Introduction
Pregnancy and childbirth have always been characterized by risks, the reduction and/or elimination of which can provide security for mother and fetus for a good subsequent development. One of the current risks is the use of illicit drugs, which, due to its serious medical and psychological aspects, in the short and long term, at the individual and social level, constitutes a widespread phenomenon throughout the world. Globally, it is estimated that 3.5-5% of the population aged 15-64 have used illicit drugs at least once and that 10-15% of these users are likely to become addicted.[
1,
2]
The steady rise in the incidence of illicit drug use (under-reported, especially self-reported)[
3,
4] has become a worrying reality in a competitive but socio-economically polarized world, but also in the context of legislative changes in certain regions/countries) by the phenomenon of legalizing the use of some previously banned hallucinogenic substances. Several in the United States and Canada have already authorized the production and sale of cannabis for non-medical use.[
5]
In Europe, 29% of the population is cited as having used drugs at least once,[
6] with the most common pattern of drug use reported in the survey being polysubstance use, the use of two or more psychoactive substances (licit or illicit), either simultaneously or sequentially.[
7] Women also account for a significant proportion of the population that uses drugs and of the population combining alcohol, tobacco and drugs.[
8]
In Romania, 13.3% of the people admitted to treatment for drug use, according to the 2023 national report of the National Anti-Drug Agency, were women, with the highest number of cases being generated by cannabis (44%) and opiates (23.1%).[
9]
Drug addiction in the female population, most of the time at childbearing age, but especially the effects of drug addiction in the case of pregnancy, are usually little known or ignored, pregnancy being often unplanned, unwanted, late detected, not medically supervised, in a poor socio-economic context, with lack of family support.[
5,
6,
10]
The use of illicit drugs during pregnancy involves maternal, fetal and neonatal risks,[
9,
11] the most common being: intrauterine fetal death, retroplacental hematoma, premature birth, impregnation syndrome (newborn asleep), newborn withdrawal syndrome (in a state of inborn dependence on the drug used by the mother during pregnancy), intrauterine growth restriction, blood- and/or sexually-transmitted infections, congenital malformations, as well as brain damage (microcephaly, cerebral infarction, intracranial hemorrhage).[
12] Recent, prospective, longitudinal studies have identified effects including neurodevelopmental effects that may persist into adulthood.[
4]
The aim of the research was to determine the incidence of newborns from mothers using drugs in Romania, to determine the effects of drugs on the fetus and newborn in order to reduce neonatal morbidity and mortality.
Methods
The study is retrospective and was conducted in the Institute for Mother and Child Health (INSMC) “Alessandrescu-Rusescu” in Bucharest, a higher-level maternity hospital that also cares for high-risk newborns. All newborns from the period 2002-2024 born to mothers who used illicit drugs before and/or during pregnancy were included in the study and four cases (two of which resulted in neonatal death) out of a total of 102 were excluded due to lack of complete data. Ninety-eight mother-newborn couples were analyzed.
We used data obtained by maternal anamnesis (illicit drug use assessed according to the National Antidrug Agency[
9] lifetime use, recent/in the last year, current/in the last month), age, residence, educational level, parity, viral infections, etc.), clinical and paraclinical examination, including toxicological examination performed on the mother and the newborn.
The toxicological examination was indicated to mothers on the basis of anamnestic, biological (hard-to-approach veins, malnutrition, positive tests for human immunodeficiency virus or hepatitis C infections), behavioral and/or social (running from hospital after delivery and abandonment of the newborn, etc.) and also the presence of clinical signs of withdrawal in their newborns. Toxicological screening using urine samples collected in the first hours after birth from the mother and her newborn, in 61 cases (59.8%), was carried out by two methods: the qualitative method by rapid test (“Multi - Drug Screening Test”) and the Quantitative Gas Chromatography-Mass Spectrometry (GC/MS) method which is a more specific chemical method of confirmation. In the remaining 37 cases (37.8%) the illicit drug was specified only anamnestically (without toxicological examination) due to the impossibility of testing (mothers running away from hospital, home birth, severe asphyxia and neonatal death, lack of rapid tests and access to toxicological laboratory, etc.).
The clinical examination of the newborn included the measurement of anthropometric parameters at birth: weight, length, head circumference and ponderal index (PI) = W (g): Length (cm)
3x100, evaluated according to Lubchenco intrauterine growth curves.[
13] The Finnegan score[
14] was used to assess the presence and severity of neonatal withdrawal syndrome.
After the data obtained from the study protocols were entered into the database fields, they were processed using the SPSS version 23.0 and Excel software packages. For descriptive statistics, mean and standard deviation, medians and quartiles were calculated for quantitative variables and frequencies and percentages for qualitative variables. In comparing quantitative data, depending on the normality of the data, the independent samples T test (for two groups with normally distributed data), Mann-Whitney U (for groups with non-normally distributed data) were used. Quantitative data were tested for normality and homogeneity of variates using Levene's test. Pearson Chi-Square, Fisher's Exact Test (for 2 groups) and Likelihood ratio (for more than 2 groups) were used for categorical data (summarized as frequencies and percentages). When more than two groups were compared, if the overall significance test indicated significance, multiple comparison (post hoc) tests were applied to determine which groups were statistically significant. The probability of error of less than 5% (p <0.05) was considered the significance level.
Results
In the period 2002-2024 in the hospital a total of 73,779 live newborns were born and 0.14% (n=102) of them were born to mothers who used illicit drugs. The incidence of newborns born to mothers with drug addiction has increased almost steadily (from a low of 0.03% in 2006 to a high of 0.3% in 2018), doubling in the last 12 years from an average of 0.1% to an average of 0.2%.
Neonatal deaths were recorded in 7.1% (n=7) of the total of 98 cases studied, of which 42.9% at ages between zero and six days and 57.1% at over 7 days. Of 7 newborns, 2 died in the first part and 5 in the last part of the studied period. All these newborns were premature with gestational ages between 24 and 35 weeks (29 weeks and 2 days) and birth weights between 800 g and 2100 g (mean 1294 g). The majority 57.1% had severe asphyxia at birth expressed by Apgar score = 1, one case a complex cardiac malformation, and one case perinatal ulcerative-necrotic enterocolitis.
Mothers with drug addiction were in the majority (55%) using multiple drugs (poly-drug use), especially in the last 12 years (62.9%), compared to the first 10 years (38.9%) when only one drug (opioid) was frequently used.
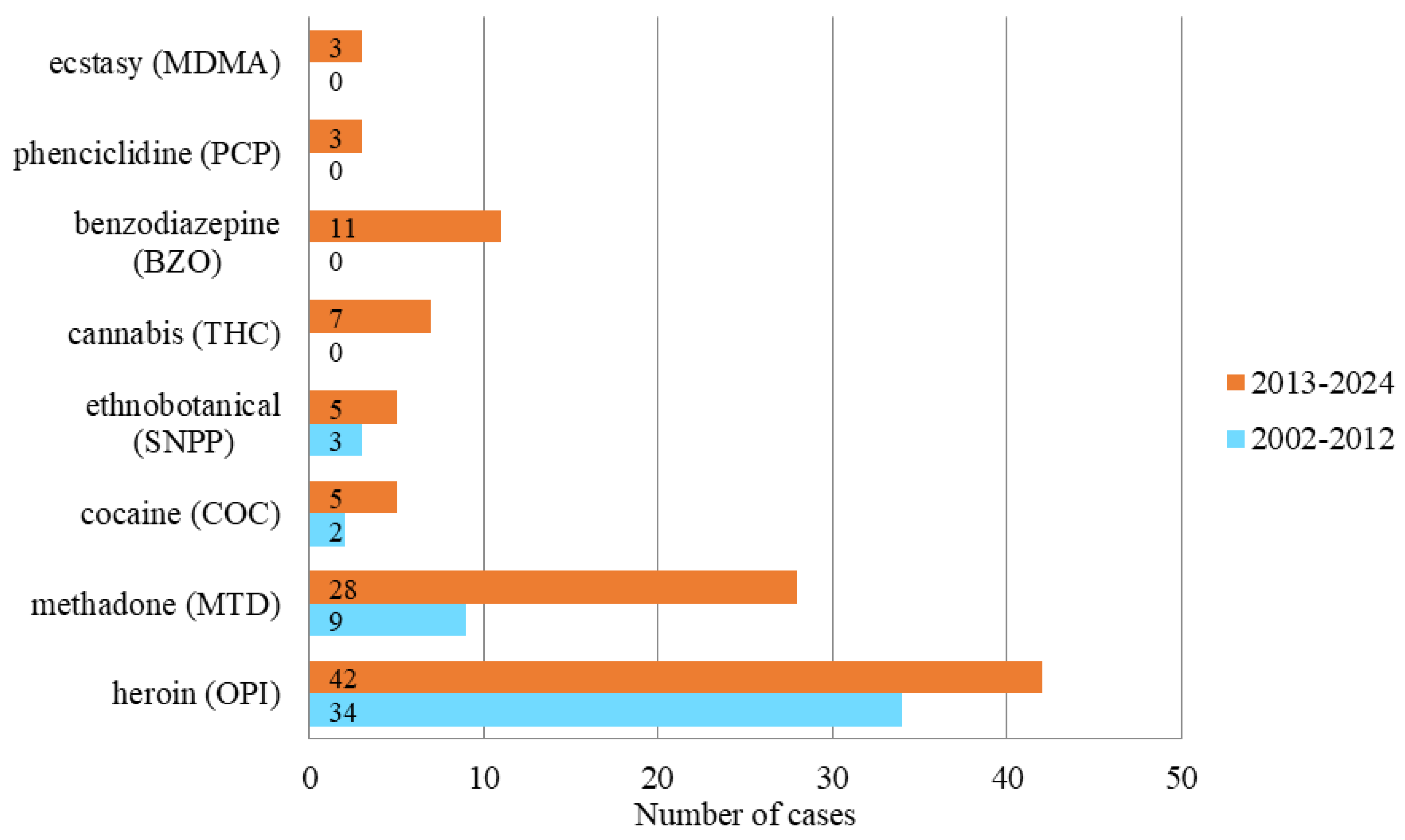
The exclusive use of a single type of drug was reported in 45% of cases, of which 33% were heroin use and smaller percentages of other illicit substances. In the last decade the use of methadone, heroin has increased and new substances have been used: cannabis, ecstasy, phencyclidine, ethnobotanicals/new psychosomatic substances (NPS), benzodiazepines (
Figure 1).
The principal characteristics of these mothers included: age below 18 years 13.3% (13 of 98), multiple gestation 75%, multiparity 56%, low level of education (67% had 0-8 years of school education) and maternal blood and/or sexually transmitted infections in 59.2% (58 cases).
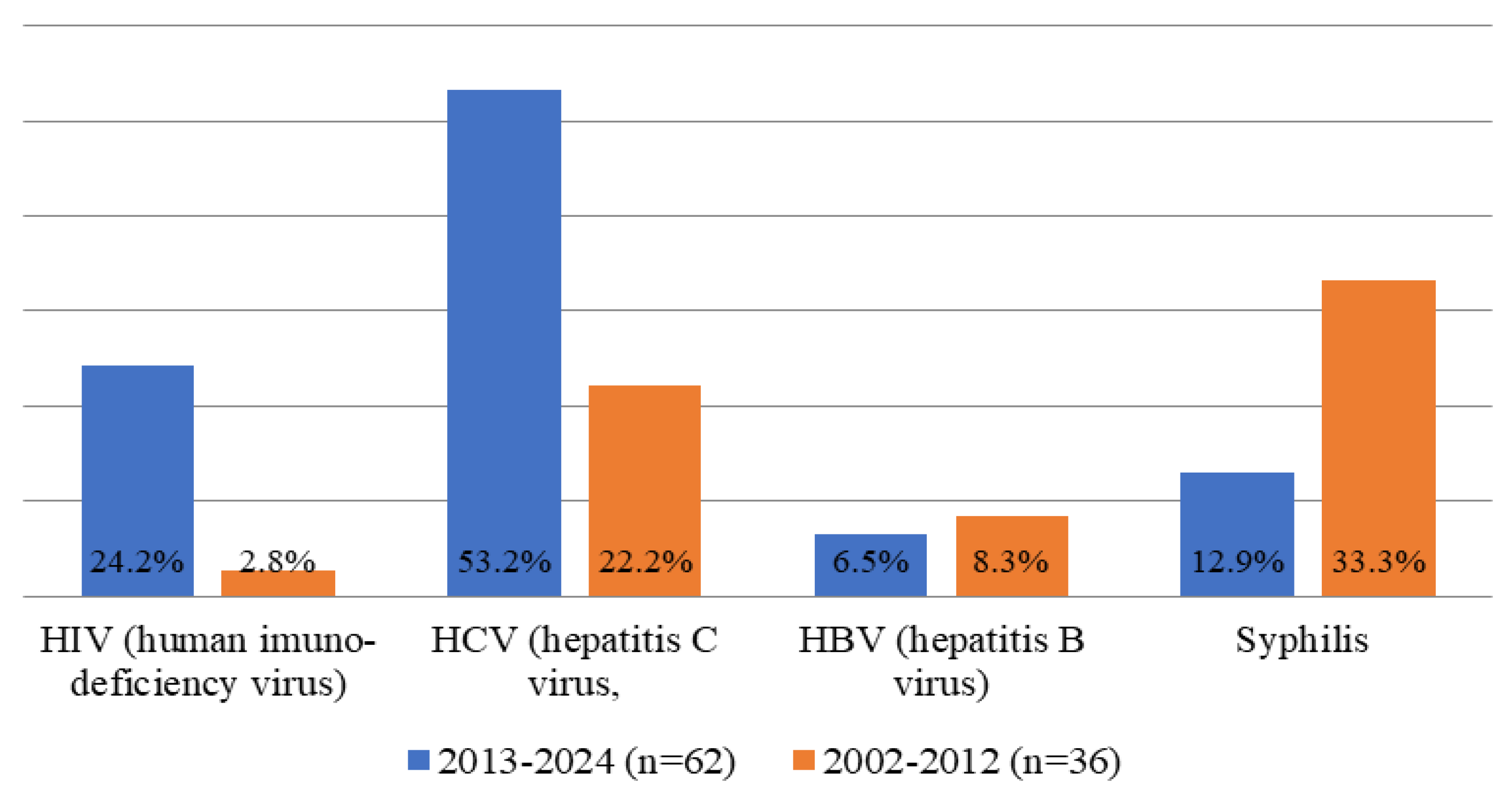
The most frequently identified were positive cases for hepatitis C virus (HCV) – 41.8%, syphilis – 20.4%, human immunodeficiency virus (HIV) – 16.3% and hepatitis B virus (HBV) – 7.1%.
The evolution of the incidence of blood-borne and/or sexually transmitted infections in drug-using mothers shows statistically significant increases between the first 10 and the last 12 years studied for hepatitis C and human immunodeficiency virus, and decrease for syphilis (
Figure 2,
Table 1).
The newborns of mothers with drug addiction, from single pregnancies and in one case from twin pregnancy, were 60.2% male and had gestational ages (GA) between 25 and 41 weeks with an average of 35 weeks and 2 days, and 39.8% of the females had gestation age between 31 and 42 weeks with an average of 37 weeks and 1 day.
Neonatal morbidity was dominated in order of incidence by: withdrawal syndrome (61.2%), risk of viral infections (HIV, HCV, HBV) and syphilis through maternal pathology (58.1%), low birth weight ≤2500 g (55.1%), prematurity (43.8%), bacterial infections (38.7%), birth asphyxia (30.6%), respiratory distress syndrome 16.3% (with respiratory support in 14.2% cases) intrauterine growth restriction with low weight for gestational age (11.2%) and ulcero-necrotic enterocolitis (10.2%).
Neonatal withdrawal syndrome (neonatal abstinence syndrome/NAS) presented an incidence of 61.2% (60 cases) of which 15% evolved with major neurological syndrome (seizures). Prematurity had a total incidence of 43.8% (43 cases) and term births represented 56.1% (55 cases), with no statistically significant differences between the incidences of the two periods (36.1% 2002-2012 and 48.3% 2013-2024, respectively, p=0.237). The gestational age was statistically significantly different in favor of the female sex, p=0.018 (the mean gestational age being 37.2 weeks (range 31 to 42 weeks), compared to 35.3 weeks (range 25 to 41 weeks) for males).
Birth weight of babies born to mothers with drug addiction ranged between 800 g and 3850 g, with an average of 2417 g; it was 55.1% ≤2500 g (12.2% for those weighing <1500 g and 43.8% for those weighing between 1500 g and 2500 g) and 45% for those weighing >2500 g.
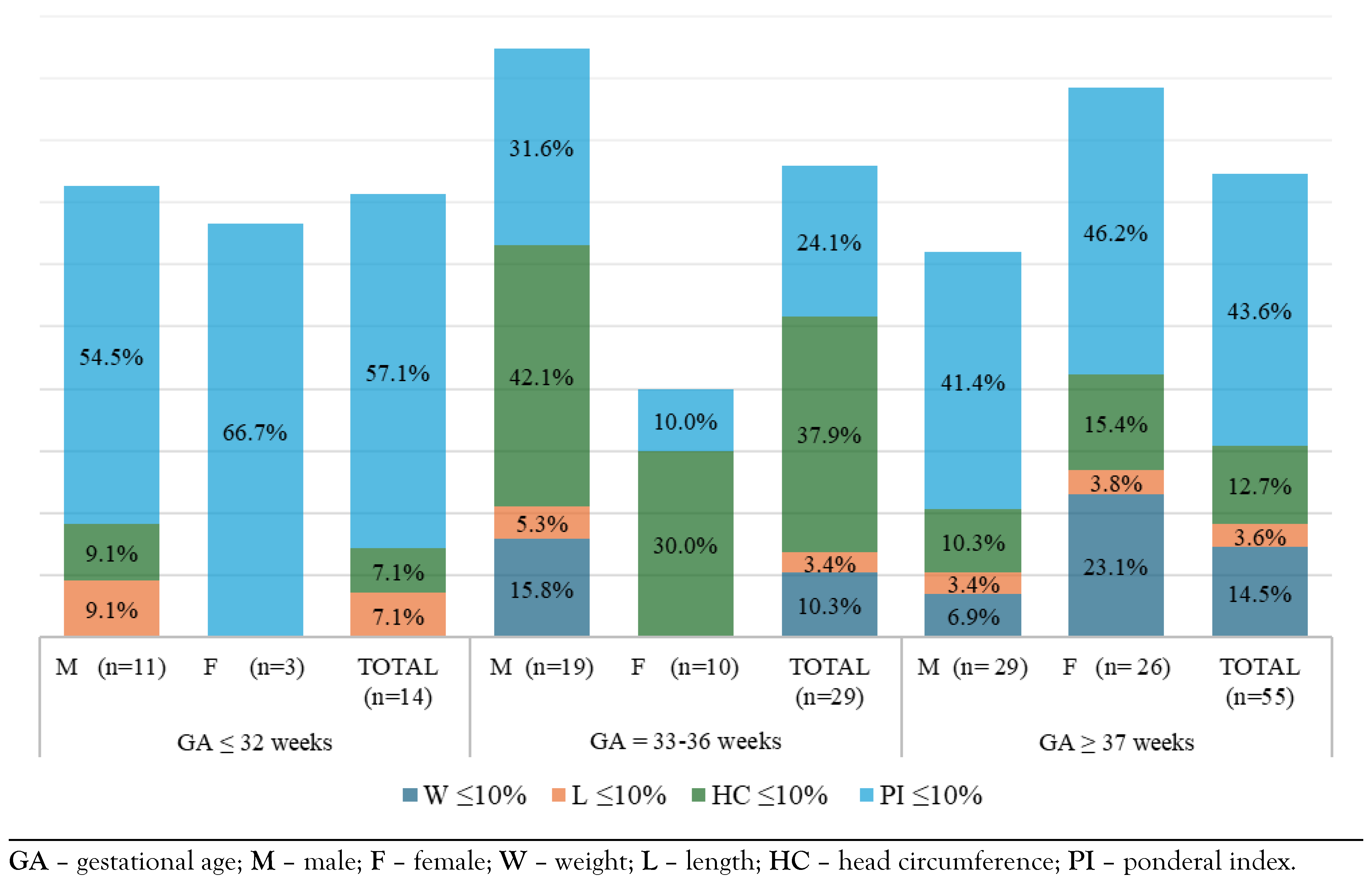
The reporting of growth parameters at gestational age according to intrauterine growth curves, identified cases situated on percentiles ≤10% indicating unsatisfactory growth, low for age. The most frequently affected early in fetal development was the ponderal index at less than 32 weeks of gestation and the head circumference at the age between 33 and 36 weeks of gestation (
Figure 3).
Regarding small head circumference for gestational age, there were statistically significant differences between incidences between 33 and 36 weeks of gestation (37.9%) compared to those with 37 weeks (12.7%), p=0.025,
Table 2.
Definite infection (neonatal bacterial) and the infectious risk conferred by maternal infections (acquired through the blood/sexual route) that can be transmitted to the fetus were present in the majority (75%) of babies born to mothers with drug addiction. The risk of congenital and/or perinatal infection, conferred by maternal pathology due to blood-borne and/or sexually transmitted diseases, required careful neonatal investigation for maternal coinfections, administration of hepatitis B vaccine and, depending on the case, hepatitis B human immunoglobulin, penicillin G for syphilis, antiretroviral medication from the first 4-6 hours of life of the newborn.
The 20 mothers with syphilis (20.4% of the total number of mothers who used drugs), were aged between 17 and 43 years with an average of 27.5 years, were multiparous in most cases (80%) and had associated infections (HIV, HCV, HBV, co-infections) in 60% of cases. They delivered prematurely in 35% of cases (seven babies) and on term in 65% of cases (13 babies). Their newborns had birth weight ≤2500 g in 60% cases (12 newborns) of which the term born with gestational age ≥37 weeks represented 25% of cases (five newborns). All the babies born to mothers with syphilis had positive tests: nontreponemal RPR (rapid plasma reagin), VDRL (venereal disease research laboratory) in 16 cases (80%) and only non-treponemal TPHA (treponema pallidum hemagglutination assay) in four cases (20%).
Neonatal infections (early and late) of bacterial cause (systemic and localized) were detected in 42.8% of cases (42 newborns), with similar incidences in the first 10 studied years 41.6% compared to the last 12 years 43.5% of the studied period. Out of all neonatal bacterial infections, 26 cases (61.9%) were present in infants born to mothers testing positive for HIV, HCV, HBV or syphilis.
Gram-negative bacteria (Escherichia coli, Enterobacter spp., Klebsiella pneumoniae) were the most frequently identified germs (89.2%) followed by group B Streptococcus, Staphylococcus aureus (10.7%).
Discussion
Illicit drug use has multiple and serious effects on the pregnant woman and her fetus/newborn child. Blood and/or sexually acquired infections by the mother, which are common with injecting drug use, are risk factors for congenital/perinatal infections.[
8] High perinatal infections incidence in these newborns can be explained by the high vulnerability to infectious aggression, favored by poor immunity in the context of prematurity, growth failure or perinatal asphyxia.
Mothers who use drugs have shown in the last decade compared to the previous period an increase in the incidence of HIV infection (24.2% vs 2.7% p=0.001), HCV infection (53.2% vs 22.2%; p=0.002), and a reduction in the incidence of syphilis (12.3% vs 33.3%, p=0.021). The preference for heroin use remains high, but the use of polydrugs has also increased (62.9% vs 38.8%; p=0.021). The use of polydrugs, involving various and multiple ways of access, can lead to a high risk of viral infections transmission.
Regarding the effects on the fetus and newborn, we observe a decrease in the incidence of withdrawal newborn syndrome in the last decade (80.5% vs. 50%, p=0.002). This can be explained by early prenatal diagnosis of drug use and medical and behavioral intervention or the increasing use of drugs with lower withdrawal effect intensity. Withdrawal syndrome in the newborn is a major symptom for the diagnosis of maternal drug use, and its absence can reduce the diagnosis rate. Therefore, it is necessary to have a good knowledge of the other effects on the fetus of maternal drug use that can increase the degree of suspicion and diagnosis. Thus, the impairment of fetal intrauterine development with the modification of anthropometric measurements (reduced head circumference, low ponderal index, reduced birth weight) unexplained by a maternal or fetal pathology should raise suspicion of drug use.
Other observations are that male newborns are born prematurely more frequently than female newborns (35 weeks vs 37 weeks; p=0.018). The cranial perimeter is below the 10th percentile in those born prematurely compared to those born at term (37.9% vs 12.7%; p=0.025). The impairment of brain growth is due to the impairment of both the placental-fetal circulation and the redistribution[
15,
16] of the fetal circulation as well as the direct effect of drugs in the fetal perfusion.
Early-onset intrauterine growth restriction at <32 weeks, symmetric/harmonious, with normal ponderal index (PI) (>10% percentile), is rarer (30% of cases) but more severe and is more common in chromosomopathies, infections, nutrient deficiency. It is associated with prematurity and increased risk of fetal death.[
17] Intrauterine growth restriction with late onset at >32 weeks (asymmetric /dysrhythmic) with ponderal index (PI) in the <10% percentile, is present in 70-80% of cases, frequently due to vascular causes (maternal hypertension), malnutrition, chronic hypoxia.[
15,
16]
The head circumference (HC) small for gestational age (located at the <10% percentile), in 20-30% of cases,[
15] impacts on later brain development. Post-mortem measurements of brain weight and head circumference show a cubic relationship between the two parameters from birth to 18 years of age,[
17] a relationship confirmed more recently by MRI imaging studies.[
16] The head circumference is a reliable marker of brain mass/volume evaluation and brain development, respectively, being associated with intelligence level and academic performance.[
15]
The long-term neurological outcome of the offspring of mothers with drug addiction depends on multiple factors, including genetic factors in interaction with the environment. Addiction through repeated maternal use of substances (alcohol, tobacco, drugs) can alter epigenetics, fortunately reversibly, leaving the possibility of therapeutic intervention. Genomewide studies in addiction pathologies have identified two types of genes: some involved in vulnerability to a psychotropic substance (alcohol, tobacco) and others involved in a more global process (alcohol, drugs) of reward and motivation (ANKK1 and DRD2 genes).[
18]
Non-invasive prenatal diagnosis using fetal DNA in maternal blood is likely to play an increasingly important role in future prenatal testing practice, although it does not replace the accuracy obtained with diagnostic tests such as chorionic villus sampling (CVS) or amniocentesis.[
19]
Interventions recommended in the research literature can help to reduce morbidity and mortality: opioid substitution treatment in pregnant women,[
20] screening and treatment of infections, identification of fetuses with intrauterine growth restriction or even arrest with high risk of intrauterine exitus and possibly saving them by early extraction/birth, even with the risks of prematurity,[
16,
17] medical surveillance of the evolution of pregnancy, prophylaxis of perinatal infections in the newborn, recovery of fetal brain growth and stimulation of neonatal neurodevelopment, through early feeding, and increased psycho-emotional attention during the period of rapid brain growth of newborns with low birth weight or with cranial perimeter damage, breastfeeding of the newborn only when indicated, and long-term monitoring of the newborn's evolution.