COVID-19 Deaths and Associated Demographic Factors in Central Java, Indonesia
Abstract
Introduction
Methods
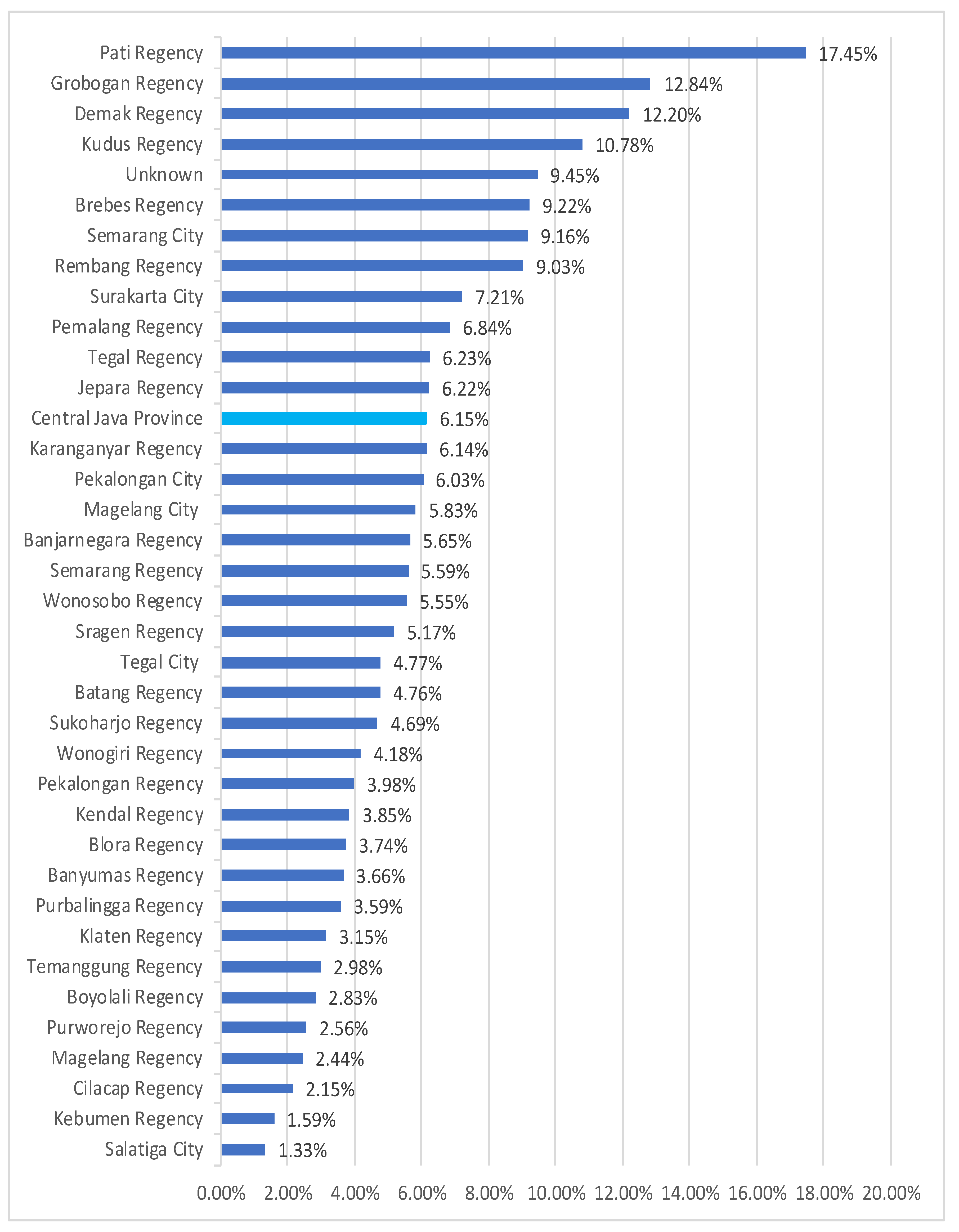
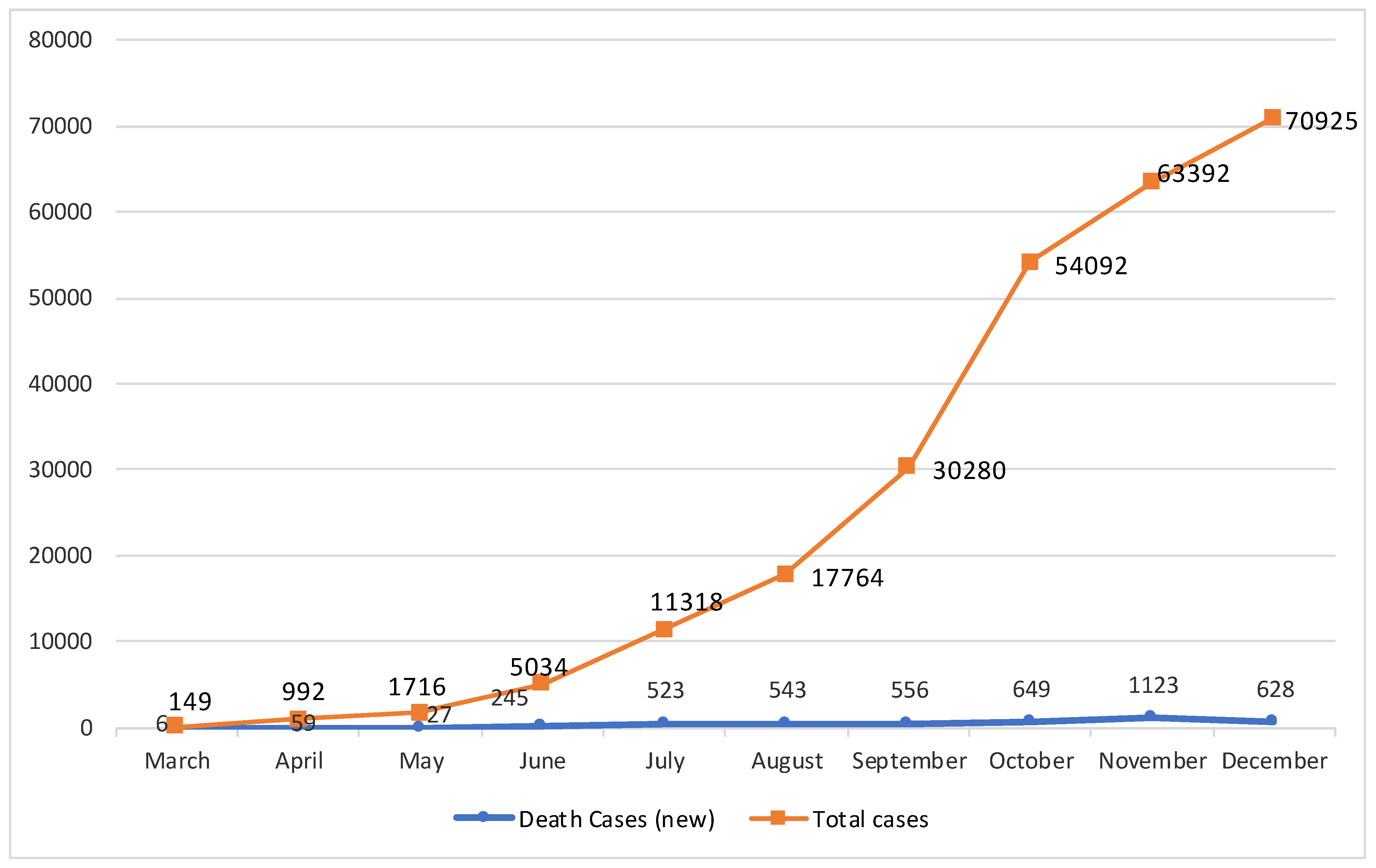
Results
Discussion
Conclusions
Funding
Authors’ Contributions Statement
Conflicts of Interest
Acknowledgments
References
- World Health Organization. Novel Coronavirus—Thailand (ex-China). 2020. Available online: https://www.who.int/csr/don/14-january-2020-novel-coronavirus-thailand-ex-china/en/ (accessed on 29 December 2020).
- World Health Organization. Media Statement on Confirmed COVID-19. 2020. Available online: https://www.who.int/indonesia/news/detail/02-03-2020-media-statement-on-covid-19 (accessed on 29 December 2020).
- World Health Organization. Weekly Epidemiological Update—20 October 2020. 2020. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update 20-october-2020 (accessed on 29 December 2020).
- Indonesian Ministry of Health. COVID-19 Update 14 December 2020. 2020. Available online: https://infeksiemerging.kemkes.go.id/document/situasi-terkini-perkembangan-covid-19-14-desember-2020/view (accessed on 29 December 2020).
- Sutiningsih, D.; Eka Fitri Rahatina, V.; Prabowo, Y.; Haryanto, A.; Agung Wibowo, M. Epidemiologic and clinical characteristics of patients with Covid-19 in Central Java, Indonesia. E3S Web Conf. 2020, 202, 12014. [Google Scholar] [CrossRef]
- Livingston, E.; Bucher, K. Coronavirus disease 2019 (COVID-19) in Italy. JAMA 2020, 323, 1335. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Laxminarayan, R.; Wahl, B.; Dudala, S.R.; et al. Epidemiology and transmission dynamics of COVID-19 in two Indian states. Science 2020, 370, 691–697. [Google Scholar] [CrossRef]
- Korean Society of Infectious Diseases and Korea Centers for Disease Control and Prevention. Analysis on 54 mortality cases of coronavirus disease 2019 in the Republic of Korea from January 19 to March 10, 2020. J Korean Med Sci. 2020, 35, e132. [Google Scholar] [CrossRef]
- Nikpouraghdam, M.; Jalali Farahani, A.; Alishiri, G.; et al. Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in IRAN: A single center study. J Clin Virol. 2020, 127, 104378. [Google Scholar] [CrossRef]
- CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020, 69, 343–346. [Google Scholar] [CrossRef]
- Parra-Bracamonte, G.M.; Lopez-Villalobos, N.; Parra-Bracamonte, F.E. Clinical characteristics and risk factors for mortality of patients with COVID-19 in a large data set from Mexico. Ann Epidemiol. 2020, 52, 93–98.e2. [Google Scholar] [CrossRef]
- Fu, L.; Fei, J.; Xiang, H.X.; et al. Influence factors of death risk among COVID-19 patients in Wuhan, China: A hospital-based case-cohort study. medRxiv. 2020. [Google Scholar] [CrossRef]
- Caramelo, F.; Ferreira, N.; Oliveiros, B. Estimation of risk factors for COVID-19 mortality -preliminary results. medRxiv. 2020. [Google Scholar] [CrossRef]
- Mizumoto, K.; Saitoh, M.; Chowell, G.; Miyamatsu, Y.; Nishiura, H. Estimating the risk of Middle East respiratory syndrome (MERS) death during the course of the outbreak in the Republic of Korea, 2015. Int J Infect Dis. 2015, 39, 7–9. [Google Scholar] [CrossRef]
- Mizumoto, K.; Endo, A.; Chowell, G.; Miyamatsu, Y.; Saitoh, M.; Nishiura, H. Real-time characterization of risks of death associated with the Middle East respiratory syndrome (MERS) in the Republic of Korea, 2015. BMC Med. 2015, 13, 228. [Google Scholar] [CrossRef]
- Jia, N.; Feng, D.; Fang, L.Q.; et al. Case fatality of SARS in mainland China and associated risk factors. Trop Med Int Health. 2009, 14, 21–27. [Google Scholar] [CrossRef]
- Wu, C.; Chen, X.; Cai, Y.; et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020, 180, 1031. [Google Scholar] [CrossRef]
- Sinclair, A.J.; Abdelhafiz, A.H. Age, frailty and diabetes -triple jeopardy for vulnerability to COVID-19 infection. EClinicalMedicine. 2020, 22, 100343. [Google Scholar] [CrossRef] [PubMed]
- Sahu, B.R.; Kampa, R.K.; Padhi, A.; Panda, A.K. C-reactive protein: A promising biomarker for poor prognosis in COVID-19 infection. Clin Chim Acta. 2020, 509, 91–94. [Google Scholar] [CrossRef]
- Palaiodimos, L.; Kokkinidis, D.G.; Li, W.; et al. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism. 2020, 108, 154262. [Google Scholar] [CrossRef]
- Chen, X.; Chughtai, A.A.; Dyda, A.; Macintyre, C.R. Comparative epidemiology of Middle East respiratory syndrome coronavirus (MERS-CoV) in Saudi Arabia and South Korea. Emerg Microbes Infect. 2017, 6, e51. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Du, X.; Chen, J.; et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J Infect. 2020, 81, e6–e12. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Cui, P.; Zeng, S.; et al. Risk factors for developing into critical COVID-19 patients in Wuhan, China: A multicenter, retrospective, cohort study. EClinicalMedicine. 2020, 25, 100471. [Google Scholar] [CrossRef]
- Wang, A.L.; Zhong, X.; Hurd, YL. Comorbidity and sociodemographic determinants in COVID-19 mortality in an US urban healthcare system. medRxiv. 2020. [Google Scholar] [CrossRef]
| A | ||||||||||||||||||||||
| Characteristics | CFR (%) Total = 6.15% | Total a F = 70,925 | % | Death | p Value | |||||||||||||||||
| Yes F = 4359 | (%) | No F = 56,290 | (%) | |||||||||||||||||||
| Age | ||||||||||||||||||||||
| Median (IQR), years | - | 42 (28–54) | - | 58 (50–65) | - | 40 (26–53) | - | <0.001 *b | ||||||||||||||
| ≥60 years (elderly) | 17.95 | 10,568 | 14.90 | 1897 | 43.52 | 6926 | 12.30 | |||||||||||||||
| 45–59 years (pre-elderly) | 8.74 | 21,590 | 30.44 | 1886 | 43.27 | 16,275 | 28.91 | |||||||||||||||
| 19–44 years (adult) | 1.77 | 31,153 | 43.92 | 550 | 12.62 | 26,217 | 46.57 | |||||||||||||||
| 10–18 years (youth) | 0.24 | 5017 | 7.07 | 12 | 0.28 | 4566 | 8.11 | |||||||||||||||
| 6–9 years (children) | 0.20 | 1004 | 1.42 | 2 | 0.05 | 877 | 1.56 | |||||||||||||||
| 1–5 years (toddlers) | 0.52 | 1155 | 1.63 | 6 | 0.14 | 1041 | 1.85 | |||||||||||||||
| 0 years (infants) | 1.37 | 438 | 0.62 | 6 | 0.14 | 388 | 0.69 | |||||||||||||||
| Gender | ||||||||||||||||||||||
| Male | 7.60 | 32,838 | 46.30 | 2497 | 57.28 | 25,604 | 45.49 | <0.001 *b | ||||||||||||||
| Female | 4.89 | 38,087 | 53.70 | 1862 | 42.72 | 30,686 | 54.51 | |||||||||||||||
| B | ||||||||||||||||||||||
| Age and gender | Male | Female | ||||||||||||||||||||
| Median (IQR) | Mean (95%CI) | Minimum–maximum | Median (IQR) | Mean (95%CI) | Minimum–Maximum | |||||||||||||||||
| Age, years | 58 (51–72) | 57.47 (57.00–57.95) | 0–92 | 57 (50–64) | 56.23 (55.68–56.78) | 0–100 | ||||||||||||||||
| C | ||||||||||||||||||||||
| Comorbidity | Total | % | Male | Female | p value | ≥60 years | <60 years | p value | ||||||||||||||
| Having comorbidity | 2868/4359 | 65.79 | 1622 | 1246 | 0.394 | 1231 | 1637 | <0.001*b | ||||||||||||||
| >1 comorbidity | 784/4359 | 17.99 | 428 | 356 | - | 364 | 420 | - | ||||||||||||||
| Diabetes mellitus | 1387/4359 | 31.82 | 722 | 665 | 0.004 *b | 573 | 814 | <0.001 *b | ||||||||||||||
| Hypertension | 817/4359 | 18.74 | 485 | 332 | 0.652 | 374 | 443 | <0.001 *b | ||||||||||||||
| Heart disease | 454/4359 | 10.42 | 262 | 192 | 0.908 | 236 | 218 | <0.001 *b | ||||||||||||||
| Kidney failure | 316/4359 | 7.25 | 216 | 100 | 0.002 *b | 115 | 201 | 0.095 b | ||||||||||||||
| Congestive heart failure | 237/4359 | 5.44 | 126 | 111 | 0.184 b | 131 | 106 | <0.001 *b | ||||||||||||||
| Stroke | 154/4359 | 3.53 | 90 | 64 | 1.000 | 85 | 69 | <0.001 *b | ||||||||||||||
| Ischemic heart disease | 97/4359 | 2.23 | 46 | 51 | 0.053 b | 40 | 57 | 0.055 b | ||||||||||||||
| Anemia | 83/4359 | 1.90 | 36 | 47 | 0.012 *b | 40 | 43 | 0.002 *b | ||||||||||||||
| Pulmonary TB | 72/4359 | 1.65 | 46 | 26 | 0.411 | 29 | 43 | 0.139 b | ||||||||||||||
| Chronic obstructive pulmonary disease | 68/4359 | 1.56 | 48 | 20 | 0.060 b | 31 | 37 | 0.019 *b | ||||||||||||||
| Cancer | 61/4359 | 1.40 | 23 | 38 | 0.003 *b | 22 | 39 | 0.506 | ||||||||||||||
| Obesity | 44/4359 | 1.01 | 24 | 20 | 0.746 | 7 | 37 | 0.048 *b | ||||||||||||||
| Hepatitis | 32/4359 | 0.73 | 22 | 10 | 0.313 | 12 | 20 | 0.567 | ||||||||||||||
| Asthma | 22/4359 | 0.50 | 11 | 11 | 0.581 | 7 | 15 | 1.000 | ||||||||||||||
| Etc. | 25/4359 | 0.57 | 11 | 14 | - | 5 | 20 | - | ||||||||||||||
| No comorbidities | 964/4359 | 22.12 | 561 | 403 | - | 300 | 664 | - | ||||||||||||||
| Unknown | 527/4359 | 12.09 | 314 | 213 | - | 365 | 162 | - | ||||||||||||||
| Univariable OR (95% CI) | p Value | Multivariable OR (95% CI) | p Value | Goodness of Fit Test for Multivariate Analysis | ||||
|---|---|---|---|---|---|---|---|---|
| Omnibus Test | Hosmer-Lemeshow Test | |||||||
| X2 | p Value | X2 | p Value | |||||
| COVID-19 fatality | ||||||||
| Elderly (≥60 years) | 5.492 (5.146–5.860) | <0.001 * | 5.360 (5.022–5.720) | <0.001 * | 2508.113 | <0.001 * | 1.278 | 0.528 |
| Male | 1.607 (1.510–1.710) | <0.001 * | 1.491 (1.398–1.589) | <0.001 * | ||||
| Presence of comorbidity | ||||||||
| Having comorbidity (Elderly) | 1.664 (1.425–1.944) | <0.001 * | - | - | - | - | - | - |
| Diabetes mellitus (DM) | ||||||||
| Elderly | 1.558 (1.310–1.853) | <0.001 * | 1.577 (1.325–1.876) | <0.001 * | 35.447 | <0.001 | 0.012 | 0.994 |
| Female | 1.282 (1.086–1.513) | 0.003 * | 1.307 (1.106–1.544) | 0.002 * | ||||
| Hypertension (Elderly) | 1.869 (1.539–2.268) | <0.001 * | - | - | - | - | - | - |
| Heart disease (Elderly) | 2.396 (1.905–3.013) | <0.001 * | - | - | - | - | - | - |
| Kidney failure | ||||||||
| Elderly | 1.266 (0.970–1.653) | 0.083 | 1.263 (0.966–1.651) | 0.088 | 13.386 | 0.001 | 4.129 | 0.127 |
| Male | 1.552 (1.185–2.031) | 0.001 * | 1.549 (1.183–2.029) | 0.001 * | ||||
| Congestive heart failure | ||||||||
| Elderly | 2.735 (2.047–3.656) | <0.001 * | 2.763 (2.066–3.696) | <0.001 * | 49.244 | <0.001 * | 0.001 | 1.000 |
| Female | 1.226 (0.922–1.631) | 0.161 | 1.277 (0.954–1.710) | 0.100 | ||||
| Stroke (Elderly) | 2.727 (1.930–3.852) | <0.001 * | - | - | - | - | - | - |
| Ischemic heart disease | ||||||||
| Elderly | 1.533 (1.014–2.380) | 0.043 * | 1.580 (1.030–2.423) | 0.036 * | 8.401 | 0.015 | 0.140 | 0.933 |
| Female | 1.543 (1.016–2.346) | 0.042 * | 0.568 (1.030–2.386) | 0.036 * | ||||
| Anemia | ||||||||
| Elderly | 2.059 (1.311–3.234) | 0.002 * | 2.106 (1.338–3.316) | 0.001 * | 16.882 | <0.001 * | 0.260 | 0.878 |
| Female | 1.817 (1.156–2.858) | 0.01 * | 1.865 (1.183–2.940) | 0.007 * | ||||
| Pulmonary TB (Elderly) | 1.493 (0.914–2.437) | 0.109 | - | - | - | - | - | - |
| Chronic obstructive pulmonary disease | ||||||||
| Elderly | 1.854 (1.129–3.046) | 0.015 * | 1.805 (1.097–2.969) | 0.020 * | 9.452 | 0.009 | 3.372 | 0.185 |
| Male | 1.724 (1.008–2.950) | 0.047 * | 1.669 (0.974–2.862) | 0.062 | ||||
| Cancer (Female) | 2.300 (1.349–3.921) | 0.002 * | - | - | - | - | - | - |
| Obesity (<60 years) | 2.388 (1.053–5.418) | 0.037 * | - | - | - | - | - | - |
| Job | Frequency | % |
|---|---|---|
| Entrepreneur | 638 | 14.64 |
| Unemployed | 497 | 11.40 |
| Minding household | 465 | 10.67 |
| Private employee | 443 | 10.16 |
| Retired | 223 | 5.12 |
| Agriculture sector | 235 | 5.39 |
| Trading | 203 | 4.66 |
| Civil servant | 174 | 3.99 |
| Freelancer | 92 | 2.11 |
| Teacher | 57 | 1.31 |
| Driver | 24 | 0.55 |
| Police | 19 | 0.44 |
| Student | 18 | 0.41 |
| State/regional owned enterprises employees | 13 | 0.30 |
| Army | 12 | 0.28 |
| Fisheries | 11 | 0.25 |
| Nurse | 10 | 0.23 |
| Doctor | 7 | 0.16 |
| Islamic teacher | 6 | 0.14 |
| Regency/city/provincial people’s representative council members | 6 | 0.14 |
| Lecturer | 5 | 0.11 |
| Honorary employees | 4 | 0.09 |
| Village apparatus | 17 | 0.39 |
| Breeder | 4 | 0.09 |
| Mechanic | 3 | 0.07 |
| Housemaid | 3 | 0.07 |
| Nun | 2 | 0.05 |
| Midwife | 2 | 0.05 |
| Pastor | 2 | 0.05 |
| Tailor | 2 | 0.05 |
| Mosque imam | 1 | 0.02 |
| Chef | 1 | 0.02 |
| Lawyer | 1 | 0.02 |
| Bricklayer | 1 | 0.02 |
| Carpenter | 1 | 0.02 |
| Blacksmith | 1 | 0.02 |
| Unknown | 1156 | 26.52 |
| Total | 4359 | 100 |
© GERMS 2021.
Share and Cite
Sutiningsih, D.; Azzahra, N.A.; Prabowo, Y.; Sugiharto, A.; Wibowo, M.A.; Lestari, E.S.; Aurorina, E. COVID-19 Deaths and Associated Demographic Factors in Central Java, Indonesia. Germs 2021, 11, 255-265. https://doi.org/10.18683/germs.2021.1262
Sutiningsih D, Azzahra NA, Prabowo Y, Sugiharto A, Wibowo MA, Lestari ES, Aurorina E. COVID-19 Deaths and Associated Demographic Factors in Central Java, Indonesia. Germs. 2021; 11(2):255-265. https://doi.org/10.18683/germs.2021.1262
Chicago/Turabian StyleSutiningsih, Dwi, Nur Azizah Azzahra, Yulianto Prabowo, Aris Sugiharto, Mufti Agung Wibowo, Endah Sri Lestari, and Estri Aurorina. 2021. "COVID-19 Deaths and Associated Demographic Factors in Central Java, Indonesia" Germs 11, no. 2: 255-265. https://doi.org/10.18683/germs.2021.1262
APA StyleSutiningsih, D., Azzahra, N. A., Prabowo, Y., Sugiharto, A., Wibowo, M. A., Lestari, E. S., & Aurorina, E. (2021). COVID-19 Deaths and Associated Demographic Factors in Central Java, Indonesia. Germs, 11(2), 255-265. https://doi.org/10.18683/germs.2021.1262




