The 1064-nm Nd:YAG Photobiomodulation vs. 20% Benzocaine Topical Gel in Inducing Mucosal Anesthetic Effect: A Double-Blind Randomized Clinical Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Randomisation and Masking
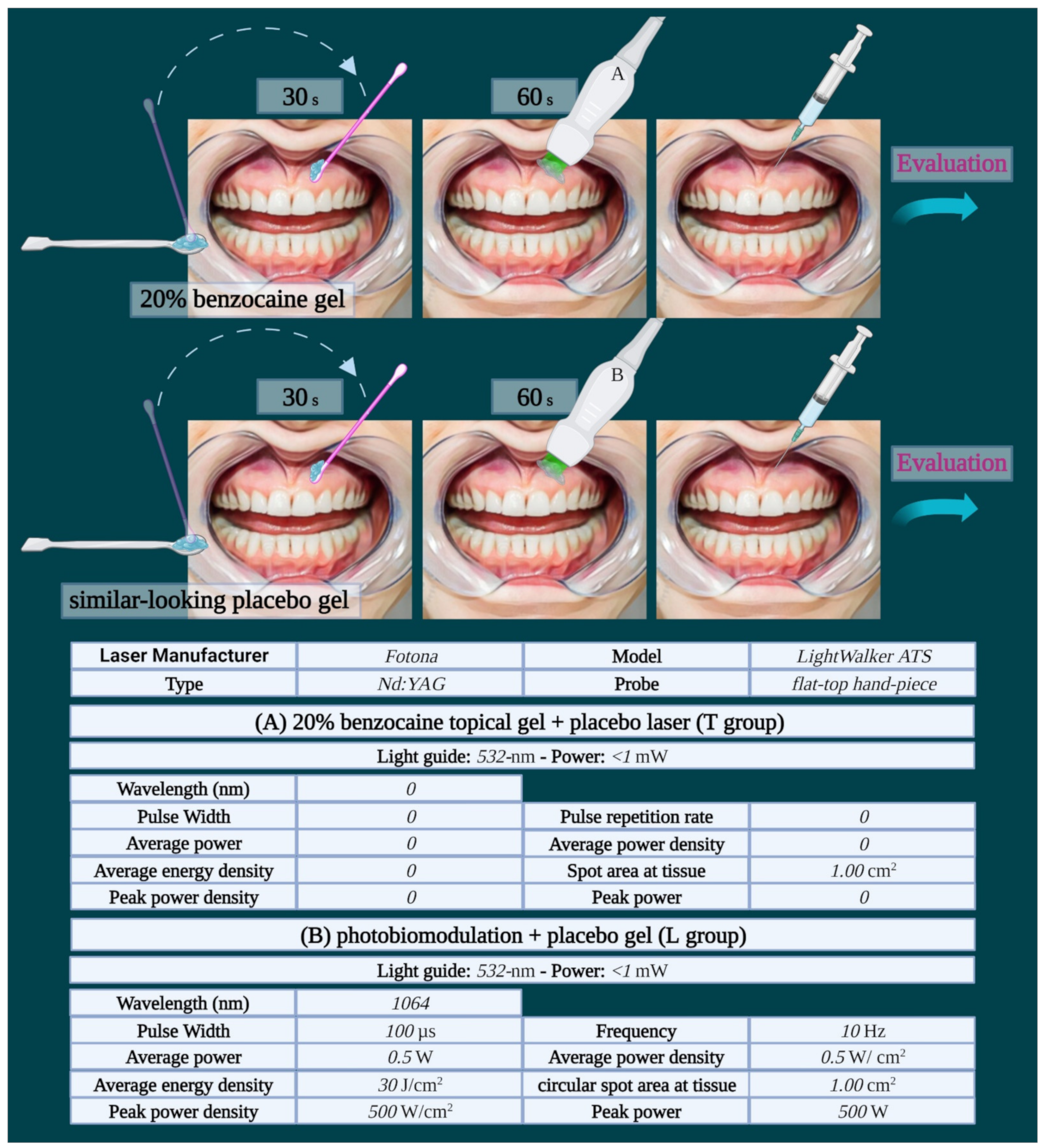
2.3. Procedure
2.3.1. 20% Benzocaine Topical Gel + Placebo Laser (T Group)
2.3.2. Photobiomodulation + Placebo Gel (L Group)
2.3.3. Local Anesthetic Injection Protocol
2.4. Evaluation
2.4.1. Visual Analog Scale (VAS)
2.4.2. Verbal Rating Scale (VRS)
2.5. Outcomes
2.6. Data Analysis
3. Results
3.1. Participants and Randomization
3.2. Primary Variable
Pain Intensity Evaluation
3.3. Secondary Variable
3.3.1. Taste Evaluation
3.3.2. Evaluation of Undesirable Numbness of the Mouth
3.3.3. Patients’ Overall Satisfaction
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bahl, R. Local anesthesia in dentistry. Anesth. Prog. 2004, 51, 138–142. [Google Scholar] [PubMed]
- Ogle, O.E.; Mahjoubi, G. Local anesthesia: Agents, techniques, and complications. Dent. Clin. N. Am. 2012, 56, 133–148. [Google Scholar] [CrossRef] [PubMed]
- Grotticelli, J. Side effects of local anesthetics. In Side Effects of Drugs Annual; Elsevier: Amsterdam, Netherlands, 2021; Volume 43, pp. 169–177. [Google Scholar] [CrossRef]
- Lee, H.-S. Recent advances in topical anesthesia. J. Dent. Anesth. Pain Med. 2016, 16, 237–244. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kravitz, N.D. The use of compound topical anesthetics: A review. J. Am. Dent. Assoc. 2007, 138, 1333–1339. [Google Scholar] [CrossRef] [Green Version]
- Bizzio, R.; Cianelli, R.; Villegas, N.; Hooshmand, M.; Robinson, M.; Hires, K.A.; Stathas, A. Exploring non-pharmacological management among anesthesia providers to reduce preoperative distress in children. J. Pediatr. Nurs. 2019, 50, 105–112. [Google Scholar] [CrossRef] [Green Version]
- FDA’s Communication to the Public. Available online: https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/safety-information-benzocaine-containing-products (accessed on 25 June 2018).
- Song, M.A.; Young-Ju, H.; Hyung-Sik, S. Literature review on the current status of herbal medicine use as topical anesthetics. J. Korean Med. Ophthalmol. Otolaryngol. Dermatol. 2020, 33, 114–125. [Google Scholar]
- Sivinagini, Y.; Ashish, R.J. Role of acupuncture and acupressure in preventing gag reflex. Drug Invent. Today 2018, 10, 116. [Google Scholar]
- Siddiqui, A.; Patel, H.J.; Bhutia, E.T.; Kade, K.; Chincholi, R.; Patil, A. Comparative evaluation of transcutaneous electronic nerve stimulation and topical anesthesia in reduction of pain perception during administration of local anesthesia in pediatric dental patients. Ann. Rom. Soc. Cell Biol. 2021, 25, 1793–1798. [Google Scholar]
- Salma, R.G.; Alsayeh, A.; Maneea, A.; Alrassan, F.; Almarshad, A. The effectiveness of electronic pulsed soft tissue vibration compared with topical anaesthesia in reducing the pain of injection of local anaesthetics in adults: A randomized controlled split-mouth clinical trial. Int. J. Oral Maxillofac. Surg. 2021, 50, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.; Gugnani, N.; Lathwal, G.; Pandit, I.K. Efficacy of different precooling agents and topical anesthetics on the pain perception durin. Int. J. Clin. Pediatric Dent. 2015, 8, 119. [Google Scholar]
- Ramírez-Carrasco, A.; Butrón-Téllez Girón, C.; Sanchez-Armass, O.; Pierdant-Pérez, M. Effectiveness of hypnosis in combination with conventional techniques of behavior management in anxiety/pain reduction during dental anesthetic infiltration. Pain Res. Manag. 2017, 2017, 1434015. [Google Scholar] [CrossRef] [PubMed]
- Ravera, S.; Colombo, E.; Pasquale, C.; Benedicenti, S.; Solimei, L.; Signore, A.; Amaroli, A. Mitochondrial bioenergetic, photobiomodulation and trigeminal branches nerve damage, what′s the connection? A review. Int. J. Mol. Sci. 2021, 22, 4347. [Google Scholar] [CrossRef] [PubMed]
- Pasquale, C.; Utyuzh, A.; Mikhailova, M.V.; Colombo, E.; Amaroli, A. Recovery from idiopathic facial paralysis (bell’s palsy) using photobiomodulation in patients non-responsive to standard treatment: A case series study. Photonics 2021, 8, 341. [Google Scholar] [CrossRef]
- Munguia, F.M.; Jang, J.; Salem, M.; Clark, G.T.; Enciso, R. Efficacy of low-level laser therapy in the treatment of temporomandibular myofascial pain: A systematic review and meta-analysis. J. Oral Facial Pain Headache 2018, 32, 287–297. [Google Scholar] [CrossRef] [PubMed]
- Doshi, S.; Jain, S.; Hegde, R. Effect of low-level laser therapy in reducing dentinal hypersensitivity and pain following periodontal flap surgery. Photomed. Laser Surg. 2014, 32, 700–706. [Google Scholar] [CrossRef] [PubMed]
- Eshghpour, M.; Shaban, B.; Ahrari, F.; Erfanian, M.; Shadkam, E. Is low level laser therapy effective for treatment of neurosensory deficits arising from sagittal split ramus osteotomy? J. Oral. Maxillofac. Surg. 2017, 75, 2085–2090. [Google Scholar] [CrossRef]
- Ghaderi, F.; Ghaderi, R.; Davarmanesh, M.; Bayani, M.; Moghadam, S.A. Pain management during needle insertion with low level laser. Eur. J. Paediatr. Dent. 2016, 17, 151–154. [Google Scholar] [PubMed]
- Jagtap, B.; Bhate, K.; Magoo, S.; Santhoshkumar, S.N.; Gajendragadkar, K.S.; Joshi, S. Painless injections–a possibility with low level laser therapy. J. Dent. Anesth. Pain Med. 2019, 19, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Hamblin, M.R.; Demidova, T.N. Mechanisms of low level light therapy. Proc. SPIE 2006, 6140, 612001. [Google Scholar]
- Amaroli, A.; Ravera, S.; Zekiy, A.; Benedicenti, S.; Pasquale, C. A narrative review on oral and periodontal bacteria microbiota photobiomodulation, through visible and near-infrared light: From the origins to modern therapies. Int. J. Mol. Sci. 2022, 23, 1372. [Google Scholar] [CrossRef]
- Hamblin, M.R. Mechanisms and mitochondrial redox signaling in photobiomodulation. Photochem. Photobiol. 2018, 94, 199–212. [Google Scholar] [CrossRef] [Green Version]
- Chow, R.T.; David, M.A.; Armati, P.J. 830 nm laser irradiation induces varicosity formation, reduces mitochondrial membrane potential and blocks fast axonal flow in small and medium diameter rat dorsal root ganglion neurons: Implications for the analgesic effects of 830 nm laser. J. Periph. Nerv. Syst. 2007, 12, 28–39. [Google Scholar] [CrossRef] [PubMed]
- Amaroli, A.; Marcoli, M.; Venturini, A.; Passalacqua, M.; Agnati, L.F.; Signore, A.; Raffetto, M.; Maura, G.; Benedicenti, S.; Cervetto, C.; et al. Near-infrared laser photons induce glutamate release from cerebrocortical nerve terminals. J. Biophot. 2018, 11, e201800102. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Huang, Y.; Wang, Y.; Lyu, P.; Hamblin, M.R. Photobiomodulation of human adipose-derived stem cells using 810 nm and 980 nm lasers operates via different mechanisms of action. Biochim. Biophys. Acta (BBA)-Gen. Subj. 2017, 1861, 441–449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santana-Blank, L.; Rodríguez-Santana, E.; Santana-Rodríguez, K.E.; Santana-Rodríguez, J.A.; Reyes, H. Water′s many roles in laser photobiomodulation. J. Canc. Res. Treat. 2015, 3, 1–5. [Google Scholar]
- Chan, A.; Armati, P.; Moorthy, A.P. Pulsed Nd:YAG laser induces pulpal analgesia: A randomized clinical trial. J. Dent. Res. 2012, 91, 79S–84S. [Google Scholar] [CrossRef]
- Ravera, S.; Ferrando, S.; Agas, D.; De Angelis, N.; Raffetto, M.; Sabbieti, M.G.; Signore, A.; Benedicenti, S.; Amaroli, A. 1064 nm Nd:YAG laser light affects transmembrane mitochondria respiratory chain complexes. J. Biophot. 2019, 12, e201900101. [Google Scholar] [CrossRef] [PubMed]
- Amaroli, A.; Benedicenti, A.; Ravera, S.; Parker, S.; Selting, W.; Panfoli, I.; Benedicenti, S. Short-pulse neodymium: Yttrium–aluminium garnet (Nd: YAG 1064 nm) laser irradiation photobiomodulates mitochondria activity and cellular multiplication of Paramecium primaurelia (Protozoa). Eur. J. Protistol. 2017, 61, 294–304. [Google Scholar] [CrossRef]
- Ribeiro, M.S.; Silva, D.D.F.T.D.; Maldonado, E.P.; de Rossi, W.; Zezell, D.M. Effects of 1047-nm neodymium laser radiation on skin wound healing. J. Clin. Laser Med. Surg. 2002, 20, 37–40. [Google Scholar] [CrossRef] [Green Version]
- Paulsen, E.; Korsholm, L.; Brandrup, F. A double-blind, placebo-controlled study of a commercial Aloe vera gel in the treatment of slight to moderate psoriasis vulgaris. J. Eur. Acad. Dermatol. Venereol. 2005, 19, 326–331. [Google Scholar] [CrossRef]
- Pasquale, C.; Colombo, E.; Benedicenti, S.; Signore, A.; Amaroli, A. 808-nm near-infrared laser photobiomodulation versus switched-off laser placebo in major aphthae management: A randomized double-blind controlled trial. Appl. Sci. 2021, 11, 4717. [Google Scholar] [CrossRef]
- Garg, A.; Kaur, D.; Sharma, S.; Abu Tahun, I.; Kumar, R. Evaluation of efficacy of 2% lidocaine gel and 20% benzocaine gel for topical anesthesia. Endodontology 2016, 28, 38–41. [Google Scholar] [CrossRef]
- Amaroli, A.; Arany, P.; Pasquale, C.; Benedicenti, S.; Bosco, A.; Ravera, S. Improving consistency of photobiomodulation therapy: A novel flat-top beam hand-piece versus standard gaussian probes on mitochondrial activity. Int. J. Mol. Sci. 2021, 22, 7788. [Google Scholar] [CrossRef] [PubMed]
- Laser Institute of America. American National Standard for Safe Use of Lasers. ANSI Z 136.1. 2014. Available online: https://www.lia.org/store/product/ansi-z1361-1014-safe-use-lasers-electronic-version (accessed on 25 June 2018).
- De Freiras, G.C.; Pozzobon, R.T.; Blaya, D.S.; Moreira, C.H. Efficacy of benzocaine 20% topical anesthetic compared to placebo prior to administration of local anesthesia in the oral cavity: A randomized controlled trial. Anesth. Prog. 2015, 62, 46–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malamed, S.F. Handbook of Local Anesthesia, 5th ed.; Elsevier Inc.: St. Louis, MO, USA, 2020. [Google Scholar]
- Rehman, N.; Qazi, S.R. efficacy of topical benzocaine in maxilla: A randomized controlled trial. Anesth. Prog. 2019, 66, 24–29. [Google Scholar] [CrossRef]
- Sirintawat, N.; Sawang, K.; Chaiyasamut, T.; Wongsirichat, N. Pain measurement in oral and maxillofacial surgery. J. Dent. Anesth. Pain Med. 2017, 17, 253–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faul, F. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Amaroli, A.; Ravera, S.; Parker, S.; Panfoli, I.; Benedicenti, A.; Benedicenti, S. 808-nm laser therapy with a flat-top handpiece photobiomodulates mitochondria activities of Paramecium primaurelia (Protozoa). Lasers Med. Sci. 2016, 31, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Amaroli, A.; Ravera, S.; Parker, S.; Panfoli, I.; Benedicenti, A.; Benedicenti, S. An 808-nm diode laser with a flat-top handpiece positively photobiomodulates mitochondria activities. Photomed. Laser Surg. 2016, 34, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Amaroli, A.; Agas, D.; Laus, F.; Cuteri, V.; Hanna, R.; Sabbieti, M.G.; Benedicenti, S. The effects of photobiomodulation of 808 nm diode laser therapy at higher fluence on the in vitro osteogenic differentiation of bone marrow stromal cells. Front. Physiol. 2018, 9, 123. [Google Scholar] [CrossRef] [Green Version]
- Amaroli, A.; Benedicenti, A.; Ferrando, S.; Parker, S.; Selting, W.; Gallus, L.; Benedicenti, S. Photobiomodulation by infrared diode laser: Effects on intracellular calcium concentration and nitric oxide production of Paramecium. Photochem. Photobiol. 2016, 92, 854–862. [Google Scholar] [CrossRef]
- Amaroli, A.; Pasquale, C.; Zekiy, A.; Utyuzh, A.; Benedicenti, S.; Signore, A.; Ravera, S. Photobiomodulation and oxidative stress: 980 nm diode laser light regulates mitochondrial activity and reactive oxygen species production. Oxidative Med. Cell Longev. 2021, 2021, 6626286. [Google Scholar] [CrossRef] [PubMed]
- Hamid, M.A.A.; Zaied, A.A.; Zayet, M.K.; Abdelmageed, H.; Hassan, E.A.; Amaroli, A. Efficacy of flat-top hand-piece using 980 nm diode laser photobiomodulation on socket healing after extraction: Split-mouth experimental model in dogs. Photochem. Photobiol. 2021, 97, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Chow, R.T.; Armati, P.J.; Laakso, E.-L.; Bjordal, J.M.; Baxter, G.D. Inhibitory effects of laser irradiation on peripheral mammalian nerves and relevance to analgesic effects: A systematic review. Photomed. Laser Surg. 2011, 29, 365–381. [Google Scholar] [CrossRef] [PubMed]
- Wesselmann, U.; Lin, S.F.; Rymer, W.Z. Effects of Q-switched Nd:YAG laser irradiation on neural impulse propagation: II. Dorsal Roots and Peripheral Nerves. Physiol. Chem. Phys. Med. NMR. 1991, 23, 81–100. [Google Scholar] [PubMed]
- Wesselmann, U.; Kerns, J.; Rymer, W. Laser effects in myelinated and nonmyelinated fibres in the rat peroneal nerve: A quantitative ultra- structural analysis. Exp. Neurol. 1994, 129, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Orchardson, R.; Peacock, J.M.; Whitters, C.J. Effect of pulsed Nd:YAG laser radiation on action potential conduction in isolated mammalian spinal nerves. Lasers Surg. Med. 1997, 21, 142–148. [Google Scholar] [CrossRef]
- Orchardson, R.; Peacock, J.; Whitters, C. Effects of pulsed Nd:YAG laser radiation on action potential conduction in nerve fibres inside teeth in vitro. J. Dent. 1998, 26, 421–426. [Google Scholar] [CrossRef]
- Karu, T. Is it time to consider photobiomodulation as a drug equivalent? Photomed. Laser Surg. 2013, 31, 189–191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kulkarni, S.; George, R.; Love, R.; Ranjitkar, S. Effectiveness of photobiomodulation in reducing pain and producing dental analgesia: A systematic review. Lasers Med. Sci. 2022, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sattayut, S. Low intensity laser for reducing pain from anesthetic palatal injection. Photomed. Laser Surg. 2014, 32, 658–662. [Google Scholar] [CrossRef] [PubMed]
- Tuk, J.G.; van Wijk, A.J.; Mertens, I.C.; Keleş, Z.; Lindeboom, J.A.; Milstein, D.M. Analgesic effects of preinjection low-level laser/light therapy (LLLT) before third molar surgery: A double-blind randomized controlled trial. Oral Surg. Oral Med. Oral Pathol Oral Radiol. 2017, 124, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Ghabraei, S.; Bolhari, B.; Nashtaie, H.M.; Noruzian, M.; Niavarzi, S.; Chiniforush, N. Effect of photobiomodulation on pain level during local anesthesia injection: A randomized clinical trial. J. Cosmet. Laser Ther. 2020, 22, 180–184. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekhar, R.; Vinay, C.; Uloopi, K.; RojaRamya, K.S.; AmruthaVarshini, I.; Penmatsa, C. Effectiveness of pre-cooling the injection site, laser biostimulation, and topical local anesthetic gel in reduction of local anesthesia injection pain in children. Int. J. Clin. Pediatr. Dent. 2021, 14, 81–83. [Google Scholar]
- Khin Hla, T.; Hegarty, M.; Russell, P.; Drake-Brockman, T.F.; Ramgolam, A.; von Ungern-Sternberg, B.S. Perception of paediatric pain: A comparison of postoperative pain assessments between child, parent, nurse, and independent observer. Paediatr. Anaesth. 2014, 24, 1127–1131. [Google Scholar] [CrossRef]
- Shekarchi, F.; Nokhbatolfoghahaei, H.; Chiniforush, N.; Mohaghegh, S.; Boroojeni, H.S.H.; Amini, S.; Biria, M. Evaluating the preemptive analgesic effect of photo-biomodulation therapy on pain perception during local anesthesia injection in children: A split-mouth triple-blind randomized controlled clinical trial. Photochem. Photobiol. 2022. [Google Scholar] [CrossRef]
- Uçar, G.; Şermet Elbay, Ü.; Elbay, M. Effects of low level laser therapy on injection pain and anesthesia efficacy during local anesthesia in children: A randomized clinical trial. Int. J. Paediatr. Dent. 2021, 32, 576–584. [Google Scholar] [CrossRef]
- Kermanshah, H.; Chiniforush, N.; Mohammadi, M.K.; Motevasselian, F. Effect of photobiomodulation therapy with 915 nm diode laser on pain perception during local anesthesia of maxillary incisors: A randomized controlled trial. Photochem. Photobiol. 2022. [Google Scholar] [CrossRef] [PubMed]
- Masocha, W.; Horvath, G.; Agil, A.; Ocana, M.; Del Pozo, E.; Szikszay, M.; Baeyens, J.M. Role of Na(+), K(+)-ATPase in morphine-induced antinociception. J. Pharmacol. Exp. Ther. 2003, 306, 1122–1128. [Google Scholar] [CrossRef] [Green Version]
- Whitters, C.; Hall, A.; Creanor, S.; Moseley, H.; Gilmour, W.; Strang, R.; Saunders, W.; Orchardson, R. A Clinical study of pulsed Nd: YAG laser-induced pulpal analgesia. J. Dent. 1995, 23, 145–150. [Google Scholar] [CrossRef]
- Chan, A.; Punnia-Moorthy, A.; Armati, P. Low-power pulsed Nd:YAG laser irradiation for pre-emptive anaesthesia: A morphological and histological study. Laser Ther. 2014, 23, 255–262. [Google Scholar] [CrossRef] [PubMed] [Green Version]




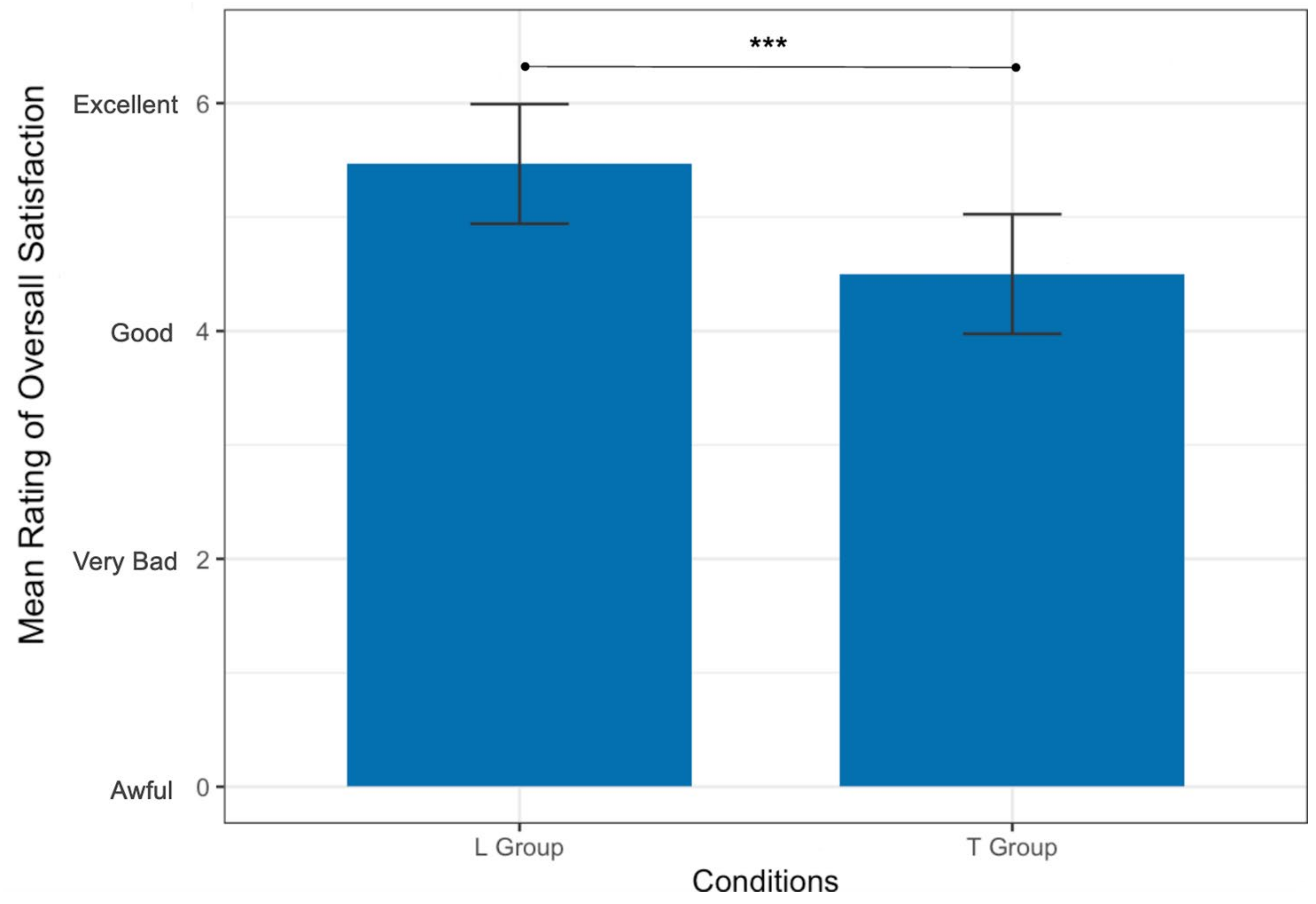
| Score | Taste | Undesirable Numbness | Overall Satisfaction |
|---|---|---|---|
| 1 | Awful | Awful | Awful |
| 2 | Very bad | Very severe | Very bad |
| 3 | Bad | Severe | Bad |
| 4 | Moderate | Moderate | Good |
| 5 | Mild | Mild | Very good |
| 6 | No taste | No numbness | Excellent |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El Feghali, R.; Tatarian, K.; Zogheib, C.; Benedicenti, S.; Pasquale, C.; Amaroli, A. The 1064-nm Nd:YAG Photobiomodulation vs. 20% Benzocaine Topical Gel in Inducing Mucosal Anesthetic Effect: A Double-Blind Randomized Clinical Trial. Photonics 2022, 9, 519. https://doi.org/10.3390/photonics9080519
El Feghali R, Tatarian K, Zogheib C, Benedicenti S, Pasquale C, Amaroli A. The 1064-nm Nd:YAG Photobiomodulation vs. 20% Benzocaine Topical Gel in Inducing Mucosal Anesthetic Effect: A Double-Blind Randomized Clinical Trial. Photonics. 2022; 9(8):519. https://doi.org/10.3390/photonics9080519
Chicago/Turabian StyleEl Feghali, Rita, Karen Tatarian, Carla Zogheib, Stefano Benedicenti, Claudio Pasquale, and Andrea Amaroli. 2022. "The 1064-nm Nd:YAG Photobiomodulation vs. 20% Benzocaine Topical Gel in Inducing Mucosal Anesthetic Effect: A Double-Blind Randomized Clinical Trial" Photonics 9, no. 8: 519. https://doi.org/10.3390/photonics9080519
APA StyleEl Feghali, R., Tatarian, K., Zogheib, C., Benedicenti, S., Pasquale, C., & Amaroli, A. (2022). The 1064-nm Nd:YAG Photobiomodulation vs. 20% Benzocaine Topical Gel in Inducing Mucosal Anesthetic Effect: A Double-Blind Randomized Clinical Trial. Photonics, 9(8), 519. https://doi.org/10.3390/photonics9080519








