Abstract
Introduction: Gastrointestinal tuberculosis is an important form of extrapulmonary tuberculosis but liver involvement is uncommon. Hepatic tuberculosis can manifest in variable manners including as a space occupying lesion, diffuse infiltration by granulomas (granulomatous hepatitis) and as liver abscess. Hepatic tuberculosis is usually associated with lesions elsewhere but the diagnosis is often not considered because of rarity. Case report: We report two cases of hepatic involvement by tuberculosis: one in the form of liver abscess and the other having multiple hypodense hepatic lesions along with peritoneal involvement. The presence of ascites, visceral scalloping and multiple hypodense lesions resulted in a diagnostic confusion with disseminated malignancy but GeneXpert Ultra (Cepheid, USA) helped in making the diagnosis. Discussion: Hepatic tuberculosis should be considered in the differential diagnosis of hepatic space occupying lesions and abscesses. This is especially important in TB endemic regions and in patients where there is involvement of other organs especially the lungs. Conclusions: Newer microbiological modalities including GeneXpert Ultra could help in making a diagnosis of hepatic tuberculosis.
Introduction
Tuberculosis of the abdomen can involve the gastrointestinal tract, peritoneum, lymph nodes or solid organs [1]. Hepatic tuberculosis is an uncommon form of abdominal tuberculosis, which may manifest in a number of clinical patterns. While hepatic tuberculosis could occur as part of miliary tuberculosis, localized forms may manifest as hepatic space occupying lesions (tuberculomas), abscesses or granulomatous hepatitis [2]. We report the cases of two patients with hepatic tuberculosis diagnosed using the GeneXpert Ultra assay (Cepheid, USA).
Case report
Case 1
A 30-year-old female patient presented with high grade fever and abdominal pain for two weeks. There was no personal history of any past diseases or tuberculosis. Her father had suffered from pulmonary tuberculosis around 8 years back, which was fully treated. She had pallor and pedal edema, breath sounds were decreased on the right lower lung bases, and on abdominal palpation tender hepatomegaly was noted. Investigations suggested severe iron deficiency anemia (hemoglobin: 5.6 g/L, MCV: 72 fL) and on liver functions tests, hypoalbuminemia (2.3 g/dL) was present. Abdominal ultrasound revealed a large hypoechoic lesion in the right lobe of liver with mild ascites and right pleural effusion. Chest X-ray showed mild right sided pleural effusion. Contrast enhanced computed tomography (CECT) CECT of the abdomen showed 14 × 7 × 11 cm of large multiloculated inter-communicating and peripherally enhancing lesion with irregular margins with perilesional edema (Figure 1). A percutaneous drainage along with antibiotics (intravenous piperacillin + tazobactam 4.5 g thrice daily and intravenous metronidazole 750 mg thrice daily for seven days) were the initial therapy. The cultures and Gram stain from the drained fluid were negative. The patient continued to have fever even after a week. To exclude tuberculosis, acid-fast bacilli (AFB) stain, culture and GeneXpert MTB/RIF Ultra were sent from the percutaneous drainage fluid after lack of response to a week of antibiotics. Xpert Ultra was positive for Mycobacterium tuberculosis, AFB culture and stain were negative. Four drug standard antitubercular therapy (ATT) was started. This included isoniazid (5 mg/kg), rifampin (10 mg/kg), pyrazinamide (25 mg/kg) and ethambutol (15 mg/kg) and after two months, pyrazinamide was stopped. The fever responded and the drain was removed after two weeks from the initial insertion. At 4 months of treatment the patient showed resolution of the abscess on ultrasound and weight gain. The ATT was stopped after completion of six months of therapy.
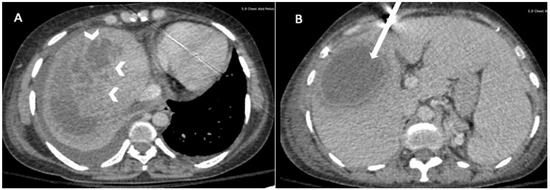
Figure 1.
(A) Hepatic multiloculated hypodense lesion with irregular margins (arrowhead) and (B) perilesional edema (white arrow).
Case 2
A 19-year-old female without any comorbidity presented with amenorrhea of 6 months and loss of appetite and weight (12 kg in 6 months). She had also noted abdominal distension without any significant pain during the past 3 months. She did not give any history of tuberculosis in the past neither any history of contact with tuberculosis in the family. On examination, she had pallor and was emaciated with a body mass index of 14.4 kg/m2. On systemic examination, there was shifting dullness to confirm ascites without any organomegaly, the respiratory system examination was unremarkable. The liver functions were normal (serum bilirubin: 0.8 mg/dL, alanine aminotransferase: 22 U/L, aspartate aminotransferase: 27 U/L, alkaline phosphatase: 78 U/L) with low albumin (2.8 g/dL). CECT of the chest and abdomen showed multiple peripheral hypodense lesions in the liver with scalloping of the liver surface along with peritoneal thickening, enhancement, and nodularity with necrotic abdominal, mesenteric, and retroperitoneal lymphadenopathy and bilateral hydrosalpinx along with random soft tissue nodules bilaterally in the lungs with centrilobular nodules in the left upper lobe (Figure 2). Ascitic fluid workup showed low serum ascites albumin gradient (SAAG: 0.7 g/dL), lymphocytic ascites with ascitic adenosine deaminase of 88 U/L. There were no AFB on concentration smear. GeneXpert Ultra was positive for Mycobacterium tuberculosis complex from the ascitic fluid and from the fluid aspirated from the hepatic lesions. She was started on weight-based ATT with isoniazid (5 mg/kg), rifampicin (10 mg/kg), ethambutol (15 mg/kg) and pyrazinamide (25 mg/kg) daily with clinical improvement after 2 weeks of treatment. At 2 months of therapy, ultrasound showed resolution of ascites with reduction in number and size of hepatic lesions. She is presently in the continuation phase with isoniazid, rifampicin and ethambutol. We plan to continue the same for a total therapy for 6 months.

Figure 2.
(A) Multiple subcapsular (white arrow) and intrahepatic (black arrow) space hypodense lesions with scalloping of liver; (B) ascites with peritoneal thickening and enhancement (white arrow).
Discussion
The clinical and radiological appearance of abdominal tuberculosis can be extremely variable and it can mimic a number of diseases including gastrointestinal malignancies, peritoneal carcinomatosis and inflammatory bowel disease [1]. Hepatic tuberculosis is a rare form of involvement that usually occurs along with involvement of other locations. Hepatic involvement could occur as part of hematogenous spread through the hepatic artery from a pulmonary focus but it may also result from dissemination from a gastrointestinal focus via the portal vein [2]. The presentation of hepatic tuberculosis could be in the form of an infiltrative pattern due to granulomatous hepatitis with hepatomegaly and elevated alkaline phosphatase [3]. Localized forms could present with single or multiple mass forming lesions in the hepatic parenchyma. Another pattern is presentation in the form of non-resolving liver abscess as in the first patient [4]. Indeed, the diagnosis must be considered in patients with liver abscess in endemic regions who do not respond to initial treatment aimed at amebic or pyogenic etiology. Molecular diagnosis including GeneXpert may help in diagnosis [4,5]. The diagnostic evaluation is guided primarily by the radiological findings. In patients with infiltrative disease (diffuse hepatomegaly, elevated alkaline phosphatase) a liver biopsy may be resorted to while in patients with mass lesion a guided percutaneous imaging-guided biopsy should be done. In patients with abscess-like lesions, as in our cases, the analysis of abscess fluid could help in reaching a diagnosis. The findings on histopathology include presence of granuloma, which can be found in around two-thirds of patients [2]. Hepatic granulomas, however, are non-specific and could occur in a large number of conditions including other infections (atypical mycobacteria, brucellosis, listeriosis, Q fever, syphilis, Whipple’s disease, schistosomiasis, toxoplasmosis, cryptococcosis, candidiasis, nocardiosis), autoimmune conditions (sarcoidosis, primary biliary cholangitis, Churg Strauss, polyarteritis nodosa), neoplastic diseases (lymphoma), metal toxicity and foreign material ingestions [6]. The presence of cheesy material may provide some degree of specificity to the diagnosis of tuberculosis [2].
The presence of multiple hypodense lesions in the liver can be confused with cystic disease of the liver, parasitic diseases like the hydatid cyst or with disseminated malignancy. In our second case, the presence of visceral scalloping also pointed to underlying malignancy, but this radiologic abnormality has also been reported in the presence of peritoneal tuberculosis [7]. Some of the lesions were subcapsular suggesting a serohepatic pattern of tuberculosis [8]. Therefore, peritoneal tuberculosis should be considered in patients who present with findings akin to peritoneal carcinomatosis, especially if cytological examination is negative for tumor cells. Microbiological positivity in the form of culture or molecular techniques provides the gold standard for diagnosis. The specificity and sensitivity of GeneXpert MTB/RIF for the diagnosis of hepatic tuberculosis is uncertain as only one case series has been reported in the past [4]. For the diagnosis of peritoneal tuberculosis the testing of ascitic fluid provided a sensitivity of 64% with 97% specificity when compared to culture. The sensitivity was 30% with 100% specificity when compared to composite reference standard [9]. Peritoneal examination with laparoscopy may need to be done in cases where diagnosis is unclear after routine examination.
Conclusions
We reported two cases of hepatic involvement by tuberculosis. The findings point to the need to consider this as a differential diagnosis of hepatic lesions in endemic regions. The diagnosis must be considered in non-resolving liver abscess and multiple hepatic hypodense lesions.
Author Contributions
AC, JS, VS: initial draft of manuscript; AC, JS, GM, DKJ, PG, VS: clinical care of patient; PG: interpretation of radiology; AC, JS, GM, DKJ: literature review; VS: manuscript drafting and review; all authors: final approval. All authors read and approved the final version of the manuscript.
Funding
None to declare.
Informed Consent Statement
Written informed consent was obtained from both patients for the publication of this case report and the accompanying images.
Conflicts of interest
All authors—none to declare.
References
- Goyal, P.; Shah, J.; Gupta, S.; Gupta, P.; Sharma, V. Imaging in discriminating intestinal tuberculosis and Crohn's disease: Past, present and the future. Expert Rev Gastroenterol Hepatol. 2019, 13, 995–1007. [Google Scholar] [CrossRef] [PubMed]
- Hickey, A.J.; Gounder, L.; Moosa, M.Y.; Drain, P.K. A systematic review of hepatic tuberculosis with considerations in human immunodeficiency virus co-infection. BMC Infect Dis. 2015, 15, 209. [Google Scholar] [CrossRef] [PubMed]
- Ozaras, R.; Yemisen, M.; Balkan, I.I. More on hepatic granulomas. Diagn Pathol. 2015, 10, 203. [Google Scholar] [CrossRef] [PubMed]
- Agarwala, R.; Dhooria, S.; Khaire, N.S.; et al. Xpert MTB/RIF for diagnosis of tubercular liver abscess. A case series. Infez Med. 2020, 28, 420–424. [Google Scholar] [PubMed]
- Sharma, K.; Gupta, N.; Goyal, K.; Duseja, A.K.; Sharma, A.; Rajwanshi, A. Evaluation of polymerase chain reaction in space-occupying lesions of liver reported as granulomatous inflammation/tuberculosis on fine-needle aspiration cytology. Cytojournal. 2017, 14, 1. [Google Scholar] [CrossRef] [PubMed]
- Culver, E.L.; Watkins, J.; Westbrook, R.H. Granulomas of the liver. Clin Liver Dis (Hoboken). 2016, 7, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Bhatia, A.; Malik, S.; Singh, N.; Rana, S.S. Visceral scalloping on abdominal computed tomography due to abdominal tuberculosis. Ther Adv Infect Dis. 2017, 4, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Yu, R.S.; Zhang, S.Z.; Wu, J.J.; Li, R.F. Imaging diagnosis of 12 patients with hepatic tuberculosis. World J Gastroenterol. 2004, 10, 1639–1642. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Soni, H.; Kumar, M.P.; et al. Diagnostic accuracy of the Xpert MTB/RIF assay for abdominal tuberculosis: A systematic review and meta-analysis. Expert Rev Anti Infect Ther. 2021, 19, 253–265. [Google Scholar] [CrossRef] [PubMed]
© GERMS 2021.