Treatment Resistant Acneiform Eruption in a Young Female: A Diagnostic Pitfall
Abstract
1. Case Presentation
2. What Is the Diagnosis?
- A.
- Acne vulgaris
- B.
- Papulopustular rosacea
- C.
- Folliculotropic mycosis fungoides
- D.
- Lupus miliaris disseminatus faciei
- E.
- Cutaneous Sarcoidosis
3. Diagnosis
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MF | Mycosis fungoides |
| FMF | Folliculotropic mycosis fungoides |
| TCR | T-cell receptor |
| PUVA | psoralen plus UVA |
| PCR | Polymerase chain reaction |
References
- Mitteldorf, C.; Stadler, R.; Sander, C.A.; Kempf, W. Folliculotropic mycosis fungoides. J. Dtsch. Dermatol. Ges. 2018, 16, 543–557. [Google Scholar] [CrossRef] [PubMed]
- Hodak, E.; Amitay-Laish, I.; Atzmony, L.; Prag-Naveh, H.; Yanichkin, N.; Barzilai, A.; Kershenovich, R.; Feinmesser, M. New insights into folliculotropic mycosis fungoides (FMF): A single-center experience. J. Am. Acad. Dermatol. 2016, 75, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Muniesa, C.; Estrach, T.; Pujol, R.M.; Gallardo, F.; Garcia-Muret, P.; Climent, J.; Servitje, O. Folliculotropic mycosis fungoides: Clinicopathological features and outcome in a series of 20 cases. J. Am. Acad. Dermatol. 2010, 62, 418–426. [Google Scholar] [CrossRef] [PubMed]
- Shamim, H.M.; Riemer, C.; Weenig, R.; Sokumbi, O.; Sciallis, G.; McEvoy, M.; Mischke, D.; Comfere, N. Acneiform Presentations of Folliculotropic Mycosis Fungoides. Am. J. Dermatopathol. 2020, 43, 85–92. [Google Scholar] [CrossRef]
- van Santen, S.; Roach, R.E.J.; van Doorn, R.; Horváth, B.; Bruijn, M.S.; Sanders, C.J.G.; de Pooter, J.C.; van Rossum, M.M.; de Haas, E.R.M.; Veraart, J.C.J.M.; et al. Clinical Staging and Prognostic Factors in Folliculotropic Mycosis Fungoides. JAMA Dermatol. 2016, 152, 992–1000. [Google Scholar] [CrossRef]
- Marschalkó, M.; Erős, N.; Kontár, O.; Hidvégi, B.; Telek, J.; Hársing, J.; Jókai, H.; Bottlik, G.; Rajnai, H.; Szepesi, Á.; et al. Folliculotropic mycosis fungoides: Clinicopathological analysis of 17 patients. J. Eur. Acad. Dermatol. Venereol. 2014, 29, 964–972. [Google Scholar] [CrossRef] [PubMed]
- Petkovic, M.; Ceovic, R.; Drvar, D.L.; Rados, J.; Toncic, R.J. Dermoscopic and trichoscopic features of follicular mycosis fungoides: A systematic review. Ital. J. Dermatol. Venereol. 2025, 160, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Geller, S.; Rishpon, A.; Myskowski, P.L. Dermoscopy in folliculotropic mycosis fungoides—A possible mimicker of follicle-based inflammatory and infectious disorders. J. Am. Acad. Dermatol. 2019, 81, e75–e76. [Google Scholar] [CrossRef] [PubMed]
- Scarisbrick, J.; Quaglino, P.; Prince, H.; Papadavid, E.; Hodak, E.; Bagot, M.; Servitje, O.; Berti, E.; Ortiz-Romero, P.; Stadler, R.; et al. The PROCLIPI international registry of early-stage mycosis fungoides identifies substantial diagnostic delay in most patients. Br. J. Dermatol. 2018, 181, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Skov, A.; Gniadecki, R. Delay in the Histopathologic Diagnosis of Mycosis Fungoides. Acta Dermato-Venereol. 2015, 95, 472–475. [Google Scholar] [CrossRef] [PubMed]
- Leal, S.; Villamizar, M.; Rojas, P.; Rueda, X. Folliculotropic Mycosis Fungoides Masquerading as Nodulocystic Acne: A Diagnostic Challenge. Cureus 2025, 17, e88442. [Google Scholar] [CrossRef] [PubMed]
- Deeths, M.J.; Chapman, J.T.; Dellavalle, R.P.; Zeng, C.; Aeling, J.L. Treatment of patch and plaque stage mycosis fungoides with imiquimod 5% cream. J. Am. Acad. Dermatol. 2005, 52, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Coors, E.A.; Schuler, G.; Von Den Driesch, P. Topical imiquimod as treatment for different kinds of cutaneous lymphoma. Eur. J. Dermatol. 2006, 16, 391–393. [Google Scholar] [PubMed]

| Disease | Sites Affected | Clinical Presentation | Histopathological Findings |
|---|---|---|---|
| Acne vulgaris | Face (esp. T-zone), chest, back | Comedones, papules, pustules, nodules; scarring | Dilated keratotic follicles, sebaceous gland hypertrophy, C. acnes colonization, neutrophilic inflammation; comedones, papules, pustules |
| Papulopustular rosacea | Central face (cheeks, nose, chin, forehead) | Central facial papules/pustules on erythematous background, flushing, telangiectasia, no comedones present | Perifollicular/perivascular lymphohistiocytic infiltrate, telangiectasia, Demodex may be present; granulomas in granulomatous subtype |
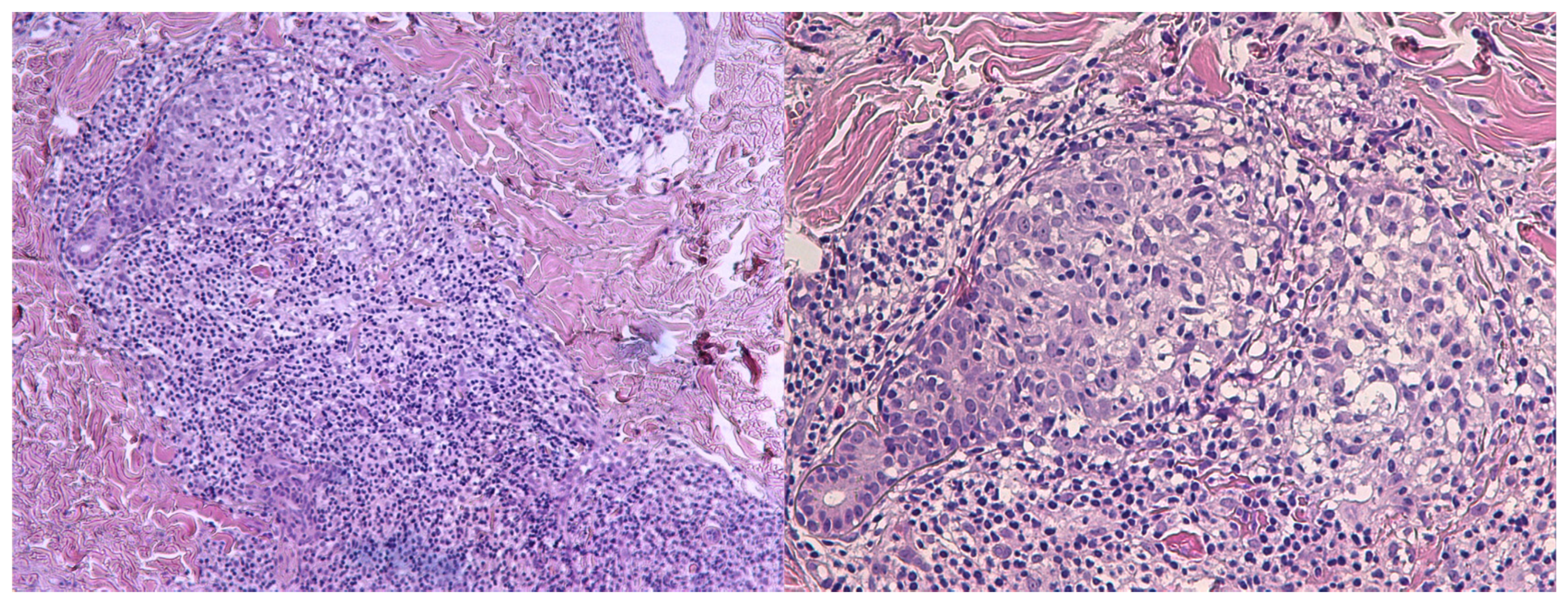
| Folliculotropic mycosis fungoides | Face (esp. head/neck), trunk, extremities | Follicular papules, acneiform lesions, plaques, alopecia, often pruritic, refractory to standard acne therapy | Dense perifollicular infiltrate of atypical CD4+ T-cells with folliculotropism, follicular mucinosis, possible large cell transformation |
| Lupus miliaris disseminatus faciei | Central face (esp. eyelids, periorbital, cheeks) | Symmetric, monomorphic, reddish-brown papules/nodules, often periorbital, scarring | Dermal epithelioid granulomas with central caseation necrosis, minimal inflammation; no mycobacterial DNA |
| Cutaneous Sarcoidosis | Face (esp. nose, periorbital, cheeks), other sites | Red-brown to violaceous papules/plaques, often chronic, may ulcerate or scar; may have systemic symptoms | Noncaseating granulomas in dermis, sparse lymphocytic infiltrate, no central necrosis |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the European Society of Dermatopathology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koumprentziotis, I.-A.; Panou, E.; Tsimpidakis, A.; Gerochristou, M.; Iliakis, T.; Marinos, L.; Stratigos, A.; Nikolaou, V. Treatment Resistant Acneiform Eruption in a Young Female: A Diagnostic Pitfall. Dermatopathology 2025, 12, 32. https://doi.org/10.3390/dermatopathology12030032
Koumprentziotis I-A, Panou E, Tsimpidakis A, Gerochristou M, Iliakis T, Marinos L, Stratigos A, Nikolaou V. Treatment Resistant Acneiform Eruption in a Young Female: A Diagnostic Pitfall. Dermatopathology. 2025; 12(3):32. https://doi.org/10.3390/dermatopathology12030032
Chicago/Turabian StyleKoumprentziotis, Ioannis-Alexios, Evdoxia Panou, Antonis Tsimpidakis, Maria Gerochristou, Theodoros Iliakis, Leonidas Marinos, Alexander Stratigos, and Vasiliki Nikolaou. 2025. "Treatment Resistant Acneiform Eruption in a Young Female: A Diagnostic Pitfall" Dermatopathology 12, no. 3: 32. https://doi.org/10.3390/dermatopathology12030032
APA StyleKoumprentziotis, I.-A., Panou, E., Tsimpidakis, A., Gerochristou, M., Iliakis, T., Marinos, L., Stratigos, A., & Nikolaou, V. (2025). Treatment Resistant Acneiform Eruption in a Young Female: A Diagnostic Pitfall. Dermatopathology, 12(3), 32. https://doi.org/10.3390/dermatopathology12030032






