Introduction
Influenza is a preventable seasonal disease with an epidemic character that has a significant negative impact on a yearly basis, on large population groups, healthcare systems, and countries’ economic performance, and reliable information regarding its burden throughout the world is still posing a major problem [
1]. According to the World Health Organization (WHO), the global influenza epidemic affects between 5-10% of the adult population annually, and around 20-30% of children [
2]. Even though starting with 2011 the case definition for influenza was updated [
3], and in 2015 the WHO issued a methodology for the estimation of disease burden associated with seasonal influenza [
4], there is still a high heterogeneity in reporting the results [
1,
5,
6]. The majority of influenza burden studies performed in the European setting have so far been concentrated on Western European countries rather than Central and Eastern European countries. Currently, for Romania, there are only two published studies regarding the burden of influenza, one taking into account the population 65 years and above [
7], and the other one, the entire population at risk of developing influenza-like illness and severe acute respiratory infections, based on national surveillance data [
8]. The current study attempts to measure the burden of influenza on five influenza seasons (2014/2015 -2018/2019), by employing a different methodology compared to the previous studies, and using the morbidity data reported at the national level in the health administrative databases for three levels of care: general practitioner (GP) offices, emergency departments and hospitals, as opposed to the existing studies that used surveillance network data only.
According to Preaud and colleagues [
9], improving the vaccination rate in the European Union (EU) population from about 45% to 75%, for at-risk groups, would have a significant annual impact in diminishing the negative outcomes of this disease, from both a public health and economic perspective.
In Romania, the influenza vaccination rate has steadily decreased from 49.4% during the 2008/2009 season to 7.4% during the 2014/2015 season in the age group of 65 years and above [
10]. During the last influenza seasons, the evolution of the vaccination rate for this age group has been variable and for the 2018/2019 season it reached 20.9%.[
11,
12] Also, regarding the influenza vaccination rate in the general population, although it has increased considerably for the past influenza seasons, it still did not exceed 7%[
11,
12] in the analyzed period and this trend impacts directly the burden of influenza in Romania.
Study Objective
The study aims to evaluate the burden of influenza associated illness in Romania by using information extracted from the morbidity and mortality healthcare administrative databases at national level in contrast with previous studies that were using information and estimation from the surveillance data network. The study also aims to cover the entire spectrum of burden of influenza associated illness by estimating data about morbidity, mortality and premature death.
Methods
The raw aggregated data regarding the number of new cases, hospitalization episodes and number of deaths were provided by the Statistical Center of the National Institute of Public Health (NIPH)[
12] from national medical administrative databases for morbidity and mortality, covering all medical providers in Romania. Datasets were received in aggregated format for different providers and periods as follows: new cases at GP level, for entire seasons 2014/15 to 2018/19, new cases at hospital level and deaths for the entire seasons 2014/15 to 2017/18, and for the first part of the season 2018/2019 (until the end of December 2018). For the rest of the season 2018/19, (January-May 2019), values were estimated accordingly. The approach used in the current paper to estimate the number of cases attributable to influenza is described below.
For the total number of reported GP cases/season and the corresponding incidence, first, we counted all cases reported by general practitioners with the following diagnoses: Influenza with identified virus (J10.x), and Influenza with unidentified influenza virus (J11.x). Since a number of initial influenza cases advance to more severe respiratory disease (infections) such as pneumonia, using only the influenza reported cases by specific diagnosis codes would determine an underestimation of the burden of influenza associated illness. Thus, using the influenza positivity rate (IPR), computed from WHO-FluNet[
13] data, we extracted all cases reported by GPs with the diagnosis Unspecified viral pneumonia (J12.x), and Other pneumonias with unspecified organisms (J18.x), as a share equal to IPR.
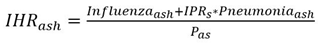
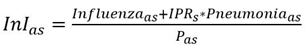
The GP incidence attributable to influenza (
InI) in a season
s for an age group
a was computed using the relation:
Where season s starts from 2014/2015 to 2018/19 and age group a represents the 0-4, 5-19, 20-49, 50-64 and 65 and above age groups.
The P
as represents the resident population for age group
a and season
s. The values for the population were available at the National Institute of Statistics, TEMPO Database [
14].
For the period analyzed, the IPR for Romania varied by season, starting with 0.540 for 2014/15 season, followed by 0.487 in 2015/16, 0.432 in 2016/17, 0.563 in 2017/18 and 0.478 in 2018/19.
The data for the number of
presentations to Emergency Departments (EDs) attributable to influenza was requested from the Romanian Department for Emergency Situations for the all seasons analyzed. However, raw data was provided only for seasons 2017/18 to 2018/19. The dataset comprised cases at national level by season regarding the attendance to emergency units by persons with influenza-like illness symptomatology according to ECDC criteria[
15] (E-ILIs). Data for unavailable seasons were estimated due to absence of raw dataset.
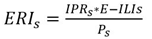
The number of Emergency Department presentations attributable to influenza (EAI) were calculated as IPR * E-ILIs for each season
s. Using this assumption, the emergency rates attributable to influenza (ERI) by season
s, becomes:
The decomposition of ERIs by age group was made, using as proxy such as the structure of cases by age group from the hospital morbidity database.
A certain number of influenza cases do not seek care at healthcare providers. Therefore, these are considered non-consulting cases. The non-consulting cases are estimated using the probability
p to consult a GP. Because no data are available for Romania, we used the value proposed by Carrat and colleagues [
16], p=0.49. Then, the non-consulting cases were computed as
p/(1-p)*GP cases.
Using all these categories of patients with influenza attributable disease we computed the total number of attributable influenza cases (TCI) per season, for each age group using the relation:
TCI = non-consulting cases + GPs reported cases + presentation to EDs. Therefore, by reporting to the resident population Pas, the total influenza attributable disease rate was obtained. In order to avoid duplication of cases, hospitalizations were accounted for separately, due to the fact that persons admitted in the hospital are counted already either at EDs before admission or at GPs, before admission (referral to hospital) or after discharge (medical leave or/and reimbursed prescription at GPs).
For the inpatient and day-hospital care, we counted all the episodes discharged with the primary diagnosis according to ICD-10 any of the following: J10.0 Influenza due to other identified influenza virus with pneumonia; J10.1 Influenza due to other identified influenza virus with other respiratory manifestations; J10.2 Influenza due to other identified influenza virus with gastrointestinal manifestations; J10.8 Influenza due to other identified influenza virus with other manifestations; J11.0 Influenza due to unidentified influenza virus with pneumonia; J11.1 Influenza due to unidentified influenza virus with other respiratory manifestations; J11.2 Influenza due to unidentified influenza virus with gastrointestinal manifestations; J11.8 Influenza due to unidentified influenza virus with other manifestations.
Then using the IPRs, defined in the previous paragraph, we extracted from all pneumonia discharged cases (J12.x and J18.x), for each season, a share equal to IPR. Based on previous seasons data, 30% of inpatient hospitalization episodes, as well as 25% of day-hospitalizations episodes attributable to influenza, occurred during the first part of the seasons (October-December). In order to compute the total number of episodes for the entire season 2018-2019, the available number of episodes were divided by 0.3, respectively by 0.25, and summed accordingly.
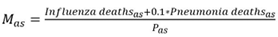
The attributable influenza hospitalization rate (IHR) for an age group
a, type of hospitalization,
h and season
s becomes:
For the mortality rate, we counted all deaths reported in a season with the main cause being any of
J10.0 to
J11.8 (influenza). According to other studies
,[
17,
18] 10% of deaths with the main cause pneumonia (any of the ICD-10 codes {
J12.0; J12.9} ꓴ {
J18.0; J18.9}) could be attributable to influenza. The estimation for the number of deaths for the missing season 2018/19 was done as follows:
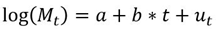
For age groups [0-4 years old] and [65+] the number of deaths has a trend in the last seasons. For both age groups the models are:
where (
Mt) = number of deaths in the season t, t=1..10 seasons,
ut = error term.
Then, using data from the last 10 seasons, the parameters for each model were estimated. For the other age groups, [5-19], [20-49] and [50-64], the number of deaths were computed taking the mean for the last seasons, since no trend was identified.
Then the mortality rates are
In both (3) and (4) relations, a represents the age group and s the seasons, the same as described for the relation (1).
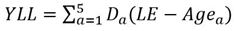
The non-discounted value of the years of life lost (YLL) due to premature death attributable to influenza complications was calculated using the relation:
Where
a = the age group,
Agea = mean of the age group
a,
Da = number of deaths in the interval and LE=74 years, the life expectancy at birth in Romania [
19]. Then, the average YLL per death was also derived [
20].
Results
Most cases of influenza infections reported by GPs for the analyzed period were found in children, followed by cases in the age group 65 years and above that had a number of cases very close to that occurring in the age groups 20-49 and 50-64 years. In the age group 0-4 years, the incidence of influenza was 4 times higher than in the age group over 65 years. The lowest influenza incidence reported by GPs was found in the adults 20-49 years, with a value five times smaller than that for the 0-4 years age group. According to current estimation, the total number of new cases reported by GPs, per season, varied in the analyzed period from a minimum of 108,412 cases in season 2016/17 to a maximum of 181,541 cases, in 2018/19. During the entire period the average number of cases per season was 146,178 (
Table 1).
Except for the 0-4 year age group, which had an increasing trend of presentations at EDs for the analyzed period, with the highest values recorded (2,500-4,000 cases/100,000 persons), the other age groups had relatively constant presentation rates during the analyzed period, and at values up to 5-10 times lower than the values recorded for the age group 0-4 years (
Table 2).
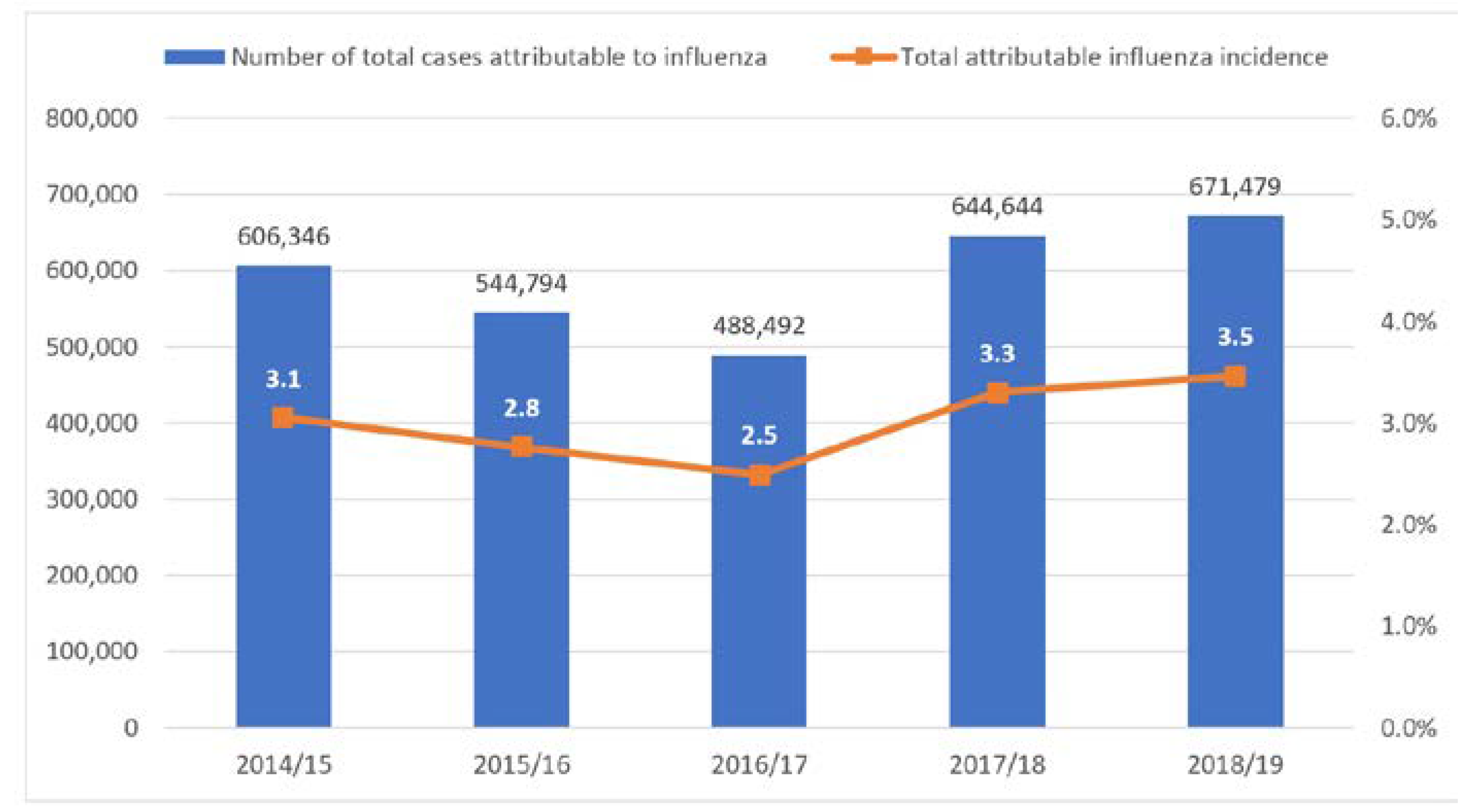
The total number of cases of influenza attributable disease reached, on average, 591,151 cases/season, with a maximum of 671,479 cases estimated for the season 2018/19 (
Figure 1). This implies that in average around 3% of the Romanian population is estimated to develop an influenza attributable disease in a season.
Hospital admission rates fluctuated from one season to another. For inpatient care, in the last five seasons the range was 153 to 220 influenza attributable disease episodes per 100,000 persons/season. The hospitalization rates in day-hospital care were significantly lower, values did not reach more than 91 influenza attributable disease episodes per 100,000 persons/season in the studied period. Infections attributable to influenza virus were responsible for 33,000 to 45,000 inpatient hospitalizations in Romania every season.
Children aged 0-4 years represented the most frequent age group hospitalized in inpatient care for influenza infections, with an average number of 1000 episodes of hospitalization per 100,000 persons/season. The second age group most frequently hospitalized was represented by 65 years and older, with an average number of 250 episodes of continuous hospitalization per 100,000 persons/season.
The most frequent, day-hospitalizations occurred in the 0-4 years age group, with a rate of ~150-214 episodes/100,000 persons. Persons from the age groups 5-19 years and 50-64 years had similar rates during the seasons 2014/15-2016/17, with values ranging from 75 to 115 episodes/100,000 persons. In the last two influenza season evaluated, the persons in the age group 65 and above had an important increase in the day-hospitalization episodes, the correspondent day-hospitalization rate for this age group doubled its value, compared with the beginning of the period. The lowest number of cases during the entire period of analysis were those from the 20-49 years age group. The day-hospitalization rate of this age group was ~3 times lower than the maximum rate observed.
In terms of hospitalization, there were 33,000 to 45,000 cases per season, representing ~7% from the total estimated number of influenza cases/season (
Table 3).
The estimations showed a negative trend for the 0-4 age group, log(Mt) = 1.779 - 0.040 * t and for the 65+ age group, log(Mt) = 2.250 + 0.034 * t, respectively. Then, a number of 22 deaths were estimated for the first group and 428 for the last one. Summing the estimated deaths from all age groups, a total number of 625 deaths were counted for the entire 2018/19 season.
An average of 577 deaths per season was estimated for the period 2014/15-2018/19 with a maximum of 664 deaths in season 2017/18.
The crude mortality rate for influenza infections, although low, increased steadily for the analyzed period and had values between two and three deaths per 100,000 persons.
The highest mortality rate due to infections attributable to influenza was found in the elderly group (65+). Here the values were 4 to 5 times higher than the values attributable to the 50-64 age group, and about 50 times higher than those of the 5-49 age group. Also, the mortality rate for the elderly group had an increasing trend, while for the other groups the rates were stable, in the analyzed period. A slightly decreasing trend of the mortality rate could be observed for the 0-4 years age group: in the 2014/15 season the rate was 3.1 deaths at 100,000 persons and in the last analyzed season it reached 2.2 deaths per 100,000 persons (
Figure 2).
Based on the National Institute of Statistics mortality data[
14] and the current computations, it was estimated that the number of deaths attributable to influenza represents in a season almost 0.25% of all causes of deaths, registered in a year in Romania.
During the analyzed seasons, an average of 6,882 potential years of life lost (PYLL)/season were estimated due to premature death attributable to influenza. This value represents an average of 35.2 years lost/100,000 persons.
Discussion
In the analyzed period a sinuous tendency may be seen for most of the indicators. This tendency suggests the alternance of high-low intensity of influenza seasons, and this pattern might be influenced by the inconstant vaccination rate especially for risk groups, and the predominant strains circulating in a season.
According to the methodology used in this study, the incidence of influenza attributable disease varied between 250-350 cases per 100,000 persons for the analyzed period. As a comparison, the incidence of influenza-like illness reported from the sentinel network throughout the country for the same period was much lower and highly variable, with values between 16 and 120 cases reported per 100,000 persons [
19].
The burden of influenza attributable illness in Romania appears to be ten times higher than the one reported by Gefenaite in 2017 [
8]. One of the main differences in the estimation of this final value is linked with the methodology used in this study, as compared with the one used in the study by Gefenaite, which was based on sentinel network reported events only.
Further qualitative studies should be employed in order to have a better understanding of the response behavior of persons working in the sentinel network. Also, another suggestion might be to include some EDs in the sentinel network for influenza.
A high variation between the analyzed age groups was observed. In particular, the age groups 0-4 and 65 and above were the highest at-risk groups for influenza attributable disease.
The most affected age group in terms of influenza attributable morbidity was 0-4 years old, both in this research as well as in the studies by Gefenaite et al [
8]. and Meerhoff et al [
21]. In line with the results achieved by Cromer al. (2014) for England [
22], in terms of hospital admission, the 0-4 age group had the leading rate, while the 65 and above group followed it. The highest hospitalization rates for the age groups 0-4 and 65 were described also by Mattias et al. (2016)[
23] for UK, but here, the leading group found was the elderly.
One possible hypothesis for the high number of cases from the age group 0-4 is the fact that this group had the lowest vaccination rate for influenza (CNSCBT) [
11]. Also, it is customary for hospitals to admit even mild cases particularly for the age group 0-4 years old, either for better monitoring or for parents’ comfort.
The most affected group in terms of influenza attributable mortality was the age group 65 years and above, the same leading age group being reported in the studies by Kovacs et al. from 2014 [
7], and by Mattias et al. (2016) [
23].
A potential hypothesis is that mortality attributable to influenza is underreported, mostly by the lack of evidence of the causal etiologic agent, also by mentioning the most frequent acute complication (e.g., acute respiratory failure, bronchopneumonia, sepsis, cardiac arrest) as the primary cause of death.
Moreover, beside the different methodological approach, the sentinel network might not be able to capture statistically representative data in order to provide a more accurate estimation of incidence of influenza attributable illnesses.
While studies from other countries[
24] show benefits in terms of morbidity and mortality reduction in case of higher vaccination coverage, the increase of low vaccination rates registered in Romania may be a challenge. According to the Organization for Economic Co-operation and Development (OECD) [
25], influenza mortality may be avoided by preventative measures, one of them being vaccination.
 (2)
(2)