Abstract
Introduction: Acute otitis and sinusitis are common complications in patients with influenza and are responsible for increased hospitalization rates. Methods: A five-year retrospective study (2018-2023) was conducted including all patients hospitalized for influenza (etiologic diagnosis by RT-PCR) to identify the incidence and characteristics of cases complicated with otitis and/or sinusitis. Cases associated with other viral co-infections were excluded from the analysis. Results: We identified a cumulative rate of 20.6% (324 cases) of acute otitis (AO) and acute sinusitis (AS) among patients with influenza. Of these, 62.3% had AO, 28.1% AS, and 9.6% concomitant AO and AS. Cases of AO were predominant in the pediatric population (97.0%), while cases of AS were more common in adults (56.1%). Influenza A viruses were identified in 67.2% of patients. The infection with influenza B viruses increased the risk of acute congestive otitis media 2.1-fold (p=0.020), and influenza A viruses increased the risk of acute maxillary sinusitis 2.7-fold (p=0.029). Late presentation to the hospital, with a median of 4 days from the onset of influenza symptoms, was identified as a factor in the occurrence of AO and AS. Conclusions: The risk of AO and AS is increased in patients with influenza, especially in the pediatric population and in late hospital presentations. These findings highlight the importance of proper monitoring and management of patients with influenza to prevent the development of complications, as well as the need to better understand the mechanisms whereby influenza viruses contribute to these secondary conditions.
Introduction
Despite being an infection that benefits from specific prophylaxis through vaccination and from specific antiviral treatment, influenza remains one of the most important acute viral infections occurring each year in humans. Many cases of influenza require hospitalization, mainly due to complications. Among these complications, acute otitis (AO) and acute sinusitis (AS) are prominent [1,2] and carry an important impact on the quality of life of patients while also simultaneously generating additional costs for health systems. For example, in a recent study of a pediatric cohort (under 14 years old) with influenza, otitis ranked first among complications, followed by pneumonia and sinusitis [3].
Inflammation induced by infection with influenza viruses is the main pathogenetic factor driving ear and sinus complications. Mucosal edema, increased secretions, and difficulty in drainage are further contributors. On the other hand, bacterial superinfections, especially with nasopharyngeal colonizers, can be responsible for AO and AS in patients with influenza. Streptococcus pneumoniae, Staphylococcus aureus and Haemophilus influenzaeare frequently incriminated as bacterial agents superinfecting influenza [4].
The burden of influenza as a result of its associated complications varies from region to region and from season to season and is related to the rate of circulation of influenza viruses, the rate of influenza vaccination, the characteristics of the affected population and the measures taken to limit virus transmission. In this context, through this five-year retrospective study, we aim to identify the incidence and describe the characteristics of patients with AO and AS who were hospitalized for influenza in one of the most important infectious disease hospitals in Romania. Our results may inform efforts to prevent and manage influenza complications.
Methods
We conducted a retrospective analysis of cases of influenza hospitalized with otic or sinus complications from January 2018 to December 2023. All cases included in the analysis were hospitalized in the National Institute of Infectious Diseases (NIID) “Prof. Dr. Matei Balș”, the largest tertiary infectious disease center in Romania, mainly serving the capital and adjacent areas in the south of the country.
We included in the analysis all consecutive cases of influenza (children and adults) in which the presence of influenza viruses was documented by RT-PCR (single or multiplex) and in which during hospitalization the otolaryngologist (ENT physician) identified complications such as acute otitis and/or acute sinusitis. We excluded cases in which influenza was diagnosed by rapid antigen detection test, those with incomplete medical records, and those in which other viral co-infections were identified by multiplex RT-PCR or rapid antigen detection test.
Case identification was done based on ICD-10 codes specific to influenza virus infection: J10, J11. Four of the authors checked all cases for meeting the inclusion criteria. For each eligible case, demographic data (age, sex), clinical data (signs and symptoms, results of ENT consult, outcome, duration of hospitalization) and laboratory data were collected from the patient records.
Otitis cases were classified into four categories: acute otitis externa (AOE), acute congestive otitis media (ACOM), acute otitis media with effusion (AOME) and acute purulent otitis media (APOM), and sinusitis cases were classified into acute maxillary sinusitis (AMS), acute ethmoid sinusitis (AES), acute frontal sinusitis (AFS) and acute sphenoid sinusitis (ASS). Cases of sinusitis where the location was not specified were labeled as acute unclassified sinusitis (AUS).
Patients were divided into three age groups as follows: children (under 18 years), adults (between 18 and 65 years) and elderly (65 years and over). Any blood tests outside the normal laboratory range were considered high or low as appropriate.
Data were analyzed using IBM SPSS Statistics for Windows, version 25 (IBM Corp., USA). Statistical significance was set at a value of p<0.05. Categorical variables were compared using the chi-square test and we report frequency (n), percentage (%), odds-ratio (OR) and confidence interval (95%CI). For numerical variables we report median and interquartile range (IQR) with 25thand 75th percentiles, while comparisons were made using Mann-Whitney U and Kruskal-Wallis H tests.
Results
General characteristics
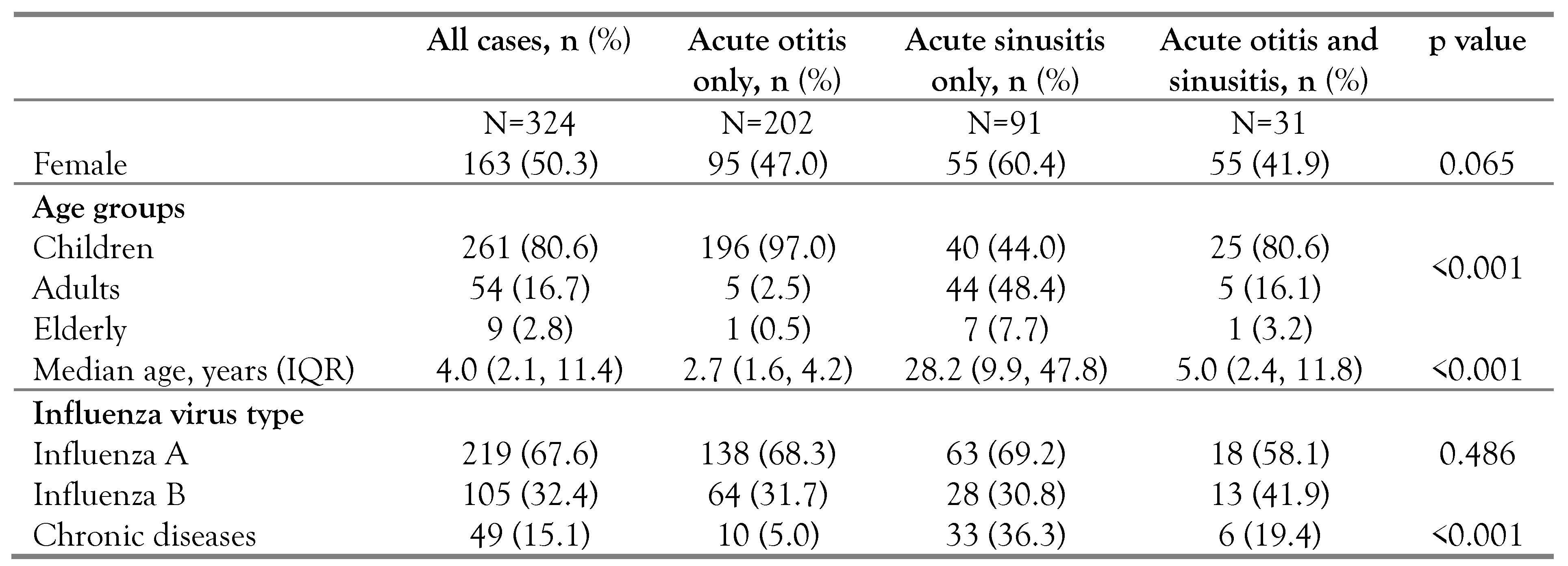
A total of 1571 cases of influenza meeting the study definition had been hospitalized during the five years and were included in the analysis. The cumulative rate of AO and AS was 20.6% (324 cases). Overall, 233 cases (71.9%) were diagnosed with otitis and 122 (37.7%) with sinusitis. Of these, 31 cases (9.4%) had concomitant otitis and sinusitis. The mean age was 4.0 years (IQR: 2.1, 11.4 years), with predominantly pediatric cases (80.6%, n=261), while only 9 cases were found in the elderly (2.8%). Influenza A viruses were identified most frequently, in 67.2% (n=221) of patients. Table 1 summarizes the general characteristics of the patients in relation to the type of complications analyzed.

Table 1.
General characteristics of patients in relation to the groups analyzed.
Clinical and laboratory features
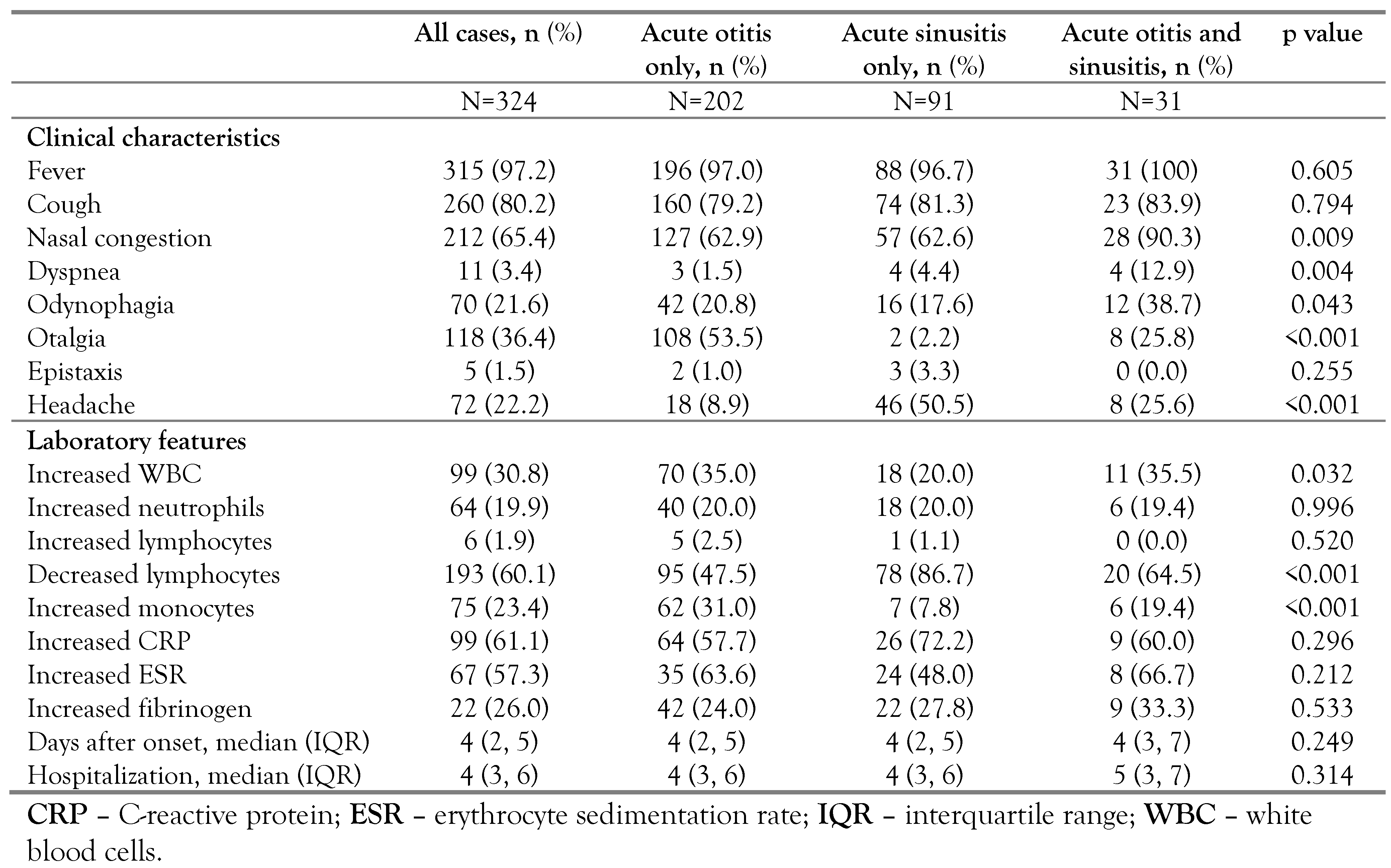
The clinical features were dominated by influenza-like symptoms, with fever (97.2%, n=315), cough (80.2%, n=260) and nasal congestion (65.4%, n=212). Otalgia was significantly more common in patients with AO (53.5%, n=108, p<0.001), headache was more common in those with AS (50.5%, n=46, p<0.001), while nasal congestion was more common in patients with concomitant otitis and sinusitis (90.3%, n=28, p=0.009). We identified no significant changes in blood tests, except for decreased lymphocyte counts more frequently in those with AS (86.7%, n=78, p<0.001), and increased monocyte counts in those with AO (31.0%, n=62, p<0.001). All clinical and laboratory characteristics are summarized in Table 2.

Table 2.
Clinical and laboratory characteristics of the groups analyzed.
Presentation to the hospital occurred in a median of 4 days (IQR: 2, 5 days) after the onset of influenza symptoms, with no differences between groups. The median length of hospital stay was 4 days (IQR: 3, 6 days) and increased by 1 day in those with concomitant otitis and sinusitis (5 days (IQR:3, 7 days), p=0.314, Table 2). Presence of chronic illness or age did not influence length of hospital stay in any of the groups analyzed (p>0.05, for each).
Classification of otitis and sinusitis by type of influenza virus
More than half of the cases of acute otitis were ACOM (56.7%, n=132), and most commonly unilateral (70.8%, n=165). AMS was the most common location of acute sinusitis (79.5%, n=97). In 28 cases (23.0%) involvement of two different sinuses was documented, and in 3 cases (2.5%) of three different sinuses. Figure 1 highlights the incidences of otitis and acute sinusitis cases by type and location.
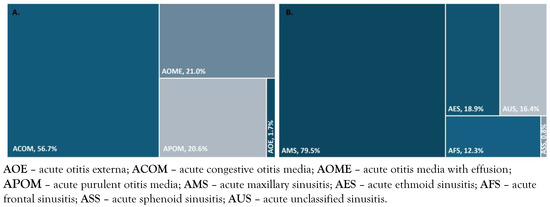
Figure 1.
Frequency of types of acute otitis (A) and acute sinusitis (B) in study patients.
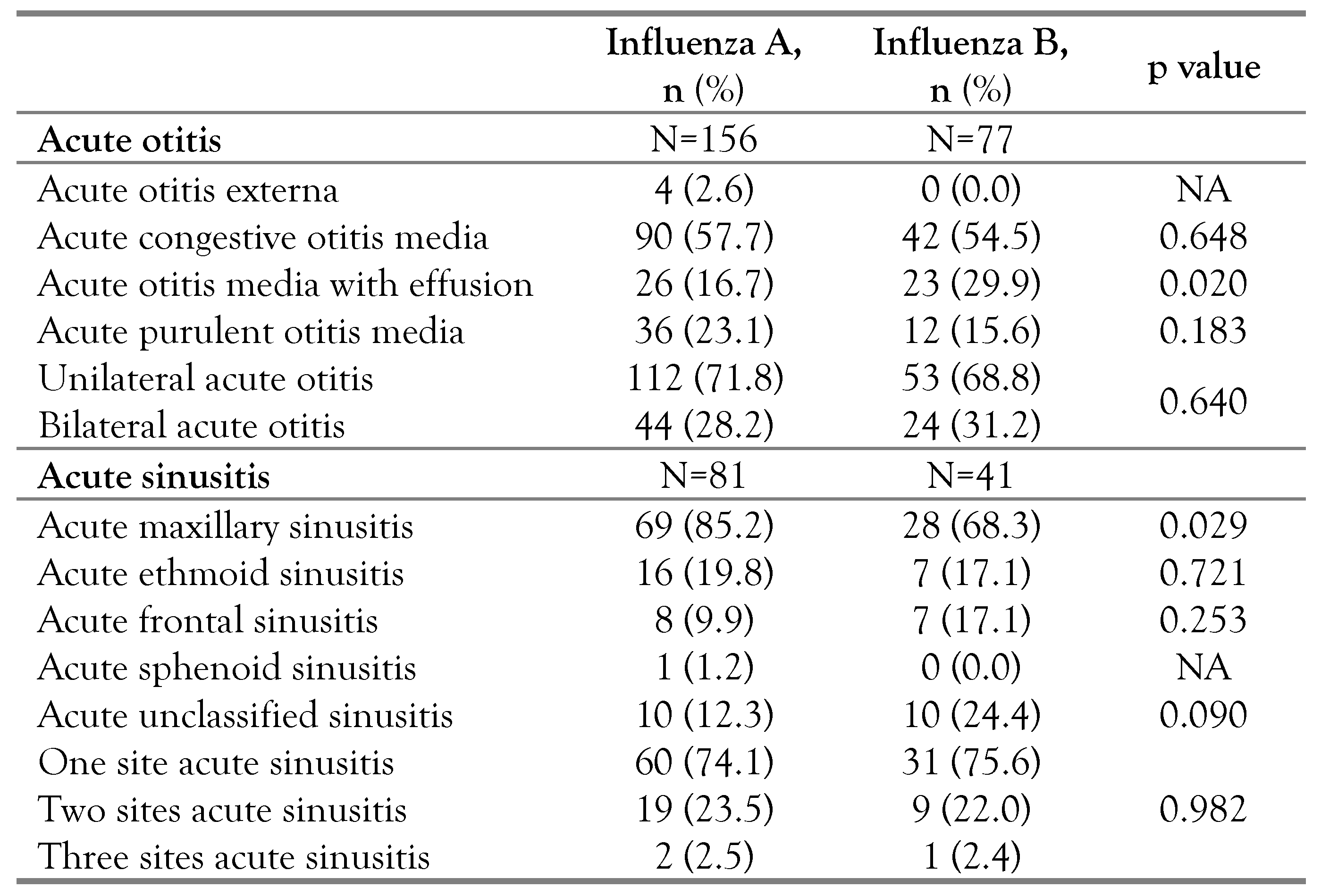
Influenza B virus infection increased the risk of ACOM 2.1-fold (p=0.020, OR=0.47, 95%CI:0.25-0.89, Table 3), and influenza A viruses increased the risk of ASM 2.7-fold (p=0.029, OR=2.67, 95%CI:1.10-6.56, Table 3).

Table 3.
Frequency of acute otitis and acute sinusitis types according to influenza viruses.
There were no differences in length of hospital stay depending on type of influenza or type of otitis or sinusitis (p>0.05 for all).
Discussion
In this study we identified a frequency of 20.6% of AO and AS in patients with influenza. Data published to date have shown variable incidences of these complications depending on the particularities of the population analyzed [3,5]. Thus, our study provides a comprehensive picture of the development of otitis and sinusitis in patients hospitalized for influenza in a large infectious disease hospital in Romania.
The majority of cases were found in the pediatric population. This is not surprising, as AOE has been shown to have an increased incidence in children, especially those under five years of age [6], where more than 70% of them experience at least one episode of otitis by this age [7].Anatomical and immune system particularities and difficulties in draining nasal secretions, are thought to be responsible for the high rates of AO in children. Our data confirm this previous knowledge also for patients with influenza, where overall the median age was 4.0 years, and in the group with only AO it was 2.7 years.
In contrast, we found that AS was more common in adults (56.1%). This is in line with the fact that paranasal sinus development is progressive over time until adulthood. At birth, children present only maxillary and ethmoid sinuses, while the sphenoid and frontal sinuses begin to pneumatize later on during childhood, a process that lasts throughout adolescence [8].
Influenza-specific symptoms dominated the clinical picture, but otalgia and headache were strongly associated with AO and AS, respectively.
Although the incidence of AO was 97%, otalgia was reported in only 53.5%, which may be explained by the fact that most young children lack the ability to subjectively report symptoms such as otalgia, sore throat or headache.
The majority of cases in our analysis were due to influenza A. However, it was noted that regardless of subtype, infection with influenza viruses can be complicated by AO or AS, and the incidence of cases is dependent on the epidemiological characteristics of each influenza season [3]. In particular, influenza B viruses were associated with a 2.1-fold increased risk for ACOM. It is known that infection with influenza B viruses is more common in children [9], which consequently leads to an increased risk of otitis.
We identified that the median length of hospital presentation from onset of influenza symptoms was 4 days, which is indicative of a late initiation of specific antiviral treatment. Several studies have shown that early treatment with oseltamivir significantly reduces complications, including otic and sinus complications, in patients with influenza [10,11], and the benefits are most pronounced in children under 5 years of age [12]. In addition, there is data showing a reduction in the rates of AO among children vaccinated for influenza [13,14], demonstrating a significant impact that influenza has on the development of otitis in the pediatric population. In Romania, however, influenza vaccination rates are low among both children [15], and adults [16,17].
The retrospective nature of the study is a limitation of our data. In addition, there was no comprehensive information on influenza A subtypes, and the identification of possible bacterial superinfections was not done systematically, so we could not provide information on the precise nature of the otitis and sinusitis of the patients in the study. However, the inclusion of a large number of influenza cases, all diagnosed by molecular virus detection provides an accurate picture of the rate of otic and sinus complications in patients hospitalized for influenza.
Conclusions
Our analysis highlights a high rate of occurrence of AO and AS in patients hospitalized with influenza, particularly among the pediatric population and those presenting late for medical evaluation and initiation of antiviral therapy. This trend highlights the need for rigorous and early assessment of patients with influenza-like illness, with a particular focus on children, in order to reduce the risk of complications.
Author Contributions
Conceptualization: VSP, ACD, DAP and OS; methodology: VSP and OS; validation: ASC and OS; formal analysis VSP, AGM, CV, RH; investigation VSP, AGM, ACD, ASC and AV; data curation CV and AV; writing—original draft preparation: VSP and OS; writing—review and editing: VSP, ASC and OS; supervision OS. All authors read and approved the final version of the manuscript.
Funding
This research received no external funding.
Conflicts of interest
All authors—none to declare.
Availability of data and material
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki and approved by the Bioethics Committee of the National Institute for Infectious Diseases “Prof. Dr. Matei Balș”, Bucharest, Romania.
References
- Heikkinen, T.; Chonmaitree, T. Importance of respiratory viruses in acute otitis media. Clin Microbiol Rev. 2003, 16, 230–241. [Google Scholar] [CrossRef] [PubMed]
- Nokso-Koivisto, J.; Marom, T.; Chonmaitree, T. Importance of viruses in acute otitis media. Curr Opin Pediatr. 2015, 27, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Hoy, G.; Kuan, G.; Lopez, R.; et al. The spectrum of influenza in children. Clin Infect Dis. 2023, 76, e1012–e1020. [Google Scholar] [CrossRef] [PubMed]
- Rynda-Apple, A.; Robinson, K.M.; Alcorn, J.F. Influenza and bacterial superinfection: Illuminating the immunologic mechanisms of disease. Infect Immun. 2015, 83, 3764–3770. [Google Scholar] [CrossRef] [PubMed]
- Hayden, F.G. Influenza virus and rhinovirus-related otitis media: Potential for antiviral intervention. Vaccine. 2000, 19 (Suppl S1), S66–S70. [Google Scholar] [CrossRef] [PubMed]
- Mohanty, S.; Podmore, B.; Cunado Moral, A.; et al. Incidence of acute otitis media from 2003 to 2019 in children ≤ 17 years in England. BMC Public Health. 2023, 23, 201. [Google Scholar] [CrossRef] [PubMed]
- Jamal, A.; Alsabea, A.; Tarakmeh, M.; Safar, A. Etiology, diagnosis, complications, and management of acute otitis media in children. Cureus. 2022, 14, e28019. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Fernandez, J.; Mirjalili, S.A.; Kirkpatrick, J. Pediatric paranasal sinuses—Development, growth, pathology, & functional endoscopic sinus surgery. Clin Anat. 2022, 35, 745–761. [Google Scholar] [CrossRef] [PubMed]
- Peltola, V.; Ziegler, T.; Ruuskanen, O. Influenza A and B virus infections in children. Clin Infect Dis. 2003, 36, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Groeneveld, G.H.; Marbus, S.D.; Ismail, N.; et al. Effectiveness of oseltamivir in reduction of complications and 30-day mortality in severe seasonal influenza infection. Int J Antimicrob Agents. 2020, 56, 106155. [Google Scholar] [CrossRef] [PubMed]
- Hanula, R.; Bortolussi-Courval, E.; Mendel, A.; Ward, B.J.; Lee, T.C.; McDonald, E.G. Evaluation of oseltamivir used to prevent hospitalization in outpatients with influenza: A systematic review and meta-analysis. JAMA Intern Med. 2024, 184, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Winther, B.; Block, S.L.; Reisinger, K.; Dutkowski, R. Impact of oseltamivir treatment on the incidence and course of acute otitis media in children with influenza. Int J Pediatr Otorhinolaryngol. 2010, 74, 684–688. [Google Scholar] [CrossRef] [PubMed]
- Norhayati, M.N.; Ho, J.J.; Azman, M.Y. Influenza vaccines for preventing acute otitis media in infants and children. Cochrane Database Syst Rev. 2017, 10, CD010089. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.W.; Huang, C.C.; Chao, W.C.; Sun, C.C.; Chiu, C.H.; Lee, T.J. Impact of influenza vaccine on childhood otitis media in Taiwan: A population-based study. PLoS ONE. 2018, 13, e0190507. [Google Scholar] [CrossRef] [PubMed]
- Miron, V.D.; Toma, A.R.; Filimon, C.; Bar, G.; Craiu, M. Optional vaccines in children-knowledge, attitudes, and practices in Romanian parents. Vaccines (Basel). 2022, 10, 404. [Google Scholar] [CrossRef] [PubMed]
- Miron, V.D.; Banica, L.; Sandulescu, O.; et al. Clinical and molecular epidemiology of influenza viruses from Romanian patients hospitalized during the 2019/20 season. PLoS ONE. 2021, 16, e0258798. [Google Scholar] [CrossRef] [PubMed]
- Draganescu, A.C.; Miron, V.D.; Streinu-Cercel, A.; et al. Circulation of influenza A viruses among patients hospitalized for severe acute respiratory infection in a tertiary care hospital in Romania in the 2018/19 season: Results from an observational descriptive epidemiological study. Medicine (Baltimore). 2021, 100, e28460. [Google Scholar] [CrossRef] [PubMed]
© GERMS 2024.