Barriers to Disinfection of Mobile Touch Screen Devices Amongst a Multidisciplinary Team in Intensive Care Units at a Tertiary Hospital
Introduction
Methods
Setting and questionnaire
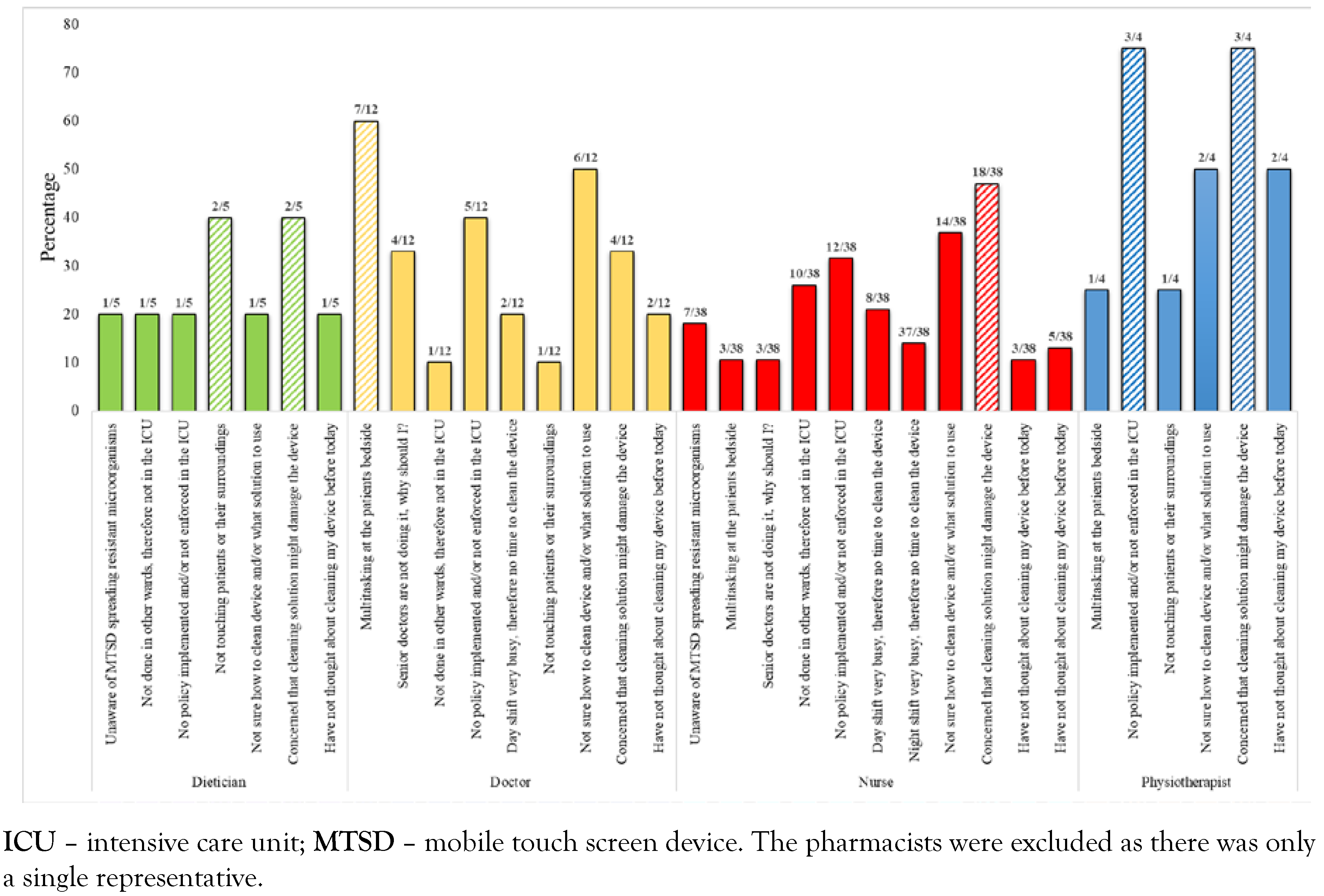
Eligibility and sample size
- n—required sample size
- P—percentage occurrence of a state or condition
- E—percentage maximum error required
- Z—value corresponding to level of confidence required
Statistical analysis and ethics
Results
Discussion
Author Contributions
Funding
Conflicts of interest
Note
Appendix A. Questionnaire
- Age
- <20
- 21–30
- 31–40
- 41–50
- >50
- Sex
- Male
- Female
- Intensive care unit
- C27
- D12
- D13
- D20
- D22
- C26
- Profession
- Medical doctor
- Nurse
- Physiotherapist
- Dietician
- Other (please specify):
- Rank
- Consultant/senior specialist
- Registrar
- Medical officer
- Nurse
- Student
- Other (please specify):
- Working time
- Day shift
- Night shift
- Average number of patients you interact with per day in the intensive care unit
- <5
- 5–10
- >10
- Do you own a mobile touch screen electronic device (cell phone, iPad, tablet etc.)?
- Yes
- No
- How often do you answer a mobile phone call in the intensive care unit?
- Never
- Sometimes
- Always
- Reason for answering or using a touch screen device at the patient’s bedside
- To look up medical information
- Consult regarding patient management or give advice to other clinicians
- Answer personal calls
- Other (please specify):
- How often do you use a handheld/personal electronic device other than a cell phone in the intensive care unit?
- Never
- Sometimes
- Always
- How often do you clean your touch screen electronic device after using it in the intensive care unit?
- Never
- Sometimes
- Always
- Do you believe electronic devices play a role in spreading resistant microorganisms in the intensive care unit?
- Yes
- No
- Do you think electronic device use should be banned in the intensive care unit?
- Yes
- No
- Are you concerned that cleaning your electronic device with a disinfectant will harm it?
- Yes
- No
- Do you know of any policy or guideline on cleaning your electronic device?
- Yes
- No
- Do you think you should wash your hands before and after using your touch screen device in the intensive care unit?
- Yes
- No
- How often do you touch a patient or their surroundings when working in the intensive care unit?
- Never
- Sometimes
- Always
- How do you decontaminate your touch screen electronic device?
- Alcohol based medium
- Chlorhexidine based medium
- Dry cloth
- Sterile water
- Ammonium based medium
- I don’t decontaminate it
- Other (please specify):
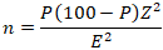
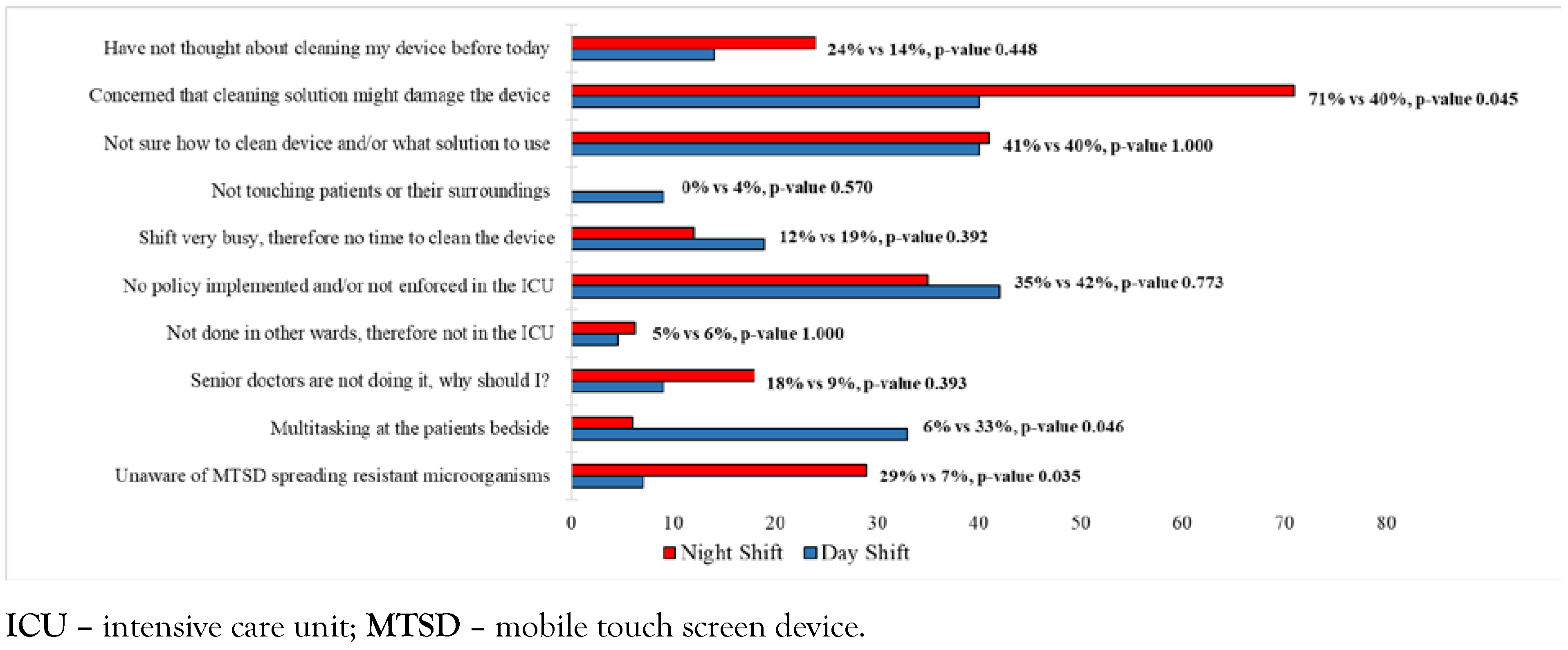
- If you don’t disinfect your electronic touch screen device in the intensive care setting regularly, what is/are the reason(s)? (More than one can be selected)
- Unaware of potential risk
- Multitasking at bedside
- Senior doctors not doing it
- Not done in other wards therefore not in the ICU
- No policy/not enforced to do it
- Day shift very busy therefore no time
- Night shift very busy therefore no time
- They are not touching patient or their surroundings
- Not sure how to clean devices/what solution to use
- Worried cleaning solution might damage the device
- Have not thought about cleaning devices before today
- Other (please specify):
References
- Martina, P.F.; Martinez, M.; Centeno, C.K.; VONSpecht, M.; Ferreras, J. Dangerous passengers: Multidrug-resistant bacteria on hands and mobile phones. J Prev Med Hyg. 2019, 60, 293–299. [Google Scholar] [CrossRef]
- Leong, X.Y.A.; Chong, S.Y.; Koh, S.E.A.; Yeo, B.C.; Tan, K.Y.; Ling, M.L. Healthcare workers’ beliefs, attitudes and compliance with mobile phone hygiene in a main operating theatre complex. Infect Prev Pract. 2020, 2, 100031. [Google Scholar] [CrossRef] [PubMed]
- Taherdoost, H. Determining sample size; How to calculate survey sample size. Int J Econ Manag Systems. 2017, 2, 237–239. [Google Scholar]
- Missri, L.; Smiljkovski, D.; Prigent, G.; et al. Bacterial colonization of healthcare workers' mobile phones in the ICU and effectiveness of sanitization. J Occup Environ Hyg. 2019, 16, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Manning, M.L.; Davis, J.; Sparnon, E.; Ballard, R.M. iPads, droids, and bugs: Infection prevention of mobile handheld devices at the point of care. Am J Infect Control. 2013, 41, 1073–1076. [Google Scholar] [CrossRef] [PubMed]
- Graveto, J.M.; Costa, P.J.; Santos, C.I. Cell phone usage by health personnel: Preventive strategies to decrease risk of cross infection in clinical context. Texto Contexto Enferm. 2018, 27, e5140016. [Google Scholar] [CrossRef][Green Version]
© GERMS 2021.
Share and Cite
Opperman, C.J.; Khan, F.; Piercy, J.L.; Samodien, N. Barriers to Disinfection of Mobile Touch Screen Devices Amongst a Multidisciplinary Team in Intensive Care Units at a Tertiary Hospital. Germs 2021, 11, 329-336. https://doi.org/10.18683/germs.2021.1270
Opperman CJ, Khan F, Piercy JL, Samodien N. Barriers to Disinfection of Mobile Touch Screen Devices Amongst a Multidisciplinary Team in Intensive Care Units at a Tertiary Hospital. Germs. 2021; 11(2):329-336. https://doi.org/10.18683/germs.2021.1270
Chicago/Turabian StyleOpperman, Christoffel J., Farheen Khan, Jenna L. Piercy, and Nazlee Samodien. 2021. "Barriers to Disinfection of Mobile Touch Screen Devices Amongst a Multidisciplinary Team in Intensive Care Units at a Tertiary Hospital" Germs 11, no. 2: 329-336. https://doi.org/10.18683/germs.2021.1270
APA StyleOpperman, C. J., Khan, F., Piercy, J. L., & Samodien, N. (2021). Barriers to Disinfection of Mobile Touch Screen Devices Amongst a Multidisciplinary Team in Intensive Care Units at a Tertiary Hospital. Germs, 11(2), 329-336. https://doi.org/10.18683/germs.2021.1270



