Seroprevalence of Rubella Virus IgG in Pregnant Women in Harare, Zimbabwe
Socio-Demographic Characteristics
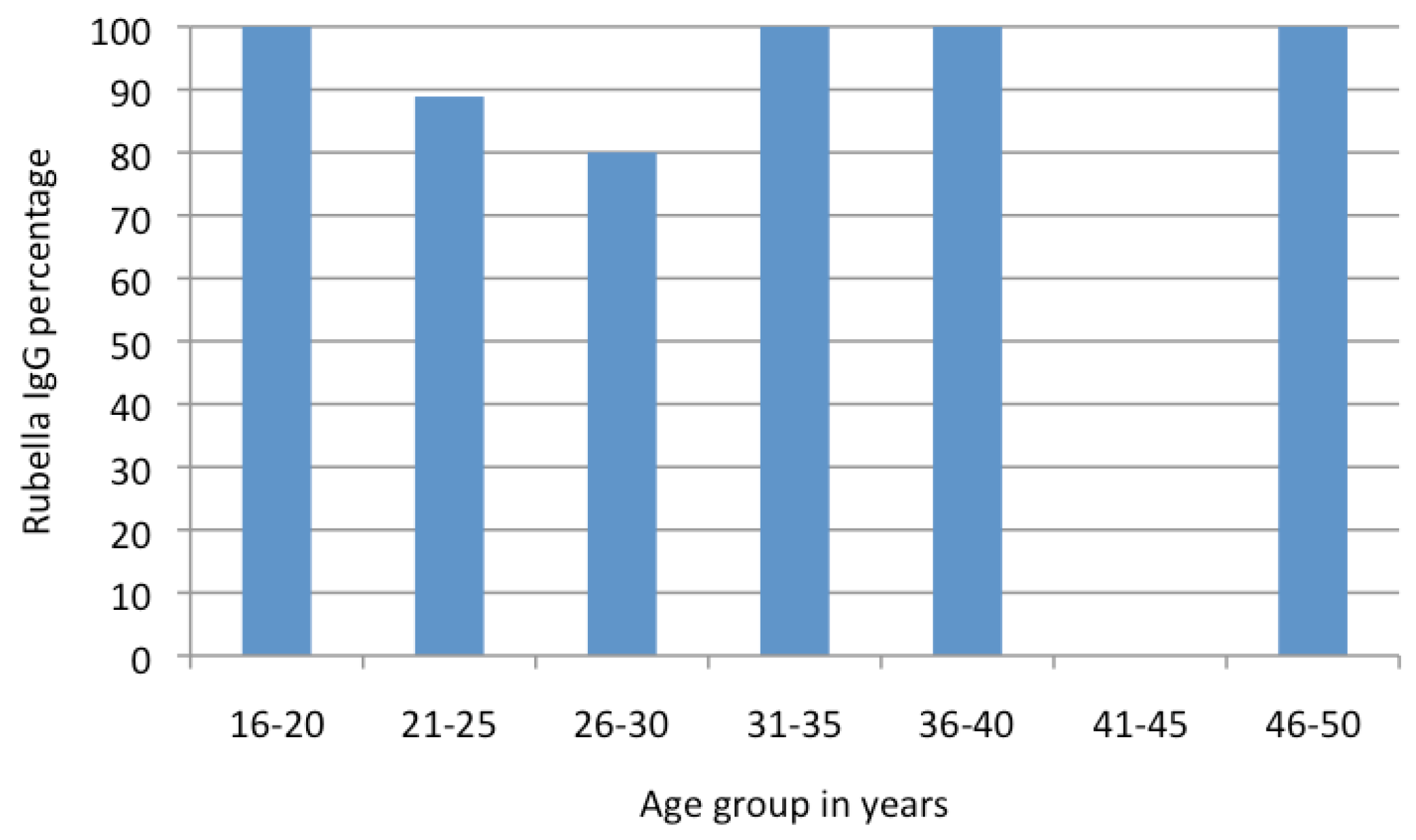
Rubella IgG Seroprevalence
Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Frey, T.K. Molecular biology of rubella virus. Adv. Virus Res. 1994, 44, 69–160. [Google Scholar] [PubMed]
- Centers for Disease Control and Prevention (CDC). Progress toward control of rubella and prevention of congenital rubella syndrome—Worldwide, 2009. MMWR Morb. Mortal. Wkly. Rep. 2010, 59, 1307–1310. [Google Scholar]
- Morice, A.; Ulloa-Gutierrez, R.; Avila-Agüero, M.L. Congenital rubella syndrome: Progress and future challenges. Expert Rev. Vaccines 2009, 8, 323–331. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Preventing congenital rubella syndrome. Wkly. Epidemiol. Rec. 2000, 75, 290–295. [Google Scholar]
- Tahita, M.C.; Hübschen, J.M.; Tarnagda, Z.; et al. Rubella seroprevalence among pregnant women in Burkina Faso. BMC Infect. Dis. 2013, 13, 164. [Google Scholar] [CrossRef] [PubMed]
- Hamdan, H.Z.; Abdelbagi, I.E.; Nasser, N.M.; Adam, I. Seroprevalence of cytomegalovirus and rubella among pregnant women in western Sudan. Virol. J. 2011, 8, 217. [Google Scholar] [CrossRef] [PubMed]
- Mwambe, B.; Mirambo, M.M.; Mshana, S.E.; et al. Sero-positivity rate of rubella and associated factors among pregnant women attending antenatal care in Mwanza, Tanzania. BMC Pregnancy Childbirth 2014, 14, 95. [Google Scholar] [CrossRef] [PubMed]
- Barreto, J.; Sacramento, I.; Robertson, S.E.; et al. Antenatal rubella serosurvey in Maputo, Mozambique. Trop. Med. Int. Health 2006, 11, 559–564. [Google Scholar] [CrossRef] [PubMed]
- Bamgboye, A.E.; Afolabi, K.A.; Esumeh, F.I.; Enweani, I.B. Prevalence of rubella antibody in pregnant women in Ibadan, Nigeria. West. Afr. J. Med. 2004, 23, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Onyenekwe, C.C.; Kehinde-Agbeyangi, T.A.; Ofor, U.S.; Arinola, O.G. Prevalence of rubella-IgG antibody in women of childbearing age in Lagos, Nigeria. West. Afr. J. Med. 2000, 19, 23–26. [Google Scholar] [PubMed]
- Best, J.M. Rubella. Semin. Fetal Neonatal Med. 2007, 12, 182–192. [Google Scholar] [CrossRef] [PubMed]
- Muller, C.P.; Kremer, J.R.; Best, J.M.; et al. Reducing global disease burden of measles and rubella: Report of the WHO Steering Committee on research related to measles and rubella vaccines and vaccination, 2005. Vaccine 2007, 25, 1–9. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Robinson, J.L.; Lee, B.E.; Preiksaitis, J.K.; Plitt, S.; Tipples, G.A. Prevention of congenital rubella syndrome—What makes sense in 2006? Epidemiol. Rev. 2006, 28, 81–87. [Google Scholar] [CrossRef] [PubMed]
| Rubella IgG Status | Frequency | Mean Age (Standard Deviation) | 95% Confidence Interval |
|---|---|---|---|
| Negative | 4 | 27.8 (2.6) | 23.6–31.9 |
| Positive | 47 | 31.2 (7.0) | 29.2–33.3 |
| Combined | 51 | 30.9 (6.8) | 29.0–32.9 |
© GERMS 2015.
Share and Cite
Mamvura, T.S.; Chin'Ombe, N.; Ruhanya, V.; Nziramasanga, P. Seroprevalence of Rubella Virus IgG in Pregnant Women in Harare, Zimbabwe. Germs 2015, 5, 50-52. https://doi.org/10.11599/germs.2015.1071
Mamvura TS, Chin'Ombe N, Ruhanya V, Nziramasanga P. Seroprevalence of Rubella Virus IgG in Pregnant Women in Harare, Zimbabwe. Germs. 2015; 5(2):50-52. https://doi.org/10.11599/germs.2015.1071
Chicago/Turabian StyleMamvura, Tafadzwa Shepherd, Nyasha Chin'Ombe, Vurayai Ruhanya, and Pasipanodya Nziramasanga. 2015. "Seroprevalence of Rubella Virus IgG in Pregnant Women in Harare, Zimbabwe" Germs 5, no. 2: 50-52. https://doi.org/10.11599/germs.2015.1071
APA StyleMamvura, T. S., Chin'Ombe, N., Ruhanya, V., & Nziramasanga, P. (2015). Seroprevalence of Rubella Virus IgG in Pregnant Women in Harare, Zimbabwe. Germs, 5(2), 50-52. https://doi.org/10.11599/germs.2015.1071




