Introduction
Efforts to reduce the spread of COVID-19 led to the temporary closing of schools, colleges, and restrictions on freedom of movement. Prevention and protection measures such as disinfection, social distancing and wearing masks were the only way to slow down the infection. Citizens of the Republic of Serbia have the opportunity to be vaccinated with 4 types of vaccines from different manufacturers approved by the Agency for Medicines and Medical Devices of the Republic of Serbia.
Doctors who are engaged in working with students should have an important role in forming attitudes and imparting knowledge to medical students regarding the importance of vaccination, which unfortunately, according to research by Kernéis et al., is not the case, because around a third of final year medical students had insufficient knowledge about vaccination, side effects as well as problem-solving strategies to improve vaccination coverage [
1]. Vaccination against COVID-19 played a significant role in reducing pandemic spread. Medical students as future healthcare workers will be vaccination role models. They will provide vaccine recommendations and counsel patients and general population about vaccination [
2]. Also, they will be exposed to patients with COVID-19 [
2]. So, it is crucial to examine and shape attitudes toward COVID-19 vaccination in this population.
The aim of this study was to examine the attitudes and acceptance of COVID-19 vaccines among Serbian preclinical and clinical medical students.
Methods
In this cross-sectional study conducted during December 2022 and January 2023, 730 students of the Faculty of Medicine of the University of Belgrade participated. The response rate was 81.7%. Student responses were collected in classrooms before the start of compulsory practical sessions using an anonymous questionnaire. The questionnaire was designed on the grounds of extensive literature review and its internal consistency was calculated for reliability analysis. The questionnaire was piloted on 15 medical students in order to assess understanding of items. The questionnaire contained 12 questions related to the attitudes and behavior of medical students regarding vaccination against COVID-19. The questionnaire also contained questions related to vaccination status, reasons for/against vaccination, choice of vaccine, future vaccination plans, opinion for which population would be affected by COVID-19 vaccine was supposed to be mandatory, had they suffered from COVID-19 and how did they get information about COVID-19 vaccines. A student was classified as vaccinated if he or she received at least one dose of a COVID-19 vaccine. The study was approved by the Ethics Committee of the Faculty of Medicine University of Belgrade (decision number: 1322/IX-44; date of approval: September 29, 2022).
Pearson`s Chi-square, Fisher's exact test and t-test were used in the data analysis. A statistically significant difference was considered at the p<0.05 level. All data were analyzed using SPSS version 20.
Results
The average age was 21.37±1.17 years for third-year medical students, while the average age of sixth-year students was 24.37±1.03 years. There were 242 female students (72.9%) in the third year, and 260 (65.3%) in the sixth year. Sixth year students were significantly more frequently vaccinated (94.5% vs 87.3%, p=0.001). The largest number of students had received the Pfizer-BioNTech vaccine (
Table 1).
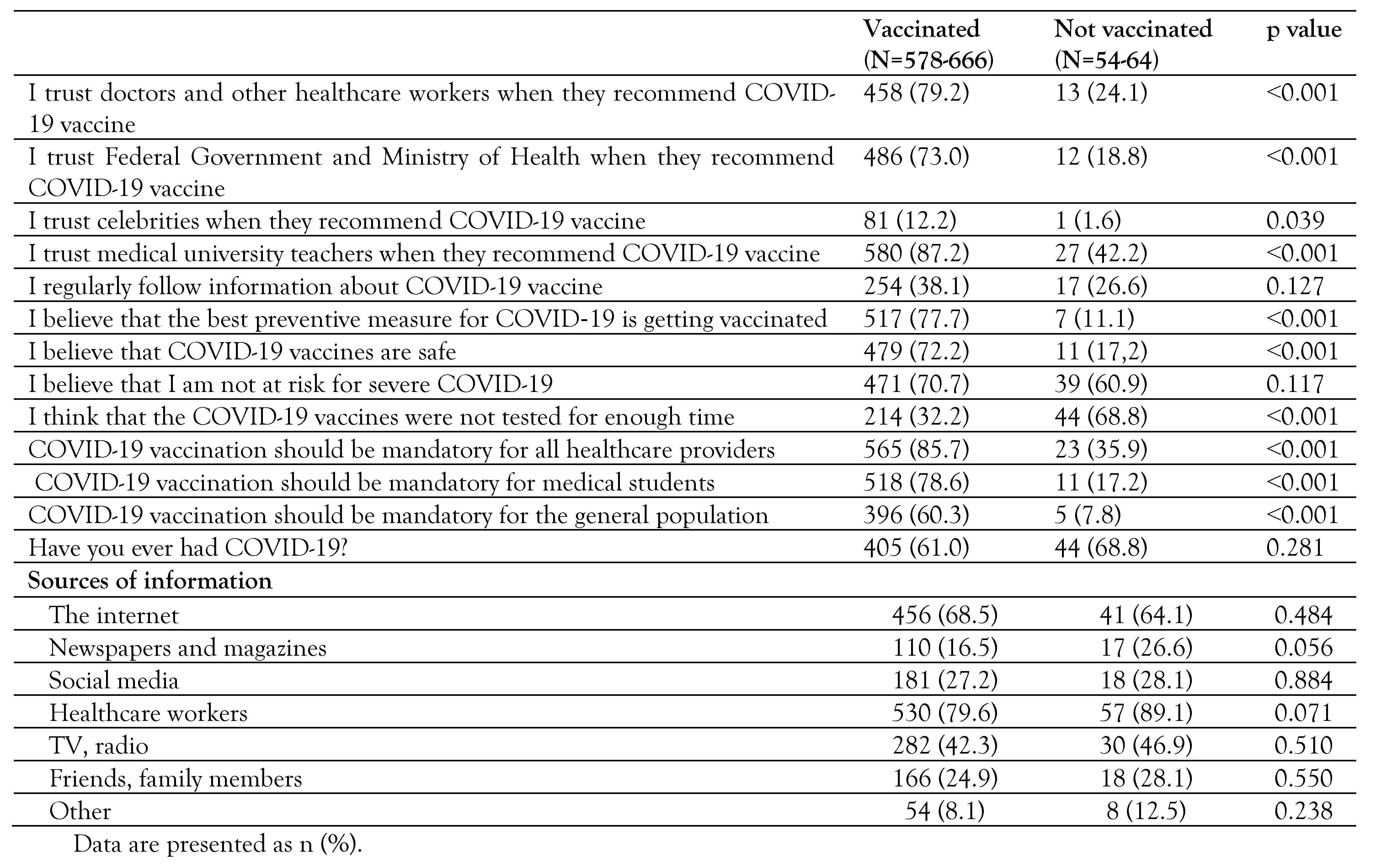
Compared to non-vaccinated students, vaccinated students trusted healthcare workers significantly more regarding the recommendation for COVID-19 vaccination (p˂0.001), the Ministry of Health (p˂0.001), and other health authorities (p=0.039), as well as teachers and associates at the Faculty of Medicine (p˂0.001). Vaccinated students were significantly more likely to believe that the best preventive measure for COVID-19 is vaccination (p˂0.001), that vaccines are safe (p˂0.001), while unvaccinated students believed that there had not been enough time to test the vaccine (p˂0.001). Vaccinated students were significantly more in favor of mandatory vaccination (p˂0.001) (
Table 2).
As the most common reasons for vaccination, students stated the desire to protect the people around them (73.8%) and the recommendation of a doctor or other medical staff.
Unvaccinated students stated the suspicion that the vaccines had not been tested enough (54.7%) and the fear of side effects of the vaccine (34.4%) as the most common reason for not receiving the vaccine.
Discussion
Vaccination coverage is higher among clinical medical students due to their level of knowledge and work with patients. Medical studies last six years at the Faculty of Medicine, of which the first three years are intended for basic subjects, while clinical subjects are attended from the fourth year of study.
In a situation where a vaccine is available, hesitancy or refusal to vaccinate is a serious problem in the fight against a pandemic. Medical students generally have a higher vaccination rate than the general population [
3]. Most medical students believed that vaccination is an important public health measure to protect their own health, the health of the patients they come into contact with, and the general community [
4].
Vaccinated students trusted healthcare workers, the Ministry of Health, and teachers and associates at the Faculty of Medicine significantly more when they recommend vaccination against COVID-19 compared to unvaccinated students. Reiter et al. suggest that doctors and medical workers are the most important factors that influence the acceptance of vaccination [
5].
Our data on students` attitudes and motivations for vaccination, and also for refusal, agree with results from other studies. The desire to protect other people was cited as the biggest motive for vaccination. According to a scoping review, the main factors for vaccine hesitancy were doubts about its safety and efficacy, being a pre-clinical medical student, and low perceived personal risk of COVID-19 [
4].
The study had certain limitations primarily due to its design. Another limitation is the period of the students' examination because the opinions and attitudes of the students changed depending on the waves of the pandemic, which led to fears, panic and concern for themselves and their loved ones. Also, we did not investigated factors influencing student hesitancy.
Conclusions
The obtained results show a high coverage of COVID-19 vaccination among students of the Faculty of Medicine in Belgrade and a high degree of trust in health authorities. Ongoing vaccine surveys will be needed to evaluate shifting attitudes around COVID-19 vaccination in this population.