Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection transmission occurs between persons through droplet and aerosols [
1]. Household contacts have a high risk of infection with a secondary attack rate as high as 27.8% among spouses of index patients [
2]. Transmission outside the home can occur at closed locations with restricted air circulation and open locations with free air movement. The transmission risk at open environment is unclear. We report a low secondary attack rate among contacts of construction laborers at locations with free unobstructed air flow compared to rates among household contacts. The present study was conducted in Chennai, located in south of India, which had 100877 cumulative confirmed SARS- CoV-2 cases on 1
st August 2020 and 121450 cumulative cases on 20
th August 2020 (20573 confirmed cases during the study period,
www.covid19india.org).
Methods
Between 1st and 20th August 2020, eighteen construction laborers diagnosed with symptomatic SARS-CoV-2 infection confirmed by RT-PCR of nasopharyngeal swab formed the index cases. Contacts were those who were exposed to the index case in the pre-symptomatic (2 days prior to symptom onset)1 or symptomatic period and satisfied at least one of the following: a) persons at residence of index case, b) persons at workplace who were exposed to the index case at close range (less than 6 feet) for ≥15 minutes, and c) persons outside the index case residence or workplace with close range contact ≥15 minutes who are traceable. All contacts were observed through daily telephonic monitoring. Contacts were questioned on duration of exposure with index case, mask use, loud talking and social distancing during exposure, details of dining and sharing of materials with index case. Contacts were considered to be compliant in mask use if they were wearing a mask covering nose and mouth during entire period of exposure. The contact was considered to be compliant with social distancing if a 6 feet distance was maintained all through the exposure period with the index case. Contacts who developed symptoms of SARS-CoV-2 infection were tested between day 3 and day 4 of symptom onset. Asymptomatic contacts were tested between day 6 and 10 from the last day of contact. Digital informed consent was obtained from participants. Ethics Committee for Observational studies, Community Research Network, Chennai approved the study.
Statistical comparisons between residential contacts and workplace contacts (open or closed environment) on exposure time with index case, dining together, loud talking, sharing of materials and confirmed SARS-CoV-2 infection were done using tests for comparison of means (t-test, analysis of variance) or proportions (Chi-square test, Z test), as appropriate. Relative risk of infection among contacts was calculated by standard statistical methods. A p value <0.05 was considered statistically significant.
Results
The contact tracing of 18 index cases (mean age 38.4 years; male, n=14) identified 514 contacts of which 496 consented for testing by RT-PCR of nasopharyngeal swab. Symptoms among index cases were fever (n=9), myalgia (n=12), cough (n=6), sore throat (n=4) and anosmia (n=4). Two of the index cases had prior diabetes mellitus and 16 had no pre-existing chronic medical illness. Four of the 18 index cases had contact history with SARS-CoV-2 infected persons; the source of infection for the remaining 14 could not be identified. All 18 index cases were living in homes with space less than 350 square feet with shared washroom and bedroom.
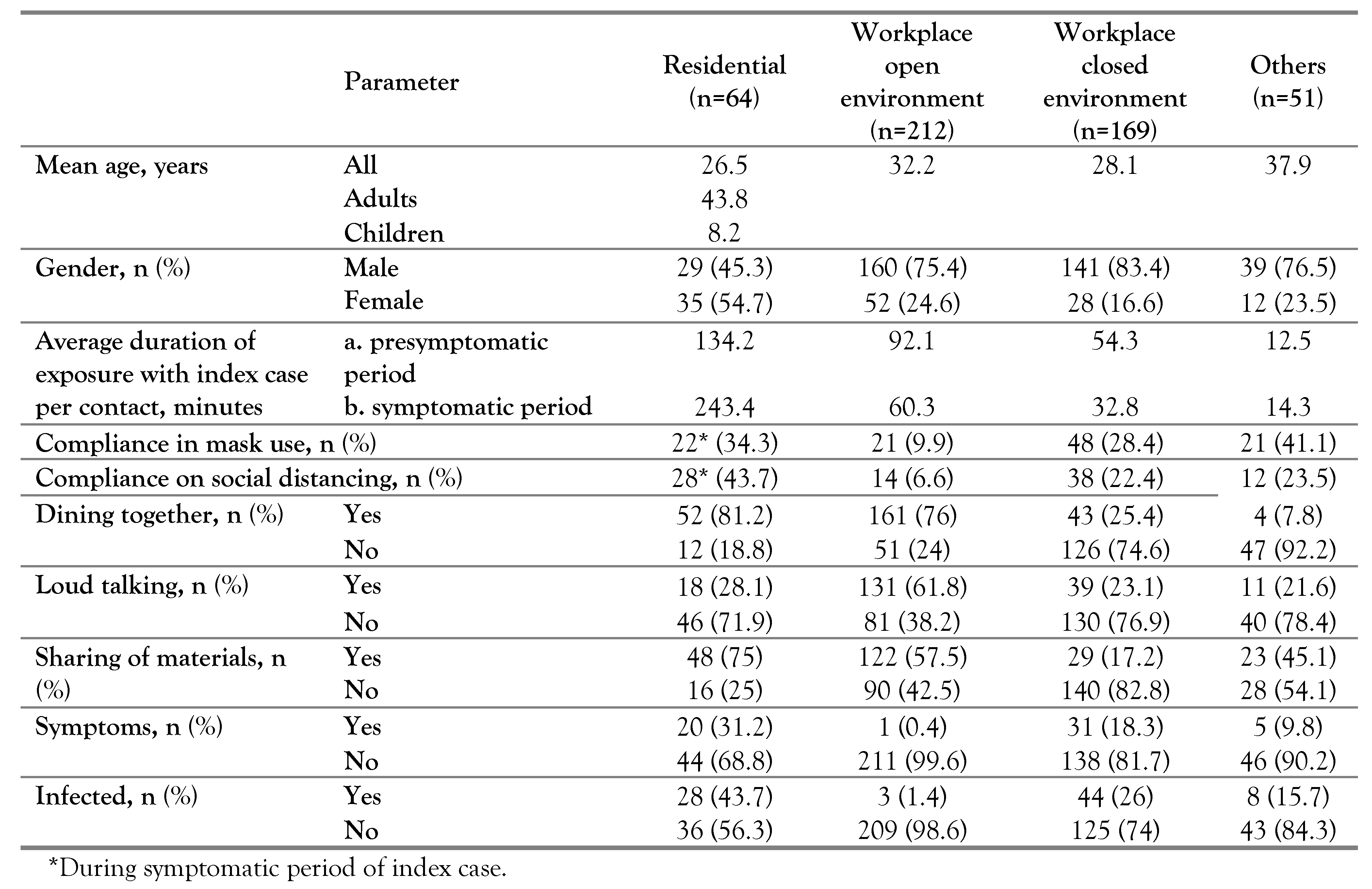
Table 1 describes the tracing observations among contacts. The mean exposure time of household contacts with index case was significantly higher than contacts at workplace (p<0.001); the frequency of dining together was not significantly different between household contacts and open environmental workplace contacts (p=0.38), while dining frequency of closed environmental work contacts was significantly lesser than open environmental contacts (p<0.0001) and household contacts (p<0.0001). The frequency of loud talking with index case was significantly higher among open environmental work contacts compared to household contacts (p<0.0001) and closed environmental work contacts (p<0.0001), while the frequency of loud talking was not significantly different between household and closed environmental work contacts (p=0.429). Frequency of sharing of material with index case among household contacts was significantly higher than open environmental (p=0.011) and closed environmental (p<0.0001) work contacts; the frequency of sharing material was higher in open than closed environmental work contacts (p=0.011). The secondary transmission rate was maximum among household contacts (n=28, 43.7%) followed by contacts at closed environment at workplace (n=44, 26%), traceable other contacts (n=8, 15.7%) and contacts at open environment at workplace (n=3, 1.4%). Open environment were tea shops, premises of building under construction and partially constructed building with only roof and beam with free non- obstructed air flow. Mask wearing was mandatory for the public in Chennai from April 13
th 2020 and index cases as well as contacts wore mostly cloth mask.
Relative risk of SARS-CoV-2 infection among household contacts was 30.9 (CI 9.7-98.3, p<0.001) compared to open environmental work contacts and 1.68 (CI 1.15-2.44, p=0.006) compared to closed environmental work contacts. Relative risk was 18.3 (CI 5.8-58.2, p<0.001) among closed environmental work contacts compared to open environmental work contacts.
Eight of the eighteen index cases required hospitalization. Four of the eight hospitalized index cases required oxygen support (3 noninvasive and 1 mechanical ventilation). Eighteen of the 83 secondary cases (9-household, 1-open environmental, 6-closed environmental, 2- others) required hospitalization. Six of 18 secondary cases required oxygen support (5- noninvasive and 1-mechanical ventilation). One index who was aged 45 years with prior diabetes mellitus and one secondary case, aged 62 years with multiple chronic illness who was a household contact (both requiring mechanical ventilation) died. Further treatment details of hospitalized patients could not be obtained. Those who were not hospitalized (n=75) received treatment from their metropolitan public health clinician (ivermectin-62, hydroxychloroquine-22, zinc and vitamin C-44).
Discussion
The study observed a low secondary attack rate (1.4%) among contacts of construction laborers at locations with free air flow compared to a 30-fold higher rate among households. Studies which report secondary attack rate have categorized the contacts as households, non-households, workplace, pre-symptomatic phase and symptomatic phase [
3,
4,
5]. There is lack of reporting on transmission with reference to ventilation of the exposure locations. Furthermore, studies on contact tracing do not report duration of contact with index case, although it appears to influence transmission as evidenced by higher rates among household contacts [
5]. While 75% of open air location contacts dined together (when masking does not happen) with the index case; it did not result in higher transmission compared to 85% of household contacts who dined together with index case at home. Improvement in ventilation practices at healthcare locations is known to decrease risk of transmission [
6]. Improvement in ventilation in the community can be done by allowing free flow of air in locations where large gatherings are expected like places of worship, restaurants, entertainment, schools, and colleges given the fact that these locations present a high risk for transmission [
7,
8].
Conclusions
Our study emphasizes the fact that free air flow has the ability to dilute or probably blow away the virus particles and lowers the transmission risk substantially.
Author Contributions
VS: study design, data acquisition, analysis, write-up, final approval. EB: concept, study design, data acquisition, analysis, revision of manuscript, final approval). All authors read and approved the final version of the manuscript.
Conflicts of interest
Both authors – none to declare.
References
- Gandhi, R.T.; Lynch, J.B.; Del Rio, C. Mild or moderate COVID-19. N Engl J Med. 2020, 383, 1757–1766. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Zhang, B.; Lu, J.; et al. Characteristics of household transmission of COVID-19. Clin Infect Dis. 2020, 71, 1943–1946. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.Y.; Jian, S.W.; Liu, D.P.; et al. Contact tracing assessment of COVID-1 transmission dynamics in Taiwan and risk at different exposure periods before and after symptom onset. JAMA Intern Med. 2020, 180, 1156–1163. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Ma, W.; Zheng, X.; Wu, G.; Zhang, R. Household transmission of SARS-CoV-2. J Infect. 2020, 81, 179–182. [Google Scholar] [CrossRef] [PubMed]
- Meyerowitz, E.A.; Richterman, A.; Gandhi, R.T.; Sax, P.E. Transmission of SARS-CoV-2: a review of viral, host, and environmental factors. Ann Intern Med. 2021, 174, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Morawska, L.; Tang, J.W.; Bahnfleth, W.; et al. How can airborne transmission of COVID-19 indoors be minimised? Environ Int. 2020, 142, 105832. [Google Scholar] [CrossRef] [PubMed]
- James, A.; Eagle, L.; Phillips, C.; et al. High COVID-19 attack rate among attendees at events at a church - Arkansas, March 2020. MMWR Morb Mortal Wkly Rep. 2020, 69, 632–635. [Google Scholar] [CrossRef] [PubMed]
- Qian, H.; Miao, T.; Liu, L.; Zheng, X.; Luo, D.; Li, Y. Indoor transmission of SARS-CoV-2. Indoor Air. 2020. [Google Scholar] [CrossRef]
Table 1.
Characteristics of secondary contacts.
Table 1.
Characteristics of secondary contacts.