Contribution of Essential Oils to the Fight against Microbial Biofilms—A Review
Abstract
1. Introduction
2. Methods
3. Discussion
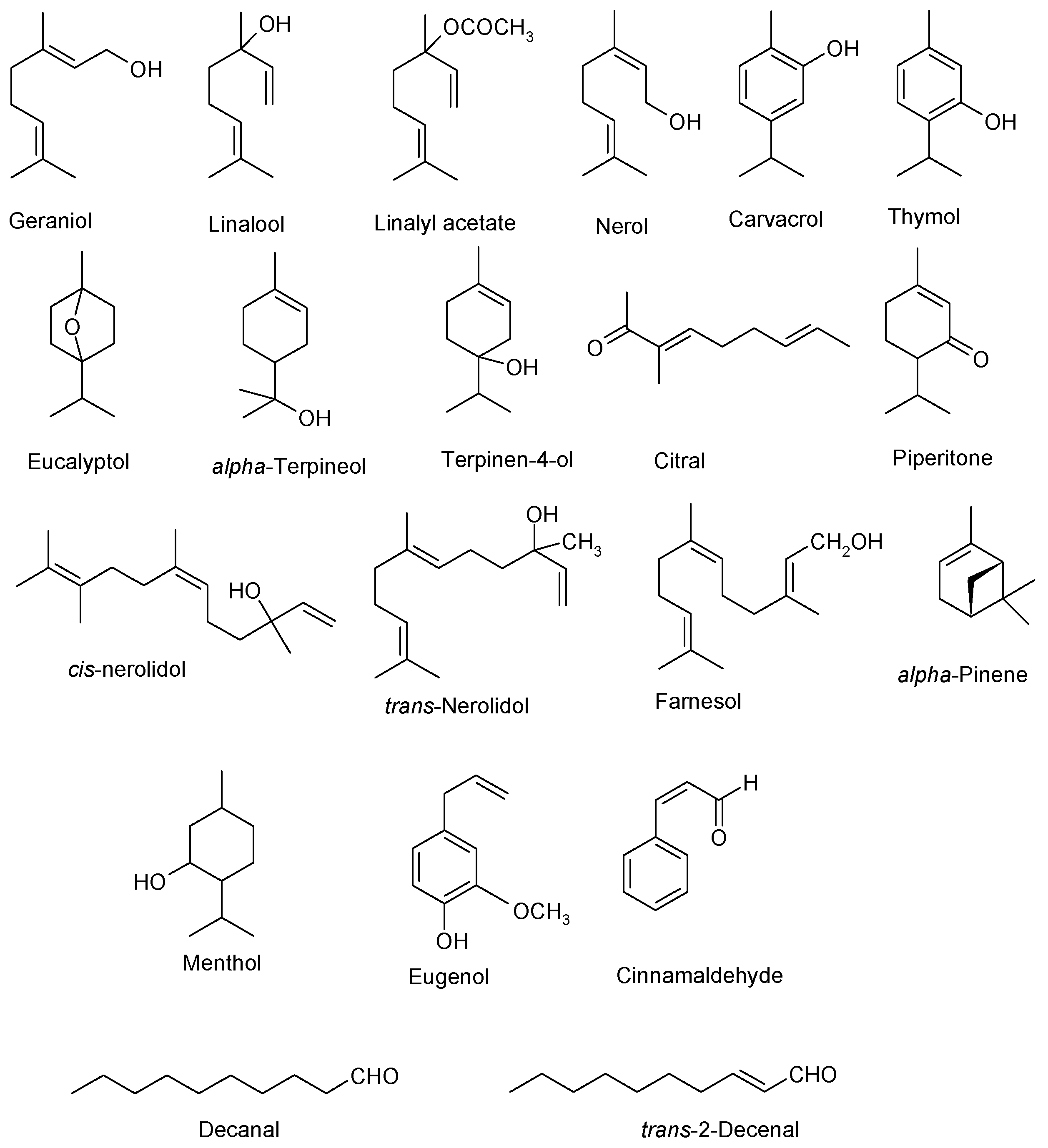
3.1. EOs Mechanism of Action as Antibiofilm Agents
3.2. Disadvantages EOs Administration
3.3. EOs Formulation
3.4. EOs as Antibiofilm Agents
3.5. EOs Used in Dentistry
3.6. EOs in Chronic Wound Infection Treatment
3.7. EOs in the BAIs Treatment
3.8. EOs Used in Food Industry
3.9. EOs as Air Disinfectants
3.10. Nanoparticles with EOs Used in Controlling and Preventing Infections
| Latin Name of Plant Source of EO | Main Components of EO | Microbial Strain That Produces Biofilms on Which the EO Has Been Tested | Reference |
|---|---|---|---|
| Boswellia papyrifera Boswellia rivae | n-octyl acetate, octanol, limonene, a-pinene, verticilla-4 (20), 7,11-triene, acetate, incensole | Staphylococcus epidermidis S. aureus C. albicans | [31] |
| Butia capitata | capric, caprylic, lauric, linoleic, myristic, oleic, palmitic, stearic acids | Aciduric bacteria Lactobacilli Streptococcus mutans | [78] |
| Cananga odorata subsp. Genuine (ylang-ylang oil) | p-cresyl methyl ether, linalool, geranyl acetate, geraniol, eucalyptol | S. aureus Klebsiella pneumoniae | [109] |
| Cinnamomum aromaticum (Cassia oil) | cinnamaldehyde, eugenol, linalool | P. aeruginosa P. putida S. aureus | [7] |
| Cinnamomum zeylanicum | e-cinnamaldehyde | Salmonella Saintpaul | [102] |
| Citrus hystrix | citronellal | S. sanguinis S. mutans | [75] |
| Coriandrum sativum | decanal, trans-2-decenal, 2-decen-1-ol, cyclodecane | C. albicans C. tropicalis C. krusei C. dubliniensis C. rugosa | [82] |
| Cupressus sempervirens | α-pinene, α-terpinolene, δ-3-carene, limonene | K.pneumoniae | [12] |
| Curcuma longa | curlone, trans-β-elemenone, germacrone, β-sesquiphellandrene, α-turmerone, αr-turmerone, α-zingiberene | S. mutans | [77] |
| Cymbopogon citratus (lemongrass oil) | geranial, neral, myrcene | C. albicans C. tropicalis C. glabrata C. krusei P. gingivalis P. intermedia Aeromonas hydrophila | [89,90,91] [73] [11] |
| Eucalyptus camaldulensis | eucalyptol | Porphyromonas gingivalis Actinobacillus actinomycetemcomitans Fusobacterium nucleatum S. mutans S. sobrinus C. albicans | [73] |
| Eugenia caryophyllata (Syzygium aromaticum) (clove oil) | biflorin, caryophyllene oxide, eugenol, eugenyl acetate, ellagic acid, gallic acid, kaempferol, myricetin, oleanolic acid, rhamnocitrin | C. albicans C. tropicalis C. glabrata C. krusei P. gingivalis P. intermedia | [73,89,90,91] |
| Laurus nobilis | acetate, eucalyptol, linalool, methyleugenol, α-terpinyl | S. epidermidis | [93,94] |
| Lavandula angustifolia (lavender essential oil, LEO) | camphor, caryophyllene, eucalyptol, lavendulyl acetate, limonene, linalool, linalyl acetate, cis-ocimene, 3-octanone, a-pinene, transocimene, terpinen-4-ol | S. aureus E. coli | [5] |
| Matricaria chamomilla (Chamomile EO) | (E)-β-farnesene α-bisabolol oxide A | S. mutans S. sobrinus Lactobacillus sp. | [71] |
| Melaleuca alternifolia (tea tree oil, TTO) | α-pinene, p-cymene, eucalyptol,terpinen-4-ol, γ-terpinene,α-terpinene, terpinolene | S. mutans | [52] |
| Proteus mirabilis | [87] | ||
| Melissa officinalis (Melissa essential oil, MEO or lemon balm) | citrals (geranial + neral, citronellal, limonene, geraniol, β-caryophyllene, β-caryophyllene oxide, and germacrene D | S. aureus E. coli | [5] |
| Mentha piperita | menthofuran, menthol, menthyl acetate, eucalyptol, menthone, α-pinene, sabinene, β-pinene | C. albicans C. dubliniensis | [34] |
| Mentha spicata | carvone, trans-carveol, myrcenecarvyl-acetate-Z | S. mutans | [73,98] |
| Ocimum gratissimum | eugenol, 1,8-cineole | S. aureus E. coli | [13] |
| Origanum vulgare (oregano oil) | carvacrol, thymol, γ-terpinene, p-cymene | S. aureus S. epidermidis | [55] |
| Pogostemon cablin (patchouli essential oil) | α-guaiene, β-caryophyllene, δ-cadinene, pogostol, (‒)-patchoulol, seychellene, α- and β-patchoulene | S. aureus K. pneumoniae | [109] |
| Rosmarinus officinalis (rosemary oil) | eucalyptol, alpha-pinene, camphor, verbenone, borneol | S. sobrinus | [73] |
| Satureja thymbra | carvacrol, thymol, p-cymene | S. simulans Lactobacillus fermentum P. putida Salmonella enterica Listeria monocytogenes | [6] |
| Thymbra capitata | carvacrol, γ-terpinene, p-cymene | Candida albicans C. glabrata C. tropicalis C. parapsilosis C. guilliermondii | [44] |
| Thymus vulgaris (thyme oil) | eucalyptol, camphor | A. hydrophila | [11] |
| Vanilla planifolia (vanilla oil) | ethylvanillin, 4-hydroxybenzaldehyde, methyl anisate, 4-hydroxybenzyl methyl ether, piperonal, vanillic acid, vanillin | S. aureus K. pneumoniae | [109] |
| Latin Name of Plant Source of EO | The Support (Medical Device) on Which the Biofilm Was Studied | Reference |
|---|---|---|
| Baccharis dracunculifolia Mentha spicata Melaleuca alternifolia | Dental biofilm | [76] [73] [52] |
| Cananga odorata subsp. genuine Pogostemoncablin Vanilla planifolia | Catheter | [109] |
| Cupressus sempervirens | Intravenous infusion tube | [12] |
| Cymbopogon citratus Thymus vulgaris Saturejathymbra | Stainless steel coupons | [11] [11] [6] |
| Eugenia caryophyllata (Syzygiumaromaticum) Thymus vulgaris | Soft contact lenses | [33] |
| Lavandula angustifolia Melissa officinalis Melaleuca alternifolia | Urological catheter, infusion tube, surgical mesh | [5] |
| Melaleuca alternifolia | Catheter-associated urinary tract infections | [87] |
| Cochlear implant | [86] | |
| Silicone tympanostomy tubes | [85] |
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rodney, M.D.; Costerton, J.W. Biofilms: Survival Mechanisms of Clinically Relevant Microorganisms. Clin. Microbiol. Rev. 2002, 15, 167–193. [Google Scholar]
- Mohammadi, Z.; Palazzi, F.; Giardino, L.; Shalavi, S. Microbial biofilms in endodontic infections: An update review. Biomed. J. 2013, 36, 59–70. [Google Scholar] [CrossRef] [PubMed]
- Lazăr, V.; Chifiriuc, M.C. Medical significance and new therapeutical strategies for biofilm associated infections. Roum. Arch. Microbiol. Immunol. 2010, 69, 125–138. [Google Scholar] [PubMed]
- Glinel, K.; Thebault, P.; Humblot, V.; Pradier, C.M.; Jouenne, T. Antibacterial surfaces developed from bio-inspired approaches. Acta Biomater. 2012, 8, 1670–1684. [Google Scholar] [CrossRef]
- Budzyñska, A.; Wiêckowska-Szakiel, M.; Sadowska, B.; Kalemba, D.; Rózalska, B. Antibiofilm Activity of Selected Plant Essential Oils and their Major Components. Pol. J. Microbiol. 2011, 60, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Chorianopoulos, N.G.; Giaouris, E.D.; Skandamis, P.N.; Haroutounian, S.A.; Nychas, G.J.E. Disinfectant test against monoculture and mixed-culture biofilms composed of technological, spoilage and pathogenic bacteria: Bactericidal effect of essential oil and hydrosol of Satureja thymbra and comparison with standard acid–base sanitizers. J. Appl. Microbiol. 2008, 104, 1586–1596. [Google Scholar] [CrossRef]
- Kavanaugh, N.L.; Ribbeck, K. Selected Antimicrobial Essential Oils Eradicate Pseudomonas spp. and Staphylococcus aureus Biofilms. Appl. Environ. Microbiol. 2012, 78, 4057–4061. [Google Scholar] [CrossRef] [PubMed]
- Burt, S. Essential oils: Their antibacterial properties and potential applications in foods—A review. Int. J. Food Microbiol. 2004, 94, 223–253. [Google Scholar] [CrossRef] [PubMed]
- Bakkali, F.; Averbeck, S.; Averbeck, D.; Idaomar, M. Biological effects of essential oils—A review. Food Chem. Toxicol. 2008, 46, 446–475. [Google Scholar] [CrossRef]
- Saviuc, C.M.; Drumea, V.; Olariu, L.; Chifiriuc, M.C.; Bezirtzoglou, E.; Lazăr, V. Essential Oils with Microbicidal and Antibiofilm Activity. Curr. Pharm. Biotechnol. 2015, 16, 137–151. [Google Scholar] [CrossRef]
- Millezi, A.F.; das Graças Cardoso, M.; Alves, E.; Piccoli, R.H. Reduction of Aeromonas hidrophyla biofilm on stainless stell surface by essential oils. Braz. J. Microbiol. 2013, 44, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Selim, S.A.; Adam, M.E.; Hassan, S.M.; Albalawi, A.R. Chemical composition, antimicrobial and antibiofilm activity of the essential oil and methanol extract of the Mediterranean cypress (Cupressus sempervirens L.). BMC Complement. Altern. Med. 2014, 14, 179. [Google Scholar] [CrossRef]
- Melo, R.S.; Albuquerque Azevedo, Á.M.; Gomes Pereira, A.M.; Rocha, R.R.; Bastos Cavalcante, R.M.; Carneiro Matos, M.N.; Ribeiro Lopes, P.H.; Gomes, G.A.; Soares Rodrigues, T.H.; Santos, H.S.d.; et al. Chemical Composition and Antimicrobial Effectiveness of Ocimum gratissimum L. Essential Oil Against Multidrug-Resistant Isolates of Staphylococcus aureus and Escherichia coli. Molecules 2019, 24, 3864. [Google Scholar] [CrossRef] [PubMed]
- Tang, C.; Chen, J.; Zhang, L.; Zhang, R.; Zhang, S.; Ye, S.; Zhao, Z.; Yang, D. Exploring the antibacterial mechanism of essential oils by membrane permeability, apoptosis and biofilm formation combination with proteomics analysis against methicillin-resistant Staphylococcus aureus. Int. J. Med. Microbiol. 2020, 5, 151435. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Horváth, B.; Šafranko, S.; Jokić, S.; Széchenyi, A.; Kőszegi, T. Antimicrobial Activity of Chamomile Essential Oil: Effect of Different Formulations. Molecules 2019, 24, 4321. [Google Scholar] [CrossRef] [PubMed]
- Fde, O.P.; Mendes, J.M.; Lima, I.O.; Mota, K.S.; Oliveira, W.A.; Ede, O.L. Antifungal activity of geraniol and citronellol, two monoterpenes alcohols, against Trichophyton rubrum involves inhibition of ergosterol biosynthesis. Pharm. Biol. 2015, 53, 228–234. [Google Scholar]
- Ortega-Ramirez, L.A.; Gutiérrez-Pacheco, M.M.; Vargas-Arispuro, I.; González-Aguilar, G.A.; Martínez-Téllez, M.A.; Ayala-Zavala, J.F. Inhibition of Glucosyltransferase Activity and Glucan Production as an Antibiofilm Mechanism of Lemongrass Essential Oil against Escherichia coli O157:H7. Antibiotics 2020, 9, 102. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Vörös-Horváth, B.; Bencsik, T.; Micalizzi, G.; Mondello, L.; Horváth, G.; Kőszegi, T.; Széchenyi, A. Antimicrobial Activity of Different Artemisia Essential Oil Formulations. Molecules 2020, 25, 2390. [Google Scholar] [CrossRef]
- Pina-Barrera, A.M.; Alvarez-Roman, R.; Baez-Gonzalez, J.G.; Amaya-Guerra, C.A.; Rivas-Morales, C.; Gallardo-Rivera, C.T.; Galindo-Rodriguez, S.A. Application of a multisystem coating based on polymeric nanocapsule containing essential oil of Thymus vulgaris L. to increase the shelf life of table grapes (Vitis vinifera L.). IEEE Trans. NanoBioscience 2019, 18, 549–557. [Google Scholar] [CrossRef]
- Alizadeh Behbahani, B.; Tabatabaei Yazdi, F.; Vasiee, A.; Mortazavi, S.A. Oliveria decumbens essential oil: Chemical compositions and antimicrobial activity against the growth of some clinical and standard strains causing infection. Microb. Pathog. 2018, 114, 449–452. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.; Shao, Y.-L.; Tang, Y.-J.; Zhou, W.-W. Antifungal Activity of Essential Oil Compounds (Geraniol and Citral) and Inhibitory Mechanisms on Grain Pathogens (Aspergillus flavus and Aspergillus ochraceus). Mol. J. Synth. Chem. Nat. Prod. Chem. 2018, 23, 2108. [Google Scholar] [CrossRef]
- Inouye, S.; Tsuruoka, T.; Uchida, K.; Yamaguchi, H. Effect of Sealing and Tween 80 on the Antifungal Susceptibility Testing of Essential Oils. Microbiol. Immunol. 2001, 45, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Abarca, R.L.; Rodríguez, F.J.; Guarda, A.; Galotto, M.J.; Bruna, J.E. Characterization of beta-cyclodextrin inclusion complexes containing an essential oil component. Food Chem. 2016, 196, 968–975. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Li, B.; Si, H.; Lin, L.; Chen, L. Release characteristics and antibacterial activity of solid state eugenol/β-cyclodextrin inclusion complex. J. Incl. Phenom. Macrocycl. Chem. 2011, 71, 207–213. [Google Scholar] [CrossRef]
- Astray, G.; Gonzalez-Barreiro, C.; Mejuto, J.C.; Rial-Otero, R.; Simal-Gándara, J. A review on the use of cyclodextrins in foods. Food Hydrocoll. 2009, 23, 1631–1640. [Google Scholar] [CrossRef]
- Zhou, Y.; Sun, S.; Bei, W.; Zahi, M.R.; Yuan, Q.; Liang, H. Preparation and antimicrobial activity of oreganoessential oil Pickering emulsion stabilized by cellulose nanocrystals. Int. J. Biol. Macromol. 2018, 112, 7–13. [Google Scholar] [CrossRef]
- Halcón, L.; Milkus, K. Staphylococcus aureus and wounds: A review of tea tree oil as a promising antimicrobial. Am. J. Infect. Control. 2004, 32, 4002–4008. [Google Scholar] [CrossRef]
- Karpanen, T.J.; Worthington, T.; Hendry, E.R.; Conway, B.R.; Lambert, P.A. Antimicrobial efficacy of chlorhexidine digluconate alone and in combination with eucalyptus oil, tea tree oil and thymol against planktonic and biofilm cultures of Staphylococcus epidermidis. J. Antimicrob. Chemother. 2008, 62, 1031–1036. [Google Scholar] [CrossRef]
- Kwiecinski, J.; Eick, S.; Wojcik, K. Effects of tea tree (Melaleuca alternifolia) oil on Staphylococcus aureus in biofilms and stationary growth phase. Int. J. Antimicrob. Agents 2009, 33, 343–347. [Google Scholar] [CrossRef]
- Sudjana, A.N.; Carson, C.F.; Carson, K.C.; Riley, T.V.; Hammer, K.A. Candida albicans adhesion to human epithelial cells and polystyrene and formation of biofilm is reduced by sub-inhibitory Melaleuca alternifolia (tea tree) essential oil. Med. Mycol. 2012, 50, 863–870. [Google Scholar] [CrossRef]
- Schillaci, D.; Arizza, V.; Dayton, T.; Camarda, L.; Di Stefano, V. In vitro anti-biofilm activity of Boswellia spp. oleogum resin essential oils. Lett. Appl. Microbiol. 2008, 47, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-Sánchez, D.; Cabo, M.L.; Rodríguez-Herrera, J.J. Antimicrobial activity of essential oils against Staphylococcus aureus biofilms. Food Sci. Technol. Int. 2014, 21, 559–570. [Google Scholar] [CrossRef] [PubMed]
- Olivier, E.I. Antimicrobial activities of selected essential oils against Fusarium oxysporum isolates and their biofilms. S. Afr. J. Bot. 2015, 99, 115–121. [Google Scholar]
- Saharkhiz, M.J.; Motamedi, M.; Zomorodian, K.; Pakshir, K.; Miri, R.; Hemyari, K. Chemical Composition, Antifungal and Antibiofilm Activities of the Essential Oil of Mentha piperita L. ISRN Pharm. 2012, 2012, 718645. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Lee, J.H.; Kim, S.I.; Cho, M.H.; Lee, J. Anti-biofilm, anti-hemolysis, and anti-virulence activities of black pepper, cananga, myrth oils, and nerolidol against Staphylococcus aureus. Appl. Microbiol. Biotechnol. 2014, 98, 9447–9457. [Google Scholar] [CrossRef] [PubMed]
- Gursoy, U.K.; Gursoy, M.; Gursoy, O.V.; Cakmakci, L.; Könönen, E.; Uitto, V.J. Anti-biofilm properties of Satureja hortensis L. essential oil against periodontal pathogens. Anaerobe 2009, 15, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Gomes, F.; Teixeira, P.; Cerca, N.; Azeredo, J.; Oliveira, R. Effect of Farnesol on Structure and Composition of Staphylococcus epidermidis Biofilm Matrix. Curr. Microbiol. 2011, 63, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Sepahi, E.; Tarighi, S.; Ahmadi, F.S.; Bagheri, A. Inhibition of quorum sensing in Pseudomonas aeruginosa by two herbal essential oils from Apiaceae family. J. Microbiol. 2015, 53, 176–180. [Google Scholar] [CrossRef]
- Pratiwi, S.U.T.; Lagendijk, E.L.; de Weert, S.; Idroes, R.; Hertiani, T.; Van den Hondel, C. Effect of Cinnamomum burmannii Nees ex Bl. and Massoiaaromatica Becc. Essential oils on planktonic growth and biofilm formation of Pseudomonas aeruginosa and Staphylococcus aureus In Vitro. Int. J. Appl. Res. Nat. Prod. 2015, 8, 1–13. [Google Scholar]
- Camporese, A. In vitro activity of Eucalyptus smithii and Juniperus communis essential oils against bacterial biofilms and efficacy perspectives of complementary inhalation therapy in chronic and recurrent upper respiratory tract infections. Infez Med. 2013, 2, 117–124. [Google Scholar]
- Benbelaïd, F.; Khadir, A.; Abdoune, M.A.; Bendahou, M.; Muselli, A.; Costa, J. Antimicrobial activity of some essential oils against oral multidrugresistant Enterococcus faecalis in both planktonic and biofilm state. Asian Pac. J. Trop. Biomed. 2014, 4, 463–472. [Google Scholar] [CrossRef]
- Negreiros, M.; Pawlowski, Â.; Zini, C.A.; Soares, G.L.G.; Motta, A.; Frazzon, A.P.G. Antimicrobial and antibiofilm activity of Baccharis psiadioides essential oil against antibiotic-resistant Enterococcus faecalis strains. Pharm. Biol. 2016, 54, 3272–3279. [Google Scholar] [CrossRef]
- Zhou, L.; Zheng, H.; Tang, Y.; Yu, W.; Gong, Q. Eugenol inhibits quorum sensing at sub-inhibitory concentrations. Biotechnol. Lett. 2013, 35, 631–637. [Google Scholar] [CrossRef]
- Palmeira-de-Oliveira, A.; Gaspar, C.; Palmeira-de-Oliveira, R.; Silva-Dias, A.; Salgueiro, L.; Cavaleiro, C.; Pina-Vaz, C.; Martinez-de-Oliveira, J.; Queiroz, J.A.; Rodrigues, A.G. The anti-Candida activity of Thymbra capitata essential oil: Effect upon pre-formed biofilm. J. Ethnopharmacol. 2012, 140, 379–383. [Google Scholar] [CrossRef]
- Dalleau, S.; Cateau, E.; Berges, T.; Berjeaud, J.M.; Imbert, C. In vitro activity of terpenes against Candida biofilms. Int. J. Antimicrob. Agents 2008, 31, 572–576. [Google Scholar] [CrossRef] [PubMed]
- Avcioglu, N.H.; Sahal, G.; Bilkay, I.S. Antibiofilm effects of citrus limonum and zingiber officinale oils on biofilm formation of Klebsiella ornithinolytica, Klebsiella oxytoca and klebsiella terrigena species. Afr. J. Tradit. Complement. Altern. Med. 2016, 13, 61–67. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kerekes, E.B.; Vidács, A.; Takó, M.; Petkovits, T.; Vágvölgyi, C.; Horváth, G.; Balázs, V.L.; Krisch, J. Anti-Biofilm Effect of Selected Essential Oils and Main Components on Mono- and Polymicrobic Bacterial Cultures. Microorganisms 2015, 7, 345. [Google Scholar] [CrossRef] [PubMed]
- Rosato, A.; Sblano, S.; Salvagno, L.; Carocci, A.; Clodoveo, M.L.; Corbo, F.; Fracchiolla, G. Anti-Biofilm Inhibitory Synergistic Effects of Combinations of Essential Oils and Antibiotics. Antibiotics 2020, 9, 637. [Google Scholar] [CrossRef] [PubMed]
- Teles, R.P.; Teles, F.R.F. Antimicrobial agents used in the control of periodontal biofilms: Effective adjuncts to mechanical plaque control. Braz. Oral. Res. 2009, 23, 39–48. [Google Scholar] [CrossRef]
- Martos, J.; Ferrer Luque, C.M.; González-Rodríguez, M.P.; Arias-Moliz, M.T.; Baca, P. Antimicrobial activity of essential oils and chloroform alone and combinated with cetrimide against Enterococcus faecalis biofilm. Eur. J. Microbiol. Immunol. 2013, 3, 44–48. [Google Scholar] [CrossRef]
- Venkateshbabu, N.; Anand, S.; Abarajithan, M.; Sheriff, S.O.; Jacob, P.S.; Sonia, N. Natural therapeutic options in endodontics—A review. Open Dent. J. 2016, 10, 214–226. [Google Scholar] [CrossRef] [PubMed]
- Santamaria, M., Jr.; Petermann, K.D.; Vedovello, A.S.; Degan, V.; Lucato, A.; Franzinic, C.M. Antimicrobial effect of Melaleuca alternifolia dental gel in orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Carson, C.F.; Hammer, K.A.; Riley, T.V. Melaleuca alternifolia (Tea Tree) Oil: A Review of Antimicrobial and Other Medicinal Properties. Clin. Microbiol. Rev. 2006, 19, 50–62. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.; Robertson, D.P.; Lappin, D.F.; Ramage, G. Commercial mouth washes are ineffective against oral MRSA biofilms. Oral Med. 2013, 115, 624–629. [Google Scholar]
- Stanecu, F.; Bancescu, G.; Constantinescu, M.V.; Defta, C. Microbial biofilm as a form of bacteria high organization and communication. Rom. J. Stomatol. 2012, 58, 284–290. [Google Scholar]
- Nostro, A.; SudanoRoccaro, A.; Bisignano, G.; Marino, A.; Cannatelli, M.A.; Pizzimenti, F.C.; Cioni, P.L.; Procopio, F.; Blanco, A.R. Effects of oregano, carvacrol and thymol on Staphylococcus aureus and Staphylococcus epidermidis biofilms. J. Med. Microbiol. 2007, 56, 519–523. [Google Scholar] [CrossRef]
- Cortelli, S.C.; Costa, F.O.; Rode, S.; Haas, A.N.; Pintode Andrade, A.K.; Pannuti, C.M.; Escobar, E.C.; de Almeida, E.R.; Cortelli, J.R.; Pedrazzi, V.; et al. Mouthrinserecommendation for prosthodontic patients. Braz. Oral Res. 2014, 28, 1–9. [Google Scholar] [CrossRef]
- Marsh, P.D. Controlling the oral biofilm with antimicrobials. J. Dent. 2010, 38, S11–S15. [Google Scholar] [CrossRef]
- Haas, A.N.; Pannuti, C.M.; Andrade, A.K.P.; Escobar, E.C.; Almeida, E.R.; Costa, F.O.; Cortelli, J.R.; Cortelli, S.C.; Rode, S.; Pedrazzi, V.; et al. Mouthwashes for the control of supragingival biofilm and gingivitis in orthodontic patients: Evidence-based recommendations for clinicians. Braz. Oral Res. 2014, 28, 1–8. [Google Scholar] [CrossRef]
- Quintas, V.; Prada-López, I.; Prados-Frutos, J.C.; Tomás, I. In situ antimicrobial activity on oral biofilm: Essential oils vs. 0.2% chlorhexidine. Clin. Oral Investig. 2015, 19, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Quintas, V.; Prada-López, I.; Donos, N.; Suárez-Quintanilla, D.; Tomás, I. Antiplaque Effect of Essential Oils and 0.2% Chlorhexidine on an In Situ Model of Oral Biofilm Growth: A Randomised Clinical Trial. PLoS ONE 2015, 10, e0117177. [Google Scholar] [CrossRef] [PubMed]
- Erriu, M.; Pili, F.M.G.; Tuveri, E.; Pigliacampo, D.; Scano, A.; Montaldo, C.; Piras, V.; Denotti, G.; Pilloni, A.; Garau, V.; et al. Oil Essential Mouthwashes Antibacterial Activity against Aggregati bacteractinomycetemcomitans: A Comparison between Antibiofilm and Antiplanktonic Effects. Int. J. Dent. 2013, 164267. [Google Scholar] [CrossRef]
- Sun, F.C.; Engelman, E.E.; McGuire, J.A. Impact of an Anticaries Mouthrinse on In Vitro Remineralization and Microbial Control. Int. J. Dent. 2014, 2014, 982071. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rasooli, I.; Shayegh, S.; Taghizadeh, M.; Astaneh, S.D.A. Phytotherapeutic Prevention of Dental Biofilm Formation. Phytother. Res. 2008, 22, 1162–1167. [Google Scholar] [CrossRef]
- Hofer, D.; Meier, A.; Sener, B.; Guggenheim, B.; Attin, T.; Schmidlin, P.R. Biofilm reduction and staining potential of a 0.05% chlorhexidine rinse containing essential oils. Int. J. Dent. Hyg. 2011, 9, 60–67. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Apolonio, J.; Faleiro, M.L.; Miguel, M.G.; Neto, L. No induction of antimicrobial resistance in Staphylococcus aureus and Listeria monocytogenes during continuous exposure to eugenol and citral. FEMS Microbiol. Lett. 2014, 354, 92–101. [Google Scholar]
- Bersan, S.M.F.; Galvão, L.C.C.; Goes, V.F.F. Action of essential oils from Brazilian native and exotic medicinal species on oral biofilms. BMC Complement. Altern. Med. 2014, 14, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Pedrazzi, V.; Escobar, E.C.; Cortelli, J.R.; Haas, A.N.; Pintode Andrade, A.K.; Pannuti, C.M.; Rodriguesde Almeida, E.; Costa, F.O.; Cortelli, S.C.; de Mello Rode, S. Antimicrobial mouth rinse use as an adjunct method in peri-implant biofilmcontrol. Braz. Oral Res. 2014, 28, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Marinković, J.; Ćulafić, D.M.; Nikolić, B.; Đukanović, S.; Marković, T.; Tasić, G.; Ćirić, A.; Marković, D. Antimicrobial potential of irrigants based on essential oils of Cymbopogon martinii and Thymus zygis towards in vitro multispecies biofilm cultured in ex vivo root canals. Arch. Oral Biol. 2020, 117, 104842. [Google Scholar] [CrossRef]
- Jongsma, M.A.; van der Mei, H.C.; Atema-Smit, J.; Busscher, H.J.; Ren, Y. In vivo biofilm formation on stainless steel bonded retainers during different oral health-care regimens. Int. J. Oral Sci. 2015, 7, 42–48. [Google Scholar] [CrossRef][Green Version]
- Braga, A.S.; de Melo Simas, L.L.; Pires, J.G.; Martines Souza, B.; de Souza Rosa de Melo, F.P.; Saldanha, L.L.; Dokkedal, A.L.; Magalhães, A.C. Antibiofilm and anti-caries effects of an experimental mouth rinse containing Matricaria chamomilla L. extract under microcosm biofilm on enamel. J. Dent. 2020, 99, 103415. [Google Scholar] [CrossRef] [PubMed]
- Rasooli, I.; Shayegh, S.; Astaneh, S. The effect of Mentha spicata and Eucalyptus camaldulensis essential oils on dental biofilm. Int. J. Dent. Hyg. 2009, 7, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Kouidhi, B.; Mohammed, Y.A.; Qurashi, A.L.; Chaieb, K. Drug resistance of bacterial dental biofilm and the potential use of natural compounds as alternative for prevention and treatment. Microb. Pathog. 2015, 80, 39–49. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho Galváo, L.C.; Furletti, V.F.; Bersan, S.M.F.; da Cunha, M.G.; Ruiz, A.L.T.G.; Ernesto de Carvalho, J.; Sartoratto, A.; Rehder, V.L.G.; Figueira, G.M.; Duarte, M.C.T.; et al. Antimicrobial activity of essential oils against Streptococcus mutans and their antiproliferative effects. Evid. Based Complement. Altern. Med. 2012. [Google Scholar] [CrossRef]
- Wongsariya, K.; Phanthong, P.; Bunyapraphatsara, N.; Srisukh, V.; Chomnawang, M.T. Synergistic interaction and mode of action of Citrus hystrix essential oil against bacteria causing periodontal diseases. Pharm. Biol. 2014, 52, 273–280. [Google Scholar] [CrossRef]
- Pedrazzi, V.; Leite, M.F.; Tavares, C.R.; Sato, S.; do Nascimento, G.C.; Issa, J.P.M. Herbal mouthwash containing extracts of Baccharis dracunculifoliaas agent for the control of biofilm: Clinical evaluation in humans. Sci. World J. 2015. [Google Scholar] [CrossRef]
- Lee, K.H.; Kim, B.S.; Keum, K.S.; Yu, H.H.; Kim, Y.-H.; Chang, B.-S.; Ra, J.-Y.; Moon, H.-D.; Seo, B.-R.; Choi, N.-Y.; et al. Essential oil of Curcuma longa inhibits Streptococcus mutans biofilm formation. J. Food Sci. 2011, 76. [Google Scholar] [CrossRef] [PubMed]
- Peraltaa, S.L.; Carvalhob, P.H.A.; van de Sandea, F.H.; Pereirac, C.M.P.; Pivaa, E.; Lund, R.G. Self-etching dental adhesive containing a natural essential oil: Anti-biofouling performance and mechanical properties. Biofouling 2013, 29, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Furletti, V.F.; Teixeira, L.P.; Obando-Pereda, G. Action of Coriandrum sativum L. essential oil upon oral Candida albicans biofilm formation. Evid. Based Complement. Altern. Med. 2011. [Google Scholar] [CrossRef]
- Oliveira, S.A.; Zambrana, J.R.; Iorio, F.B.; Pereira, C.A.; Jorge, A.O. The antimicrobial effects of Citrus limonum and Citrus aurantium essential oils on multi-species biofilms. Braz. Oral. Res. 2014, 28, 22–27. [Google Scholar] [CrossRef]
- Freires, I.A.; Bueno-Silva, B.; Câmara de Carvalho Galvão, L.; Duarte, M.C.T.; Sartoratto, A.; Figueira, G.M.; de Alencar, S.M.; Rosalen, P.L. The effect of essential oils and bioactive fractions on Streptococcus mutans and Candida albicans biofilms: A confocal analysis. Evid. Based Complement. Altern. Med. 2015. [Google Scholar] [CrossRef]
- de Almeida Freires, I.; Murata, R.M.; Furletti, V.F. Coriandrum sativum L. (Coriander) essential oil: Antifungal activity and mode of action on Candida spp., and molecular targets affected in human whole-genome expression. PLoS ONE 2014, 9, e099086. [Google Scholar] [CrossRef]
- Alves, F.R.F.; Neves, M.A.S.; Silva, M.G.; Rôças, I.N.; Siqueira, J.F., Jr. Antibiofilm and antibacterial activities of farnesol and xylitol as potential endodontic irrigants. Braz. Dent. J. 2013, 24, 224–229. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Anghel, I.; Grumezescu, A.M.; Holban, A.M.; Ficai, A.; Anghel, A.G.; Chifiriuc, M.C. Biohybrid nanostructured iron oxide nanoparticles and Satureja hortensis to prevent fungal biofilm development. Int. J. Mol. Sci. 2013, 14, 18110–18123. [Google Scholar] [CrossRef] [PubMed]
- Park, H.; Jang, C.H.; Cho, Y.B.; Choi, C.H. Antibacterial effect of Tea-tree oil on methicillin-resistant Staphylococcus aureus biofilm formation of the tympanostomy tube: An in vitro study. In Vivo 2007, 21, 1027–1030. [Google Scholar]
- Brady, A.J.; Farnan, T.B.; Toner, J.G.; Gilpin, D.F.; Tunney, M.M. Treatment of a cochlear implant biofilm infection: A potential role for alternative antimicrobial agents. Ann. Otol. Rhinol. Laryngol. 2010, 124, 729–738. [Google Scholar] [CrossRef]
- Malic, S.; Jordan, R.P.C.; Waters, M.G.J.; Stickler, D.J.; Williamsa, D.W. Biocide activity against urinary catheter pathogen. Antim. Agents Chemother. 2014, 58, 1192–1194. [Google Scholar] [CrossRef][Green Version]
- Saviuc, C.; Dascălu, L.; Chifiriuc, M.C.; Rădulescu, V.; Oprea, E.; Popa, M.; Hristu, R.; Stanciu, G.; Lazăr, V. The inhibitory activity of pomelo essential oil on the bacterial biofilms development on soft contact lenses. Roum. Arch. Microbiol. Immunol. 2010, 69, 145–152. [Google Scholar]
- Gbenou, J.D.; Ahounou, J.F.; Akakpo, H.B.; Laleye, A.; Yayi, E.; Gbaguidi, F.; Baba-Moussa, L.; Darboux, R.; Dansou, P.; Moudachirou, M.; et al. Phytochemical composition of Cymbopogon citratus and Eucalyptus citriodora essential oils and their anti-inflammatory and analgesic properties on Wistar rats. Mol. Biol. Rep. 2013, 40, 1127–1134. [Google Scholar] [CrossRef]
- Nassar, M.I.; Gaara, A.H.; El-Ghorab, A.H.; Farrag, A.-R.H.; Shen, H.; Huq, E.; Mabry, T. Chemical constituents of Clove (Syzygium aromaticum, Fam. Myrtaceae) and their antioxidant activity. Rev Latinoamer. Quím. 2007, 35, 47–57. [Google Scholar]
- Khan, M.S.A.; Ahmad, I. Biofilm inhibition by Cymbopogon citratus and Syzygium aromaticum essential oils in the strains of Candida albicans. J. Ethnopharmacol. 2012, 140, 416–423. [Google Scholar] [CrossRef]
- Kim, Y.G.; Lee, J.H.; Kim, S.I.; Baek, K.H.; Lee, J. Cinnamon bark oil and its components inhibit biofilm formation and toxin production. Int. J. Food Microbiol. 2015, 195, 30–39. [Google Scholar] [CrossRef]
- Chmit, M.; Kanaan, H.; Habib, J.; Abbass, M.; Mcheik, A.; Chokr, A. Antibacterial and antibiofilm activities of polysaccharides, essential oil, and fatty oil extracted from Laurus nobilis growing in Lebanon. Asian Pac. J. Trop. Med. 2014, 7, S546–S552. [Google Scholar] [CrossRef]
- Caredda, A.; Marongiu, B.; Porcedda, S.; Soro, C. Supercritical carbon dioxide extraction and characterization of Laurus nobilis essential oil. J. Agric. Food Chem. 2002, 50, 1492–1496. [Google Scholar] [CrossRef]
- Nostro, A.; Scaffaro, R.; D’Arrigo, M.; Botta, L.; Filocamo, A.; Marino, A.; Bisignano, G. Development and characterization of essential oil component-based polymer films: A potential approach to reduce bacterial biofilm. Appl. Microbiol. Biotechnol. 2013, 97, 9515–9523. [Google Scholar] [CrossRef]
- Coughlan, L.M.; Cotter, P.D.; Hill, C.; Alvarez-Ordóñez, A. New weapons to fight old enemies: Novel strategies for the (bio)control of bacterial biofilms in the food industry. Front. Microbiol. 2016. [Google Scholar] [CrossRef]
- Giaouris, E.; Heir, E.; Hébraud, M.; Chorianopoulos, N.; Langsrud, S.; Møretrø, T.; Habimana, O.; Desvaux, M.; Renier, S.; Nychas, G.J. Attachment and biofilm formation by foodborne bacteria in meat processing environments: Causes, implications, role of bacterial interactions and control by alternative novel methods. Meat Sci. 2014, 97, 298–309. [Google Scholar] [CrossRef] [PubMed]
- Znini, M.; Bouklah, M.; Majidi, L.; Kharchouf, S.; Aouniti, A.; Bouyanzer, A.; Hammouti, B.; Costa, J.; Al-Deyab, S.S. Chemical composition and inhibitory effect of Mentha spicata essential oil on the corrosion of steel in molar hydrochloric acid. Int. J. Electrochem. Sci. 2011, 6, 691–704. [Google Scholar]
- Gachkar, L.; Yadegari, D.; Rezaei, M.B.; Taghizadeh, M.; Astaneh, S.A.; Rasooli, I. Chemical and biological characteristics of Cuminum cyminum and Rosmarinus officinalis essential oils. Food Chem. 2007, 102, 898–904. [Google Scholar] [CrossRef]
- Valeriano, C.; de Oliveira, T.L.C.; de Carvalhoa, S.M.; das Graças Cardoso, M.; Alves, E.; Piccoli, R.H. The sanitizing action of essential oil-based solutions against Salmonella enterica serotype Enteritidis S64 biofilm formation on AISI 304 stainless steel. Food Control 2012, 25, 673–677. [Google Scholar] [CrossRef]
- Piovezan, M.; Uchida, N.S.; da Silva, A.F.; Grespan, R.; Santos, P.R.; Silva, E.L.; Cuman, R.K.N.; Machinski Junior, M.; Mikcha, J.M.G. Effect of cinnamon essential oil and cinnamaldehyde on Salmonella Saintpaul biofilm on a stainless steel surface. J. Gen. Appl. Microbiol. 2014, 60, 119–121. [Google Scholar] [CrossRef]
- Karampoula, F.; Giaouris, E.; Deschamps, J.; Doulgeraki, A.I.; Nychas, G.-J.E.; Dubois-Brissonnet, F. Hydrosol of Thymbra capitata is a highly efficient biocide against Salmonella enterica serovar Typhimurium biofilms. Appl. Environ. Microbiol. 2016, 82, 5309–5319. [Google Scholar] [CrossRef]
- Liu, Q.; Niu, H.; Zhang, W.; Mu, H.; Sun, C.; Duan, J. Synergy among thymol, eugenol, berberine, cinnamaldehyde and streptomycin against planktonic and biofilm-associated food-borne pathogens. Lett. Appl. Microbiol. 2015, 60, 421–430. [Google Scholar] [CrossRef]
- Laird, K.; Armitage, D.; Phillips, C. Reduction of surface contamination and biofilms of Enterococcus sp. and Staphylococcus aureus using a citrus-based vapour. J. Hosp. Infect. 2012, 80, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Qayyum, S.; Khan, A.U. Nanoparticles vs. biofilms: A battle against another paradigm of antibiotic resistance. Med. Chem. Commun. 2016, 7, 1479–1498. [Google Scholar] [CrossRef]
- Chifiriuc, M.C.; Grumezescu, V.; Grumezescu, A.M.; Saviuc, C.; Lazăr, V.; Andronescu, E. Hybrid magnetite nanoparticles/Rosmarinus officinalis essential oil nanobiosystem with antibiofilm activity. Nanoscale Res. Lett. 2012, 7, 209. [Google Scholar] [CrossRef] [PubMed]
- Iannitelli, A.; Grande, R.; Di Stefano, A.; Di Giulio, M.; Sozio, P.; Bessa, L.J.; Laserra, S.; Paolini, C.; Protasi, F.; Cellini, L. Potential antibacterial activity of carvacrol-loaded poly(DL-lactide-co-glycolide) (PLGA) nanoparticles against microbial biofilm. Int. J. Mol. Sci. 2011, 12, 5039–5051. [Google Scholar] [CrossRef]
- Bilcu, M.; Grumezescu, A.M.; Oprea, A.E.; Popescu, R.C.; Mogoșanu, G.D.; Hristu, R.; Stanciu, G.A.; Mihailescu, D.F.; Lazar, V.; Bezirtzoglou, E.; et al. Efficiency of vanilla, patchouli and ylang ylang essential oils stabilized by iron oxide@C14 nanostructures against bacterial adherence and biofilms formed by Staphylococcus aureus and Klebsiella pneumoniae clinical strains. Molecules 2014, 19, 17943–17956. [Google Scholar] [CrossRef]
- Liakos, I.L.; Grumezescu, A.M.; Holban, A.M.; Florin, I.; D’Autilia, F.; Carzino, R.; Bianchini, P.; Athanassiou, A. Polylacticacid-lemongrass essential oil nanocapsules with antimicrobial properties. Pharmaceuticals 2016, 9, 42. [Google Scholar] [CrossRef]
- Grumezescu, A.M.; Andronescu, E.; Oprea, A.E.; Holban, A.M.; Socol, G.; Grumezescu, V.; Chifiriuc, M.C.; Iordache, F.; Maniu, H. MAPLE fabricated magnetite@ Melissa officinalis and polylactic acid: Chitosan coated surfaces with anti-staphylococcal properties. J. Sol-Gel Sci. Technol. 2015, 73, 612–619. [Google Scholar] [CrossRef]
- Giongo, J.L.; de Almeida Vaucher, R.; Fausto, V.P.; Quatrin, P.M.; Lopes, L.Q.S.; Santos, R.C.V.; Gündel, A.; Gomes, P.; Steppe, M. Anti-Candida activity assessment of Pelargonium graveolens oil free and nanoemulsion in biofilm formation in hospital medical supplies. Microb. Pathog. 2016, 100, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Shemesh, R.; Krepker, M.; Natan, M.; Danin-Poleg, Y.; Banin, E.; Kashi, Y.; Nitzan, N.; Vaxman, A.; Segal, E. Novel LDPE/halloysite nanotube films with sustained carvacrol release for broad-spectrum antimicrobial activity. RSC Adv. 2015, 5, 87108–87117. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nuță, D.C.; Limban, C.; Chiriță, C.; Chifiriuc, M.C.; Costea, T.; Ioniță, P.; Nicolau, I.; Zarafu, I. Contribution of Essential Oils to the Fight against Microbial Biofilms—A Review. Processes 2021, 9, 537. https://doi.org/10.3390/pr9030537
Nuță DC, Limban C, Chiriță C, Chifiriuc MC, Costea T, Ioniță P, Nicolau I, Zarafu I. Contribution of Essential Oils to the Fight against Microbial Biofilms—A Review. Processes. 2021; 9(3):537. https://doi.org/10.3390/pr9030537
Chicago/Turabian StyleNuță, Diana Camelia, Carmen Limban, Cornel Chiriță, Mariana Carmen Chifiriuc, Teodora Costea, Petre Ioniță, Ioana Nicolau, and Irina Zarafu. 2021. "Contribution of Essential Oils to the Fight against Microbial Biofilms—A Review" Processes 9, no. 3: 537. https://doi.org/10.3390/pr9030537
APA StyleNuță, D. C., Limban, C., Chiriță, C., Chifiriuc, M. C., Costea, T., Ioniță, P., Nicolau, I., & Zarafu, I. (2021). Contribution of Essential Oils to the Fight against Microbial Biofilms—A Review. Processes, 9(3), 537. https://doi.org/10.3390/pr9030537









