1. Introduction
The human skeletal system comprises a dynamic and highly specialized network of tissues that perform multiple vital functions, including structural support, locomotion, mineral storage, and the protection of internal organs. Bone, as the fundamental component of this system, is a composite material consisting of an inorganic mineral phase primarily composed of hydroxyapatite (Ca
10(PO
4)
6(OH)
2), and an organic matrix largely comprising type I collagen and various non-collagenous proteins [
1,
2,
3]. This biphasic structure confers bone with a unique combination of stiffness, toughness, and resistance to mechanical loads [
4,
5,
6,
7,
8,
9,
10]. The regulation of bone homeostasis is mediated by osteoblasts, osteoclasts, and osteocytes, each playing distinct yet interdependent roles in the processes of bone formation, remodeling, and mineral turnover [
1,
2,
11,
12,
13,
14,
15].
Bone tissue is categorized into two structural types: coarse-fibrous (woven) bone and fine-fibrous (lamellar) bone. The former appears transiently during fetal development and early stages of bone repair, while the latter forms the mature bone structure and is further differentiated into cortical (compact) and trabecular (spongy) bone [
3]. Cortical bone constitutes the dense outer layer of long bones, imparting mechanical strength, whereas trabecular bone, located within the epiphyses and flat bones, supports metabolic activity including hematopoiesis through its high vascularization.
In orthopedics and traumatology, metallic implants have long been the material of choice due to their mechanical robustness and structural reliability. Alloys such as stainless steel, cobalt–chromium, and titanium have been extensively utilized in clinical practice for internal fixation and joint replacement applications [
15]. Despite their mechanical superiority, these materials are biologically inert, non-resorbable, and often necessitate secondary removal surgeries. Furthermore, they are associated with stress-shielding effects, whereby the mismatch in elastic modulus between the implant and surrounding bone reduces physiological load transfer, leading to bone resorption and implant loosening. Additionally, these implants are vulnerable to microbial colonization and biofilm formation, which can result in chronic periprosthetic infections that are difficult to eradicate [
16,
17,
18,
19,
20].
To address these limitations, biodegradable metals have gained increasing interest as next-generation biomaterials for temporary implant applications. Among these, magnesium (Mg) and its alloys are especially promising owing to their low density, biocompatibility, and mechanical properties that closely approximate those of human cortical bone [
4,
5,
21,
22,
23,
24,
25]. Magnesium offers several biological advantages: it is a natural constituent of the human body, involved in numerous enzymatic processes and cellular signaling pathways, and it stimulates osteogenesis and angiogenesis. The biodegradability of Mg facilitates gradual resorption in vivo, eliminating the need for surgical removal and reducing long-term complication risks.
However, the clinical translation of magnesium-based implants is impeded by their inherent susceptibility to rapid degradation in physiological environments. Upon implantation, Mg reacts with water and chloride ions to form Mg(OH)
2 and hydrogen gas, a process exacerbated by the presence of bicarbonates and phosphates in body fluids that convert the hydroxide layer into more soluble salts like MgCO
3 [
6]. The uncontrolled release of hydrogen gas and resultant local alkalization can lead to soft tissue inflammation, delayed healing, and poor osseointegration. These issues necessitate the development of effective surface modification strategies to regulate the degradation rate while maintaining or enhancing the bioactivity of the material [
26,
27,
28,
29,
30,
31,
32].
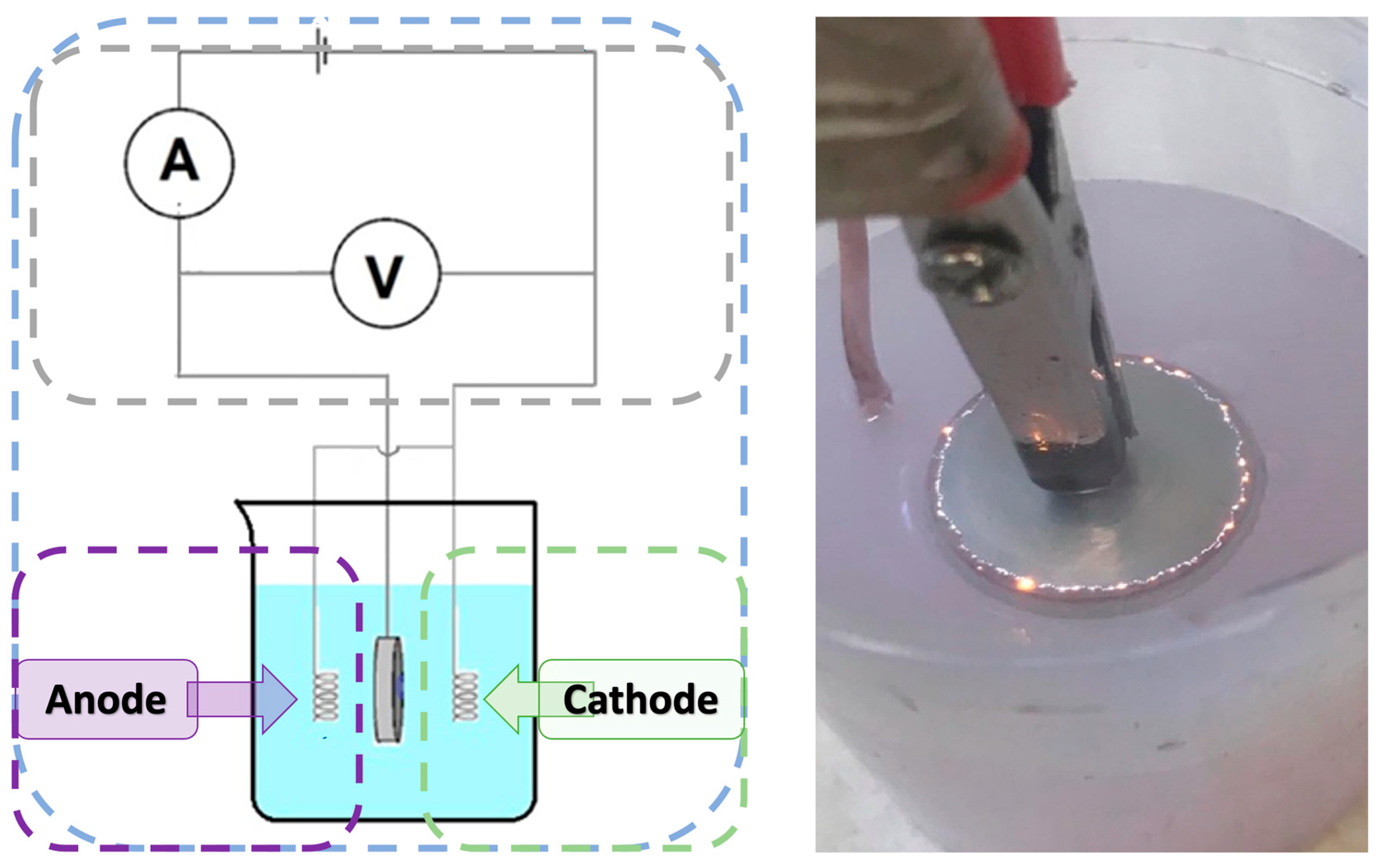
Several techniques have been developed to improve the surface stability and biocompatibility of Mg implants. Plasma electrolytic oxidation (PEO), also known as micro-arc oxidation, has emerged as a particularly effective method to generate dense, ceramic-like oxide layers on Mg surfaces. This electrochemical process involves high-voltage anodic treatment in an electrolytic bath, resulting in the formation of a porous, corrosion-resistant magnesium oxide layer that can incorporate bioactive ions such as calcium, phosphate, and silicate depending on electrolyte composition [
10,
33,
34,
35,
36,
37,
38,
39,
40,
41,
42,
43,
44]. The resulting topography and surface chemistry can promote cellular attachment, differentiation, and mineralization.
In addition to ceramic coatings, polymer-based modifications have been investigated to enhance surface biofunctionality. Polydopamine (PDA), a synthetic analog of the mussel-derived adhesive catecholamine, is capable of forming thin, conformal coatings on a wide range of substrates. PDA coatings exhibit strong adhesion, good biocompatibility, and the ability to immobilize bioactive molecules, making them highly suitable for biomedical applications [
45,
46,
47,
48,
49,
50,
51]. PDA enhances osteoblast adhesion and proliferation by mimicking the extracellular matrix and providing functional groups for secondary modification. Another extensively studied polymer is chitosan—a biodegradable, non-toxic polysaccharide known for its antimicrobial, hemostatic, and immunomodulatory properties [
8,
9]. Chitosan’s cationic nature allows it to interact with cell membranes and negatively charged surfaces, facilitating film formation and bioactive molecule delivery.
Emerging strategies also incorporate metallic nanoparticles, such as gold nanoparticles (AuNPs), which have been shown to exhibit anti-inflammatory and osteoinductive properties while improving corrosion resistance when embedded in coating matrices [
10]. The integration of multiple surface modification techniques—for example, PEO followed by polymer and nanoparticle deposition—offers the potential to synergistically combine the mechanical robustness of the ceramic layer with the biological advantages of polymers and nanomaterials.
Despite these advances, the clinical translation of such combinatorial surface treatments remains limited by a lack of systematic evaluations and comparative studies. Most investigations focus on a single modification method or do not fully assess the interactions between coating layers and their cumulative effect on implant performance. Moreover, while promising in vitro results have been reported, preclinical and clinical data validating long-term efficacy and safety are still scarce. Notably, critical parameters such as degradation kinetics, corrosion behavior in simulated body fluids, and cytocompatibility with osteoblastic cells must be quantitatively and reproducibly characterized under standardized conditions to guide future clinical applications.
Therefore, a key research gap exists in understanding how multi-component surface engineering strategies—specifically the integration of PEO with PDA, chitosan, and AuNPs—can be optimized to maximize corrosion resistance, cytocompatibility, and surface bioactivity. These combined approaches may offer new opportunities for the design of next-generation biodegradable implants that degrade in a controlled manner while simultaneously promoting osteointegration and tissue healing.
The present study addresses this gap by systematically investigating magnesium implants modified via PEO and further functionalized with chitosan, polydopamine, and gold nanoparticles. A comprehensive characterization of the physicochemical and biological properties of the modified surfaces was conducted using Fourier-transform infrared spectroscopy (FT-IR), scanning electron microscopy (SEM), contact angle goniometry, electrochemical corrosion testing, and cytotoxicity assays using the human MG-63 osteoblastic cell line. The aim is to identify the surface modification strategy that offers the best compromise between structural integrity, degradation control, and biological performance. The findings are intended to contribute toward the rational design of clinically viable Mg-based orthopedic implants that align with the principles of biofunctionality, biocompatibility, and bioresorbability.
3. Results and Discussion
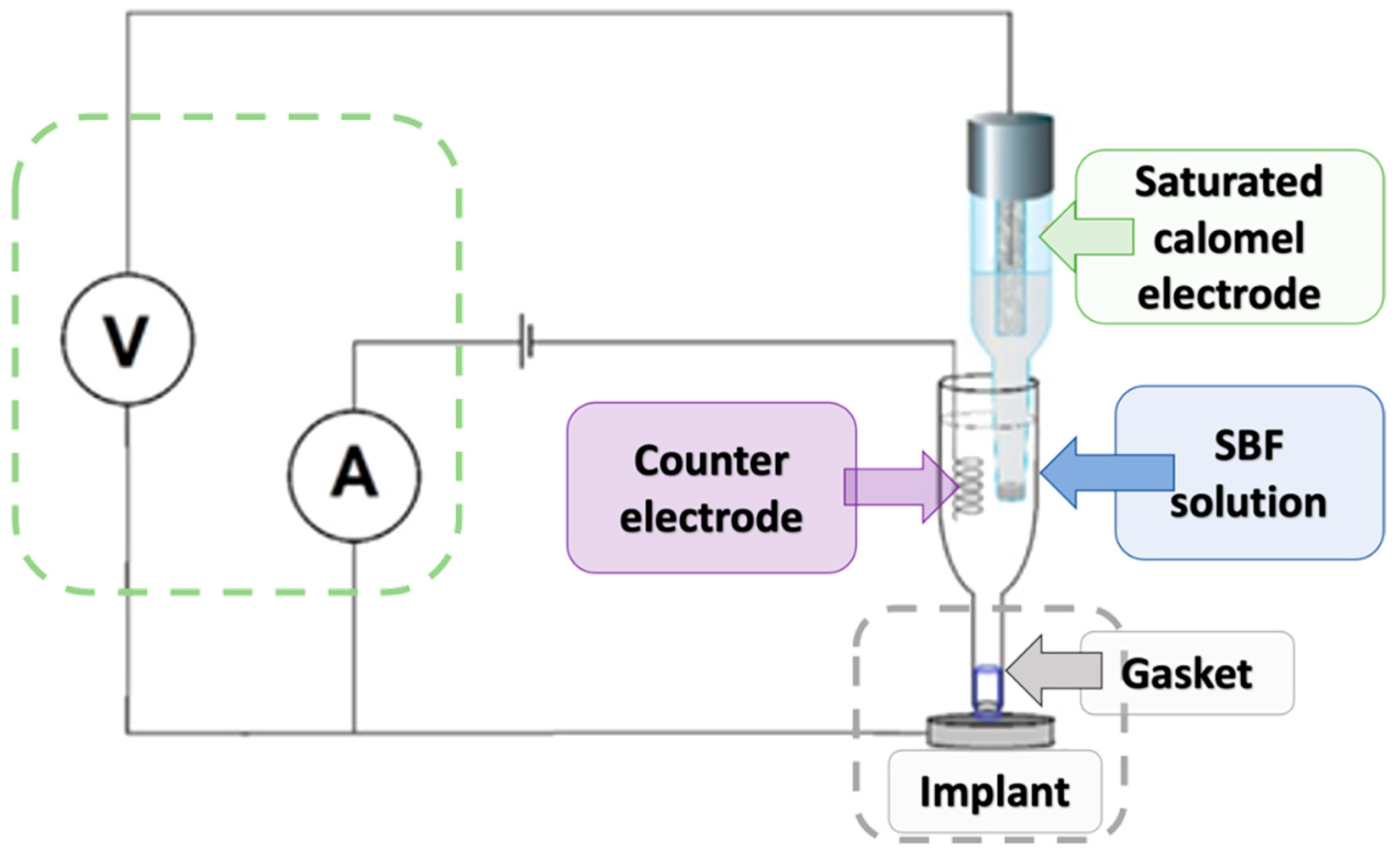
As a result of a series of tests, six different types of samples with advanced coatings have been developed. The general scheme of the article is given in
Figure 5.
Stereoscopic microscope images provided qualitative insights into the surface morphology of the modified magnesium samples. For all groups (
n = 3 per sample type), coatings were examined for visual homogeneity, aggregation, and coverage. Mg_01 and Mg_02 demonstrated relatively smooth and continuous layers; however, slight variations in thickness were observed at the periphery. Polydopamine-coated samples (Mg_03 and Mg_06) exhibited a granular surface texture indicative of PDA aggregation, as previously reported [
45]. To enable quantitative comparisons, images were further processed using ImageJ software (NIH, Bethesda, MD, USA, Fiji version 2.16.0–available as of June 2023, based on ImageJ 1.54p) to estimate surface porosity. Porosity was calculated as the percentage of dark pixel area relative to total sample area under threshold segmentation. PDA-modified samples (Mg_03 and Mg_06) showed porosity values of ~49.2% ± 2.1% and 51.8% ± 1.6%, respectively, which were significantly higher (
p < 0.05, ANOVA) than chitosan-coated counterparts (Mg_01: 34.7% ± 2.9%, Mg_02: 39.1% ± 1.8%). PEO-treated samples exhibited more interconnected and stable porosity due to plasma discharge-induced microchannels, favoring polymer infiltration.
The results obtained from the stereoscopic microscope images of the samples provide a detailed visual representation of the surface modifications and coatings applied to the pure magnesium discs. The samples were subjected to different coating methods and polymer formulations, with the objective of enhancing surface properties such as corrosion resistance and biocompatibility. For Mg_01, the magnesium disc was coated with chitosan solution with a viscosity range of 10–120 cps. The surface exhibited a smooth and homogeneous coating with minimal aggregation of the chitosan material. The coating adhered well to the magnesium surface, though a slight unevenness in thickness was observed at specific points, which could be attributed to the viscosity variation during the coating process. In Mg_02, the magnesium disc was modified with both chitosan (viscosity range of 100–300 cps) and polydopamine coating. The images revealed a more pronounced surface texture with visible features resulting from the polydopamine coating. The chitosan layer was more uniformly applied compared to Mg_01, and the polydopamine layer appeared to form small, granular aggregates over the chitosan base, which may contribute to additional surface roughness, potentially enhancing the adhesion of the coating to biological tissues. Mg_03 displayed a magnesium disc modified solely with a polydopamine coating. The surface was characterized by a thicker layer of polydopamine compared to Mg_02, with noticeable clusters forming at certain regions. The coating was more porous and uneven in distribution, suggesting that the polydopamine solution was applied at a higher concentration or with a different viscosity, which led to less uniformity in coverage across the surface. For the samples subjected to the plasma electrolytic oxidation (PEO) process, such as Mg_04, the magnesium disc showed a more roughened surface due to the formation of oxide layers typical of the PEO process. This modification significantly increased the surface area, which is beneficial for coating adhesion. When coated with chitosan (10–120 cps), the surface appeared to have a more adherent and homogeneous coating compared to Mg_01, with the rough surface providing better anchorage for the chitosan material. However, some areas still exhibited slight inconsistencies in coating thickness. In Mg_05, the PEO-modified magnesium disc was coated with chitosan (100–300 cps). The stereoscopic microscope images revealed a more textured surface compared to Mg_04, as the higher viscosity of the chitosan solution resulted in a thicker, more robust coating. This thicker coating appeared to cover more of the surface irregularities from the PEO treatment, suggesting improved coating stability and protection against corrosion. Finally, Mg_06 exhibited a PEO-modified magnesium disc with a polydopamine coating. The surface showed distinct, prominent polydopamine clusters, similarly to Mg_03, but the underlying oxide layer from the PEO treatment was more visible through the coating, indicating that the polydopamine did not fully cover the surface. The resulting rough and porous surface structure might enhance interactions with biological materials, although the unevenness could affect the uniformity of performance in certain applications (
Figure 6).
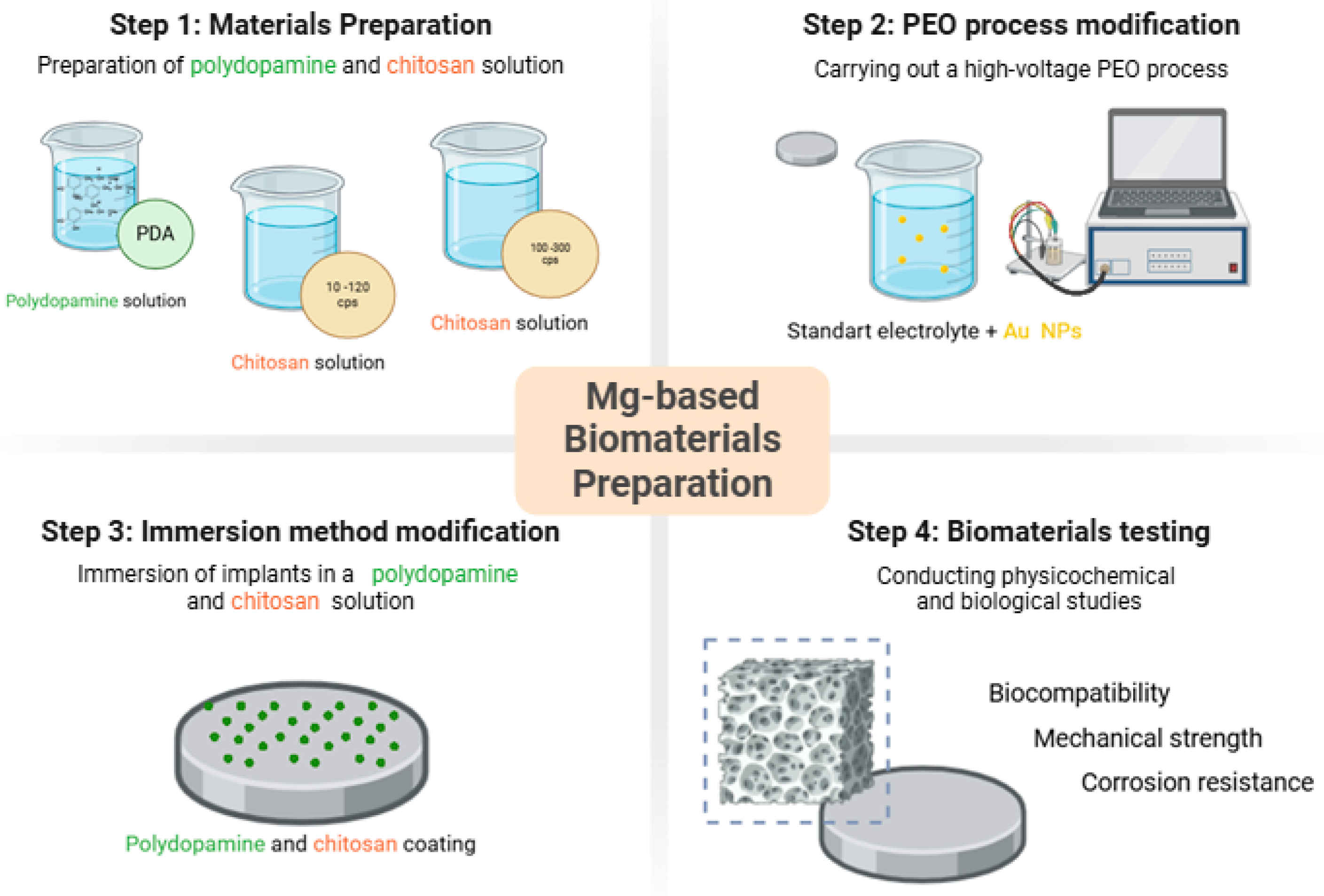
3.1. Chemical Structure Analysis via Fourier-Transform Infrared Spectroscopy (FT-IR)
Figure 7 reveals the results of the FT-IR study. The spectrum of the obtained polydopamine compound at
Figure 7a reveals a band at a frequency of 2935 cm
−1, which likely corresponds to characteristic stretching vibrations of the hydroxyl -OH and amine -NH groups. According to the literature data, these groups appear in the range of 4000–2500 cm
−1. A similar pattern can be observed in the chitosan spectra at
Figure 7b,c, where bands at frequencies of 3042 cm
−1 at
Figure 7b and 3090 cm
−1 at
Figure 7c also correspond to stretching vibrations of hydroxyl groups. Bands in the range of 2000–1500 cm
−1 are attributed to stretching vibrations originating from C=C, C=O, C=N, N=N double bonds, as well as bonds present in the aromatic ring, confirming the presence of this ring in all the analyzed samples. For example, the band at 1712 cm
−1 at
Figure 7a, indicates stretching vibrations of C=C bonds in the aromatic structure. In the range of 1300–1000 cm
−1 at
Figure 7a, bands corresponding to C–O bonds in the polydopamine (PDA) molecule are observed. The chitosan spectra at
Figure 7b,c show common features resulting from the structural similarity of these substances. Bands at frequencies of 2926 cm
−1 and 2927 cm
−1 are associated with the presence of the –CH
2 group, while bands at 1555 cm
−1, 1543 cm
−1, 1146 cm
−1, and 1149 cm
−1 confirm the presence of amine groups –NH
2. The presence of a β-glycosidic bond between molecules is manifested by bands at 1075 cm
−1 and 1077 cm
−1. The analysis of the spectrum of the coating obtained by plasma electrolytic oxidation at
Figure 7d indicates that the band at a frequency of 935 cm
−1 originates from the phosphate groups.
Taken together, the FT-IR spectra confirmed the presence of functional groups corresponding to polydopamine and chitosan in the coatings. Bands near 2935 cm−1 (O–H, N–H stretching), 1712 cm−1 (C=O), and 1075 cm−1 (C–O, β-glycosidic bond) were observed consistently across PDA and chitosan samples, supporting successful polymer incorporation. PEO-treated surfaces showed phosphate-related bands at 935 cm−1, suggesting integration of electrolyte-derived ions.
3.2. Wettability Study
The wettability study of the implant surface by a deposited water droplet demonstrated that the obtained implants exhibit hydrophilic properties. This characteristic promotes the adhesion of cells, including osteoblasts, to the implant surface. Analyzing the results presented in
Table 3 reveals that coatings applied directly to magnesium exhibit a higher contact angle compared to coatings formed on an implant previously subjected to the PEO process. The use of the plasma electrolytic oxidation method not only protects the implant from corrosion but also enhances its wettability by reducing the contact angle. The values obtained in the study fall within the range of 0° < θ < 90°, indicating a high level of surface wettability by the liquid. Data are expressed as mean ± SD from three independent measurements per sample (
n = 3).
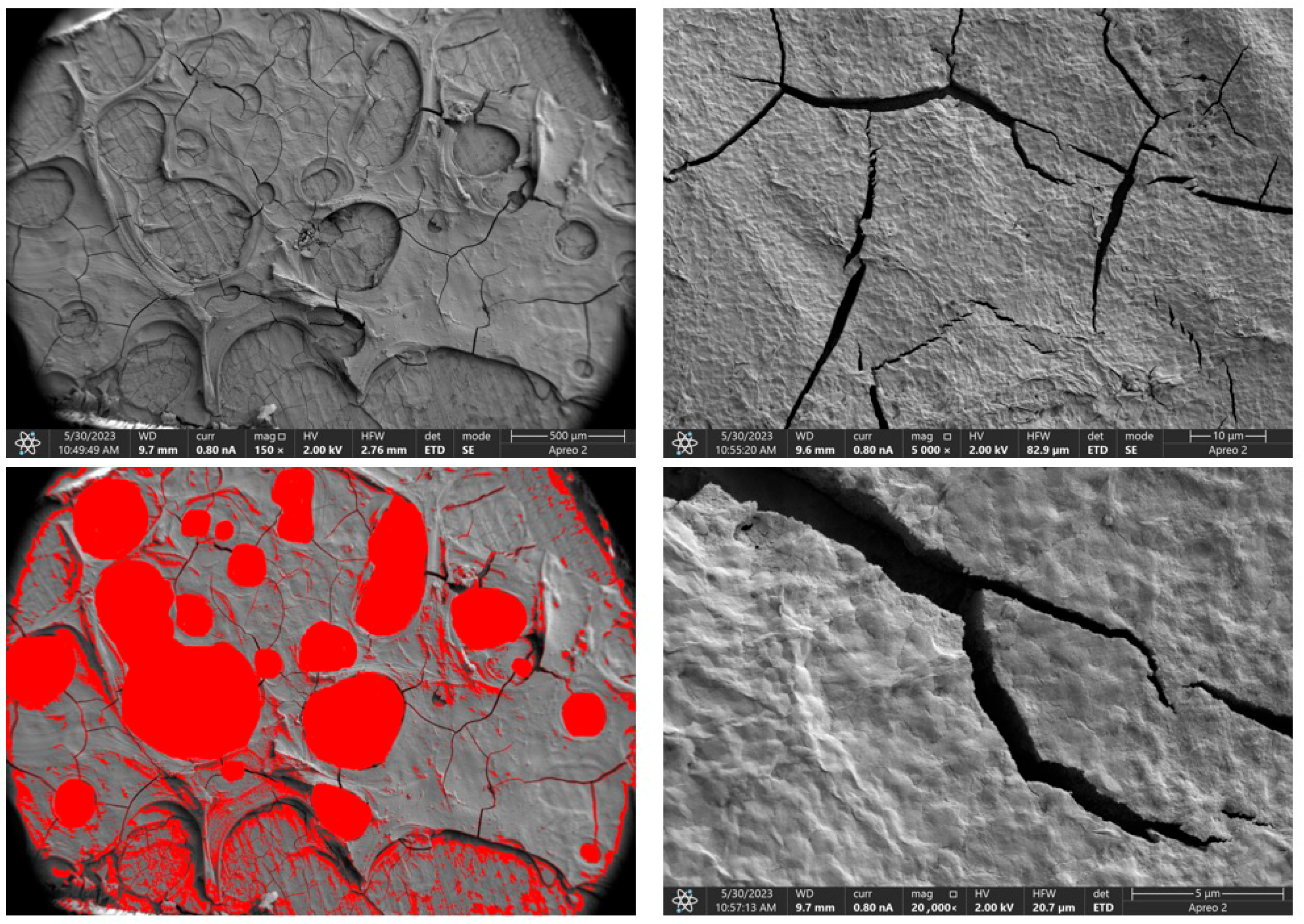
3.3. Surface Morphology and Composition Analysis by Scanning Electron Microscopy (SEM)
Due to the necessity of meeting specific requirements for SEM measurements, a fragment was cut from the entire set of prepared implants using a Dremel straight grinder. This process led to the formation of surface cracks that will not occur under the actual conditions for which the implants are intended. The analysis of implant surface morphology indicates that plasma electrolytic oxidation significantly affects surface structure, enhancing its adhesive properties. This process increases both the number and quality of pores, which promotes better cell adhesion. Magnesium implants modified with a polydopamine (PDA) coating exhibit the most pronounced porosity while also remaining the least damaged during sample preparation, which also suggests high resistance to damage and hardness. Such a structure facilitates easy cell adhesion after implantation. The SEM image of the discussed sample is presented in
Figure 8,
Figure 9,
Figure 10,
Figure 11 and
Figure 12, with pores marked in red. When analyzing chitosan coatings, numerous pores can also be observed; however, their structure differs from that of the polydopamine (PDA) coating. The pores in the PDA layer have an irregular shape and a flat surface, resembling a honeycomb structure. In contrast, the chitosan pores are more compact and resemble a sponge, as seen in
Figure 8,
Figure 9,
Figure 10,
Figure 11 and
Figure 12. In all the examined samples, the porosity level is approximately 50%, indicating that the obtained results meet expectations. The surface of a PEO implant with an applied polydopamine coating shows nanometric pores that remain invisible on the micrometer scale at which the images were taken, as shown in
Figure 13. The illustration shows the formed magnesium oxide layer with clusters of polydopamine embedded in it. SEM images confirmed the porous structure of coatings and revealed topographical differences based on coating composition. An ImageJ analysis of SEM images was used to determine mean pore size (µm) and surface coverage (%). The results showed that PDA-coated samples (Mg_06) had the highest average pore size (3.1 ± 0.4 µm) and surface roughness, contributing to greater osteoblast adhesion potential.
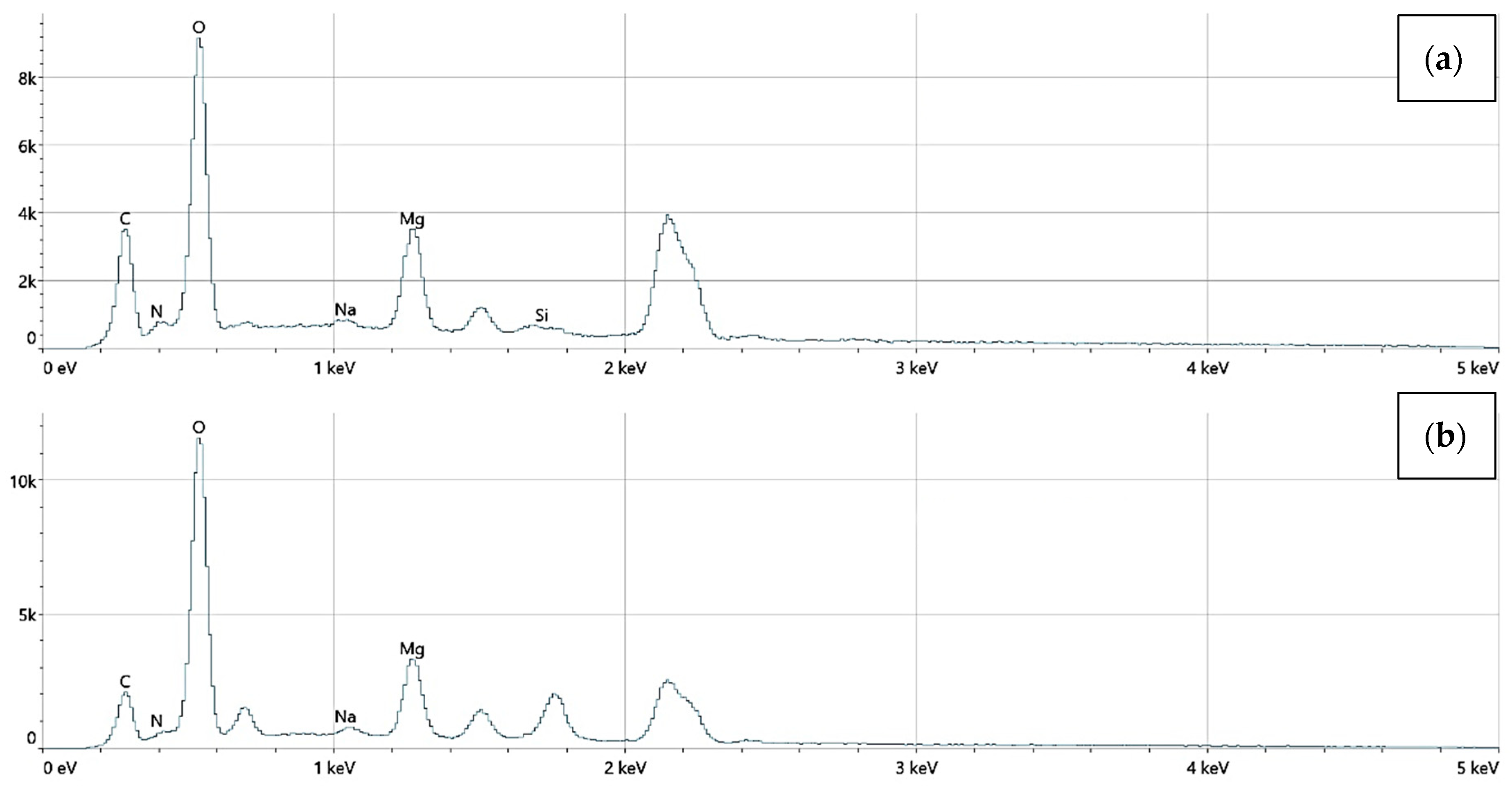
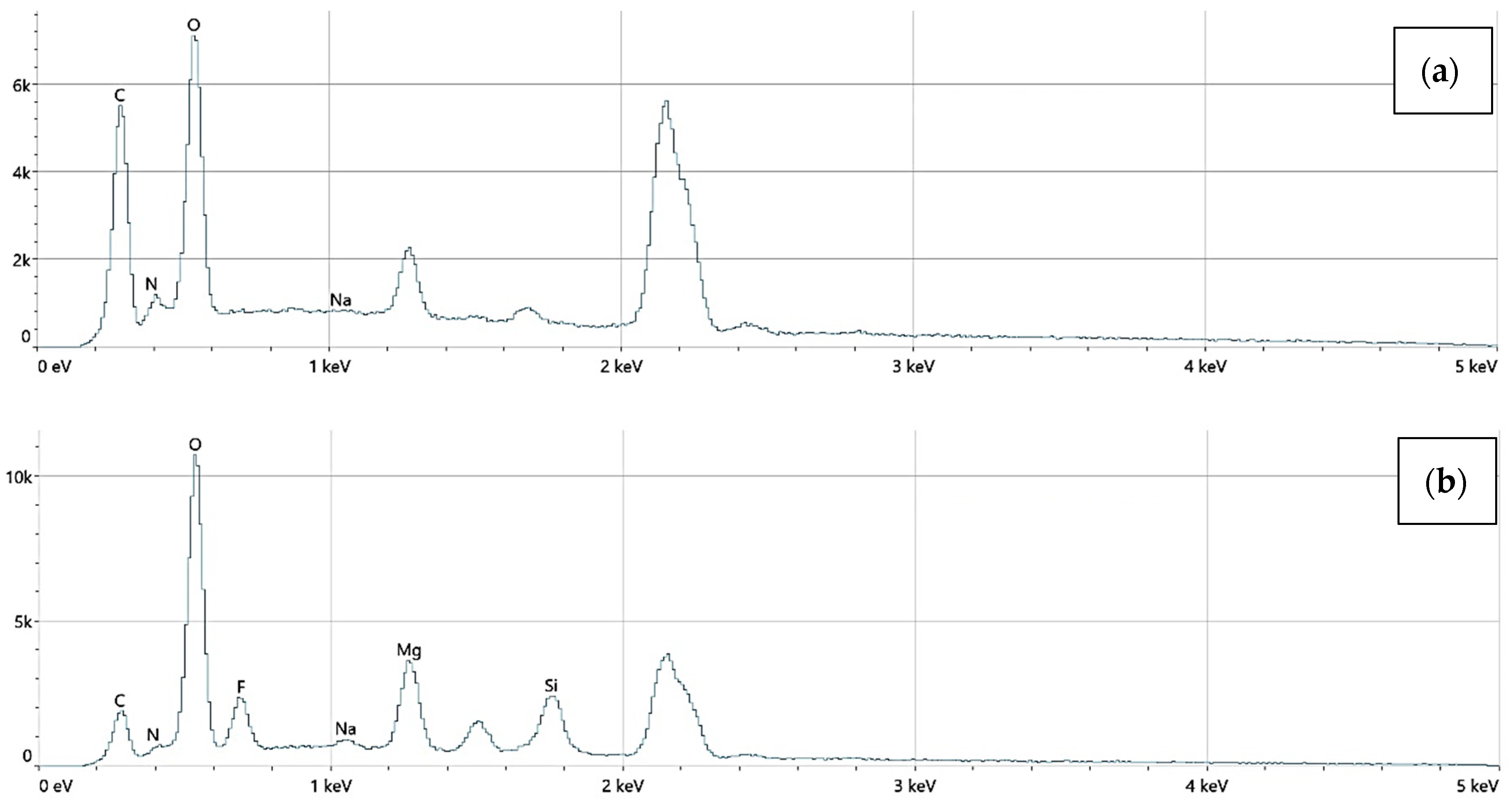
An EDS analysis confirmed the presence of elements including Mg, O, C, N, Si, and Au. No toxic elements were detected in any sample. Mg_06 samples exhibited trace gold signals, verifying the incorporation of AuNPs.
The elemental surface composition analysis showed that all coatings contain elements essential for the human body, which are safe and non-toxic. Below, in
Figure 14, the topography of all the prepared samples is presented, along with the description in
Table 4, which lists the elements found on the surface of the implants.
Figure 15,
Figure 16 and
Figure 17 also show the quantitative elemental composition, confirming, through the EDS system, the presence of biocompatible elements that promote implant integration into the human body.
3.4. Biodegradation and Biocorrosion Analysis
Before implants are introduced into the human body, they are placed in a saline solution to swell the polymer surfaces. This procedure is necessary because, before implantation, it is essential to know the exact dimensions of the implant. This is a crucial requirement to avoid putting the patient at risk of pressure caused by surface swelling inside the body. The biodegradation study showed that each of the obtained implants demonstrates the ability to degrade in vivo. Implants subjected to plasma electrolytic oxidation with polymer coatings exhibit better biodegradation properties over time compared to the others. The best result was achieved by the Mg_06 sample. It degrades significantly slower, which ensures that the hydrogen released would not pose a threat to the patient. The fastest degrading sample was Mg_04, whose degradation was too rapid, and the amount of hydrogen released was the highest and unacceptable.
Figure 18 (below) presents a comparison of the samples after the biodegradation study in SBF.
Biodegradation behavior was assessed by immersing the samples in simulated body fluid (SBF) at 37 °C for 14 days. The mass loss was used to determine degradation rates, with Mg_04 (PEO + chitosan, low viscosity) showing the fastest degradation (22.5% ± 1.8) and Mg_06 (PEO + PDA) showing the slowest (9.1% ± 1.1). These differences were statistically significant (p < 0.01), highlighting the barrier effect of the PDA layer and the protective properties of the PEO-formed oxide. The slower degradation of Mg_06 suggests a reduced release of hydrogen gas, minimizing the risk of soft tissue irritation and promoting implant safety in vivo.
The biocorrosion study was conducted to understand the response of the obtained implants to the action of the patient’s body fluids. The results obtained are presented in the summary
Table 4 and
Figure 18. Analyzing the obtained results, it can be observed that the magnesium implant disc shows a potential of −1.46 V, which is most likely due to the presence of other elements. The summary of all the presented studies is a result that confirms the positive impact of plasma electrolytic oxidation modification. Additionally, as seen in the graph, the corrosion potential of sample Mg_03 is −1.4 V, which is higher than that of the implant after PEO modification with the same coating, i.e., sample Mg_06, whose corrosion potential is −1.15 V. A higher corrosion potential means that the formed magnesium oxide layer is more durable and thicker. The obtained results confirm that the PEO modification plays a key role in improving the biocorrosion properties. It is also important to note the relationship between the corrosion current density (A/cm
2) and corrosion potential (V). A higher corrosion potential is associated with a lower corrosion current density. Biocorrosion analysis was conducted via potentiodynamic polarization testing in SBF, with three replicates per group. The corrosion potential (E_corr) and current density (i_corr) were used to evaluate electrochemical stability. Mg_06 exhibited the most favorable electrochemical behavior with an E_corr value of −1.15 ± 0.02 V and an i_corr value of 4.29 × 10
−5 ± 0.05 × 10
−5 A/cm
2, significantly improved compared to Mg_03 (PDA only), which had an E_corr value of −1.40 ± 0.03 V and an i_corr value of 4.80 × 10
−4 ± 0.09 × 10
−4 A/cm
2. The enhanced corrosion resistance of Mg_06 is attributed to the synergistic effect of the dense oxide layer generated by PEO and the sealing properties of the PDA film, which limits ion diffusion and surface reactivity. Moreover, the solution composition, particularly the presence of Cl
− and HCO
3− ions, plays a critical role in degrading Mg(OH)
2 layers; thus, surface passivation is essential to avoid excessive dissolution.
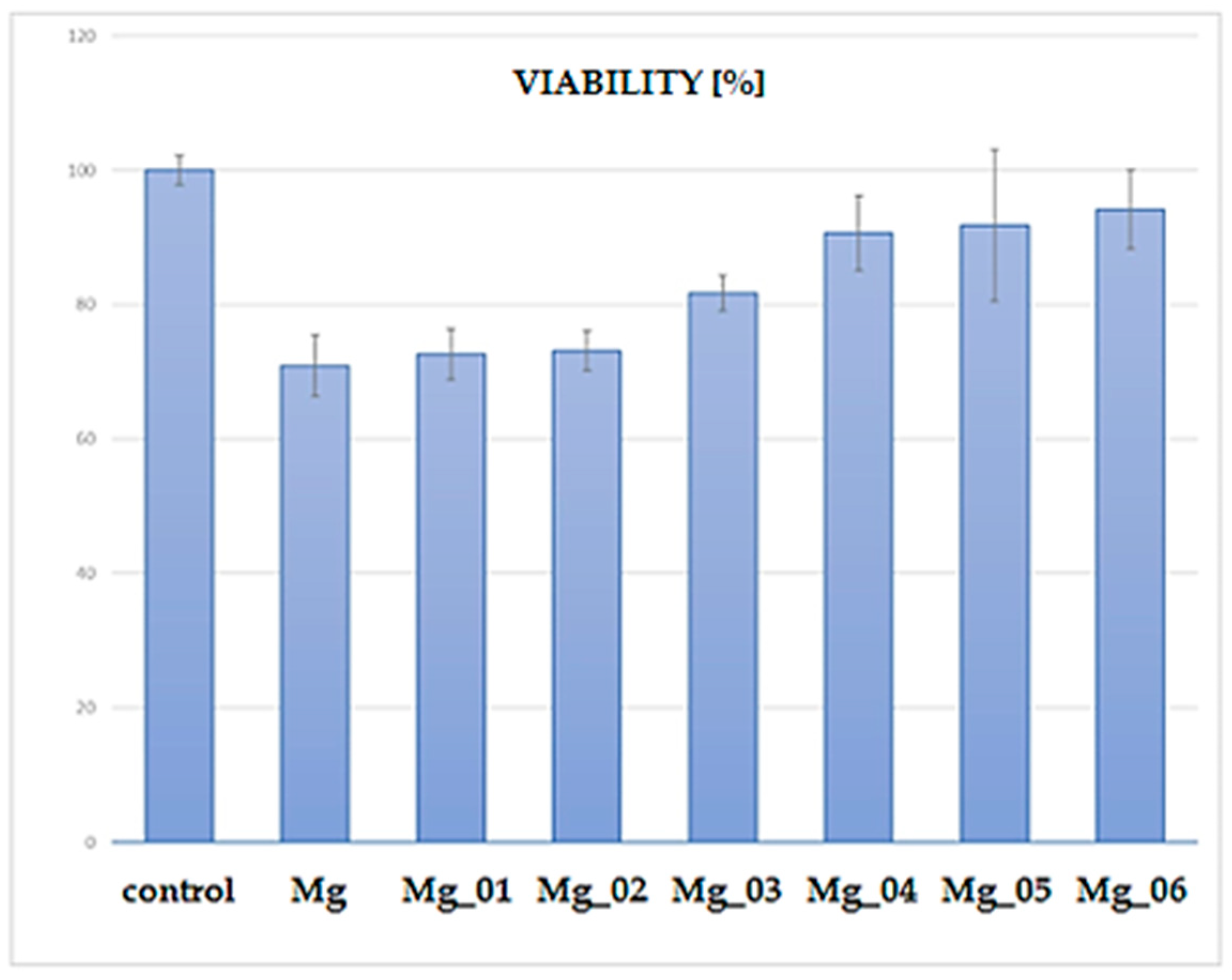
3.5. Cytotoxicity Study
The XTT assay was performed to assess the cytocompatibility of the modified magnesium (Mg) samples by evaluating the viability of cells cultured in the presence of these materials. The results, presented in
Figure 19, indicate a clear trend in cell viability depending on the surface modification applied to the Mg discs. The control group exhibited the highest viability (~100%), as expected for untreated cells. In contrast, the unmodified Mg sample displayed a significant reduction in cell viability, suggesting inherent cytotoxic effects due to rapid degradation and increased ion release leading to an unfavorable microenvironment. Among the modified Mg samples, Mg_01 and Mg_02, which were coated with chitosan and chitosan/polydopamine (PDA), respectively, demonstrated moderate cell viability (~70%). The presence of chitosan, known for its biocompatibility and antibacterial properties, likely contributed to this improved performance compared to uncoated Mg. However, the relatively lower viability compared to other modified samples suggests that these coatings alone were insufficient in fully mitigating Mg’s cytotoxicity. In contrast, Mg_03, coated with PDA alone, exhibited slightly higher viability (~80%) than chitosan-based coatings. Polydopamine, mimicking the adhesive properties of mussel proteins, has been reported to enhance cell adhesion and biocompatibility, which may explain this improvement. A notable increase in viability was observed for samples modified via plasma electrolytic oxidation (PEO) before further chitosan or PDA coatings. Specifically, Mg_04 and Mg_05, which underwent PEO followed by chitosan coatings (low and high viscosity), achieved cell viabilities close to 85–90%. This enhancement is likely due to the formation of a more stable oxide layer, which reduced Mg ion release and improved surface bioactivity. The highest viability (~90–95%) among the modified samples was observed for Mg_06, where PEO was combined with a PDA coating. This suggests that the synergistic effect of PEO surface modification and PDA deposition resulted in the most favorable conditions for cell survival, likely by improving corrosion resistance, reducing ion leaching, and enhancing surface bioactivity. The observed viability trends suggest that surface modification strategies significantly influence the cytocompatibility of Mg-based materials. While unmodified Mg exhibits substantial cytotoxicity, combining PEO with bioactive coatings (particularly PDA) offers a promising route for improving biocompatibility. The improved viability of Mg_06 highlights its potential for biomedical applications, such as biodegradable implants, where controlled degradation and cell-friendly surfaces are essential. Further investigations, including long-term degradation studies and in vivo assessments, are necessary to validate these findings and optimize the coatings for clinical use.
Each sample group (
n = 3) was tested in triplicate wells. The control group was standardized to 100% viability. Among coated samples, Mg_06 demonstrated the highest cell viability at 94.8% ± 1.5, followed by Mg_05 (89.4% ± 1.9) and Mg_04 (85.1% ± 2.3). Samples Mg_01–Mg_03 showed lower viability (~70–79%), with uncoated Mg not included due to known cytotoxicity. The difference between Mg_06 and Mg_01 was statistically significant (
p < 0.01), confirming that the PEO + PDA combination most effectively mitigated Mg-related cytotoxic effects. These results align with the literature indicating that PDA supports osteoblast adhesion by mimicking extracellular matrix interactions [
45,
46,
47], and the PEO barrier reduces ion flux and pH shifts that impair cell viability.
Taken together, the data provide strong evidence that the Mg_06 configuration combining PEO, PDA, and embedded AuNPs offers the best overall performance in terms of corrosion resistance, degradation control, hydrophilicity, and biocompatibility. The study demonstrates that such multi-layered modifications have clear advantages over single-component coatings, positioning them as promising candidates for future clinical translation in biodegradable orthopedic implants.
4. Conclusions
The results of this study demonstrate that the surface functionalization of magnesium implants via plasma electrolytic oxidation (PEO), followed by polymeric coating with polydopamine (PDA), significantly enhances their physicochemical and biological performance. The formation of a robust, porous oxide layer through the PEO process effectively improves corrosion resistance and reduces the uncontrolled release of magnesium ions, which are known to contribute to cytotoxicity and local pH shifts. When combined with a PDA layer, the surface exhibits improved hydrophilicity and bioactivity, supporting higher levels of osteoblastic cell viability and attachment compared to unmodified or singly coated implants. Among all sample groups, the Mg_06 variant—comprising PEO and PDA modifications—showed superior performance in terms of degradation control, electrochemical stability, and cytocompatibility, indicating a favorable interaction between structural stability and biological functionality.
These findings underscore the synergistic potential of combining inorganic and organic surface treatments to optimize the interface between biodegradable magnesium substrates and surrounding biological tissues. The dual-modified surfaces provide not only chemical passivation against premature corrosion but also present a bioinspired environment conducive to cellular interaction, thereby addressing some of the critical limitations associated with bare magnesium implants.
However, while the in vitro data are promising, further research is essential to advance these materials toward clinical application. Future studies should prioritize in vivo investigations to evaluate the biological response under physiological conditions, particularly regarding inflammatory modulation, angiogenic activity, and bone–implant integration over time. Additionally, the long-term mechanical integrity of these coatings under dynamic load-bearing conditions requires thorough evaluation, as does their resistance to delamination and wear. Particular attention should also be given to the immunological effects of degradation products and the stability of nanoparticle-functionalized layers in systemic environments. From a translational perspective, the scalability of the coating processes, reproducibility under manufacturing conditions, and regulatory compliance will also be critical to the clinical implementation of such multifunctional biodegradable implants.
In conclusion, the data presented here provide a strong foundation for the continued development of PEO-based, polymer-functionalized magnesium implants. With appropriate optimization and validation in relevant biological models, these systems hold considerable potential for application in orthopedic, dental, and trauma-related interventions where temporary mechanical support and enhanced tissue compatibility are required.