A Novel Approach to Immediate Implants: The CastleWall Surgical Technique
Abstract
:1. Introduction
2. Materials and Methods
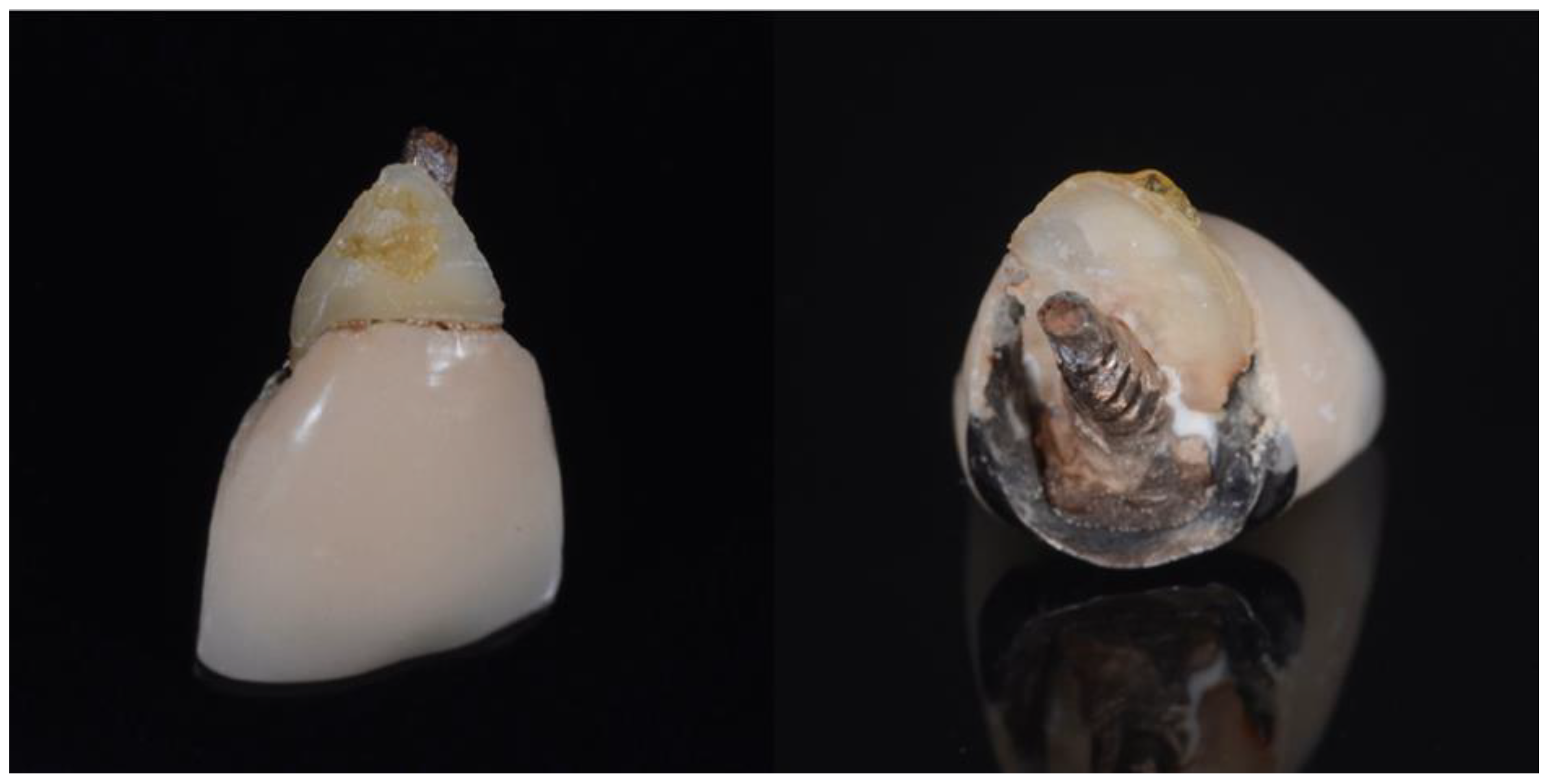
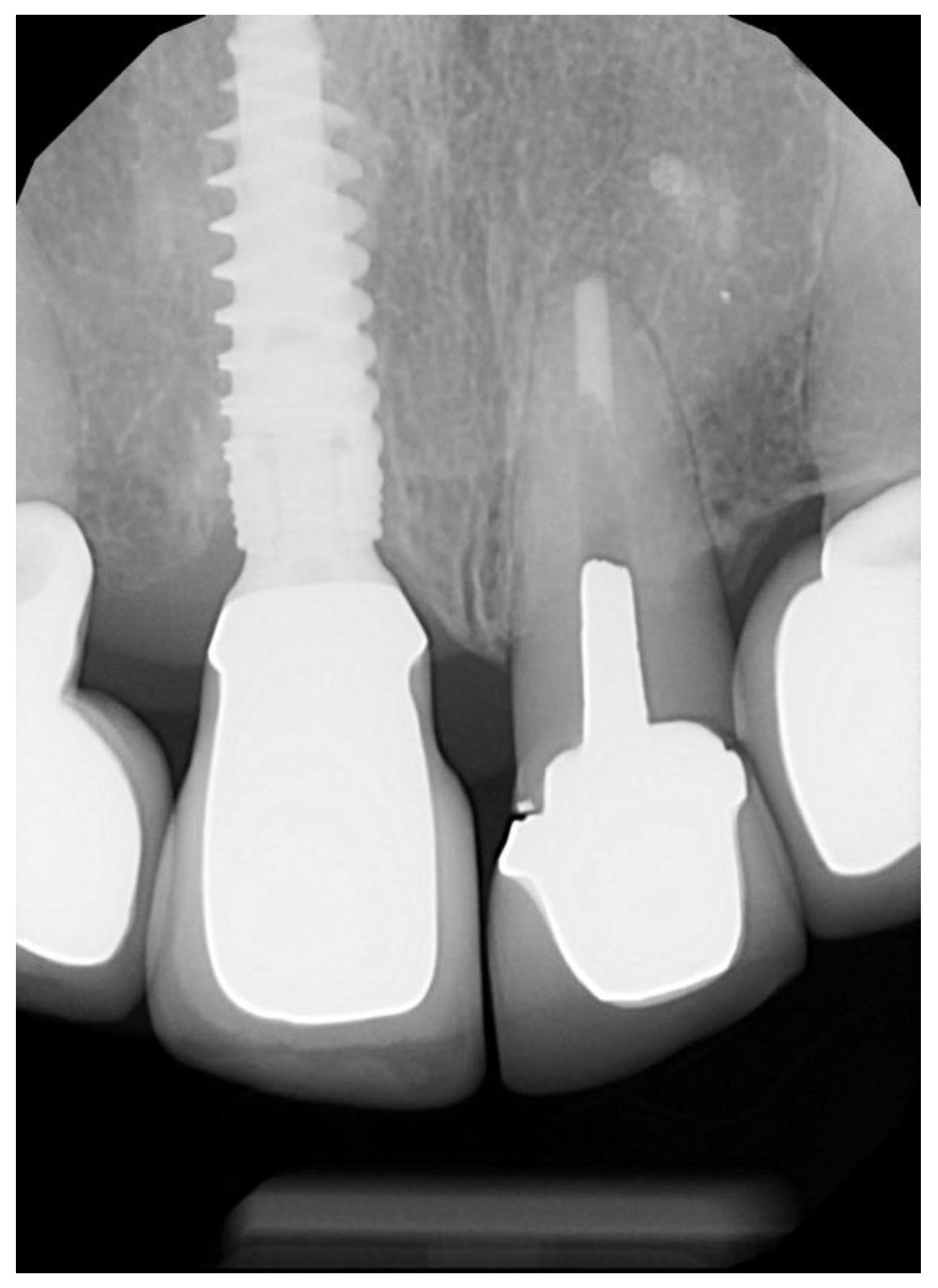
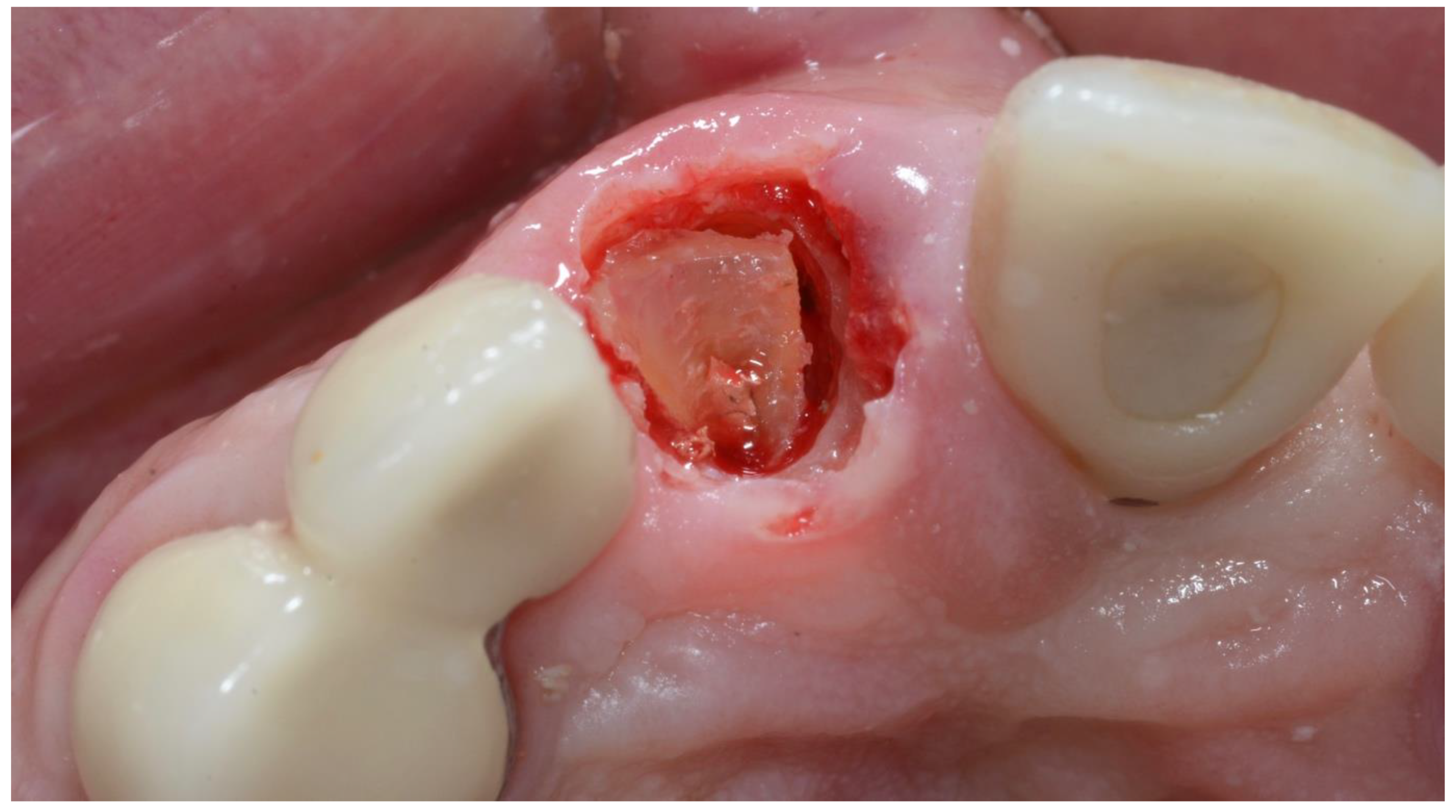
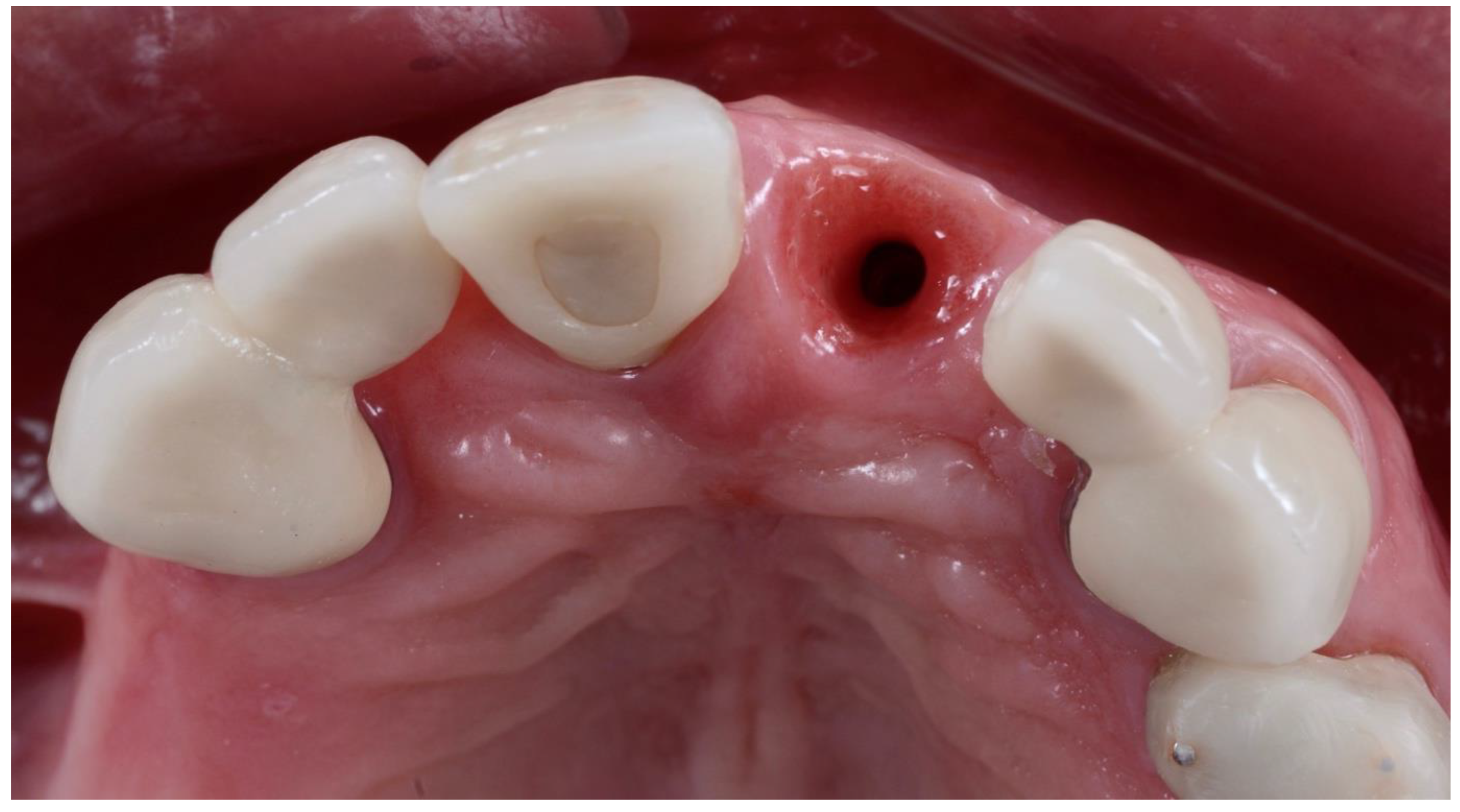
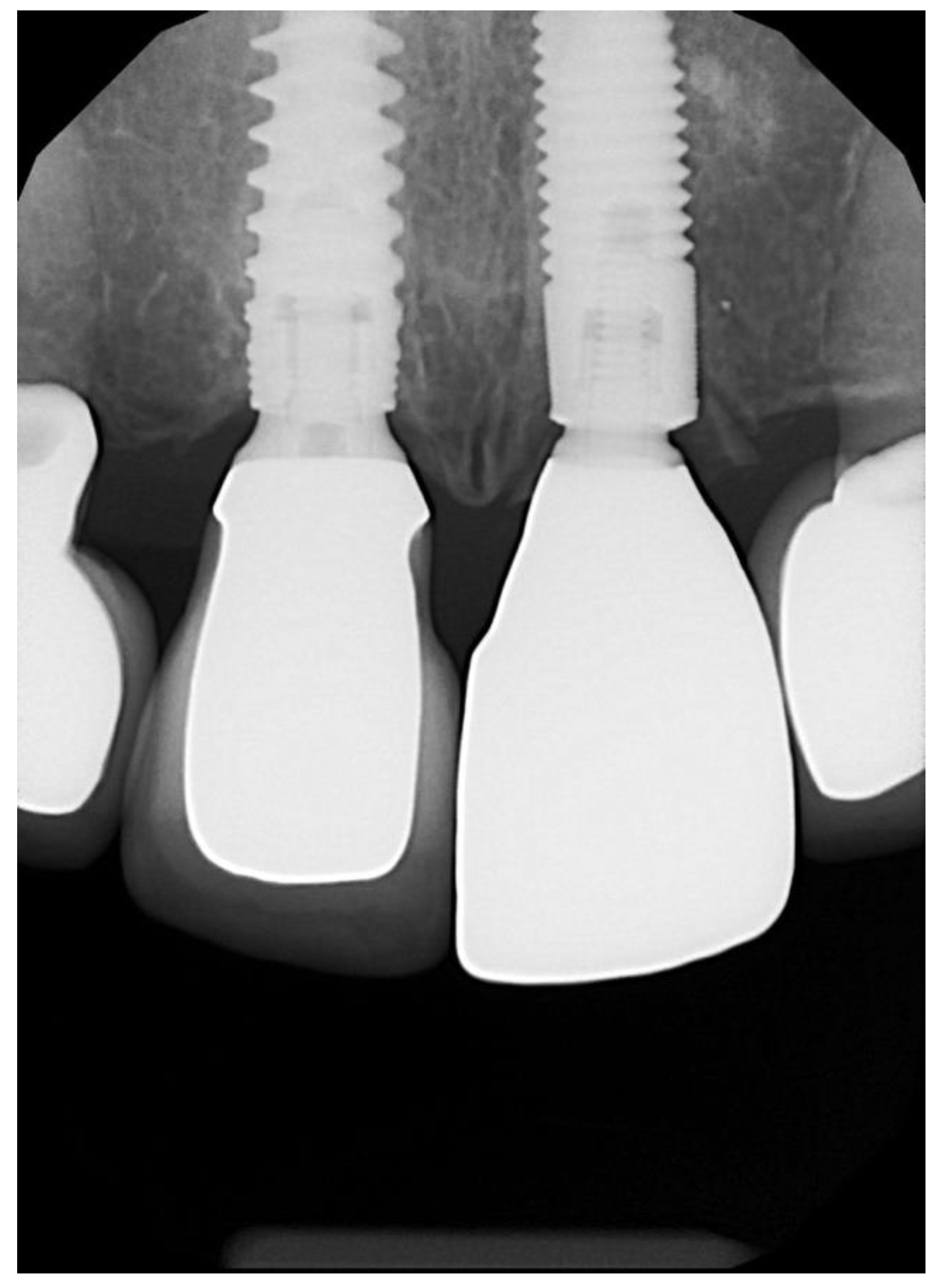
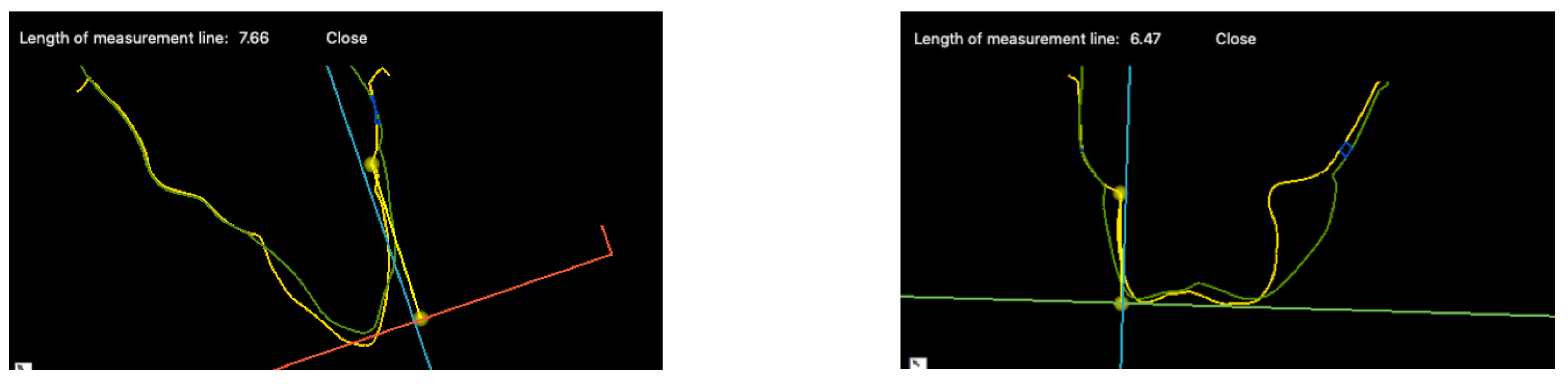
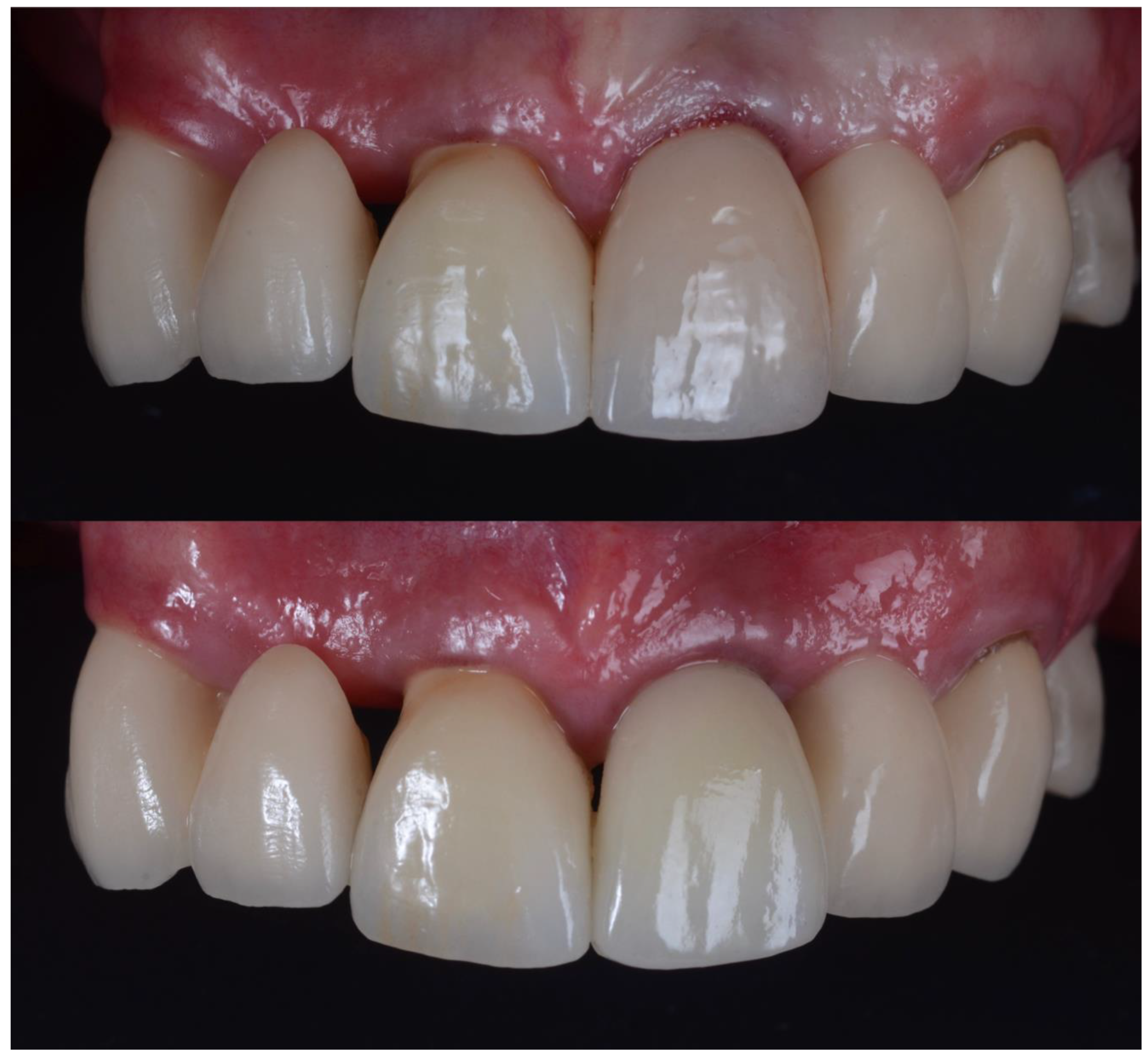
2.1. Surgical Technique
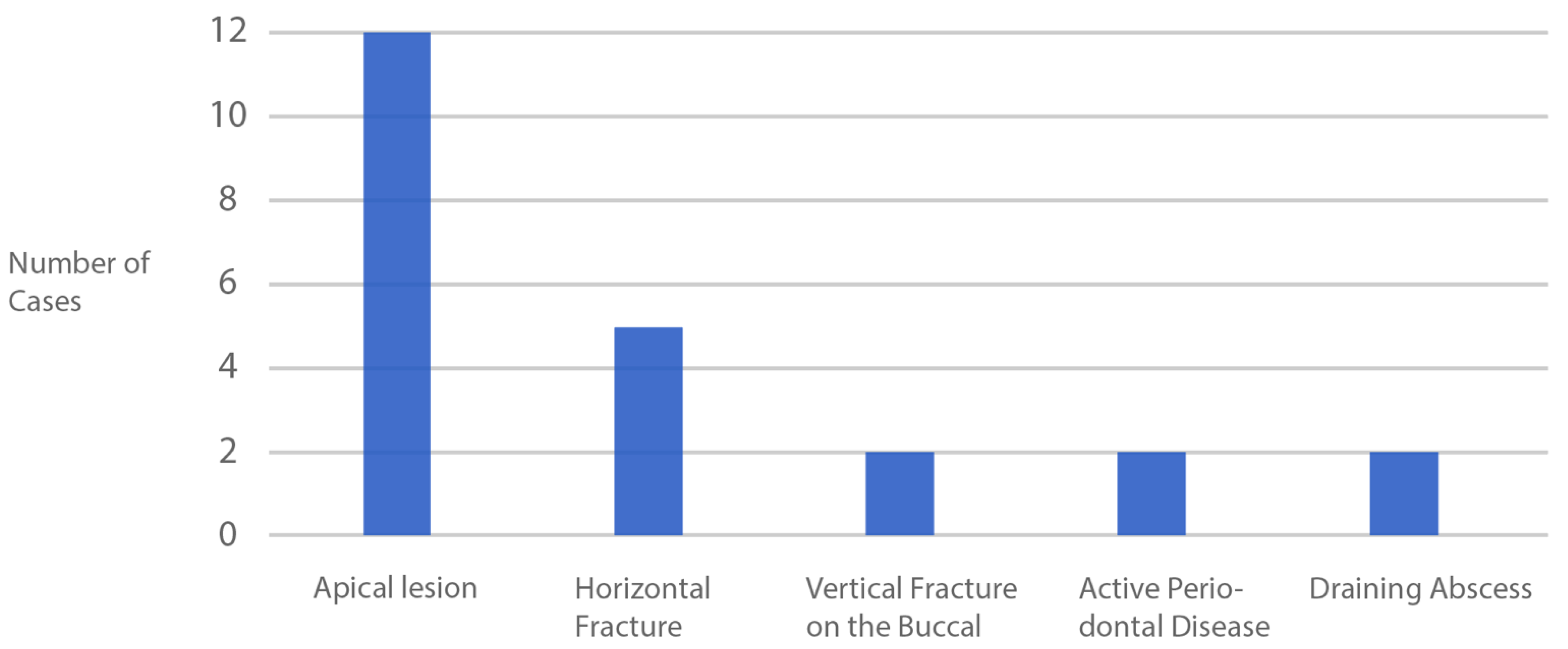
2.2. Complications
2.3. Data Accumulation
2.4. Statistical Analysis
3. Results
4. Discussion
| Technique | Author | Length of Study (Years) | Mesial Papillary Recession (mm) | Distal Papillary Recession (mm) | MD Buccal Recession | Mid-Buccal Recession (mm) | MD Buccal Bone Loss (mm) | |
|---|---|---|---|---|---|---|---|---|
| Socket-Shield | 360-degree socket shield | Cameron Castle 2022 | 2 | −0.26 ± 0.55 | −0.29 ± 0.52 | −0.30 ± 0.32 | −0.66 ± 0.64 | n.a. |
| Buccal socket shield | Bäumer et al., 2017 [5] | 5 | n.a. | n.a. | −0.37 ± 0.30 | −0.33 ± 0.23 | n.a. | |
| Traditional | No graft | Gavilán R 2017 [25] | 1 | −0.89 ± 0.41 | −0.84 ± 0.50 | −0.71 ± 0.35 | −1.10 ± 0.64 | n.a. |
| Bovine bone in gap | Gavilán R 2017 [25] | 1 | −0.95 ± 0.62 | −0.84 ± 0.46 | −0.79 ± 0.44 | −0.82 ± 0.53 | n.a. | |
| Bovine bone in gap | Van Nimwegen et al., 2018 [26] | 1 | n.a. | n.a. | −0.49 ± 0.54 | −0.48 ± 1.13 | −0.47 ± 0.55 | |
| Bovine in gap + CTG on buccal | Zuiderveld et al., 2020 [27] | 1 | n.a. | n.a. | −0.68 ± 0.59 | 0.20 ± 0.70 | −0.81 ± 0.66 | |
Future Studies
5. Conclusions
Funding
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Chappuis, V.; Araújo, M.; Buser, D. Clinical relevance of dimensional bone and soft tissue alterations post-extraction in esthetic sites. Periodontol. 2000 2017, 73, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics Restor. Dent. 2003, 23, 313–323. [Google Scholar]
- Staehler, P.; Abraha, S.; Bastos, J.; Zuhr, O.; Hürzeler, M. The socket-shield technique: A step-by-step protocol after 12 years of experience. Int. J. Esthet. Dent. 2020, 15, 288–305. [Google Scholar] [PubMed]
- Chen, S.; Buser, D. Esthetic outcomes following immediate and early implant placement in the anterior maxilla—A systematic review. Int. J. Oral Maxillofac Implant. 2014, 29, 186–215. [Google Scholar] [CrossRef] [Green Version]
- Bäumer, D.; Zuhr, O.; Rebele, S.; Hürzeler, M. Socket Shield Technique for immediate implant placement—Clinical, radiographic and volumetric data afer 5 years. Clin. Oral Impla. Res. 2017, 28, 1450–1458. [Google Scholar] [CrossRef]
- Esposito, M.; Maghaireh HGrusovin, M.G.; Ziounas, I.; Worthington, H.V. Soft tissue managment for dental implants:what are the most effective techniques? A Cochrane systematic reivew. Eur. J. Oral Implant. 2012, 5, 221–238. [Google Scholar]
- Lin, G.H.; Chan, H.L.; Wang, H.L. Effects of currently available surgical and restorative interventions on reducing midfacial mucosal recession of immediately placed single-tooth implants: A systematic review. J. Periodontol. 2014, 85, 92–102. [Google Scholar] [CrossRef]
- Hsu, Y.; Lin, G.; Wang, H. Effects of Platform-Switching on Peri-implant Soft and Hard Tissue Outcomes: A Systematic Review and Meta-analysis. Int. J. Oral Max. Implant. 2017, 32, 9–24. [Google Scholar] [CrossRef]
- Cosyn, J.; De Rouck, T. Aesthetic outcome of single-tooth implant restorations following early implant placement and guided bone regeneration: Crown and soft tissue dimensions compared with contralateral teeth. Clin. Oral Imp. Res. 2009, 20, 1063–1069. [Google Scholar] [CrossRef]
- Cosyn, J.; De Bruyn, H.; Cleymaet, R. Soft Tissue Preservation and Pink Aesthetics around Single Immediate Implant Restorations: A 1-Year Prospective Study. Clin. Implant. Dent. Relat. Res. 2013, 15, 847–857. [Google Scholar] [CrossRef]
- Jung, R.; Philipp, A.; Annen, B.; Signorelli, L.; Thoma, D.; Hammerle, C.; Attin, T.; Schmidlin, P. Radiographic evaluation of different techniques for ridge preservation after tooth extraction: A randomized controlled clinical trial. J. Clin. Periodontol. 2012, 40, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Hürzeler, M.B.; Zuhr, O.; Schupbach, P.; Rebele, S.F.; Emannouilidis, N.; Fickl, S. The socket-shield technique: A proof-of-principle report. J. Clin. Periodontol. 2010, 37, 855–862. [Google Scholar] [CrossRef]
- Kan, J.; Rungcharassaeng, K. Proximal Socket Shield for Interimplant Papilla Preservation in the Esthetic Zone. Int. J. Perio. Res. Dent. 2013, 33, e24–e31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cherel, F.; Etienne, D. Papilla preservation between two implants: A modified socket-shield technique to maintain the scalloped anatomy? A case report. Quintessence Int. 2014, 45, 23–30. [Google Scholar] [PubMed]
- Aslan, S. Improved volume and contour stability with thin socket-shield preparation in immediate implant placement and provisionalizatin in the esthetic zone. Int. J. Esth. Dent. 2018, 13, 172–183. [Google Scholar]
- Troiano, M.; Benincasa, M.; Sanchez, P.; Calvo-Guirado, J.L. Bundle bone preservatin with Root-T-Belt: Case Study. Ann. Oral. Max. Surg. 2014, 2, 7. [Google Scholar]
- Calvo-Guirado, J.L. Different configuration of socket-shield technique in perimplant bone preservation: An experimental study in dog mandible. Ann. Anat. -Anat. Anz. 2016, 208, 109–115. [Google Scholar] [CrossRef]
- Braut, V.; Bornstein, M.M.; Belser, U.; Buser, D. Thickness of the anterior maxillary facial bone wall-a retrospective radiographic study using cone beam computed tomography. Int. J. Periodontics Restor. Dent. 2011, 31, 125–131. [Google Scholar]
- Januário, A.L.; Duarte, W.R.; Barriviera, M. Dimension of the facial bone wall in the anterior maxilla: A cone-beam computed tomography study. Clin. Oral Implant. Res. 2011, 22, 1168–1171. [Google Scholar] [CrossRef]
- Gluckman, H.; Salama, M.; Du Toit, J. A retrospective evaluation of 128 socket-shield cases in the esthetic zone and posterior sites: Partial extraction therapy with up to 4 years follow-up. Clin. Implant. Dent. Relat. Res. 2017, 20, 122–129. [Google Scholar] [CrossRef]
- Zuhr, O.; Staehler, P.; Hüerzeler, M. Complication Management of a Socket Shield Case After 6 Years of Function. Int. J. Perio. Rest. Dent. 2020, 40, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Hinze, M.; Janousch, R.; Goldhahn, S.; Schlee, M. Volumetric alterations around single-tooth implants using the socket-shield technique: Preliminary results of a prospective case series. Int. J. Esth. Dent. 2018, 13, 146–170. [Google Scholar]
- Schneider, D.; Grunder, U.; Ender, A.; Hammerle, C.H.; Jung, R.E. Volume gain and stability of per-implant tissue following bone and soft tissue agumentation: 1-ear results from a prospective cohort study. Clin. Oral Imp. Res. 2011, 22, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Carnevale, G.; Sterrantino, S.; Di Febo, G. Soft and hard tissue wound healing following tooth preparation to the alveolar crest. Int. J. Periodontics Restor. Dent. 1983, 3, 36–53. [Google Scholar]
- Gavilán, R.C. 3D Volumetric Changes of Tissue Contour After Immediate Implant Placement with and without Xenograft in the Horizontal Gap: A Randomized Controlled Clinical Trial. Ph.D. Thesis, University of Southern California ProQuest Dissertations Publishing, Los Angeles, CA, USA, 2017. [Google Scholar]
- van Nimwegen, W.G.; Raghoebar, G.M.; Zuiderveld, E.G.; Jung, R.E.; Meijer, H.J.A.; Mühlemann, S. Immediate placement and provisionalization of implants in the aesthetic zone with or without a connective tissue graft: A 1-year randomized controlled trial and volumetric study. Clin. Oral Implant. 2018, 29, 671–678. [Google Scholar] [CrossRef]
- Zuiderveld, E.G.; van Nimwegen, W.G.; Meijer, H.J.A.; Jung, R.E.; Muehlemann, S.; Vissink, A.; Raghoebar, G.M. Effect of connective tissue grafting on buccal bone changes based on cone beam computed tomography scans in the aesthetic zone of single immediate implants: A 1-year randomized controlled trial. J. Perio. 2020, 92, 553–561. [Google Scholar] [CrossRef]
- Siormpas, K.; Miltiadis, M.; Kontsiotou-Siormpa, E.; Garber, D.; Kotsakis, G. Immediate Implant Placement in the Esthetic Zone Utilizing the "Root-Membrane" Technique: Clinical Results up to 5 Years Postloading. Int. J. Oral Maxillofac. Implant. 2014, 29, 1397–1405. [Google Scholar] [CrossRef] [Green Version]
- Wolff, L.; Dahlen, G.; Aeppli, D. Bacteria as Risk Marker for Periodontitis. J. Periodontol. 1994, 64, 498–510. [Google Scholar] [CrossRef]
- Björk, A. Facial growth in man, studied with the aid of metallic implants. Acta. Odontol. Scand. 1955, 13, 9–34. [Google Scholar] [CrossRef]
- Gluckman, H.; Du Toit, J.; Salama, M.; Nagy, K.; Dard, M. A decade of the socet-shield technique: A step-by-step partial extraction therapy protocol. Int. J. Esth. Dent. 2020, 15, 212–225. [Google Scholar]










| Inclusion Criteria |
|---|
| Medically healthy adult |
| Vertical fracture including on the buccal aspect |
| Horizontal fractures at or below bone level |
| Acute and chronic apical infection |
| Acute periodontal disease |
| Informed consent |
| Immediate implant using CastleWall Surgical Technique |
| Exclusion Criteria |
| Primary stability <25 Ncm |
| Patient not available for final review |
| Models not taken prior to treatment |
| Models not clear or incomplete around treatment site |
| Case No | Site (FDI) | MD Buccal (mm) | MD Lingual (mm) | Mid-Buccal Recession (mm) | Mid-Lingual Recession (mm) |
|---|---|---|---|---|---|
| 1 | 17 | −0.77 | −0.69 | −1.40 | −1.00 |
| 2 | 22 | 0 | n.a | −0.76 | n.a. |
| 3 | 24 | −0.22 | 0.21 | 0.32 | −0.34 |
| 4 | 22 | −0.43 | 0.02 | −1.27 | −0.89 |
| 5 | 24 | −0.29 | −0.37 | −0.36 | −0.48 |
| 6 | 16 | 0.08 | n.a. | −0.28 | n.a. |
| 7 | 14 | −0.10 | 0.03 | −1.61 | −0.25 |
| 8 | 35 | 0.18 | −0.26 | −0.51 | −0.52 |
| 9 | 11 | −0.24 | 0.02 | 0.31 | 0.57 |
| 10 | 33 | −0.18 | n.a. | −0.92 | −0.02 |
| 11 | 26 | n.a. | n.a. | n.a. | n.a. |
| 12 | 44 | −0.15 | 0.04 | −0.87 | −0.70 |
| 13 | 26 | −0.78 | n.a. | −0.94 | −1.22 |
| 14 | 25 | 0.10 | −0.21 | −1.71 | −1.48 |
| 15 | 24 | 0.20 | −0.03 | −1.48 | −0.66 |
| 16 | 26 | −0.98 | n.a. | −0.93 | −2.99 |
| 17 | 26 | −0.20 | −0.68 | 0.58 | −1.75 |
| 18 | 23 | −0.09 | −0.18 | −0.77 | −0.48 |
| 19 | 26 | −0.62 | n.a. | −1.57 | −2.02 |
| 20 | 24 | −0.32 | −0.07 | 0.24 | −0.85 |
| 21 | 21 | −0.87 | −0.30 | −1.13 | −2.43 |
| 22 | 25 | −0.44 | 0.01 | −1.29 | −0.54 |
| 23 | 35 | −0.28 | n.a. | −0.51 | −0.74 |
| 24 | 16 | −0.32 | 0.04 | −0.35 | −0.02 |
| 25 | 36 | −0.12 | −0.56 | 0.26 | −0.93 |
| 26 | 44 | −0.51 | n.a. | −0.18 | n.a. |
| 27 | 35 | −0.61 | −0.64 | −0.90 | −1.69 |
| 28 | 14 | −0.87 | 0.07 | −1.01 | −1.72 |
| 29 | 14 | −0.13 | 0.06 | −0.80 | 0.39 |
| 30 | 45 | 0.02 | −0.06 | 0.07 | 0 |
| 31 | 25 | −0.15 | n.a. | −0.14 | −0.66 |
| Case No | Site (FDI) | Pre-op Mesial (mm) | Post-op Mesial (mm) | Mesial Recession (mm) | Pre-op Distal (mm) | Post-op Distal (mm) | Distal Recession (mm) |
|---|---|---|---|---|---|---|---|
| 1 | 17 | n.a. | n.a. | n.a. | n.a. | ||
| 2 | 22 | 4.25 | 4.22 | −0.03 | 2.99 | 2.92 | −0.24 |
| 3 | 24 | 3.92 | 3.91 | −0.01 | 3.43 | 2.92 | −0.51 |
| 4 | 22 | 5.85 | 4.50 | −1.35 | 4.34 | 3.15 | −1.19 |
| 5 | 24 | 4.92 | 5.03 | 0.11 | 3.41 | 3.31 | −0.10 |
| 6 | 16 | 2.60 | 2.22 | −0.38 | 3.17 | 2.46 | −0.71 |
| 7 | 14 | 3.13 | 3.42 | 0.29 | 1.35 | 1.91 | 0.56 |
| 8 | 35 | 2.94 | 2.93 | −0.01 | 2.84 | 2.97 | 0.13 |
| 9 | 11 | 4.27 | 3.74 | −0.53 | 3.46 | 2.38 | −1.08 |
| 10 | 33 | 2.81 | 2.52 | −0.29 | 1.29 | 1.64 | 0.35 |
| 11 | 26 | n.a. | n.a. | n.a. | n.a. | ||
| 12 | 44 | n.a. | n.a. | n.a. | n.a. | ||
| 13 | 26 | n.a. | n.a. | n.a. | n.a. | ||
| 14 | 25 | n.a. | n.a. | n.a. | n.a. | ||
| 15 | 24 | n.a. | n.a. | n.a. | n.a. | ||
| 16 | 26 | 3.00 | 2.80 | −0.20 | 2.09 | 2.43 | 0.34 |
| 17 | 26 | n.a. | n.a. | n.a. | n.a. | ||
| 18 | 23 | 3.26 | 2.97 | −0.29 | 2.36 | 2.29 | −0.07 |
| 19 | 26 | n.a. | n.a. | n.a. | n.a. | ||
| 20 | 24 | 4.87 | 4.07 | −0.80 | 2.62 | 2.65 | 0.03 |
| 21 | 21 | 5.96 | 6.56 | 0.60 | 5.48 | 5.29 | −0.19 |
| 22 | 25 | n.a. | n.a. | n.a. | n.a. | ||
| 23 | 35 | n.a. | n.a. | n.a. | n.a. | ||
| 24 | 16 | n.a. | n.a. | n.a. | n.a. | ||
| 25 | 36 | n.a. | n.a. | n.a. | n.a. | ||
| 26 | 44 | n.a. | n.a. | n.a. | n.a. | ||
| 27 | 35 | n.a. | n.a. | n.a. | n.a. | ||
| 28 | 14 | 5.53 | 4.01 | −1.52 | 4.09 | 3.04 | −1.05 |
| 29 | 14 | 4.73 | 4.88 | 0.15 | 3.09 | 2.80 | −0.29 |
| 30 | 45 | 4.22 | 3.98 | −0.24 | 3.64 | 3.35 | −0.29 |
| 31 | 25 | 0.99 | 1.03 | 0.04 | 1.86 | 1.22 | −0.64 |
| Variable | n | Mean ± SD | Median (IQR) | p-Value * |
|---|---|---|---|---|
| MD Buccal | 30 | −0.30 ± 0.32 | −0.23 (0.41) | <0.001 |
| Molar | 8 | −0.46 ± 0.38 | −0.47 (0.62) | |
| Premolar | 16 | −0.22 ± 0.29 | −0.19 (0.34) | |
| Incisor | 6 | −0.30 ± 0.31 | −0.21 (0.34) | |
| MD Lingual | 21 | −0.17 ± 0.27 | −0.06 (0.33) | 0.664 |
| Molar | 4 | −0.47 ± 0.35 | −0.62 (0.43) | |
| Premolar | 13 | −0.09 ± 0.23 | −0.03 (0.25) | |
| Incisor | 4 | −0.11 ± 0.16 | −0.80 (0.26) | |
| Mid-buccal Recession | 30 | −0.66 ± 0.64 | −0.79 (0.95) | 0.001 |
| Molar | 8 | −0.58 ± 0.77 | −0.64 (1.16) | |
| Premolar | 16 | −0.67 ± 0.65 | −0.66 (0.99) | |
| Incisor | 6 | −0.76 ± 0.56 | −0.85 (0.37) | |
| Mid-lingual Recession | 27 | −0.87 ± 0.84 | −0.70 (1.14) | <0.001 |
| Molar | 7 | −1.42 ± 0.94 | −1.22 (1.09) | |
| Premolar | 15 | −0.68 ± 0.58 | −0.66 (0.51) | |
| Incisor | 5 | −0.65 ± 1.13 | −0.48 (0.87) | |
| Mesial Papillary Recession | 17 | −0.26 ± 0.55 | −0.20 (0.42) | 0.144 |
| Molar | 2 | −0.29 ± 0.13 | −0.29 (0.18) | |
| Premolar | 9 | −0.22 ± 0.58 | −0.01 (0.35) | |
| Incisor | 6 | −0.32 ± 0.64 | −0.30 (0.31) | |
| Distal Papillary Recession | 17 | −0.29 ± 0.52 | −0.24 (0.67) | 0.144 |
| Molar | 2 | −0.19 ± 0.74 | −0.19 (1.05) | |
| Premolar | 9 | −0.24 ± 0.47 | −0.29 (0.54) | |
| Incisor | 6 | −0.40 ± 0.60 | −0.22 (1.01) |
| Case No. | Tooth No | Bleeding * (%) | Swelling * (%) | Pain * (%) | Satisfaction (%) | Swelling (Days) | Pain (Days) | Analgesics (Days) |
|---|---|---|---|---|---|---|---|---|
| 1 | 17 | 100 | 100 | 90 | 100 | 0 | 1 | 0 |
| 2 | 22 | 100 | 100 | 100 | 100 | 0 | 0 | 0 |
| 3 | 24 | 100 | 80 | 90 | 100 | 2 | 1 | 1 |
| 4 | 22 | 100 | 100 | 80 | 100 | 0 | 2 | 1 |
| 5 | 24 | 100 | 100 | 80 | 100 | 0 | 2 | 1 |
| 6 | 16 | 100 | 100 | 90 | 100 | 0 | 1 | 1 |
| 7 | 14 | 100 | 100 | 100 | 100 | 0 | 0 | 0 |
| 8 | 35 | 100 | 100 | 90 | 100 | 0 | 2 | 0 |
| 9 | 11 | 100 | 100 | 100 | 100 | 0 | 0 | 2 |
| 10 | 33 | 100 | 100 | 80 | 90 | 0 | 2 | 0 |
| 11 | 26 | 100 | 100 | 80 | 90 | 0 | 2 | 0 |
| 12 | 44 | 100 | 100 | 90 | 90 | 0 | 1 | 1 |
| 13 | 26 | 100 | 100 | 90 | 100 | 0 | 0 | 0 |
| 14 | 25 | 100 | 100 | 80 | 80 | 0 | 2 | 1 |
| 15 | 24 | 100 | 100 | 80 | 80 | 0 | 2 | 1 |
| 16 | 26 | 100 | 100 | 100 | 100 | 0 | 0 | 0 |
| 17 | 26 | 100 | 100 | 90 | 100 | 0 | 1 | 1 |
| 18 | 23 | 100 | 100 | 100 | 100 | 0 | 0 | 0 |
| 19 | 26 | 100 | 100 | 100 | 100 | 0 | 0 | 0 |
| 20 | 24 | 100 | 80 | 90 | 100 | 2 | 1 | 2 |
| 21 | 21 | 100 | 100 | 90 | 100 | 0 | 0.5 | 0 |
| 22 | 25 | 100 | 100 | 80 | 100 | 0 | 1 | 1 |
| 23 | 35 | 100 | 100 | 100 | 100 | 0 | 0 | 0 |
| 24 | 16 | 100 | 100 | 90 | 100 | 0 | 2 | 2 |
| 25 | 36 | 100 | 100 | 100 | 100 | 0 | 0 | 0 |
| 26 | 44 | 100 | 100 | 100 | 100 | 0 | 0 | 0 |
| 27 | 25 | 100 | 100 | 80 | 100 | 0 | 1 | 1 |
| 28 | 14 | 100 | 100 | 100 | 100 | 0 | 0 | 0 |
| 29 | 14 | 100 | 100 | 100 | 100 | 0 | 0 | 0 |
| 30 | 45 | 100 | 100 | 85 | 100 | 0 | 1 | 1 |
| 31 | 25 | 100 | 100 | 100 | 100 | 0 | 0 | 0 |
| Mean | 100 | 98.71 | 91.13 | 97.74 | 0.13 | 0.82 | 0.55 | |
| Median | 100 | 100 | 90 | 100 | 0 | 1 | 0 | |
| SD | 0 | 4.99 | 8.14 | 5.60 | 0.50 | 0.82 | 0.68 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castle, C. A Novel Approach to Immediate Implants: The CastleWall Surgical Technique. Dent. J. 2022, 10, 62. https://doi.org/10.3390/dj10040062
Castle C. A Novel Approach to Immediate Implants: The CastleWall Surgical Technique. Dentistry Journal. 2022; 10(4):62. https://doi.org/10.3390/dj10040062
Chicago/Turabian StyleCastle, Cameron. 2022. "A Novel Approach to Immediate Implants: The CastleWall Surgical Technique" Dentistry Journal 10, no. 4: 62. https://doi.org/10.3390/dj10040062
APA StyleCastle, C. (2022). A Novel Approach to Immediate Implants: The CastleWall Surgical Technique. Dentistry Journal, 10(4), 62. https://doi.org/10.3390/dj10040062





