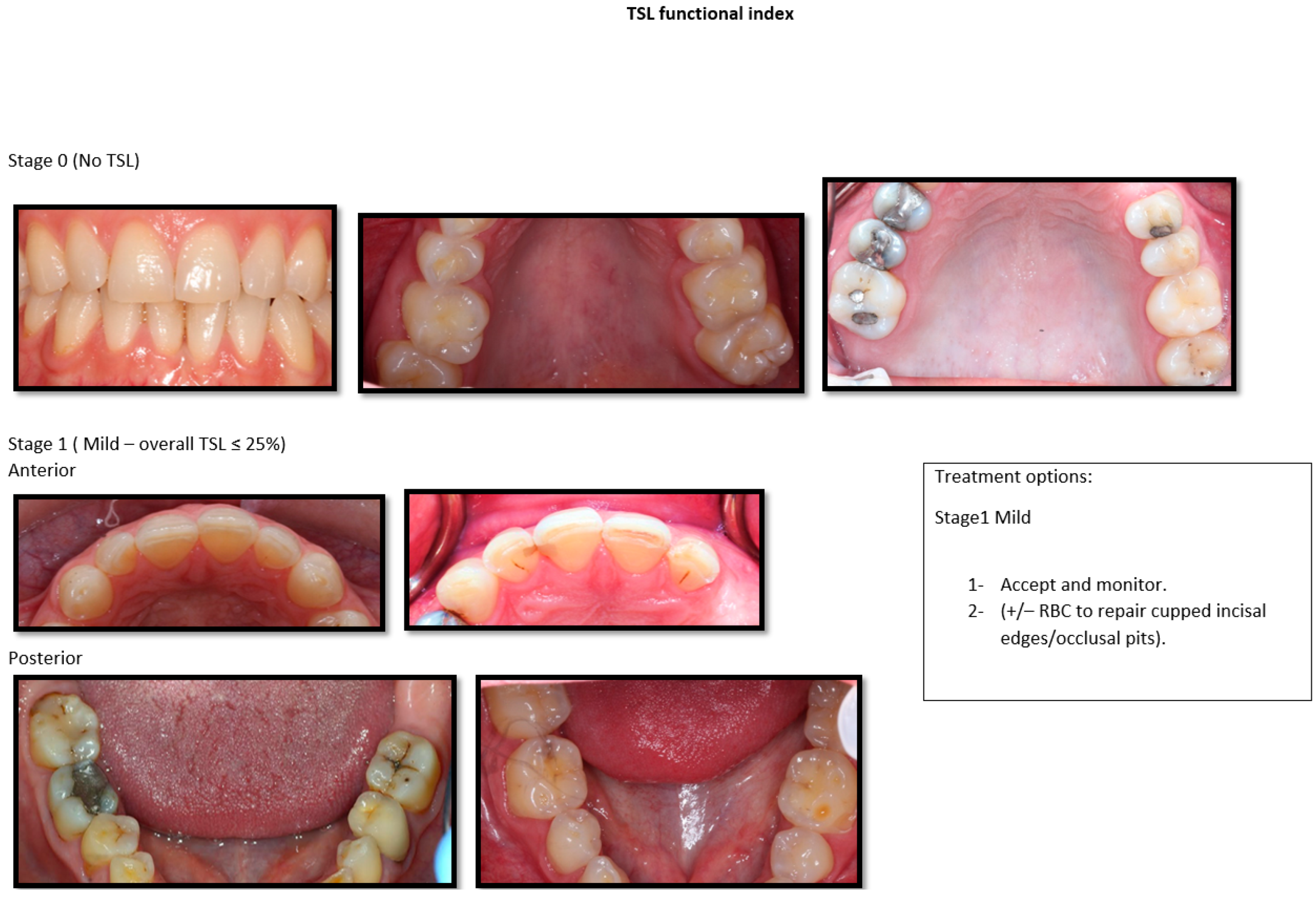
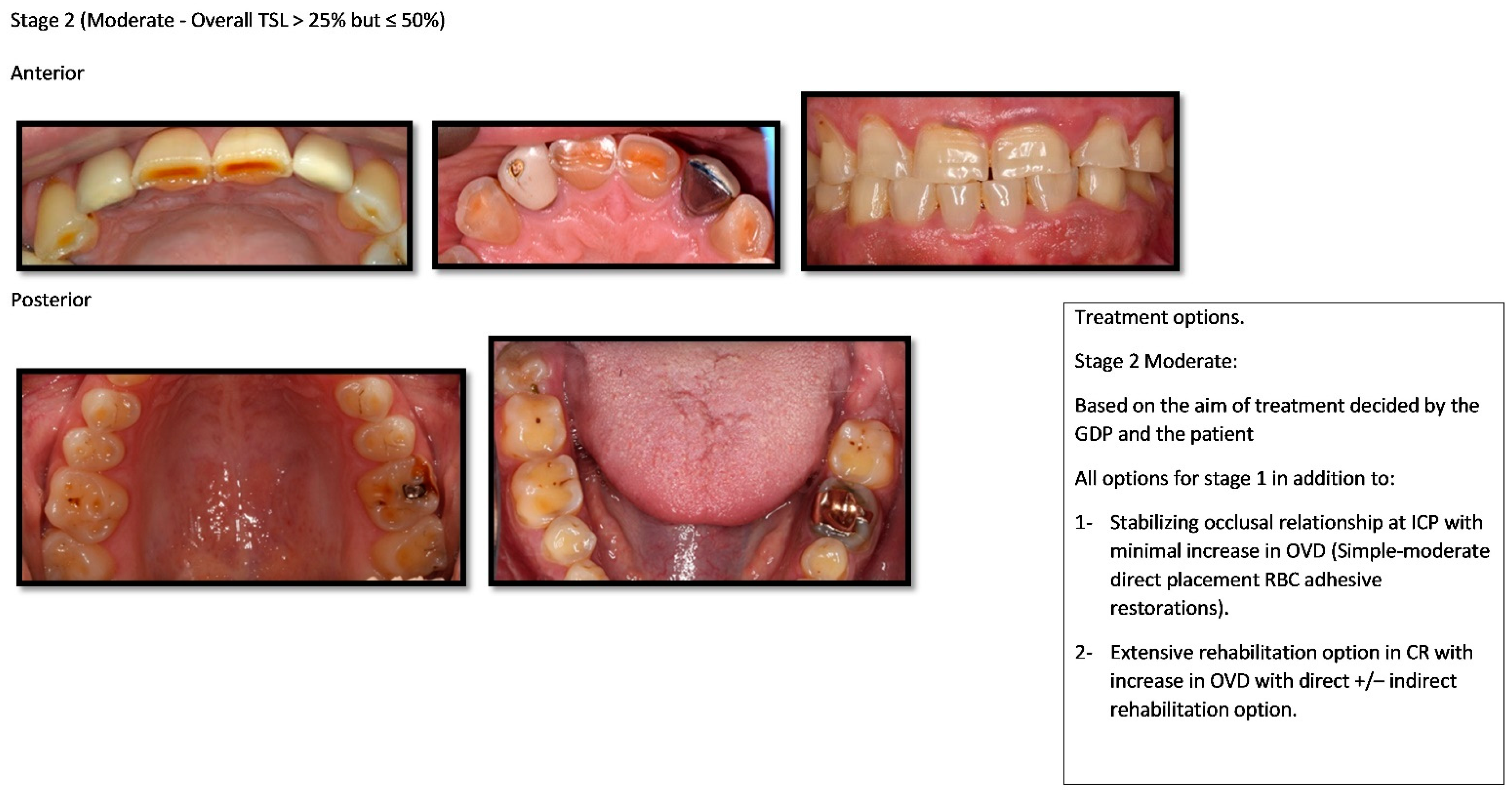
3.7. Providing the Photographic Index Based on Examiners Classification
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| TSL | Tooth Surface Loss |
| OVD | Occlusal Vertical Dimension |
| IOTN | Index for Orthodontic Treatment Needs |
| TWI | Tooth Wear Index |
| BEWE | Basic Erosive Wear Examination |
| CAD-CAM | Computer Aided Design—Computer Aided Manufacturing |
| CCDH | Charles Clifford dental hospital |
| BPE | Basic Periodontal Examination |
References
- Cunha-Cruz, J.; Pashova, H.; Packard, J.D.; Zhou, L.; Hilton, T.J. Tooth wear: Prevalence and associated factors in general practice patients. Community Dent. Oral Epidemiol. 2010, 38, 228–234. [Google Scholar] [CrossRef]
- Ahmed, K.E.; Murbay, S. Survival rates of anterior composites in managing tooth wear: Systematic review. J. Oral Rehabil. 2016, 43, 145–153. [Google Scholar] [CrossRef]
- Bartlett, D.W.; Lussi, A.; West, N.X.; Bouchard, P.; Sanz, M.; Bourgeois, D. Prevalence of tooth wear on buccal and lingual surfaces and possible risk factors in young European adults. J. Dent. 2013, 41, 1007–1013. [Google Scholar] [CrossRef]
- Li, M.H.M.; Bernabé, E. Tooth wear and quality of life among adults in the United Kingdom. J. Dent. 2016, 55, 48–53. Available online: http://linkinghub.elsevier.com/retrieve/pii/S0300571216301890 (accessed on 3 November 2018). [CrossRef]
- Todic, J.; Mitic, A.; Lazic, D.; Radosavljevic, R.; Staletovic, M. Effects of bruxism on the maximum bite force. Vojnosanit. Pregl. 2017, 74, 138–144. Available online: http://www.doiserbia.nb.rs/Article.aspx?ID=0042-84501600165T (accessed on 15 March 2018). [CrossRef]
- Geographic Comparisons of the Incidence of Dental Erosion: A Two Centre Study. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2842.1983.tb00121.x (accessed on 2 March 2022).
- Vanuspong, W.; Eisenburger, M.; Addy, M. Cervical tooth wear and sensitivity: Erosion, softening and rehardening of dentine; effects of pH, time and ultrasonication. J. Clin. Periodontol. 2002, 29, 351–357. Available online: http://dx.doi.org/10.1034/j.1600-051X.2002.290411.x (accessed on 20 May 2016). [CrossRef]
- Katsoulis, J.; Nikitovic, S.G.; Spreng, S.; Neuhaus, K.; Mericske-Stern, R. Prosthetic rehabilitation and treatment outcome of partially edentulous patients with severe tooth wear: 3-Years results. J. Dent. 2011, 39, 662–671. [Google Scholar] [CrossRef]
- Bardsley, P.F. The evolution of tooth wear indices. Clin. Oral Investig. 2008, 12 (Suppl. S1), 15–19. [Google Scholar] [CrossRef]
- Eccles, J.D. Dental erosion of nonindustrial origin. A clinical survey and classification. J. Prosthet. Dent. 1979, 42, 649–653. [Google Scholar] [CrossRef]
- Ganss, C.; Lussi, A. Current erosion indices—Flawed or valid? Clin. Oral Investig. 2008, 12, 1–3. Available online: http://link.springer.com/10.1007/s00784-007-0182-4 (accessed on 8 May 2016). [CrossRef]
- Bardsley, P.F.; Taylor, S.; Milosevic, A. Epidemiological studies of tooth wear and dental erosion in 14-year-old children in North West England. Part 1: The relationship with water fluoridation and social deprivation. Br. Dent. J. 2004, 197, 413–416. [Google Scholar] [CrossRef]
- Bartlett, D.; Ganss, C.; Lussi, A. Basic Erosive Wear Examination (BEWE): A new scoring system for scientific and clinical needs. Clin. Oral Investig. 2008, 12 (Suppl. S1), 65–68. [Google Scholar] [CrossRef]
- Bartlett, D. Summary of: Evaluation of the basic erosive wear examination (BEWE) for use in general dental practice. Br. Dent. J. 2012, 213, 128–129. Available online: http://www.ncbi.nlm.nih.gov/pubmed/22878338 (accessed on 15 January 2018). [CrossRef][Green Version]
- Kim, S.H.; Park, Y.S.; Kim, M.K.; Kim, S.; Lee, S.P. Methods for quantitative measurement of tooth wear using the area and volume of virtual model cusps. J. Periodontal. Implant. Sci. 2018, 48, 124–134. [Google Scholar] [CrossRef]
- Brook, P.H.; Shaw, W.C. The development of an index of orthodontic treatment priority. Eur. J. Orthod. 1989, 11, 309–320. Available online: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L19501578%0Ahttp://limo.libis.be/resolver?&sid=EMBASE&issn=01415387&id=doi:&atitle=The+development+of+an+index+of+orthodontic+treatment+priority.&stitle=Eur+J+Orthod&title=European+j (accessed on 4 December 2016). [CrossRef]
- Millward, A.; Shaw, L.; Smith, A.J.; Rippin, J.W.; Harrington, E. The distribution and severity of tooth wear and the relationship between erosion and dietary constituents in a group of children. Int. J. Paediatr. Dent. 1994, 4, 151–157. [Google Scholar] [CrossRef]
- Oilo, G.; Dahl, B.L.; Hatle, G.; Gad, A.L. An index for evaluating wear of teeth. Acta Odontol. Scand. 1987, 45, 361–365. [Google Scholar] [CrossRef]
- Dahl, B.L.; Oilo, G.; Andersen, A.; Bruaset, O. The suitability of a new index for the evaluation of dental wear. Acta Odontol. Scand. 1989, 47, 205–210. [Google Scholar] [CrossRef]
- Larsen, I.B.; Westergaard, J.; Stoltze, K.; Larsen, A.I.; Gyntelberg, F.; Holmstrup, P. A clinical index for evaluating and monitoring dental erosion. Community Dent. Oral Epidemiol. 2000, 28, 211–217. Available online: http://www.ncbi.nlm.nih.gov/pubmed/10830648 (accessed on 12 January 2017). [CrossRef]
- Sawai, M. An easy classification for dental cervical abrasions. Dent. Hypotheses 2014, 5, 142. Available online: http://www.dentalhypotheses.com/text.asp?2014/5/4/142/140589 (accessed on 20 March 2018). [CrossRef]
- Wetselaar, P.; Lobbezoo, F. The tooth wear evaluation system: A modular clinical guideline for the diagnosis and management planning of worn dentitions. J. Oral Rehabil. 2016, 43, 69–80. [Google Scholar] [CrossRef]
- AL-Omiri, M.K.; Harb, R.; Hammad, O.A.A.; Lamey, P.J.; Lynch, E.; Clifford, T.J. Quantification of tooth wear: Conventional vs new method using toolmakers microscope and a three-dimensional measuring technique. J. Dent. 2010, 38, 560–568. Available online: http://dx.doi.org/10.1016/j.jdent.2010.03.016 (accessed on 23 May 2018). [CrossRef]
- Satterthwaite, J.D. Tooth surface loss: Tools and tips for management. Dent. Update 2017, 39, 86–96. [Google Scholar] [CrossRef]
- Chu, F.C.S.; Chow, T.W.; Smales, R.J.; Newsome, P.R.H.; Siu, A.S.C. Restorative Management of the Worn Dentition: 4. Generalized Toothwear. Dent. Update 2017, 29, 318–324. [Google Scholar] [CrossRef][Green Version]
- Abduo, J.; Lyons, K. Clinical considerations for increasing occlusal vertical dimension: A review. Aust. Dent. J. 2012, 57, 2–10. [Google Scholar] [CrossRef]
- Lee, S.; Nam, S.; Lee, S. Evaluation of the effectiveness of the new tooth wear measurement parameters. Anat. Cell Biol. 2015, 48, 284–291. [Google Scholar] [CrossRef]
- Dawood, A.; Patel, S. The Dental Practicality Index-assessing the restorability of teeth. Br. Dent. J. 2017, 222, 755–758. Available online: https://doi.org/10.1038/sj.bdj.2017.447 (accessed on 7 February 2019). [CrossRef]
- McDonald, A.; Setchell, D. Developing a tooth restorability index. Dent. Update 2005, 32, 343–384. [Google Scholar] [CrossRef]
- West, N.X.; Joiner, A. Enamel mineral loss. J. Dent. 2014, 42, S2–S11. Available online: https://doi.org/10.1016/S0300-5712(14)50002-4 (accessed on 14 June 2018). [CrossRef]
- Al-Khayatt, A.S.; Ray-Chaudhuri, A.; Poyser, N.J.; Briggs, P.F.A.; Porter, R.W.J.; Kelleher, M.G.D.; Eliyas, S. Direct composite restorations for the worn mandibular anterior dentition: A 7-year follow-up of a prospective randomised controlled split-mouth clinical trial. J. Oral Rehabil. 2013, 40, 389–401. [Google Scholar] [CrossRef]


| 95% Confidence Interval | |||
|---|---|---|---|
| Intraclass Correlation | Lower Bound | Upper Bound | |
| Maxillary anterior arch | 0.805 | 0.70 | 0.91 |
| Maxillary posterior arch | 0.81 | 0.71 | 0.91 |
| Mandibular anterior arch | 0.845 | 0.76 | 0.93 |
| Mandibular posterior arch | 0.76 | 0.64 | 0.88 |
| Aesthetic impact | 0.825 | 0.73 | 0.92 |
| Number of samples | Number of Examiners Scored Grades 0–3 for Each Sample | ||||||||
| Maxillary anterior | Maxillary posterior | ||||||||
| 0 | 1 | 2 | 3 | 0 | 1 | 2 | 3 | ||
| 1 | 3 | 7 | 1 | 9 | |||||
| 2 | 10 | 3 | 7 | ||||||
| 3 | 1 | 9 | 8 | 2 | |||||
| 4 | 2 | 8 | 1 | 9 | |||||
| 5 | 2 | 1 | 7 | 8 | 2 | ||||
| 6 | 2 | 8 | 7 | 3 | |||||
| 7 | 3 | 7 | 1 | 9 | |||||
| 8 | 1 | 2 | 7 | 3 | 6 | 1 | |||
| 9 | 10 | 2 | 7 | 1 | |||||
| 10 | 5 | 5 | 1 | 9 | |||||
| 11 | 1 | 9 | 3 | 7 | |||||
| 12 | 7 | 3 | 7 | 3 | |||||
| 13 | 2 | 8 | 9 | 1 | |||||
| 14 | 2 | 6 | 2 | 8 | 2 | ||||
| 15 | 2 | 6 | 2 | 5 | 5 | ||||
| 16 | 5 | 5 | 1 | 9 | |||||
| 17 | 10 | 7 | 3 | ||||||
| 18 | 10 | 4 | 6 | ||||||
| 19 | 8 | 2 | 7 | 3 | |||||
| 20 | 3 | 7 | 1 | 9 | |||||
| Number of samples | Number of Examiners Scored Grades 0–3 for Each Sample | ||||||||
| Mandibular anterior | Mandibular posterior | ||||||||
| 0 | 1 | 2 | 3 | 0 | 1 | 2 | 3 | ||
| 1 | 1 | 9 | 8 | 2 | |||||
| 2 | 1 | 9 | 8 | 2 | |||||
| 3 | 1 | 6 | 3 | 8 | 2 | ||||
| 4 | 9 | 1 | 2 | 8 | |||||
| 5 | 8 | 2 | 7 | 3 | |||||
| 6 | 10 | 1 | 9 | ||||||
| 7 | 1 | 7 | 2 | 2 | 8 | ||||
| 8 | 10 | 3 | 7 | ||||||
| 9 | 1 | 5 | 4 | 2 | 1 | 7 | |||
| 10 | 3 | 7 | 8 | 2 | |||||
| 11 | 1 | 3 | 6 | 4 | 6 | ||||
| 12 | 9 | 1 | 7 | 3 | |||||
| 13 | 6 | 4 | 5 | 5 | |||||
| 14 | 10 | 10 | |||||||
| 15 | 8 | 2 | 3 | 7 | |||||
| 16 | 4 | 6 | 8 | 2 | |||||
| 17 | 1 | 8 | 1 | 3 | 6 | 1 | |||
| 18 | 4 | 6 | 1 | 9 | |||||
| 19 | 9 | 1 | 2 | 8 | |||||
| 20 | 1 | 9 | 1 | 9 | |||||
| Number of samples | Number of Examiners Scored Grades 0–3 for Each Sample | ||||
| 0 | 1 | 2 | 3 | ||
| 1 | 8 | 2 | |||
| 2 | 10 | ||||
| 3 | 1 | 9 | |||
| 4 | 8 | 2 | |||
| 5 | 1 | 9 | |||
| 6 | 6 | 4 | |||
| 7 | 1 | 1 | 8 | ||
| 8 | 1 | 9 | |||
| 9 | 1 | 9 | |||
| 10 | 1 | 8 | 1 | ||
| 11 | 5 | 5 | |||
| 12 | 8 | 2 | |||
| 13 | 9 | 1 | |||
| 14 | 3 | 7 | |||
| 15 | 1 | 9 | |||
| 16 | 8 | 2 | |||
| 17 | 10 | ||||
| 18 | 3 | 7 | |||
| 19 | 1 | 9 | |||
| 20 | 1 | 1 | 8 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deeban, Y.; Moharamzadeh, K.; Abuzayeda, M.; Martin, N. Development of a Clinically Relevant Index for Tooth Wear Treatment Needs. Dent. J. 2022, 10, 80. https://doi.org/10.3390/dj10050080
Deeban Y, Moharamzadeh K, Abuzayeda M, Martin N. Development of a Clinically Relevant Index for Tooth Wear Treatment Needs. Dentistry Journal. 2022; 10(5):80. https://doi.org/10.3390/dj10050080
Chicago/Turabian StyleDeeban, Yahya, Keyvan Moharamzadeh, Moosa Abuzayeda, and Nicolas Martin. 2022. "Development of a Clinically Relevant Index for Tooth Wear Treatment Needs" Dentistry Journal 10, no. 5: 80. https://doi.org/10.3390/dj10050080
APA StyleDeeban, Y., Moharamzadeh, K., Abuzayeda, M., & Martin, N. (2022). Development of a Clinically Relevant Index for Tooth Wear Treatment Needs. Dentistry Journal, 10(5), 80. https://doi.org/10.3390/dj10050080








