Antibiotics Efficiency in the Infection Complications Prevention after Third Molar Extraction: A Systematic Review
Abstract
1. Introduction
Prescribing Antibiotics in Dentistry
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Sources of Information
2.3. Search Strategy
2.4. Selection of Studies
Exclusion and Inclusion Criteria
- The articles published before 1 July 2011;
- In vitro studies or animals;
- Not full texts;
- Patients with other accompanying diseases;
- Inappropriate information in articles; or
- Articles with 2 groups, one of which was a placebo group.
- Randomized controlled trials (RCTs) in humans;
- Third molar extraction;
- Antibiotic prophylaxis (e.g., prevention);
- Sex: men and women;
- Age: 18+; and
- Amoxicillin use.
2.5. Data Collection Process and Items
2.6. Study Risk of Bias Assessment
- The randomization process;
- Deviations from intended interventions;
- Missing outcome data;
- Measurement of the outcome; and
- Selection of the reported result.
3. Results
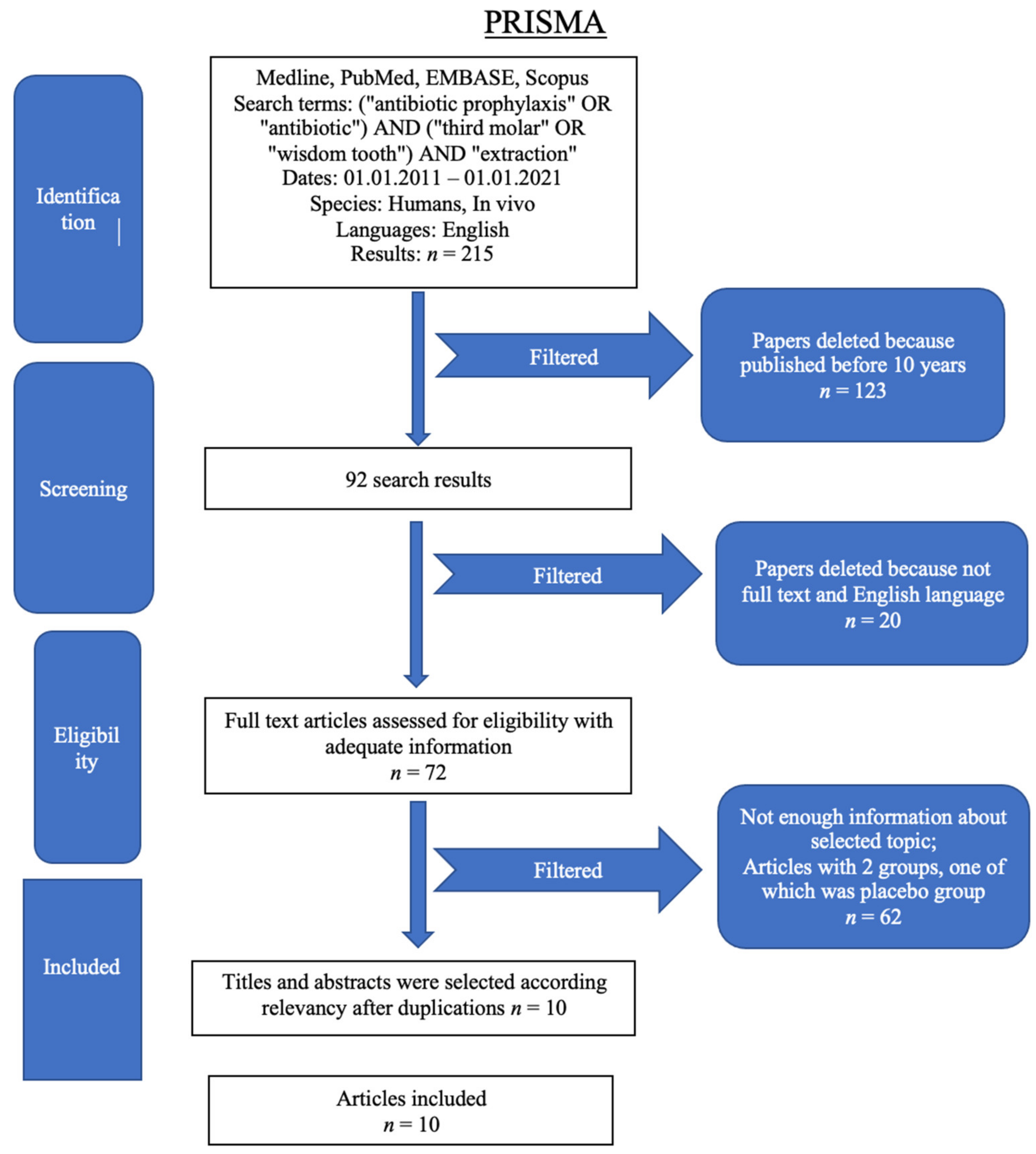
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias within Studies
4. Discussion
Review Study Discussion
5. Conclusions
6. Other Information
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lodi, G.; Sardella, A.; Salis, A.; Demarosi, F.; Tarozzi, M.; Carrassi, A. Tooth Extraction in Patients Taking Intravenous Bisphosphonates: A Preventive Protocol and Case Series. J. Oral Maxillofac. Surg. 2010, 68, 107–110. [Google Scholar] [CrossRef] [PubMed]
- WHO Publishes List of Bacteria for Which New Antibiotics Are Urgently Needed. Available online: https://www.who.int/news/item/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed (accessed on 12 April 2022).
- Abushaheen, M.A.; Muzaheed; Fatani, A.J.; Alosaimi, M.; Mansy, W.; George, M.; Acharya, S.; Rathod, S.; Divakar, D.D.; Jhugroo, C.; et al. Antimicrobial Resistance, Mechanisms and Its Clinical Significance. Dis. Mon. 2020, 66, 100971. [Google Scholar] [CrossRef] [PubMed]
- Ramu, C.; Padmanabhan, T.V. Indications of Antibiotic Prophylaxis in Dental Practice- Review. Asian Pac. J. Trop. Biomed. 2012, 2, 749. [Google Scholar] [CrossRef]
- Sayed, N.; Bakathir, A.; Pasha, M.; Al-Sudairy, S. Complications of Third Molar Extraction: A Retrospective Study from a Tertiary Healthcare Centre in Oman. Sultan Qaboos Univ. Med. J. 2019, 19, e230. [Google Scholar] [CrossRef]
- Chen, Y.W.; Lee, C.T.; Hum, L.; Chuang, S.K. Effect of Flap Design on Periodontal Healing after Impacted Third Molar Extraction: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Surg. 2017, 46, 363–372. [Google Scholar] [CrossRef]
- Varvara, G.; Bernardi, S.; Piattelli, M.; Cutilli, T. Rare and Life-Threatening Complication after an Attempted Lower Third Molar Extraction: Lemierre Syndrome. Ann. R. Coll. Surg. Engl. 2019, 101, e52. [Google Scholar] [CrossRef]
- Menon, R.K.; Gopinath, D.; Li, K.Y.; Leung, Y.Y.; Botelho, M.G. Does the Use of Amoxicillin/Amoxicillin–Clavulanic Acid in Third Molar Surgery Reduce the Risk of Postoperative Infection? A Systematic Review with Meta-Analysis. Int. J. Oral Maxillofac. Surg. 2019, 48, 263–273. [Google Scholar] [CrossRef]
- Marchionni, S.; Toti, P.; Barone, A.; Covani, U.; Esposito, M. The Effectiveness of Systemic Antibiotic Prophylaxis in Preventing Local Complications after Tooth Extraction. A Systematic Review. Eur. J. Oral Implantol. 2017, 10, 127–132. [Google Scholar]
- Arteagoitia, M.I.; Barbier, L.; Santamaría, J.; Santamaría, G.; Ramos, E. Efficacy of Amoxicillin and Amoxicillin/Clavulanic Acid in the Prevention of Infection and Dry Socket after Third Molar Extraction. A Systematic Review and Meta-Analysis. Med. Oral Patol. Oral Y Cir. Bucal 2016, 21, e494–e504. [Google Scholar] [CrossRef]
- Blatt, S.; Al-Nawas, B. A Systematic Review of Latest Evidence for Antibiotic Prophylaxis and Therapy in Oral and Maxillofacial Surgery; Springer: Berlin/Heidelberg, Germany, 2019; Volume 47, ISBN 0123456789. [Google Scholar]
- Ramos, E.; Santamaría, J.; Santamaría, G.; Barbier, L.; Arteagoitia, I. Do Systemic Antibiotics Prevent Dry Socket and Infection after Third Molar Extraction? A Systematic Review and Meta-Analysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 122, 403–425. [Google Scholar] [CrossRef]
- Yoshida, H.; Matsuda, S.; Aratani, T.; Tsukamoto, H.; Yoshimura, H.; Sano, K.; Iwasaki, H. Collaboration with an Infection Control Team Promoted Appropriate Antibiotic Use for Third Molar Extraction at a Japanese Hospital. J. Infect. Chemother. 2020, 26, 531–534. [Google Scholar] [CrossRef] [PubMed]
- Gill, A.S.; Morrissey, H.; Rahman, A. A Systematic Review and Meta-Analysis Evaluating Antibiotic Prophylaxis in Dental Implants and Extraction Procedures. Medicina 2018, 54, 95. [Google Scholar] [CrossRef] [PubMed]
- Guerrini, L.; Monaco, A.; Pietropaoli, D.; Ortu, E.; Giannoni, M.; Marci, M.C. Antibiotics in Dentistry: A Narrative Review of Literature and Guidelines Considering Antibiotic Resistance. Open Dent. J. 2019, 13, 383–398. [Google Scholar] [CrossRef]
- Lodi, G.; Azzi, L.; Varoni, E.M.; Pentenero, M.; del Fabbro, M.; Carrassi, A.; Sardella, A.; Manfredi, M. Antibiotics to Prevent Complications Following Tooth Extractions. Cochrane Database Syst. Rev. 2021, 2, CD003811. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef]
- López-Cedrún, J.L.; Pijoan, J.I.; Fernández, S.; Santamaria, J.; Hernandez, G. Efficacy of Amoxicillin Treatment in Preventing Postoperative Complications in Patients Undergoing Third Molar Surgery: A Prospective, Randomized, Double-Blind Controlled Study. J. Oral Maxillofac. Surg. 2011, 69, e5–e14. [Google Scholar] [CrossRef]
- Siddiqi, A.; Morkel, J.A.; Zafar, S. Antibiotic Prophylaxis in Third Molar Surgery: A Randomized Double-Blind Placebo-Controlled Clinical Trial Using Split-Mouth Technique. Int. J. Oral Maxillofac. Surg. 2010, 39, 107–114. [Google Scholar] [CrossRef]
- Sisalli, U.; Lalli, C.; Carone, L.; Maida, S.; Manzoli, L.; Serra, E.; Dolci, M. Amoxicillin and Clavulanic Acid vs Ceftazidime in the Surgical Extraction of Impacted Third Molar: A Comparative Study. Int. J. Immunopathol. Pharmacol. 2012, 25, 771–774. [Google Scholar] [CrossRef]
- Duvall, N.B.; Fisher, T.D.; Hensley, D.; Hancock, R.H.; Vandewalle, K.S. The Comparative Efficacy of 0.12% Chlorhexidine and Amoxicillin to Reduce the Incidence and Magnitude of Bacteremia during Third Molar Extractions: A Prospective, Blind, Randomized Clinical Trial. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 115, 752–763. [Google Scholar] [CrossRef]
- Bortoluzzi, M.C.; Capella, D.L.; Barbieri, T.; Pagliarini, M.; Cavalieri, T.; Manfro, R. A Single Dose of Amoxicillin and Dexamethasone for Prevention of Postoperative Complications in Third Molar Surgery: A Randomized, Double-Blind, Placebo Controlled Clinical Trial. J. Clin. Med. Res. 2013, 5, 26. [Google Scholar] [CrossRef][Green Version]
- Iglesias-Martín, F.; García-Perla-García, A.; Yañez-Vico, R.; Aced-Jiménez, E.; Arjona-Gerveno, E.; González-Padilla, J.D.; Gutierrez-Pérez, J.L.; Torres-Lagares, D. Comparative Trial between the Use of Amoxicillin and Amoxicillin Clavulanate in the Removal of Third Molars. Med. Oral Patol. Oral Y Cirugía Bucal 2014, 19, e612. [Google Scholar] [CrossRef] [PubMed]
- Milani, B.A.; Bauer, H.C.; Sampaio-Filho, H.; Horliana, A.C.R.T.; Perez, F.E.G.; Tortamano, I.P.; Jorge, W.A. Antibiotic Therapy in Fully Impacted Lower Third Molar Surgery: Randomized Three-Arm, Double-Blind, Controlled Trial. Oral Maxillofac. Surg. 2015, 19, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Braimah, R.O.; Ndukwe, K.C.; Owotade, J.F.; Aregbesola, S.B. Impact of Oral Antibiotics on Health-Related Quality of Life after Mandibular Third Molar Surgery: An Observational Study. Niger. J. Clin. Pract. 2017, 20, 1189. [Google Scholar] [CrossRef]
- Sidana, S.; Mistry, Y.; Gandevivala, A.; Motwani, N. Evaluation of the Need for Antibiotic Prophylaxis During Routine Intra-Alveolar Dental Extractions in Healthy Patients: A Randomized Double-Blind Controlled Trial. J. Evid. Based Dent. Pract. 2017, 17, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Mariscal-Cazalla, M.d.M.; Manzano-Moreno, F.J.; García-Vázquez, M.; Vallecillo-Capilla, M.F.; Olmedo-Gaya, M.V. Do Perioperative Antibiotics Reduce Complications of Mandibular Third Molar Removal? A Double-Blind Randomized Controlled Clinical Trial. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 131, 286–294. [Google Scholar] [CrossRef]
- Cochrane Handbook for Systematic Reviews of Interventions|Cochrane Training. Available online: https://training.cochrane.org/handbook (accessed on 12 February 2022).
- Pantawane, M.V.; Chipper, R.T.; Robertson, W.B.; Khan, R.J.K.; Fick, D.P.; Dahotre, N.B. Evolution of Surface Morphology of Er:YAG Laser-Machined Human Bone. Lasers Med. Sci. 2019, 35, 1477–1485. [Google Scholar] [CrossRef] [PubMed]
- Leroy, R.; Bourgeois, J.; Verleye, L.; Declerck, D.; Depuydt, P.; Eloot, A.; Carvalho, J.C.; Teughels, W.; Cauwels, R.; Leprince, J.; et al. Guideline on the prudent prescription of antibiotics in the dental office. Available online: https://kce.fgov.be/en/guideline-on-the-prudent-prescription-of-antibiotics-in-the-dental-office (accessed on 12 February 2022).
- Bianco, A.; Cautela, V.; Napolitano, F.; Licata, F.; Pavia, M. Appropriateness of Antibiotic Prescription for Prophylactic Purposes among Italian Dental Practitioners: Results from a Cross-Sectional Study. Antibiotics 2021, 10, 547. [Google Scholar] [CrossRef]
- Wilson, W.; Taubert, K.A.; Gewitz, M.; Lockhart, P.B.; Baddour, L.M.; Levison, M.; Bolger, A.; Cabell, C.H.; Takahashi, M.; Baltimore, R.S.; et al. Prevention of Infective Endocarditis: Guidelines from the American Heart Association. JCDA 2008, 74, 449–453. [Google Scholar] [CrossRef]
- Sollecito, T.P.; Abt, E.; Lockhart, P.B.; Truelove, E.; Paumier, T.M.; Tracy, S.L.; Tampi, M.; Beltrán-Aguilar, E.D.; Frantsve-Hawley, J. The Use of Prophylactic Antibiotics Prior to Dental Procedures in Patients with Prosthetic Joints: Evidence-Based Clinical Practice Guideline for Dental Practitioners—A Report of the American Dental Association Council on Scientific Affairs. J. Am. Dent. Assoc. 2015, 146, 11–16.e8. [Google Scholar] [CrossRef]
- Abt, E.; Hellstein, J.W.; Lockhart, P.B.; Mariotti, A.J.; Sollecito, T.P.; Truelove, E.L.; Armstrong, S.; de Rossi, S.S.; Epstein, J.B.; Laudenbach, J.M.; et al. American Dental Association Guidance for Utilizing Appropriate Use Criteria in the Management of the Care of Patients with Orthopedic Implants Undergoing Dental Procedures. J. Am. Dent. Assoc. 2017, 148, 57–59. [Google Scholar] [CrossRef]
- Weiser, T.; Richter, E.; Hegewisch, A.; Muse, D.D.; Lange, R. Efficacy and Safety of a Fixed-Dose Combination of Ibuprofen and Caffeine in the Management of Moderate to Severe Dental Pain after Third Molar Extraction. Eur J. Pain 2018, 22, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Varvara, G.; Bernardi, S.; Cutilli, T.; Bianchi, S.; Sinjari, B.; Piattelli, M. Anti-Inflammatory Steroid Use in Impacted Third Molar Surgery: A Systematic Review. J. Biol. Regul. Homeost. Agents 2017, 31, 1095–1099. [Google Scholar] [PubMed]
- Balamurugan, R. Evaluation and Comparison of Anti-Inflammatory Properties of Ibuprofen Using Two Drug Delivery Systems after Third Molar Surgery: Using Chitosan Microspheres as a Carrier for Local Drug Delivery in to the Third Molar Socket and through the Oral Route. Br. J. Oral Maxillofac. Surg. 2021, 59, 191–196. [Google Scholar] [CrossRef]
- Ramires, G.A.D.; de Souza Santos, A.M.; Momesso, G.A.C.; Polo, T.O.B.; Silva, W.P.P.; Barbosa, S.; Bassi, A.P.F.; Faverani, L.P. Combination of Etodolac and Dexamethasone Improves Preemptive Analgesia in Third Molar Surgery: A Randomized Study. Clin. Oral Investig. 2021, 25, 2297–2305. [Google Scholar] [CrossRef]
- Payer, M.; Tan, W.C.; Han, J.; Ivanovski, S.; Mattheos, N.; Pjetursson, B.E.; Zhuang, L.; Fokas, G.; Wong, M.C.M.; Acham, S.; et al. The Effect of Systemic Antibiotics on Clinical and Patient-Reported Outcome Measures of Oral Implant Therapy with Simultaneous Guided Bone Regeneration. Clin. Oral Implant. Res. 2020, 31, 442–451. [Google Scholar] [CrossRef]
- Lockhart, P.B.; Brennan, M.T.; Thornhill, M.; Michalowicz, B.S.; Noll, J.; Bahrani-Mougeot, F.K.; Sasser, H.C. Poor Oral Hygiene as a Risk Factor for Infective Endocarditis–Related Bacteremia. J. Am. Dent. Assoc. 2009, 140, 1238. [Google Scholar] [CrossRef]
- Hasheminia, D.; Moaddabi, A.; Moradi, S.; Soltani, P.; Moannaei, M.; Issazadeh, M. The Efficacy of 1% Betadine Mouthwash on the Incidence of Dry Socket after Mandibular Third Molar Surgery. J. Clin. Exp. Dent. 2018, 10, e445. [Google Scholar] [CrossRef]
- Requena-Calla, S.; Funes-Rumiche, I. Effectiveness of Intra-Alveolar Chlorhexidine Gel in Reducing Dry Socket Following Surgical Extraction of Lower Third Molars. A Pilot Study. J. Clin. Exp. Dent. 2016, 8, e160. [Google Scholar] [CrossRef]
- Peterson, L. Principles of Management of Impacted Teeth. In Contemporary Oral and Maxillofacial Surgery; Peterson, L.J., Ellis, E., Hupp, J.R., Tucker, M.R., Eds.; Mosby: Maryland Heights, MO, USA, 1998. [Google Scholar]
- Renton, T.; Smeeton, Y.; McGurk, M. Factors Predictive of Difficulty of Mandibular Third Molar Surgery. Br. Dent. J. 2001, 190, 607–610. [Google Scholar] [CrossRef]
- Synan, W.; Stein, K. Management of Impacted Third Molars. Oral Maxillofac. Surg. Clin. N. Am. 2020, 32, 519–559. [Google Scholar] [CrossRef]
- Cervino, G.; Cicciù, M.; Biondi, A.; Bocchieri, S.; Herford, A.S.; Laino, L.; Fiorillo, L. Antibiotic Prophylaxis on Third Molar Extraction: Systematic Review of Recent Data. Antibiotics 2019, 8, 53. [Google Scholar] [CrossRef] [PubMed]
- Huttner, A.; Bielicki, J.; Clements, M.N.; Frimodt-Møller, N.; Muller, A.E.; Paccaud, J.P.; Mouton, J.W. Oral Amoxicillin and Amoxicillin–Clavulanic Acid: Properties, Indications and Usage. Clin. Microbiol. Infect. 2020, 26, 871–879. [Google Scholar] [CrossRef] [PubMed]
- Segura-Egea, J.J.; Gould, K.; Şen, B.H.; Jonasson, P.; Cotti, E.; Mazzoni, A.; Sunay, H.; Tjäderhane, L.; Dummer, P.M.H. European Society of Endodontology Position Statement: The Use of Antibiotics in Endodontics. Int. Endod. J. 2018, 51, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Martins, J.R.; Chagas, O.L.; Velasques, B.D.; Bobrowski, Â.N.; Correa, M.B.; Torriani, M.A. The Use of Antibiotics in Odontogenic Infections: What Is the Best Choice? A Systematic Review. J. Oral Maxillofac. Surg. 2017, 75, 2606.e1–2606.e11. [Google Scholar] [CrossRef]
- Ndukwe, K.C.; Braimah, R.O.; Owotade, J.F.; Aregbesola, S.B. Comparative Efficacy of Amoxicillin/Clavulanic Acid and Levofloxacin in the Reduction of Postsurgical Sequelae After Third Molar Surgery: A Randomized, Double-Blind, Clinical Trial in a Nigerian University Teaching Hospital. Niger. J. Surg. Off. Publ. Niger. Surg. Res. Soc. 2016, 22, 70. [Google Scholar] [CrossRef]
| Author | Year | Type of Study | Sample Size | Protocols | Results |
|---|---|---|---|---|---|
| López-Cedrún et al. [18] | 2011 | RCT | 123 | Preoperative amoxicillin (2 g AMX 2 h before surgery) vs. postoperative amoxicillin (15 tablets of amoxicillin 500 mg to be taken immediately after surgery 3 times daily for 5 days) vs. placebo (4 placebo tablets 2 h preoperatively and 15 tablets of placebo taken 3 times daily for 5 days) | Placebo group—5 socket infections and 1 suture dehiscence. No differences in side effects between the groups. |
| Siddiqi et al. [19] | 2011 | RCT | 89 | Group 1—placebo; Group 2—amoxicillin 1 g 1 h before surgery; Group 3—metronidazole 800 mg 1 h before surgery | There was no difference in surgical wound infection between groups. |
| Sisalli et al. [20] | 2012 | RCT | 107 | Amoxicillin clavulanate (875 mg + 125 mg per os three times a day for 5 days) vs. ceftazidime (1 g i.m., two times a day for 5 days) in postoperative period | In Group 1 (amoxicillin + clavulanic acid)—1 wound infection, 1 nausea, 1 headache, 1 diarrhea; In Group 2 (Ceftazidime)—1 heartburn |
| Duvall et al. [21] | 2013 | RCT | 30 | Chlorhexidine 0.12% rinse vs. amoxicillin (2 g) vs. placebo before the surgery | There were no differences between groups in bacteremia. |
| Bortoluzzi et al. [22] | 2013 | RCT | 50 | Group 1: 2 g of amoxicillin + 8 mg of dexamethasone; Group 2: 2 g of amoxicillin + 8 mg of placebo; Group 3: 8 mg of dexamethasone + 2 g of placebo and Group 4—placebo preoperative | 1—alveolar infection, 2 cases—alveolar osteitis. No differences were between postoperative complications. |
| Iglesias-Martin et al. [23] | 2014 | RCT | 546 | Amoxicillin (1 g) vs. amoxicillin and clavunate (875/125 mg) postoperative | No differences between two groups. Group 1—patients with gastrointestinal complications. |
| Milani et al. [24] | 2015 | RCT | 80 | Amoxicillin preoperative (1 group:1 h before surgery + 500 mg 8/8 h for 7 days; 2 group:1 h before surgery + 500 mg 8/8 h for 7 days) vs. placebo preoperative (1 h before surgery and 500 mg 8/8 h for 7 days) | There was no difference between groups. |
| Braimah et al. [25] | 2017 | RCT | 135 | Amoxicillin with clavulanic acid (1 group: 1 gram preoperatively and then 625 mg for 5 days; 2 group: 1 g preoperatively only) vs. levofloxacin (1 g preoperatively only) | Quality of life (QoL) was assessed between 3 groups of different protocols of antibiotic treatment. There were differences between 3 groups. |
| Sidana et al. [26] | 2017 | RCT | 400 | Group A: anti-inflammatory drugs in the postoperative period. Group B: Amoxicillin 500 mg orally thrice daily for three days + anti-inflammatory drugs in the postoperative period only. Group C: a single dose of Amoxicillin 500 mg one hour prior to the extraction procedure. Group D: mouthwash starting 15 min prior the procedure for a period of 7 days + anti-inflammatory drugs. | There was no difference between the groups to pain, swelling, or post extraction complications. |
| Mariscal-Cazalla et al. [27] | 2021 | RCT | 92 | Group 1—750 mg amoxicillin before and after the surgery; Group 2 after surgery; Group 3 placebo before and after surgery. | Pain and inflammation were higher in group 3 than in groups 1 and 2. |
| Study | The Randomization Process | Deviations from the Intended Interventions | Missing Outcome Data | Measurement of Outcome Data | Selection of the Reported Result |
|---|---|---|---|---|---|
| Sisalli et al., 2012 [20] | Some concerns | Some concerns | Low risk | Some concerns | Some concerns |
| Duvall et al., 2013 [21] | Low risk | Low risk | Low risk | Low risk | Low risk |
| Milani et al., 2015 [24] | Low risk | Low risk | Low risk | Low risk | Low risk |
| Braimah et al., 2017 [25] | Low risk | Low risk | Low risk | Low risk | Low risk |
| Iglesias-Martin et al., 2014 [23] | Some concerns | Some concerns | Low risk | Low risk | Low risk |
| López-Cedrún et al., 2011 [18] | Low risk | Low risk | Low risk | Low risk | Low risk |
| Siddiqi et al., 2011 [19] | Low risk | Low risk | Low risk | Low risk | Low risk |
| Sidana et al., 2017 [26] | Low risk | Low risk | Low risk | Low risk | Low risk |
| Bortoluzzi et al., 2013 [22] | Some concerns | Some concerns | Low risk | Low risk | Low risk |
| Mariscal-Cazalla et al., 2020 [27] | Low risk | Low risk | Low risk | Low risk | Low risk |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sologova, D.; Diachkova, E.; Gor, I.; Sologova, S.; Grigorevskikh, E.; Arazashvili, L.; Petruk, P.; Tarasenko, S. Antibiotics Efficiency in the Infection Complications Prevention after Third Molar Extraction: A Systematic Review. Dent. J. 2022, 10, 72. https://doi.org/10.3390/dj10040072
Sologova D, Diachkova E, Gor I, Sologova S, Grigorevskikh E, Arazashvili L, Petruk P, Tarasenko S. Antibiotics Efficiency in the Infection Complications Prevention after Third Molar Extraction: A Systematic Review. Dentistry Journal. 2022; 10(4):72. https://doi.org/10.3390/dj10040072
Chicago/Turabian StyleSologova, Diana, Ekaterina Diachkova, Ilana Gor, Susanna Sologova, Ekaterina Grigorevskikh, Liana Arazashvili, Pavel Petruk, and Svetlana Tarasenko. 2022. "Antibiotics Efficiency in the Infection Complications Prevention after Third Molar Extraction: A Systematic Review" Dentistry Journal 10, no. 4: 72. https://doi.org/10.3390/dj10040072
APA StyleSologova, D., Diachkova, E., Gor, I., Sologova, S., Grigorevskikh, E., Arazashvili, L., Petruk, P., & Tarasenko, S. (2022). Antibiotics Efficiency in the Infection Complications Prevention after Third Molar Extraction: A Systematic Review. Dentistry Journal, 10(4), 72. https://doi.org/10.3390/dj10040072








