Theory and Practice in Digital Behaviour Change: A Matrix Framework for the Co-Production of Digital Services That Engage, Empower and Emancipate Marginalised People Living with Complex and Chronic Conditions
Abstract
1. Introduction
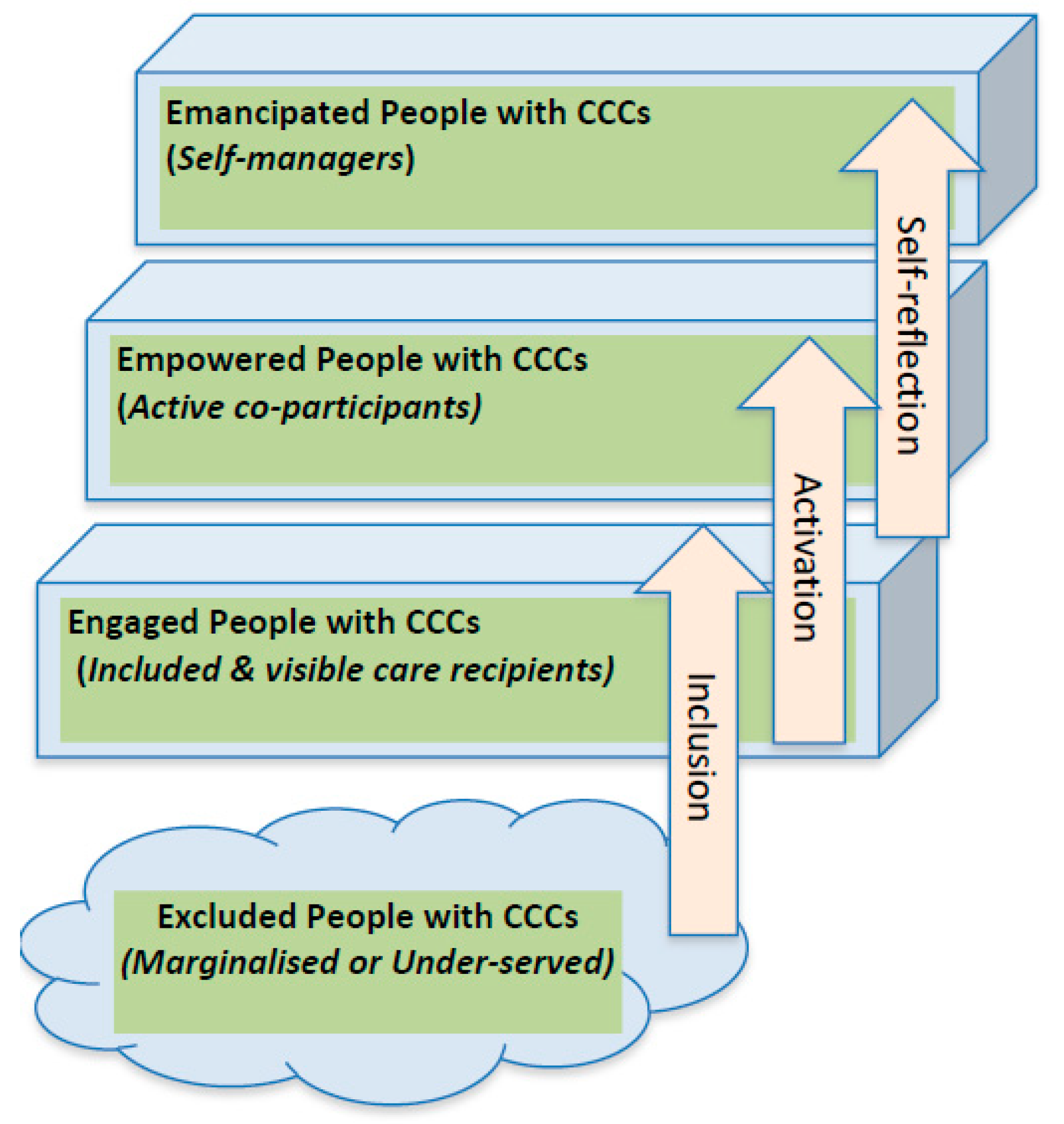
2. From Excluded to Engaged
“If one is truly to succeed in leading a person to a specific place, one must first and foremost take care to find him where he is and begin there”.[10]
“… all true helping begins with a humbling. The helper must first humble himself under the person he wants to help and thereby understand that to help is not to dominate but to serve, that to help is not to be the most dominating but the most patient, that to help is a willingness for the time being to put up with being in the wrong and not understanding what the other understands”.[10]
- (i)
- Finding effective triggers to stimulate social inclusion and initial user engagement and participation in e-health interventions [32];
- (ii)
- Identifying new modes of communication that address information stickiness, health and digital health literacy and aid user interest in sustained behavioural change [33]; and
- (iii)
3. From Engaged to Empowered
“Empowered individuals are able to and motivated for taking action(s) in daily life to the extent that they wish to do so, to improve their health and well-being. A necessary prerequisite is that they are health literate, i.e., have the knowledge and competencies to manage their health and well-being, they are self-aware and can choose to be involved in the co-management of their health, and able to adjust their health-related behaviour if meaningful for them.Health-related empowerment interventions aim to equip individuals and their caregivers whenever appropriate with the capacity to collaborate in decisions related to the condition to the extent that they wish and are able to do so; to enable co-management of the condition; through mutual agreement between the individuals and their formal and informal caregivers; and to develop the individuals confidence and coping skills, enabling them to manage the physical, emotional and social impacts of their condition that affects their everyday life.Empowering interventions foster the development of health literacy among staff and the people that they serve.”[40]
4. From Empowered to Emancipated
5. Readiness for Transitioning
Co-Production of Digital Health Behaviour Change Services: The 4E Matrix Framework
6. Discussion
7. A Demonstration of the Use of the 4E Matrix—The Danish Epital Experience
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kushniruk, A.; Nøhr, C. Participatory Design, User Involvement and Health IT Evaluation. Stud. Health Technol. Inform. 2016, 222, 139–151. [Google Scholar] [CrossRef] [PubMed]
- Batalden, M.; Batalden, P.; Margolis, P.; Seid, M.; Armstrong, G.; Opipari-Arrigan, L.; Hartung, H. Coproduction of healthcare service. BMJ Qual. Saf. 2016, 25, 509–517. [Google Scholar] [CrossRef] [PubMed]
- May, C.R.; Eton, D.T.; Boehmer, K.; Gallacher, K.; Hunt, K.; MacDonald, S.; Mair, F.S.; May, C.M.; Montori, V.M.; Richardson, A.; et al. Rethinking the patient: Using Burden of Treatment Theory to understand the changing dynamics of illness. BMC Health Serv. Res. 2014, 14. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6. [Google Scholar] [CrossRef] [PubMed]
- Webb, T.L.; Joseph, J.; Yardley, L.; Michie, S. Using the Internet to Promote Health Behavior Change: A Systematic Review and Meta-analysis of the Impact of Theoretical Basis, Use of Behavior Change Techniques, and Mode of Delivery on Efficacy. J. Med. Internet Res. 2010, 12, e4. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.; Allen, J.; Bell, R.; Bloomer, E.; Goldblatt, P. WHO European review of social determinants of health and the health divide. Lancet 2012, 380, 1011–1029. [Google Scholar] [CrossRef]
- Coulter, A.; Parsons, S.; Askham, J.; World Health Organization. Regional Office for Europe, European Observatory on Health Systems and Policies. Where Are the Patients in Decision-Making about Their Own care? 2008. Available online: www.who.int/management/general/decisionmaking/WhereArePatientsinDecisionMaking.pdf (accessed on 10 September 2018).
- Mackert, M.; Mabry-Flynn, A.; Champlin, S.; Donovan, E.E.; Pounders, K. Health Literacy and Health Information Technology Adoption: The Potential for a New Digital Divide. J. Med. Internet Res. 2016, 18, e264. [Google Scholar] [CrossRef] [PubMed]
- Mankins, J.C. Technology readiness and risk assessments: A new approach. Acta Astronaut. 2009, 65, 1208–1215. [Google Scholar] [CrossRef]
- Kierkegaard, S.; Hong, E.H.; Hong, H.V. Kierkegaard’s Writings, XXII: The Point of View; Princeton University Press: Princeton, NJ, USA, 2009; ISBN 978-1-4008-3240-8. [Google Scholar]
- Showell, C.; Turner, P. The PLU problem: Are we designing personal ehealth for people like us? Stud. Health Technol. Inform. 2013, 183, 276–280. [Google Scholar] [PubMed]
- Hart, J.T. The inverse care law. Lancet 1971, 1, 405–412. [Google Scholar] [CrossRef]
- Hamine, S.; Gerth-Guyette, E.; Faulx, D.; Green, B.B.; Ginsburg, A.S. Impact of mHealth Chronic Disease Management on Treatment Adherence and Patient Outcomes: A Systematic Review. J. Med. Internet Res. 2015, 17, e52. [Google Scholar] [CrossRef] [PubMed]
- Bossen, D.; Veenhof, C.; Dekker, J.; de Bakker, D. The Effectiveness of Self-Guided Web-Based Physical Activity Interventions among Patients with a Chronic Disease: A Systematic Review. J. Phys. Act. Health 2014, 11, 665–677. [Google Scholar] [CrossRef] [PubMed]
- Elliot, A.J.; Mooney, C.J.; Douthit, K.Z.; Lynch, M.F. Predictors of Older Adults’ Technology Use and Its Relationship to Depressive Symptoms and Well-being. J. Gerontol. B Psychol. Sci. Soc. Sci. 2014, 69, 667–677. [Google Scholar] [CrossRef] [PubMed]
- Bertelsen, P.; Kanstrup, A.M.; Madsen, J. Steps toward Technology Design to Beat Health Inequality—Participatory Design Walks in a Neighbourhood with High Health Risks. Stud. Health Technol. Inform. 2017, 233, 158–172. [Google Scholar] [PubMed]
- Kanstrup, A.M.; Bertelsen, P.; Madsen, J.Ø. Design with the feet: Walking methods and participatory design. In Proceedings of the 13th Participatory Design Conference, Windhoek, Namibia, 4–10 October 2014; Volume 1, pp. 51–60. [Google Scholar]
- Davy, C.; Bleasel, J.; Liu, H.; Tchan, M.; Ponniah, S.; Brown, A. Effectiveness of chronic care models: Opportunities for improving healthcare practice and health outcomes: A systematic review. BMC Health Serv. Res. 2015, 15. [Google Scholar] [CrossRef] [PubMed]
- Karppinen, P.; Oinas-Kukkonen, H.; Alahäivälä, T.; Jokelainen, T.; Keränen, A.-M.; Salonurmi, T.; Savolainen, M. Persuasive user experiences of a health Behavior Change Support System: A 12-month study for prevention of metabolic syndrome. Int. J. Med. Inf. 2016, 96, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Arnrich, B.; Mayora, O.; Bardram, J.; Tröster, G. Pervasive Healthcare: Paving the Way for a Pervasive, User-centered and Preventive Healthcare Model. Methods Inf. Med. 2010, 49, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Fogg, B. A behavior model for persuasive design. In Proceedings of the 4th International Conference on Persuasive Technology, Claremont, CA, USA, 26–29 April 2009; ACM Press: New York, NY, USA, 2009; p. 1. [Google Scholar]
- Halpern, D.; Service, O.; Thaler, R. Inside the Nudge Unit: How Small Changes Can Make a Big Difference; WH Allen: London, UK, 2016; ISBN 978-0-7535-5655-9. [Google Scholar]
- Voyer, B. “Nudging” behaviours in healthcare: Insights from behavioural economics. Br. J. Healthc. Manag. 2015, 21, 130–135. [Google Scholar] [CrossRef]
- Yee, K.C.; Wong, M.C.; Turner, P. Pokemon Go: Ubiquitous Computing Delivering Better Health or Co-Incidental Health Benefits from Technology Use? A Participatory Observational Study. Stud. Health Technol. Inform. 2017, 234, 389–394. [Google Scholar] [PubMed]
- Glasemann, M.; Kanstrup, A.M.; Ryberg, T. Making chocolate-covered broccoli: Designing a mobile learning game about food for young people with diabetes. In Proceedings of the Conference on Designing Interactive Systems, Aarhus, Denmark, 16–20 August 2010; ACM Press: New York, NY, USA, 2010; p. 262. [Google Scholar]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Kayser, L.; Kushniruk, A.; Osborne, R.H.; Norgaard, O.; Turner, P. Enhancing the Effectiveness of Consumer-Focused Health Information Technology Systems Through eHealth Literacy: A Framework for Understanding Users’ Needs. JMIR Hum. Factors 2015, 2, e9. [Google Scholar] [CrossRef] [PubMed]
- Batterham, R.W.; Hawkins, M.; Collins, P.A.; Buchbinder, R.; Osborne, R.H. Health literacy: Applying current concepts to improve health services and reduce health inequalities. Public Health 2016, 132, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Osborne, R.; Kayser, L. Skills and characteristics of the e-health literate patient. BMJ 2018, k1656. [Google Scholar] [CrossRef] [PubMed]
- Morison, E.E. Men, Machines, and Modern Times; M.I.T. Press: Cambridge, MA, USA, 2008; ISBN 978-0-262-13025-7. [Google Scholar]
- Kleijnen, M.; Lee, N.; Wetzels, M. An exploration of consumer resistance to innovation and its antecedents. J. Econ. Psychol. 2009, 30, 344–357. [Google Scholar] [CrossRef]
- Craig Lefebvre, R.; Tada, Y.; Hilfiker, S.W.; Baur, C. The Assessment of User Engagement with eHealth Content: The eHealth Engagement Scale1. J. Comput. Mediat. Commun. 2010, 15, 666–681. [Google Scholar] [CrossRef]
- Elwyn, G.; Taubert, M.; Kowalczuk, J. Sticky knowledge: A possible model for investigating implementation in healthcare contexts. Implement. Sci. 2007, 2. [Google Scholar] [CrossRef] [PubMed]
- Warsi, A.; Wang, P.S.; LaValley, M.P.; Avorn, J.; Solomon, D.H. Self-management education programs in chronic disease: A systematic review and methodological critique of the literature. Arch. Intern. Med. 2004, 164, 1641–1649. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Ham, C. Improving Care for People with Long-Term Conditions: A Review of UK and International Frameworks; University of Birmingham, Health Services Management Centre: Birmingham, UK, 2005; ISBN 0-7044-2584-X. [Google Scholar]
- Wodchis, W.P.; Dixon, A.; Anderson, G.M.; Goodwin, N. Integrating care for older people with complex needs: key insights and lessons from a seven-country cross-case analysis. Int. J. Integr. Care 2015, 15. [Google Scholar] [CrossRef]
- Scott, K.; Simonds, A. Psychosocial and Cultural Factors Influencing Patient Education. Health Educ. Monogr. 1968, 1, 9–28. [Google Scholar] [CrossRef]
- Scott, K. Simonds Health education and medical care: Focus on the patient. Health Educ. Monogr. 1963, 1, 32–40. [Google Scholar]
- Cummings, E.; Turner, P. Patients at the centre: Methodological considerations for evaluating evidence from health interventions involving patients use of web-based information systems. Open Med. Inform. J. 2010, 4, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Kayser, L.; Karnoe, A.; Duminski, E.; Somekh, D.; Vera-Munoz, C. A new understanding of empowerment in a health context. 2018; submitted. [Google Scholar]
- Eskildsen, N.B.; Joergensen, C.R.; Thomsen, T.G.; Ross, L.; Dietz, S.M.; Groenvold, M.; Johnsen, A.T. Patient empowerment: A systematic review of questionnaires measuring empowerment in cancer patients. Acta Oncol. 2017, 56, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Sheldon, K.M.; Elliot, A.J. Goal striving, need satisfaction, and longitudinal well-being: The self-concordance model. J. Pers. Soc. Psychol. 1999, 76, 482–497. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.O.; Velicer, W.F. The transtheoretical model of health behavior change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Zoffmann, V.; Hörnsten, Å.; Storbækken, S.; Graue, M.; Rasmussen, B.; Wahl, A.; Kirkevold, M. Translating person-centered care into practice: A comparative analysis of motivational interviewing, illness-integration support, and guided self-determination. Patient Educ. Couns. 2016, 99, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, B.; Currey, J.; Haigh, B.; Dunning, T.; Zoffmann, V. An online self-management intervention for young adults with type 1 diabetes: Guided Self-Determination program. Aust. Diabetes Educ. 2017, 20, 1–9. [Google Scholar]
- Habermas, J.; Shapiro, J.J. Knowledge and Human Interests; Beacon Press: Boston, MA, USA, 1971; ISBN 978-0-8070-1541-4. [Google Scholar]
- Botin, L.; Bertelsen, P.; Nøhr, C. (Eds.) Techno-Anthropology in Health Informatics: Methodologies for Improving Human-Technology Relations; Studies in health technology and informatics; IOS Press: Amsterdam, The Netherland; Washington, DC, USA, 2015; ISBN 978-1-61499-559-3. [Google Scholar]
- Nohr, C.; Botin, L.; Zhu, X.X. How Can Health Information Technologies Contribute to Improve Health Care Services for High-Need Patients? Stud. Health Technol. Inform. 2017, 241, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Pezdek, K.; Rasiński, L. Between exclusion and emancipation: Foucault’s ethics and disability. Nurs. Philos. 2017, 18, e12131. [Google Scholar] [CrossRef] [PubMed]
- Raymaker, D.M. Intersections of Critical Systems Thinking and Community Based Participatory Research: A Learning Organization Example with the Autistic Community. Syst. Pract. Action Res. 2016, 29, 405–423. [Google Scholar] [CrossRef] [PubMed]
- Showell, C.; Cummings, L.; Turner, P. The Invisibility of Disadvantage: Why Do We Not Notice? Stud. Health Technol. Inform. 2017, 388–392. [Google Scholar] [CrossRef]
- Gulbrandsen, P.; Clayman, M.L.; Beach, M.C.; Han, P.K.; Boss, E.F.; Ofstad, E.H.; Elwyn, G. Shared decision-making as an existential journey: Aiming for restored autonomous capacity. Patient Educ. Couns. 2016, 99, 1505–1510. [Google Scholar] [CrossRef] [PubMed]
- Fredriksson, M.; Eriksson, M.; Tritter, J. Who wants to be involved in health care decisions? Comparing preferences for individual and collective involvement in England and Sweden. BMC Public Health 2018, 18. [Google Scholar] [CrossRef] [PubMed]
- Medibank. Australians Giving up on Living in Good Health. 2014. Available online: https://www.medibank.com.au/content/about/media-centre/2014/07/australians-giving-up-on-a-healthy-life/jcr%3acontent/par/download/file.res/MED14005_HEALTH_CHECK_2_FINAL.pdf (accessed on 10 September 2018).
- Willis, K.F.; Robinson, A.; Wood-Baker, R.; Turner, P.; Walters, E.H. Participating in Research: Exploring Participation and Engagement in a Study of Self-Management for People with Chronic Obstructive Pulmonary Disease. Qual. Health Res. 2011, 21, 1273–1282. [Google Scholar] [CrossRef] [PubMed]
- Tomes, N. Patient empowerment and the dilemmas of late-modern medicalisation. Lancet 2007, 369, 698–700. [Google Scholar] [CrossRef]
- Kelder, J.; Turner, P. Lost in Translation? Critical Reflection on Qualitative Approaches for Informing Information Systems Design. In Proceedings of the QuallIT2005: Challenges for Qualitative Research, Brisbane, Australia, 23–25 November 2005. [Google Scholar]
- Valentijn, P.P.; Schepman, S.M.; Opheij, W.; Bruijnzeels, M.A. Understanding integrated care: A comprehensive conceptual framework based on the integrative functions of primary care. Int. J. Integr. Care 2013, 13, e010. [Google Scholar] [CrossRef] [PubMed]
- Åberg, A.; Halvorsen, K.; From, I.; Bruhn, Å.; Oestreicher, L.; Melander-Wikman, A. A Study Protocol for Applying User Participation and Co-Learning—Lessons Learned from the eBalance Project. Int. J. Environ. Res. Public Health 2017, 14, 512. [Google Scholar] [CrossRef] [PubMed]
- Visek, A.J.; Achrati, S.M.; Mannix, H.M.; McDonnell, K.; Harris, B.S.; DiPietro, L. The Fun Integration Theory: Toward Sustaining Children and Adolescents Sport Participation. J. Phys. Act. Health 2015, 12, 424–433. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.C.; Turner, P.; MacIntyre, K.; Yee, K.C. Pokémon-Go: Why Augmented Reality Games Offer Insights for Enhancing Public Health Interventions on Obesity-Related Diseases. Stud. Health Technol. Inform. 2017, 241, 128–133. [Google Scholar] [PubMed]
- Broers, V.J.V.; De Breucker, C.; Van den Broucke, S.; Luminet, O. A systematic review and meta-analysis of the effectiveness of nudging to increase fruit and vegetable choice. Eur. J. Public Health 2017, 27, 912–920. [Google Scholar] [CrossRef] [PubMed]
- VicHealth. Behavioural Insights and Healthier Lives; Victorian Health Promotion Foundation: Melbourne, Australia, 2016. Available online: https://www.vichealth.vic.gov.au/media-and-resources/publications/behavioural-insights-and-healthier-lives (accessed on 10 September 2018).
- Almond, H.; Cummings, E.; Turner, P. Avoiding Failure for Australia’s Digital Health Record: The Findings from a Rural E-Health Participatory Research Project. Stud. Health Technol. Inform. 2016, 227, 8–13. [Google Scholar] [CrossRef] [PubMed]
- WHO Framework on Integrated People-Centred Health Services, a Report by the Secretariat. Available online: http://www.who.int/servicedeliverysafety/areas/people-centred-care/en/ (accessed on 11 May 2017).
- Hibbard, J.H.; Stockard, J.; Mahoney, E.R.; Tusler, M. Development of the Patient Activation Measure (PAM): Conceptualizing and Measuring Activation in Patients and Consumers: Development of the Patient Activation Measure (PAM). Health Serv. Res. 2004, 39, 1005–1026. [Google Scholar] [CrossRef] [PubMed]
- Osborne, R.H.; Elsworth, G.R.; Whitfield, K. The Health Education Impact Questionnaire (heiQ): An outcomes and evaluation measure for patient education and self-management interventions for people with chronic conditions. Patient Educ. Couns. 2007, 66, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Osborne, R.H.; Batterham, R.W.; Elsworth, G.R.; Hawkins, M.; Buchbinder, R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 2013, 13, 658. [Google Scholar] [CrossRef] [PubMed]
- Kayser, L.; Karnoe, A.; Furstrand, D.; Batterham, R.; Christensen, K.B.; Elsworth, G.; Osborne, R.H. A Multidimensional Tool Based on the eHealth Literacy Framework: Development and Initial Validity Testing of the eHealth Literacy Questionnaire (eHLQ). J. Med. Internet Res. 2018, 20, e36. [Google Scholar] [CrossRef] [PubMed]
- Phanareth, K.; Vingtoft, S.; Christensen, A.S.; Nielsen, J.S.; Svenstrup, J.; Berntsen, G.K.R.; Newman, S.P.; Kayser, L. The Epital Care Model: A New Person-Centered Model of Technology-Enabled Integrated Care for People with Long Term Conditions. JMIR Res. Protoc. 2017, 6, e6. [Google Scholar] [CrossRef] [PubMed]
- Lindskrog, S.; Christensen, K.B.; Osborne, R.H.; Vingtoft, S.; Phanareth, K.; Kayser, L. How patient reported outcome measures from heiQ, HLQ and SF-36 can be used to follow people with COPD in an ehealth based 24/7 service, the ‘Epital Care Model’. J. Med. Internet Res. under review.
- McCabe, C.; McCann, M.; Brady, A.M. Computer and mobile technology interventions for self-management in chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2017. [Google Scholar] [CrossRef] [PubMed]

| Levels | Excluded | Engaged | Empowered | Emancipated | |||
|---|---|---|---|---|---|---|---|
| Individual Personal and social contexts | Unattended | Social inclusion | Pro-active responses tailored to the attributes and contexts of DDDs. (e.g., Participatory Design (PD) Walks; Fun Theory) | Activation of Literacy (textual, technical, health) | Pro-actively supporting increased literacy, self-determination and empowerment. (e.g., Guided Self-Determination) | Self-Reflection | Users pro-actively lead choices of behaviour and lifestyle with their chronic conditions. |
| Provider Interactions with health and care providers | Unrecorded | Social interactions co-designed through response to DDDs needs, preferences and capabilities (e.g., Nudging) | Social interactions framed to target empowerment of DDDs (e.g., Behaviour Change Support System) | Interactions are user-led and health professionals become facilitators of individual self-management strategies. (e.g., Wagner, WHO) | |||
| Health System System interactions with health services and technology | Unaware | Systems and technologies designed to pro-actively ensure inclusion of DDDs. (e.g., SDOH, HIA and CBPR) | Health services and technology re-designed to pro-actively support DDDs. (e.g., Picker Institute) | Health service and technology innovation led by users facilitated by the system. (e.g., Von Hippel; Christensen) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kayser, L.; Nøhr, C.; Bertelsen, P.; Botin, L.; Villumsen, S.; Showell, C.; Turner, P. Theory and Practice in Digital Behaviour Change: A Matrix Framework for the Co-Production of Digital Services That Engage, Empower and Emancipate Marginalised People Living with Complex and Chronic Conditions. Informatics 2018, 5, 41. https://doi.org/10.3390/informatics5040041
Kayser L, Nøhr C, Bertelsen P, Botin L, Villumsen S, Showell C, Turner P. Theory and Practice in Digital Behaviour Change: A Matrix Framework for the Co-Production of Digital Services That Engage, Empower and Emancipate Marginalised People Living with Complex and Chronic Conditions. Informatics. 2018; 5(4):41. https://doi.org/10.3390/informatics5040041
Chicago/Turabian StyleKayser, Lars, Christian Nøhr, Pernille Bertelsen, Lars Botin, Sidsel Villumsen, Chris Showell, and Paul Turner. 2018. "Theory and Practice in Digital Behaviour Change: A Matrix Framework for the Co-Production of Digital Services That Engage, Empower and Emancipate Marginalised People Living with Complex and Chronic Conditions" Informatics 5, no. 4: 41. https://doi.org/10.3390/informatics5040041
APA StyleKayser, L., Nøhr, C., Bertelsen, P., Botin, L., Villumsen, S., Showell, C., & Turner, P. (2018). Theory and Practice in Digital Behaviour Change: A Matrix Framework for the Co-Production of Digital Services That Engage, Empower and Emancipate Marginalised People Living with Complex and Chronic Conditions. Informatics, 5(4), 41. https://doi.org/10.3390/informatics5040041







