A Decade of Change in Susceptibility Patterns of Gram-Negative Blood Culture Isolates: A Single Center Study
Abstract
Background
Methods
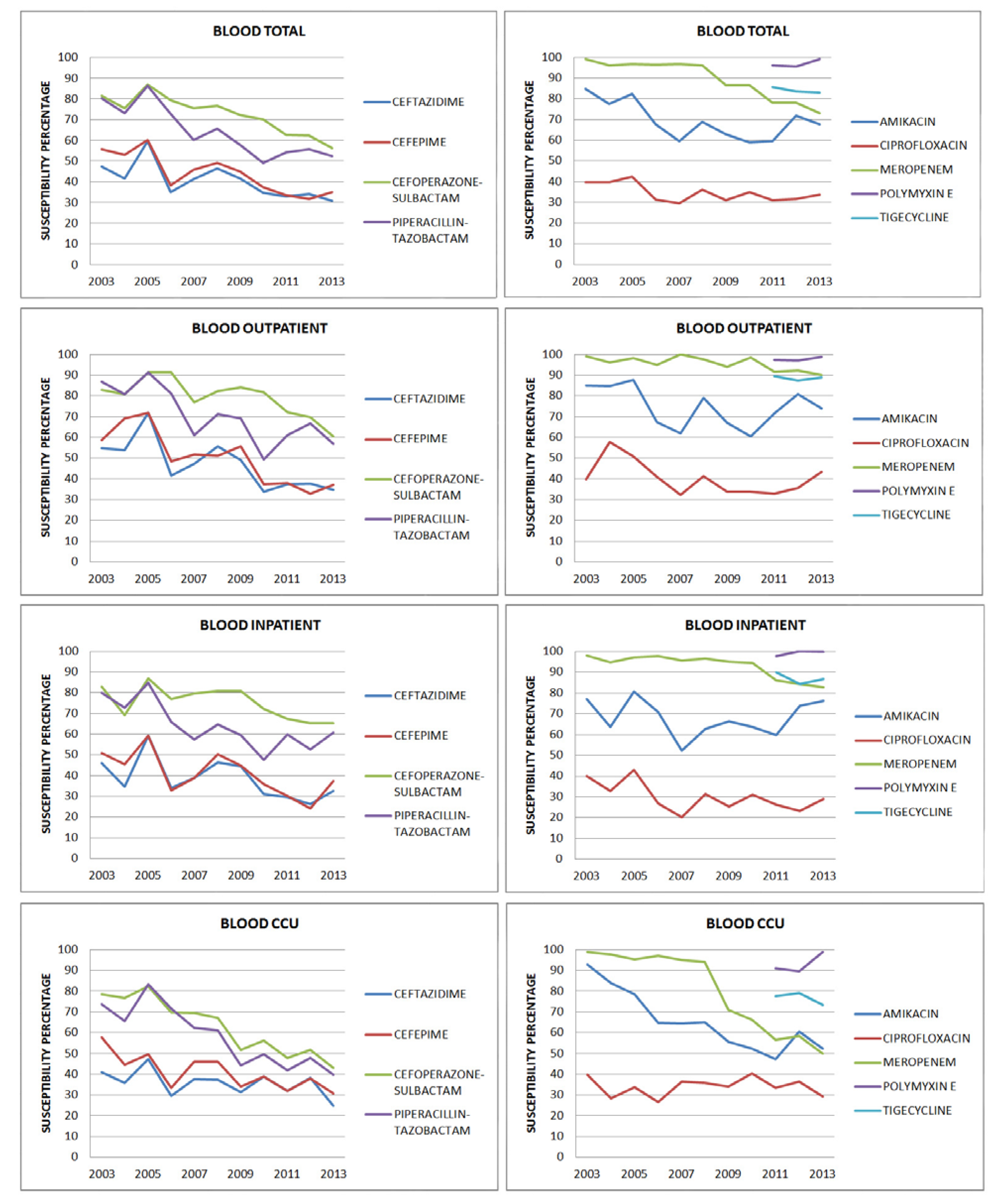
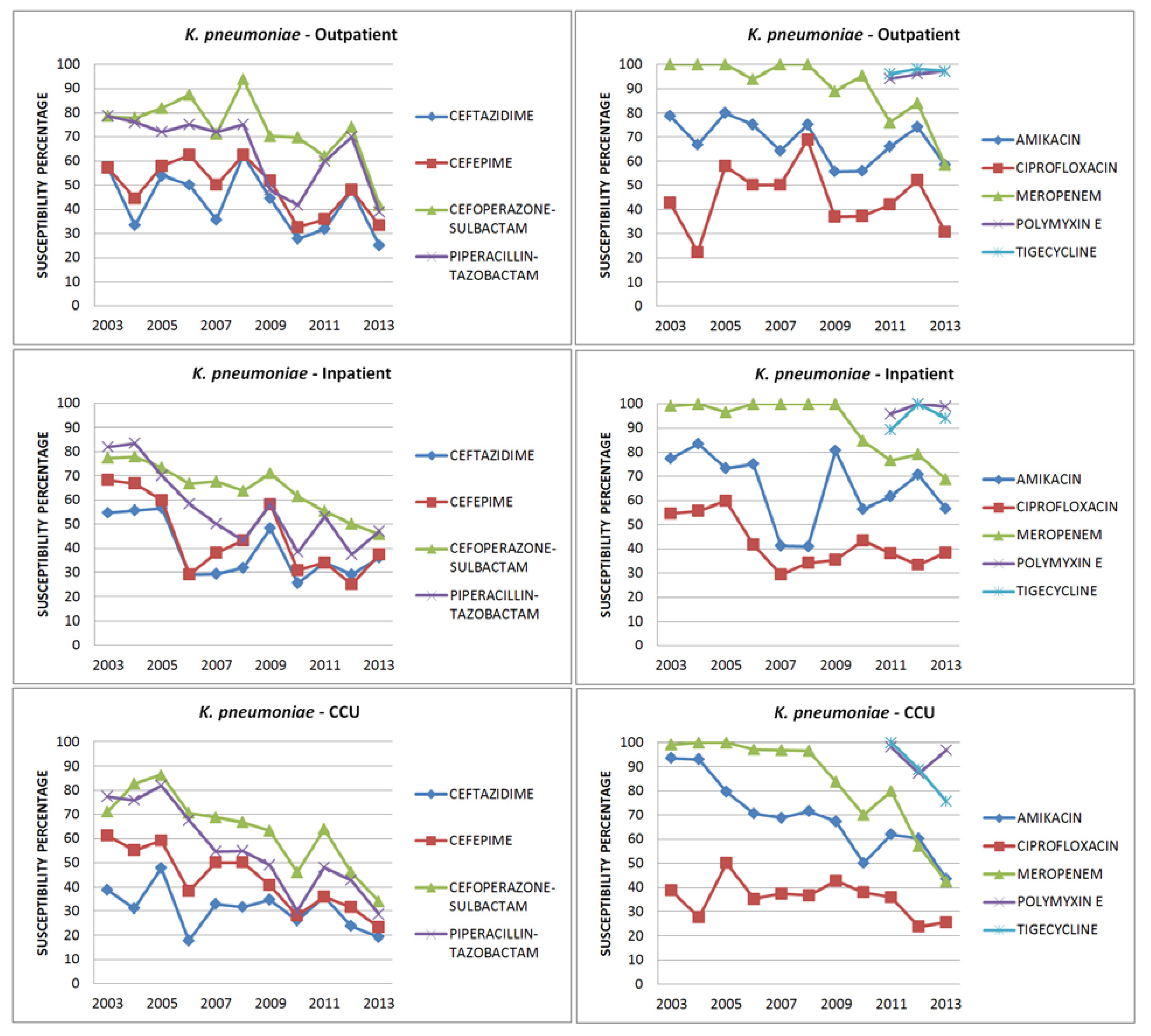
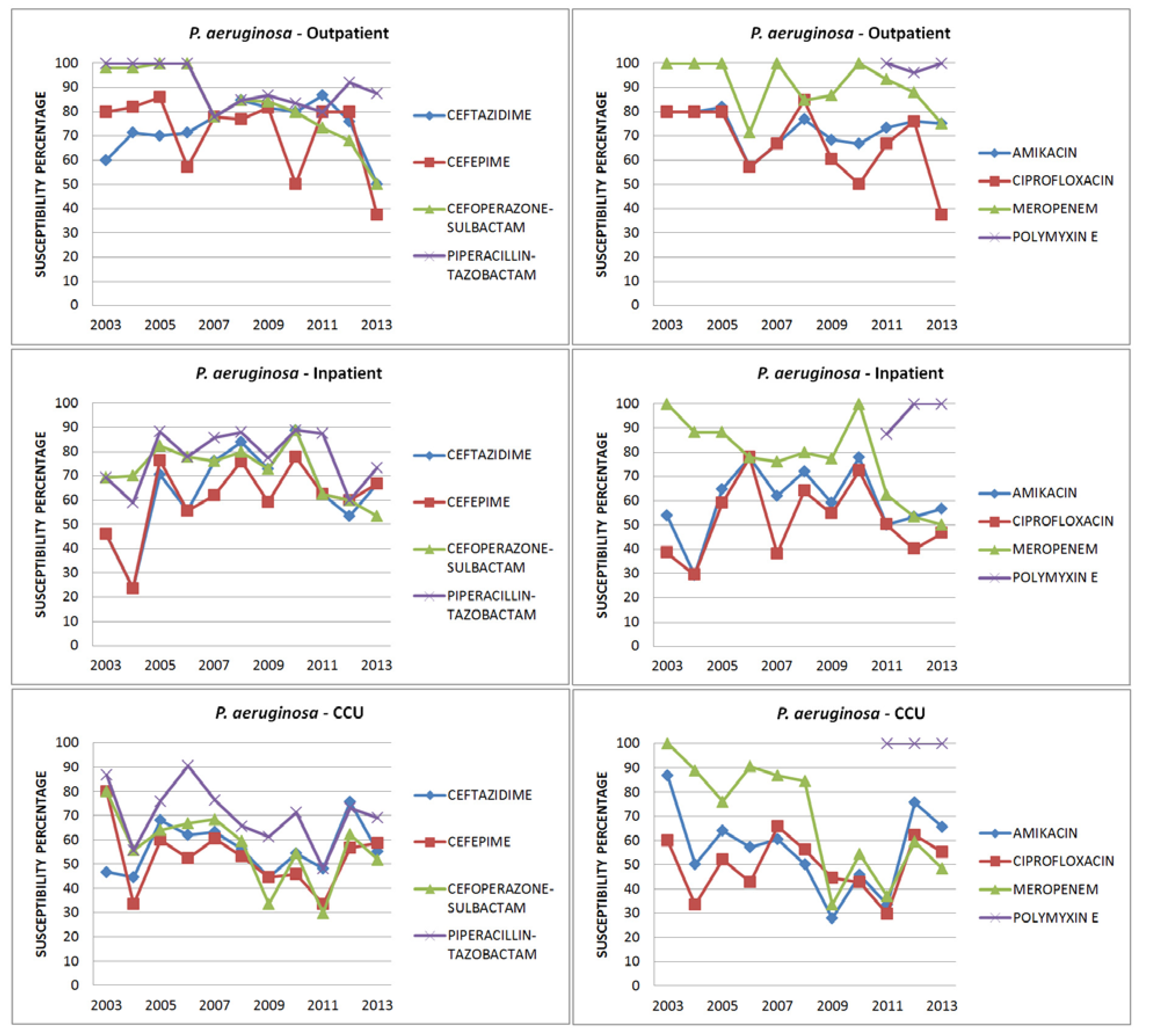
Results
| Ceftazidime | Cefepime | |||||||
|---|---|---|---|---|---|---|---|---|
| 2003 % | 2013 % | Resistance comparison 2003 vs. 2013 | 2003 % | 2013 % | Resistance comparison 2003 vs. 2013 | |||
| Z score | p value | Z score | p value | |||||
| E. coli | ||||||||
| Total | 44 | 29 | 3.466 | .00058 | 47 | 35 | 2.4535 | .01428 |
| Outpatient | 53 | 41 | 1.0466 | .29372 | 56 | 41 | 1.2927 | .19706 |
| Inpatient | 40 | 24 | 1.7747 | .07672 | 40 | 32 | 0.8882 | .37346 |
| CCU | 41 | 21 | 2.0918 | .03662 | 46 | 34 | 1.1173 | .26272 |
| K. pneumoniae | ||||||||
| Total | 50 | 27 | 3.2198 | .00128 | 62 | 30 | 4.7265 | 0 |
| Outpatient | 57 | 25 | 2.1543 | .03156 | 57 | 33 | 1.543 | .12356 |
| Inpatient | 55 | 36 | 1.5663 | .11642 | 68 | 37 | 2.5915 | .0096 |
| CCU | 39 | 19 | 2.2114 | .0217 | 61 | 23 | 3.8936 | .0001 |
| P. aeruginosa | ||||||||
| Total | 51 | 57 | -1.0625 | .28914 | 57 | 55 | 0.6747 | .50286 |
| Outpatient | 60 | 50 | 0.3519 | .72634 | 80 | 38 | 1.4954 | .13362 |
| Inpatient | 46 | 67 | -1.2635 | .20766 | 46 | 67 | -1.2635 | .20766 |
| CCU | 47 | 55 | -0.5354 | .5892 | 80 | 59 | 1.4181 | .1556 |
| Cefoperazone-sulbactam | Piperacillin-tazobactam | |||||||
| 2003 % | 2013 % | Resistance comparison 2003 vs. 2013 | 2003 % | 2013 % | Resistance comparison 2003 vs. 2013 | |||
| Z score | p value | Z score | p value | |||||
| E. coli | ||||||||
| Total | 87 | 76 | 2.253 | .02444 | 78 | 65 | 2.5117 | .01174 |
| Outpatient | 85 | 81 | 0.4732 | .63836 | 88 | 68 | 2.8022 | .03752 |
| Inpatient | 93 | 77 | 1.9972 | .0455 | 83 | 68 | 1.9536 | .5118 |
| CCU | 84 | 71 | 1.4529 | 1.14706 | 65 | 60 | 0.4428 | .65994 |
| K. pneumoniae | ||||||||
| Total | 78 | 41 | 4.9607 | 0 | 77 | 38 | 5.9395 | 0 |
| Outpatient | 79 | 42 | 2.3453 | .01878 | 79 | 39 | 2.5198 | .01174 |
| Inpatient | 77 | 46 | 2.6293 | .00854 | 82 | 47 | 2.9157 | .0035 |
| CCU | 77 | 34 | 3.5991 | .00032 | 71 | 29 | 4.784 | 0 |
| P. aeruginosa | ||||||||
| Total | 82 | 52 | 2.2574 | .02382 | 85 | 77 | 0.9561 | .33706 |
| Outpatient | 98 | 50 | 1.0817 | .28014 | 100 | 88 | 0.8229 | .41222 |
| Inpatient | 69 | 53 | 0.9705 | .33204 | 69 | 73 | 0.2755 | .77948 |
| CCU | 80 | 52 | 1.8259 | .06724 | 87 | 69 | 1.2853 | .19706 |
| Amikacin | Ciprofloxacin | Meropenem | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2003 % | 2013 % | Resistance comparison 2003 vs. 2013 | 2003 % | 2013 % | Resistance comparison 2003 vs. 2013 | 2003 % | 2013 % | Resistance comparison 2003 vs. 2013 | ||||
| Z score | p value | Z score | p value | Z score | p value | |||||||
| E. coli | ||||||||||||
| Total | 90 | 89 | 0.147 | .88076 | 31 | 31 | 0.8808 | .37886 | 100 | 95 | 1.1698 | .242 |
| Outpatient | 88 | 89 | -0.127 | .89656 | 32 | 57 | -2.0645 | .0394 | 100 | 100 | 1.0596 | .29372 |
| Inpatient | 87 | 90 | -0.481 | .63122 | 30 | 21 | 0.1237 | .26272 | 100 | 96 | 0.2368 | .81034 |
| CCU | 95 | 90 | 0.8454 | .39532 | 32 | 26 | 0.6924 | .4902 | 100 | 91 | 1.8349 | .06724 |
| K. pneumoniae | ||||||||||||
| Total | 88 | 53 | 4.9262 | 0 | 46 | 32 | 1.9986 | .0455 | 99 | 54 | 5.5334 | 0 |
| Outpatient | 79 | 58 | 1.3386 | .18024 | 43 | 31 | 0.8245 | .41222 | 100 | 60 | 2.3496 | .01878 |
| Inpatient | 77 | 57 | 0.7648 | .0784 | 55 | 39 | 1.3516 | .17702 | 99 | 59 | 1.6498 | .09894 |
| CCU | 94 | 44 | 4.567 | 0 | 39 | 26 | 1.4054 | .15854 | 99 | 43 | 5.274 | 0 |
| P. aeruginosa | ||||||||||||
| Total | 74 | 66 | 0.9967 | .31732 | 59 | 47 | 0.4977 | .61708 | 100 | 65 | 3.4913 | .00048 |
| Outpatient | 80 | 75 | 0.2082 | .83366 | 80 | 38 | 1.4954 | .13362 | 100 | 75 | 1.2154 | .22246 |
| Inpatient | 54 | 57 | -0.171 | .86502 | 38 | 47 | 0.4976 | .61708 | 100 | 50 | 1.1662 | .242 |
| CCU | 87 | 66 | 1.4932 | .31732 | 60 | 55 | 0.3064 | .75656 | 100 | 48 | 3.431 | .0006 |
| Amikacin | Ceftazidime | Cefoperazone- sulbactam | Piperacillin- tazobactam | Meropenem | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OP | IP | CCU | OP | IP | CCU | OP | IP | CCU | OP | IP | CCU | OP | IP | CCU | |
| 2003 | 85 | 77 | 93 | 55 | 46 | 41 | 83 | 83 | 78 | 87 | 80 | 73 | 99 | 98 | 99 |
| 2004 | 85 | 64 | 84 | 54 | 35 | 36 | 81 | 69 | 77 | 81 | 73 | 65 | 96 | 95 | 98 |
| 2005 | 88 | 81 | 78 | 72 | 59 | 47 | 91 | 87 | 82 | 91 | 85 | 83 | 98 | 97 | 95 |
| 2006 | 67 | 71 | 65 | 41 | 34 | 29 | 91 | 77 | 70 | 81 | 66 | 72 | 95 | 98 | 97 |
| 2007 | 62 | 52 | 64 | 47 | 39 | 38 | 77 | 80 | 69 | 61 | 58 | 62 | 100 | 96 | 95 |
| 2008 | 79 | 63 | 65 | 56 | 46 | 37 | 82 | 81 | 67 | 71 | 65 | 61 | 98 | 97 | 94 |
| 2009 | 67 | 66 | 56 | 49 | 44 | 31 | 84 | 81 | 52 | 69 | 60 | 44 | 94 | 95 | 71 |
| 2010 | 61 | 63 | 52 | 34 | 31 | 39 | 82 | 72 | 56 | 49 | 48 | 50 | 99 | 94 | 66 |
| 2011 | 72 | 60 | 47 | 37 | 29 | 32 | 72 | 67 | 48 | 61 | 60 | 42 | 92 | 86 | 57 |
| 2012 | 81 | 74 | 60 | 38 | 26 | 38 | 70 | 65 | 52 | 67 | 53 | 48 | 92 | 84 | 58 |
| 2013 | 74 | 76 | 52 | 35 | 32 | 25 | 60 | 65 | 43 | 57 | 61 | 40 | 79 | 83 | 50 |
| Total | E. coli | Klebsiella | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2011 | 2012 | 2013 | 2011 | 2012 | 2013 | |
| OUTPATIENT | |||||||||
| Polymyxin E | 97 | 93 | 99 | 98 | 98 | 100 | 100 | 96 | 100 |
| Tigecycline | 89 | 87 | 89 | 98 | 100 | 100 | 96 | 98 | 97 |
| INPATIENT | |||||||||
| Polymyxin E | 98 | 100 | 100 | 100 | 100 | 100 | 88 | 100 | 100 |
| Tigecycline | 90 | 84 | 87 | 100 | 100 | 99 | 89 | 100 | 94 |
| CCU | |||||||||
| Polymyxin E | 91 | 90 | 99 | 100 | 95 | 100 | 100 | 100 | 100 |
| Tigecycline | 77 | 79 | 73 | 100 | 95 | 98 | 100 | 89 | 76 |
| Pseudomonas | Acinetobacter | ||||||||
| 2011 | 2012 | 2013 | 2011 | 2012 | 2013 | ||||
| OUTPATIENT | |||||||||
| Polymyxin E | 94 | 96 | 97 | ||||||
| Tigecycline | |||||||||
| INPATIENT | |||||||||
| Polymyxin E | 96 | 100 | 99 | ||||||
| Tigecycline | |||||||||
| CCU | |||||||||
| Polymyxin E | 98 | 87 | 97 | 100 | 98 | 95 | |||
| Tigecycline | 100 | 98 | 80 | ||||||
| 2011 % | 2013 % | Comparison of resistance 2011 vs. 2013 | ||
|---|---|---|---|---|
| Z score | p value | |||
| OUTPATIENT | ||||
| Polymyxin E | 97 | 98 | -0.7752 | .4354 |
| Tigecycline | 89 | 88 | 0.1196 | .90448 |
| INPATIENT | ||||
| Polymyxin E | 97 | 99 | -1.866 | .06148 |
| Tigecycline | 89 | 86 | 0.9364 | .34722 |
| CCU | ||||
| Polymyxin E | 91 | 98 | -3.8051 | .00014 |
| Tigecycline | 77 | 73 | 0.9889 | .32218 |
| TOTAL BLOOD ISOLATES | ||||
| Polymyxin E | 95 | 99 | -4.1913 | 0 |
| Tigecycline | 83 | 81 | 1.0556 | .28914 |
Discussion
Conclusion
Author Contributions
Conflicts of Interest
References
- Biedenbach, D.J.; Moet, G.J.; Jones, R.N. Occurrence and antimicrobial resistance pattern comparisons among bloodstream infection isolates from the SENTRY Antimicrobial Surveillance Program (1997-2002). Diagn Microbiol Infect Dis 2004, 50, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Marra, A.R.; Camargo, L.F.; Pignatari, A.C.; et al. Nosocomial bloodstream infections in Brazilian hospitals: Analysis of 2,563 cases from a prospective nationwide surveillance study. J Clin Microbiol 2011, 49, 1866–1871. [Google Scholar] [PubMed]
- Lee, N.Y.; Lee, H.C.; Ko, N.Y.; et al. Clinical and economic impact of multidrug resistance in nosocomial Acinetobacter baumannii bacteremia. Infect Control Hosp Epidemiol 2007, 28, 713–719. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Sharma, S.; Arora, A.; Gupta, A. Changing trends of in vitro antimicrobial resistance patterns in blood isolates in a tertiary care hospital over a period of 4 years. Indian J Med Sci 2010, 64, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Chadhary, M.; Kumar, S.; Payasi, A. Prevalence and antimicrobial sensitivity of ESBL producing Gram- negative bacteria from clinical settings in India from 2010 to 2012. Int J Med Med Sci 2013, 46, 1212–1217. [Google Scholar]
- Jain, S.; Khety, Z. Changing antimicrobial resistance pattern of isolates from an ICU over a 2 year period. J Assoc Physicians India 2012, 60, 27–28,33. [Google Scholar] [PubMed]
- Kumhar, G.D.; Ramachandran, V.G.; Gupta, P. Bacteriological analysis of blood culture isolates from neonates in a tertiary care hospital in India. J Health Popul Nutr 2002, 20, 343–347. [Google Scholar]
- Kaul, S.; Brahmadathan, K.N.; Jagannati, M.; et al. One year trends in the gram-negative bacterial antibiotic susceptibility patterns in a medical intensive care unit in South India. Indian J Med Microbiol 2007, 25, 230–235. [Google Scholar] [CrossRef] [PubMed]
- Rajeevan, S.; Ahmad, S.M.; Jasmin, P.T. Study of prevalence and antimicrobial susceptibility pattern in blood isolates from a tertiary care hospital in North Kerala, India. Int J Curr Microbiol App Sci 2014, 3, 655–662. [Google Scholar]
- Chhina, D.; Gupta, V. Bacteriological profile and antimicrobial susceptibility pattern of blood isolates from a tertiary care hospital in North India. Int J Pharm Res Biosci 2013, 2, 24–35. [Google Scholar]
- Vanitha Rani, N.; Kannan, G.; Venkata Narendra, M.; et al. A retrospective study on blood stream infections and antibiotic susceptibility patterns in a tertiary care teaching hospital. Int J Pharm Pharm Sci 2012, 4, 543–548. [Google Scholar]
- Gopalakrishnan, R.; Sureshkumar, D. Changing trends in antimicrobial susceptibility and hospital acquired infections over an 8 year period in a tertiary care hospital in relation to introduction of an infection control programme. J Assoc Physicians India 2010, 58 Suppl, 25–31. [Google Scholar] [PubMed]
- Clinical and Laboratory Standards Institute. Performance Standards For Antimicrobial Susceptibility Testing; Thirteenth to Twenty Third Informational Supplements; CLSI document M100-18; Clinical and Laboratory Standards Institute: Wayne, PA, 2003-2013. [Google Scholar]
- Nair, P.K.; Vaz, M.D. Prevalence of carbapenem resistant Enterobacteriaceae from a tertiary care hospital in Mumbai, India. J Microbiol Infect Dis 2013, 3, 207–210. [Google Scholar] [CrossRef]
- Gupta, N.; Limbago, B.M.; Patel, J.B.; Kallen, A.J. Carbapenem-resistant Enterobacteriaceae: Epidemiology and prevention. Clin Infec Dis 2011, 53, 60–67. [Google Scholar] [CrossRef]
- Mohamudha Parveen, R.; Harish, B.N.; Parija, S.C. Emerging carbapenem resistance among nosocomial isolates of Klebsiella pneumoniae in South India. Int J Pharma Biosci 2010, 1, 1–11. [Google Scholar]
- Kumarasamy, K.K.; Toleman, M.A.; Walsh, T.R.; et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: A molecular, biological, and epidemiological study. Lancet Infect Dis 2010, 10, 597–602. [Google Scholar] [CrossRef]
- Gupta, E.; Mohanty, S.; Sood, S.; Dhawan, B.; Das, B.K.; Kapil, A. Emerging resistance to carbapenems in a tertiary care hospital in north India. Indian J Med Res 2006, 124, 95–98. [Google Scholar] [PubMed]
- Sinha, N.; Agarwal, J.; Srivastava, S.; Singh, M. Analysis of carbapenem-resistant Acinetobacter from a tertiary care setting in North India. Indian J Med Microbiol 2013, 31, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Chennai Declaration Team. "Chennai Declaration": 5-year plan to tackle the challenge of anti-microbial resistance. Indian J Med Microbiol 2014, 32, 221–228.


| Outpatient | Inpatient | CCU | Total | |
|---|---|---|---|---|
| All isolates | 1111 | 1365 | 1652 | 4128 |
| E. coli | 687 | 774 | 457 | 1918 |
| K. pneumoniae | 286 | 396 | 568 | 1250 |
| P. aeruginosa | 138 | 195 | 295 | 628 |
| A. baumannii | - | - | 332 | 332 |
2003 % | 2013 % | Resistance comparison 2003 vs. 2013 | ||
|---|---|---|---|---|
| OUTPATIENT | Z score | p value | ||
| Amikacin | 85 | 74 | 1.4888 | .13622 |
| Ceftazidime | 55 | 35 | 2.3068 | .02088 |
| Cefepime | 58 | 37 | 2.4384 | .01468 |
| Ciprofloxacin | 40 | 43 | -0.4112 | .6818 |
| Cefoperazone- sulbactam | 83 | 60 | 2.7667 | .0056 |
| Piperacillin- tazobactam | 87 | 57 | 3.6607 | .00026 |
| Meropenem | 96 | 79 | 2.7931 | .00528 |
| INPATIENT | ||||
| Amikacin | 77 | 76 | 0.128 | .89656 |
| Ceftazidime | 46 | 32 | 2.0772 | .03752 |
| Cefepime | 51 | 37 | 2.014 | .0444 |
| Ciprofloxacin | 40 | 29 | 1.7445 | .08186 |
| Cefoperazone- sulbactam | 83 | 65 | 2.7752 | .00544 |
| Piperacillin- tazobactam | 80 | 61 | 2.2309 | .00338 |
| Meropenem | 88 | 83 | 0.9845 | .32708 |
| CCU | ||||
| Amikacin | 93 | 52 | 6.6121 | 0 |
| Ceftazidime | 41 | 25 | 2.838 | .00452 |
| Cefepime | 58 | 31 | 4.4315 | 0 |
| Ciprofloxacin | 40 | 29 | 1.8114 | .0703 |
| Cefoperazone- sulbactam | 78 | 43 | 5.5771 | 0 |
| Piperacillin- tazobactam | 73 | 40 | 5.3191 | 0 |
| Meropenem | 99 | 50 | 7.9709 | 0 |
| TOTAL | ||||
| Amikacin | 86 | 66 | 5.2925 | 0 |
| Ceftazidime | 46 | 30 | 4.3462 | 0 |
| Cefepime | 56 | 34 | 5.335 | 0 |
| Ciprofloxacin | 40 | 31 | 2.3333 | .0198 |
| Cefoperazone- sulbactam | 81 | 56 | 6.4772 | 0 |
| Piperacillin- tazobactam | 79 | 52 | 6.8697 | 0 |
| Meropenem | 95 | 69 | 7.3563 | 0 |
© GERMS 2015.
Share and Cite
Alagesan, M.; Gopalakrishnan, R.; Panchatcharam, S.N.; Dorairajan, S.; Ananth, T.M.; Venkatasubramanian, R. A Decade of Change in Susceptibility Patterns of Gram-Negative Blood Culture Isolates: A Single Center Study. GERMS 2015, 5, 65-77. https://doi.org/10.11599/germs.2015.1073
Alagesan M, Gopalakrishnan R, Panchatcharam SN, Dorairajan S, Ananth TM, Venkatasubramanian R. A Decade of Change in Susceptibility Patterns of Gram-Negative Blood Culture Isolates: A Single Center Study. GERMS. 2015; 5(3):65-77. https://doi.org/10.11599/germs.2015.1073
Chicago/Turabian StyleAlagesan, Murali, Ram Gopalakrishnan, Senthur Nambi Panchatcharam, Sureshkumar Dorairajan, Thirunarayan Mandayam Ananth, and Ramasubramanian Venkatasubramanian. 2015. "A Decade of Change in Susceptibility Patterns of Gram-Negative Blood Culture Isolates: A Single Center Study" GERMS 5, no. 3: 65-77. https://doi.org/10.11599/germs.2015.1073
APA StyleAlagesan, M., Gopalakrishnan, R., Panchatcharam, S. N., Dorairajan, S., Ananth, T. M., & Venkatasubramanian, R. (2015). A Decade of Change in Susceptibility Patterns of Gram-Negative Blood Culture Isolates: A Single Center Study. GERMS, 5(3), 65-77. https://doi.org/10.11599/germs.2015.1073




