1. Introduction
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) that causes the coronavirus disease-2019 (COVID-19) is a novel coronavirus that has a high fatality and morbidity rate [
1]. After receiving reports of 118,000 cases and 4291 deaths in 114 nations, the World Health Organization (WHO) declared COVID-19 a pandemic on 11 March 2020 [
2]. Globally, as of 15 July 2022, there were more than 6.4 million reported fatalities and over 565.6 million confirmed cases [
1]. As the novel coronavirus continues to evolve, there are still many limitations to our knowledge of who exactly this virus would impact critically.
In light of the current circumstances surrounding the global COVID-19 pandemic, this study delves into the intricacies of post-hospitalisation mortality risk among patients in South Africa’s Limpopo province. The unprecedented challenges posed by the pandemic have necessitated a thorough understanding of the factors influencing patient outcomes. By investigating these factors, we aim to shed light on the complexities of COVID-19 mortality risk, offering insights that can aid healthcare professionals, policymakers, and researchers in navigating the evolving landscape of patient care.
Indeed, the COVID-19 pandemic has prompted extensive research into understanding the disease’s clinical manifestations, risk factors, and outcomes. Mortality risk assessment is a pivotal aspect of this research, aiming to identify the factors contributing to higher mortality rates among patients hospitalised due to laboratory-confirmed COVID-19. Theoretical frameworks have underscored several critical concepts in this context. For instance, clinical severity and the presence of comorbidities have been identified as key factors influencing outcomes. Severe cases that necessitate hospitalisation are often linked to adverse outcomes, while patients with pre-existing conditions such as diabetes, cardiovascular diseases, and respiratory ailments face an elevated mortality risk [
3,
4].
Additionally, the immune response to COVID-19 plays a pivotal role in disease progression and outcomes. Dysregulated immune responses, including cytokine storms, have been associated with severe cases and poor outcomes [
5]. Furthermore, age and gender are established risk factors for severe outcomes. Older adults are more vulnerable, and gender differences in mortality rates have been observed, with males generally experiencing higher mortality [
6].
A number of studies have investigated the factors that influence post-hospitalisation mortality risk. For instance, [
7] examined a cohort of COVID-19 patients and found that advanced age, high Sequential Organ Failure Assessment (SOFA) scores, and elevated d-dimer levels were associated with increased mortality risk post-hospitalisation.
Another significant study by [
8] identified age, male sex, and various comorbidities (such as diabetes, obesity, and cardiovascular diseases) as independent risk factors for COVID-19-related mortality. Another study by [
9] highlighted ethnic and racial disparities that impact mortality risk, with Black and Asian individuals having higher mortality risks even after adjusting for age, sex, and comorbidities.
On 27 March 2020, South Africa experienced its first COVID-19 fatality [
10]. Since then, the nation has recorded 88.9 thousand citizen deaths due to the pandemic. Furthermore, 839 people died on 19 January 2021, the largest daily death reported during the outbreak. South Africa was the most affected nation in the region as of 24 October 2021, with more than 2.91 million infection cases [
11]. The South Africa National Institute for Communicable Diseases (NICD) verified the country’s first COVID-19 case on 5 March 2020 [
10,
11]. Since then, the South African government has successfully implemented a robust and successful national response to stop COVID-19 (see SAResponsetoCOVID-19, 2020, for main steps and dates [
10]).
Be that as it may, it has become crucial to look back and examine the mortality and associated risk factors among COVID-19 hospitalised patients in the Limpopo province of South Africa as we continue to count the costs of the devastating effects of the pandemic. Indeed, pinpointing the causes of mortality among COVID-19 patients in both urban and rural contexts within the province could help us better understand the disease and the necessity of these findings in developing efficient preventive and therapeutic strategies for future pandemics.
Several studies have identified age, underlying medical conditions, severity of illness, and laboratory markers as significant risk factors associated with mortality rate [
12,
13]. However, there are still gaps in the literature regarding the long-term outcomes of COVID-19 patients, especially those who survive hospitalisation. Most studies have focused on short-term outcomes, such as mortality rates during hospitalisation, and there is a need for more research on the long-term outcomes of COVID-19 patients. Again, some studies have only included patients from specific regions or populations, limiting their findings’ generalisability. Generally, more research is needed to fully understand the risk factors associated with mortality among hospitalised COVID-19 patients and to improve the accuracy of predicting patient outcomes. The study aims to conduct a retrospective post-hospitalisation COVID-19 mortality risk assessment of patients in the Limpopo province of South Africa.
It is envisaged that the findings of this study will help improve our understanding of the factors that influence mortality rate among hospitalised COVID-19 patients and help us identify potential interventions that may improve patient outcomes. The outline of the paper is as follows: literature review and materials and methods are presented in
Section 2 and
Section 3, respectively. The results and discussions are presented in
Section 4, ending with the concluding remarks in
Section 5.
2. Literature Review
The COVID-19 pandemic has spurred extensive research aimed at understanding the clinical aspects, risk factors, and management strategies for patients affected by the virus. In this context, several studies have sought to uncover predictive factors for COVID-19 severity, mortality risk, and the specific implications for patients with comorbidities such as diabetes mellitus and hypertension.
Zhou et al. (2021) employed machine learning techniques to analyse longitudinal measurements and identified eleven routine clinical features that effectively predict the severity of COVID-19 cases, offering valuable insights into risk assessment [
14]. Similarly, Onder et al. (2020) examined case-fatality rates in Italy, elucidating characteristics associated with patients who succumbed to COVID-19 and contributing to understanding disease outcomes [
15].
The management of diabetes mellitus (DM) amid the COVID-19 pandemic presented unique challenges. Koliaki et al. (2020) discussed practical issues and concerns surrounding the clinical management of DM patients during the pandemic [
16]. In their research, [
17] focused on inpatient COVID-19 mortality risk assessments, specifically exploring the interplay of diabetes mellitus. Their study employed interpretable machine learning models, enhancing the understanding of mortality risks in patients with diabetes.
The intersection of COVID-19 and diabetes mellitus has been a topic of significant interest. Investigating mortality outcomes, [
18] highlighted that patients with both COVID-19 and diabetes face increased mortality risks, emphasizing the importance of tailored interventions. Yang et al. (2020) developed predictive models for clinical deterioration among COVID-19 patients, utilizing machine learning and readily available clinical data to enhance prognosis accuracy [
19].
In another dimension, short-term outcomes of newly diagnosed diabetes in COVID-19 patients were explored by Zhou et al. (2020). They identified distinct types of diabetes arising from COVID-19 infection, deepening our understanding of the complexities of these intertwined conditions [
3].
In terms of long-term outcomes, a study by [
20] found that nearly one-third of COVID-19 patients experienced long-term symptoms such as fatigue and shortness of breath, even after hospitalisation. This highlights the importance of understanding the long-term outcomes of COVID-19 patients beyond just survival time. A study by [
20] found that COVID-19 patients with severe illness who received convalescent plasma therapy had a lower risk of mortality compared to those who did not receive the therapy. This suggests that convalescent plasma therapy may be an effective intervention for improving patient outcomes.
Bambra et al. (2020) delve into gender-based health disparities brought about by the COVID-19 pandemic, drawing insights from the concept of the ‘gender health paradox’. This paradox highlights the consistent finding that men generally have higher mortality rates and shorter life expectancies, while women report higher levels of morbidity. Their study introduces the ‘gender health paradox’ and the various explanations encompassing biological, social, economic, and political factors contributing to it. They also discuss international data on gender-based inequalities in COVID-19 morbidity and mortality rates, indicating that women tend to be diagnosed more frequently, yet men exhibit higher mortality rates. They further examine the potential long-term consequences of the pandemic’s aftermath on gender-based health inequalities, focusing on the repercussions of government policy responses and the emerging economic crisis. It suggests that these factors might lead to increased mortality among men and heightened morbidity among women [
21].
In another study, Muñoz-Price et al. (2020) looked into the association between race and COVID-19 outcomes, considering variables such as age, sex, socioeconomic status, and comorbidities. Their study involves 2595 adults tested for COVID-19 and explores factors related to COVID-19 positivity, hospitalisation, intensive care unit admission, mechanical ventilation, and death. The findings indicate that the Black race is associated with an increased likelihood of COVID-19 positivity (odds ratio [OR], 5.37), and this association remains after adjusting for factors like age and sex [
22].
Campbel et al. (2021) [
23] develop predictive models that stratify hospitalised COVID-19 patients by their risk of severe outcomes, such as ICU admission, acute respiratory distress syndrome development, or intubation. The models were designed using hierarchical ensemble classification techniques and trained on a dataset of 229 COVID-19 patients. These models utilised easily accessible information, including patient characteristics, vital signs at admission, and basic lab results. The assessment of the models was based on precision (positive predictive value) and recall (sensitivity) to determine their ability to categorise patients into increasing risk groups. The study used a separate cohort of 330 patients for validation, maintaining pre-defined test cut-offs. The results showed that the models achieved high precision, particularly in the lowest risk groups, and the proportion of severe outcomes consistently increased with escalating risk groups. Notably, attributes such as C-reactive protein, lactate dehydrogenase, and D-dimer were frequently identified as significant contributors to the risk assessments. The study concluded that machine learning-based models utilising routinely collected admission data can effectively assess the risk of severe outcomes in COVID-19 patients during hospitalisation [
23].
While a substantial body of research has illuminated the retrospective post-hospitalisation COVID-19 mortality risk assessment among patients in South Africa, a notable gap exists in the comprehensive exploration of survival models, specifically tailored to this population. While studies by [
24,
25], among others, have delved into patient-specific characteristics and the potential of machine learning, there is still a distinct lack of studies focusing on implementing survival analysis techniques. Survival models, encompassing Kaplan-Meier estimators and Cox proportional hazards models, offer a nuanced perspective by accounting for time-to-event outcomes. These models could provide insights into the temporal patterns of mortality and uncover factors that may be time-dependent in influencing post-hospitalisation COVID-19 mortality. Furthermore, survival analysis can be particularly valuable in understanding the long-term implications of COVID-19 and capturing the dynamics of recovery and mortality beyond the immediate hospitalisation period. Addressing this gap by incorporating survival models into the assessment framework can contribute to a more comprehensive understanding of mortality risk factors and guide the development of targeted interventions.
4. Results and Discussion
This section presents the study results and discussion, utilising secondary data from the Department of Health in the Limpopo province in South Africa. The data were collected on patients who had COVID-19 and symptoms of the disease admitted across Limpopo province hospitals, and the data is accessed in Microsoft Excel format.
Table 1 presents the description of the variables and the dataset codes. Data for survival regression models require a specific structure, and variables that did not meet the standard were omitted from the analysis.
At the outset of our analysis, we initiated an extensive exploration of the dataset utilizing descriptive statistics, as demonstrated in
Table 2. This fundamental phase provides us with a valuable opportunity to grasp the distribution and grouping of patients across various categories. Through our engagement with descriptive statistics, we establish a solid groundwork for our ensuing analyses, facilitating the discovery of inherent patterns, emerging trends, and prospective insights that will underpin our research endeavours.
The descriptive statistics from
Table 2 and
Figure 1 offer valuable insights into the characteristics of the study population and their relevance to the topic in terms of mortality rates and risk factors associated with COVID-19. The descriptive statistics tables provide a comprehensive overview of various aspects within the context of the research on retrospective post-hospitalisation COVID-19 mortality risk assessment of patients in South Africa. These tables offer insights into different variables related to the study population. In terms of gender distribution, 52.6% of patients were female, and 47.4% were male. The distribution across facility types indicates that 49.2% were in private general hospitals, 42.5% in district hospitals, and 8.2% in provincial tertiary hospitals. Regarding districts, 68.8% of patients were from Capricorn, 27.8% from Mopani, and 3.4% from Waterberg. The outcomes of hospitalisation show that 76.3% of patients died in the hospital, while 23.7% were discharged alive. Comorbidity prevalence is detailed across
Table 2, with conditions like hypertension (87.9% without, 12.1% with), diabetes (83.5% without, 16.5% with), asthma (89.9% without, 10.1% with), chronic pulmonary disease (94.1% without, 5.9% with), tuberculosis (90.7% without, 9.3% with) (
Table 2), and obesity (86.3% without, 13.7% with). Oxygenation (46.4% received oxygen, 53.6% did not) and ventilation (18.6% received ventilation, 81.4% did not) during hospitalisation are also highlighted. These statistics collectively provide a comprehensive understanding of the demographic, clinical, and intervention-related characteristics of the study population, contributing to a comprehensive assessment of COVID-19 mortality risk among patients in South Africa.
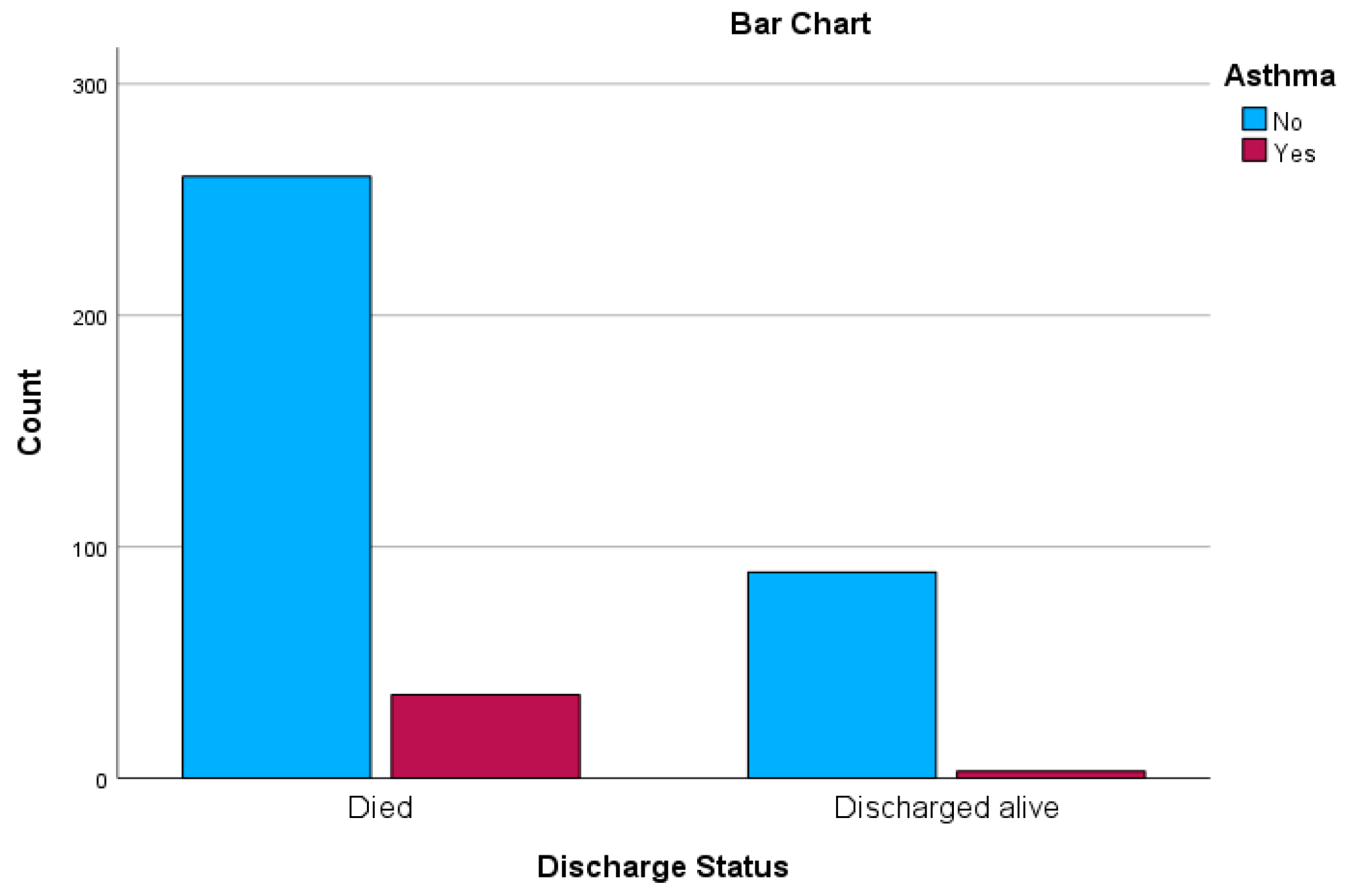
In the upcoming sections, we introduce crosstabulation as an integral component of our results and discussion presentation, with the intention of delving further into the intricate interplay between variables. This analytical methodology provides us with the means to investigate the mutual influence of diverse factors on outcomes, thereby revealing potential associations that may be obscured otherwise. Through the utilisation of crosstabulation, we have the opportunity to unearth subtle insights that enrich our comprehension of the intricate dynamics inherent to our research domain. These results are presented in
Table 3 and
Table 4, together with graphs in
Figure 1 and
Figure 2 displaying the distribution of hypertension and asthma in relation to discharged status.
Table 3 presents the results of Chi-Square tests assessing the association between the presence of hypertension and the discharge status of patients in the context of the research. These tests aim to determine whether there is a significant relationship between the two variables—hypertension and discharged status—and to ascertain if the presence of hypertension has an impact on the likelihood of being discharged alive or dying after hospitalisation.
The Pearson Chi-Square test statistic is 10.496 with one degree of freedom, yielding an asymptotic significance level of 0.001. This indicates a statistically significant relationship between hypertension and discharged status. The Continuity Correction Chi-Square value is 9.344 with the same degrees of freedom and a significance level of 0.002, which further strengthens the evidence of a significant association. The Likelihood Ratio test also yields a Chi-Square value of 9.380 with one degree of freedom and a significance level of 0.002.
The Fisher’s Exact Test, often employed when dealing with small cell sizes, demonstrates a significant exact two-sided p-value of 0.003 and a significant one-sided p-value of 0.002. This indicates a notable relationship between hypertension and discharged status, even when considering smaller sample sizes or rare occurrences.
Similarly,
Table 4 presents the outcomes of Chi-Square tests investigating the association between the presence of asthma and the discharge status of patients within the research context. These tests aim to establish whether there is a significant relationship between these two variables and whether the presence of asthma affects the likelihood of being discharged alive or dying following hospitalisation.
The Pearson Chi-Square test statistic results in a value of 6.151 with one degree of freedom, yielding a two-sided asymptotic significance level of 0.013. This indicates a statistically significant connection between asthma and discharged status, suggesting that asthma might influence patient outcomes after hospitalisation for COVID-19. Similarly, the Continuity Correction Chi-Square value is 5.206 with a significance level of 0.023, strengthening the evidence of a significant association.
The Likelihood Ratio test yields a Chi-Square value of 7.577 with one degree of freedom and a significance level of 0.006. This further emphasises the statistically significant relationship between asthma and discharge status.
The Fisher’s Exact Test, designed for small cell sizes, exhibits an exact two-sided p-value of 0.010 and a one-sided p-value of 0.007. These small p-values suggest a noteworthy association between asthma and the likelihood of being discharged or dying after COVID-19 hospitalisation, even when considering smaller sample sizes or rare occurrences.
Importantly, all expected cell counts in the table are greater than 5, and the minimum expected count is 9.25, satisfying the prerequisite for the application of Chi-Square tests. The tests are computed for a 2 × 2 table.
In summary, the findings of
Table 4 underscore a statistically significant link between the presence of asthma and the discharge status of patients post-hospitalisation. This suggests that asthma might have a discernible impact on the outcomes of COVID-19 patients, potentially influencing the course of their recovery or mortality. These results hold implications for healthcare strategies and patient care approaches, warranting further investigation into the relationship between asthma and COVID-19 outcomes.
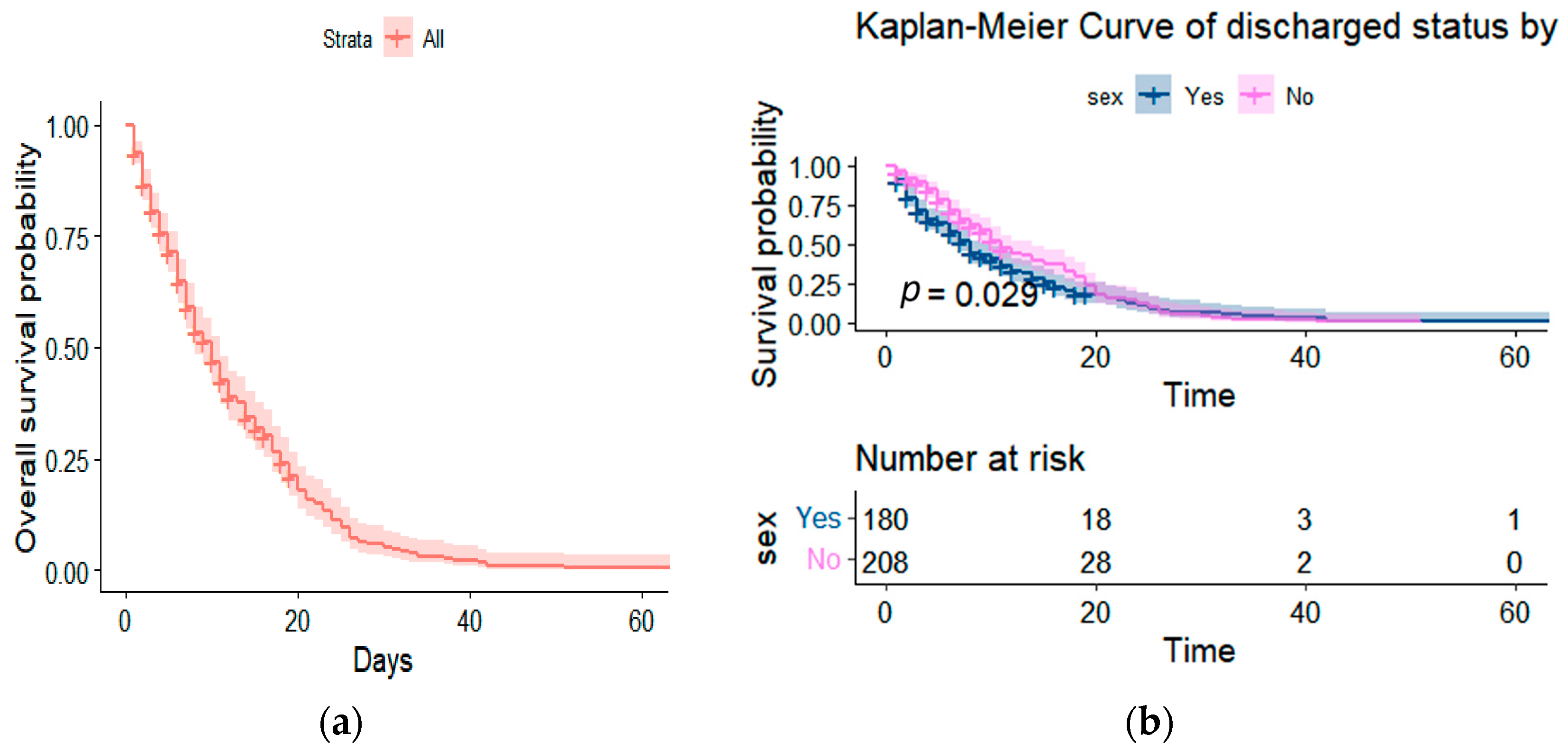
Before delving into the application of semiparametric and parametric models, we begin our analysis by examining the Kaplan-Meier survival function. Initially, we explore the overall survival function to gain a holistic view of the mortality trends within our dataset. Additionally, we dissect this function based on gender, allowing us to discern potential disparities in survival probabilities between male and female patients. These preliminary steps pave the way for a comprehensive investigation of our data, enabling us to subsequently fit semiparametric and parametric models. We aim to unravel the complex interplay of variables influencing COVID-19 mortality outcomes through these models.
It is also evident from
Figure 3 that the overall survival of patients for the first 60 days declines steadily, with the survival function amongst males and females being significant, with a
p-value of 0.029.
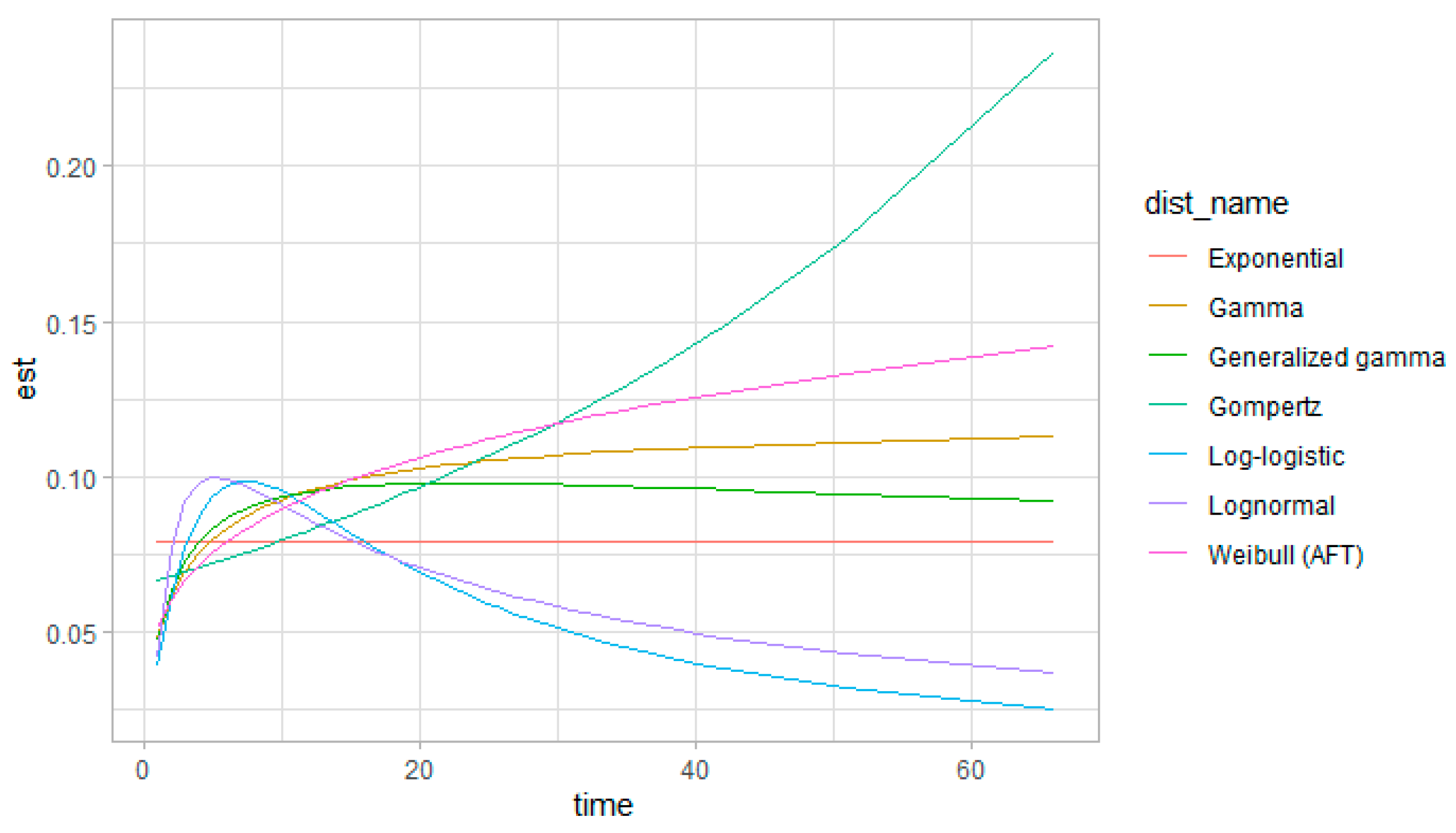
In our pursuit to comprehensively understand the intricate landscape of COVID-19 mortality risk assessment among post-hospitalised patients in South Africa, we turn our attention to the fitting of semiparametric and parametric models. These advanced analytical techniques hold the potential to unravel the multifaceted associations between various risk factors and mortality outcomes. By applying semiparametric and parametric models, we endeavour to go beyond descriptive insights, delving into the underlying mechanisms that drive mortality trends. Through this approach, we aspire to unearth valuable insights that can inform targeted interventions and strategies for improving patient outcomes within the context of the South African healthcare landscape. These models were compared using the loglikelihood after checking the underlying assumptions. The selected model is presented in
Table 5, whereas the competitive models are presented in
Appendix A.
When comparing the models and selecting the best-fitted one based on loglikelihood and AIC, it is essential to consider the assumptions and clinical relevance of the models in addition to their statistical fit. The frailty regression model presented in
Table 5 has a higher loglikelihood −1237.52 compared to the parametric survival models displayed in
Appendix A. Again, the frailty regression model has the advantage of directly accounting for frailty, which may have clinical relevance to our problem statement. This model assumes a random effect for frailty, allowing for individual heterogeneity in the baseline hazard.
Table 5 presents a comprehensive analysis of parameter estimates within the frailty regression model, offering valuable insights into the mortality risk assessment of post-hospitalised COVID-19 patients in the context of the research topic. Each parameter estimate, along with its associated Hazard Ratio (HR), 95% Confidence Interval (CI), and
p-value, provides a detailed understanding of the impact of various characteristics on mortality outcomes.
Among the factors examined, the presence of asthma does not appear to exert a statistically significant influence on mortality risk, as evidenced by the non-significant HR of 0.83 (95% CI: 0.48 to 1.46, p = 0.5). This suggests that asthma might not play a substantial role in determining COVID-19-related mortality among the studied patients. In contrast, diabetes emerges as a significant contributor to mortality risk, with patients having a 1.69 times higher hazard of mortality (95% CI: 1.03 to 2.76, p = 0.038) compared to those without diabetes. This emphasises the importance of managing diabetes as a crucial comorbidity to mitigate the risk of adverse outcomes following COVID-19 hospitalisation.
Hypertension stands out as a notable risk factor, significantly elevating the hazard of mortality. Patients with hypertension exhibit a substantial 3.31 times higher hazard of mortality (95% CI: 1.61 to 6.81, p = 0.001), underscoring the critical need to address this comorbidity in COVID-19 patient management strategies. Intriguingly, tuberculosis seems to have a protective effect, resulting in a reduced hazard of mortality among affected patients. The HR of 0.38 (95% CI: 0.18 to 0.79, p = 0.010) implies that individuals with tuberculosis experience a lower risk of mortality, suggesting potential immune responses or effective medical interventions associated with tuberculosis that warrant further investigation.
Notably, obesity does not significantly alter mortality risk among the studied patients, as indicated by an HR of 0.74 (95% CI: 0.42 to 1.30, p = 0.3). This implies that obesity might not play a prominent role in influencing mortality outcomes in this specific context. Geographic disparities are also evident, with patients from the Capricorn district facing an alarmingly higher hazard of mortality (HR: 17.1, 95% CI: 7.61 to 38.3, p < 0.001) compared to the reference district, Mopani. This highlights the need to address regional variations in healthcare access and outcomes.
Medical interventions play a significant role as well. Ventilation during hospitalisation is associated with a substantial reduction in the hazard of mortality (HR: 0.34, 95% CI: 0.22 to 0.54, p < 0.001), underlining its critical importance in the treatment of severe COVID-19 cases. Gender differences also come to the forefront, with males having a higher hazard of mortality (HR: 1.55, 95% CI: 1.09 to 2.21, p = 0.015), suggesting potential gender-related disparities in COVID-19 outcomes.
In the broader context of our problem, these parameter estimates provide invaluable insights into the intricate interplay between various characteristics and mortality risks among post-hospitalised COVID-19 patients. These findings hold profound implications for healthcare interventions and patient management strategies. Addressing diabetes, hypertension, regional disparities, and medical interventions such as ventilation become imperative for improving outcomes. Overall, these parameter estimates significantly contribute to our understanding of COVID-19 mortality risk assessment and offer crucial guidance for tailored strategies to enhance patient care and outcomes in South Africa.
In relation to previous research, diabetes is identified as a significant risk factor for mortality, aligning with previous studies that have consistently reported the detrimental impact of diabetes on COVID-19 outcomes [
20,
30,
31]. Similarly, hypertension is found to be strongly associated with increased mortality risk, corroborating evidence suggesting hypertension as a risk factor for severe illness in COVID-19 patients [
30,
31]. Nonetheless, these results have implications for risk stratification and targeted interventions to improve patient care and outcomes. They can inform healthcare providers in identifying and providing appropriate care to individuals with diabetes and hypertension who are at higher risk of mortality. Additionally, the findings highlight the need for integrated care for individuals with comorbidities to optimise COVID-19 management and reduce mortality rates. Further studies are warranted to validate these findings and explore potential mechanisms underlying the observed associations.