The Development and Evaluation of the Application for Assessing the Fall Risk Factors and the Suggestion to Prevent Falls in Older Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Population, Inclusion, and Exclusion Criteria
- (1)
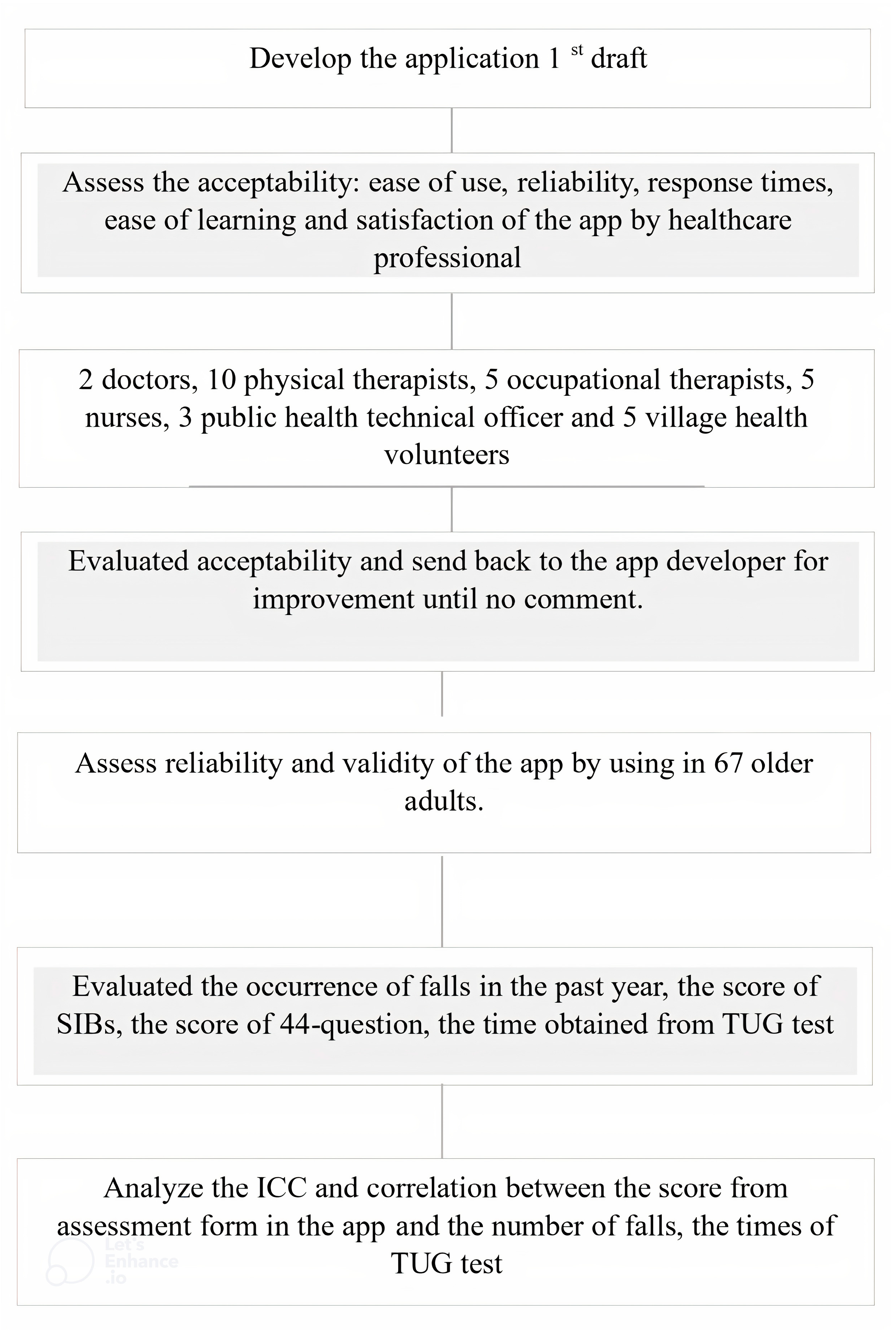
- A total of 30 healthcare professionals, including 2 doctors, 10 physical therapists, 5 occupational therapists, 5 nurses, 3 public health technical officers, and 5 village health volunteers, all of whom had more than five years of professional experience in their respective fields.
- (2)
- The study population consisted of 3569 older adults aged 60 and above, residing in Thasala District, Nakhon Si Thammarat Province. The inclusion criteria were living in their own residence and proficient in Thai, with access to the Internet. Those who were unable to do everyday activities and those who had dementia were excluded. Daily functional ability was assessed using the Barthel Index of Activities of Daily Living. A score of 4 or below (out of 20) indicated total dependence and was used as an exclusion criterion. Cognitive screening was performed using the Mini-Mental State Examination (MMSE-Thai 2002). Participants were excluded if their scores indicated cognitive impairment, defined as follows: a score of ≤14 out of 23 for those with no formal education; ≤17 out of 23 for those with education up to 7th grade; and ≤22 out of 23 for those with education beyond 8th grade.
2.3. Subject and Sample Size
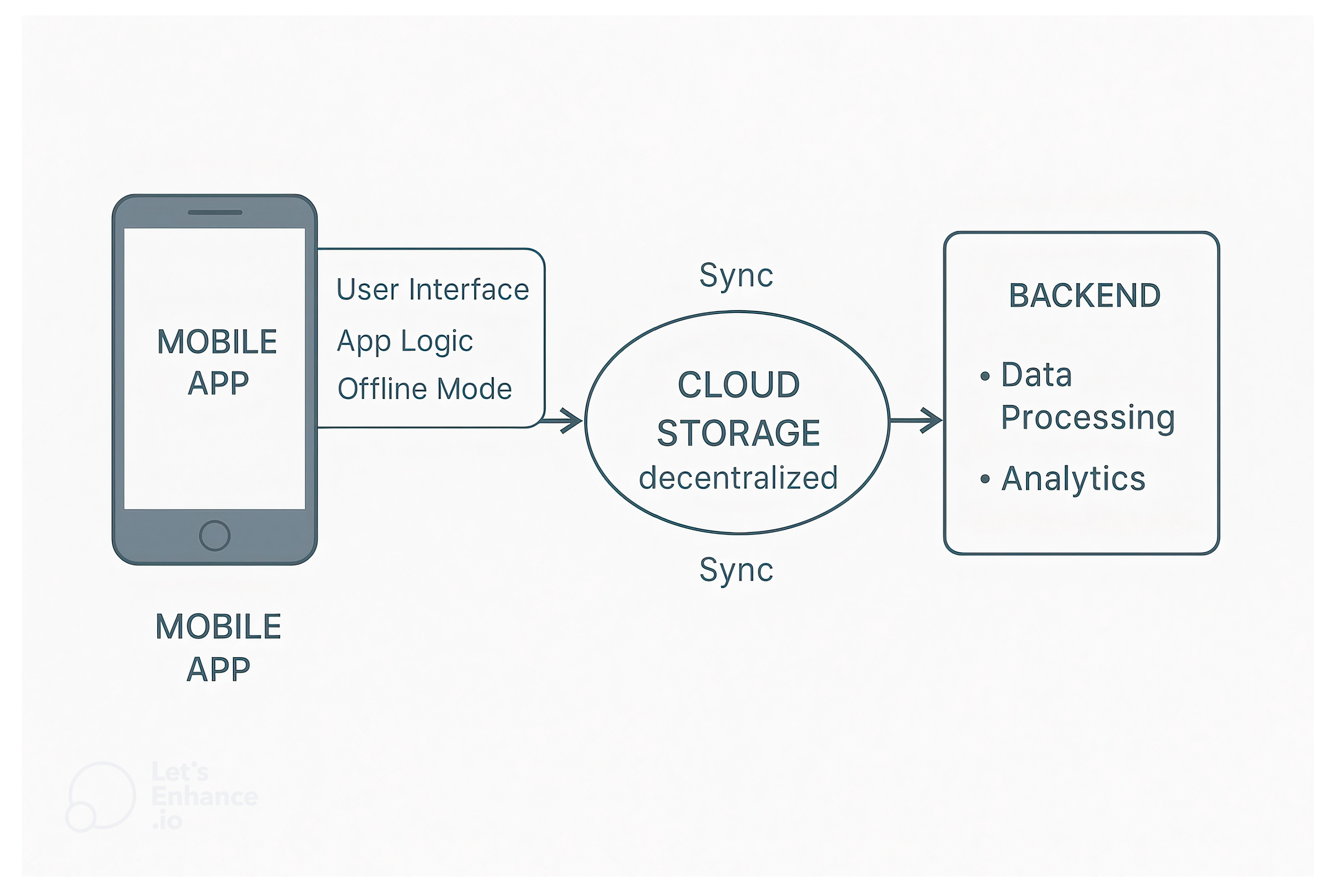
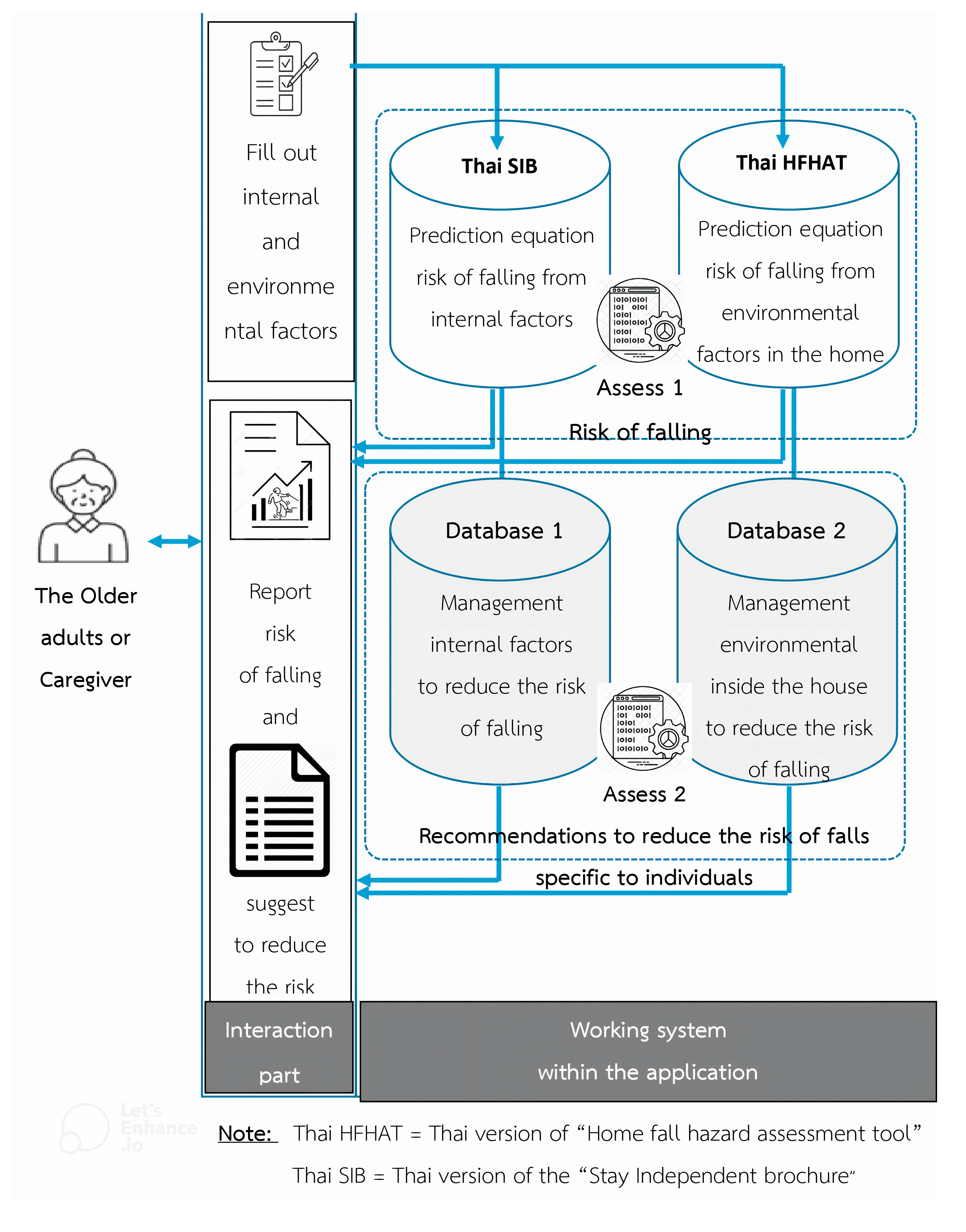
2.4. Application Development and System Architecture
2.5. Outcome and Tools
| Outcomes | Detail, Tools, and Measure Method |
| Health Professional outcomes | |
| Ease of Use | Users can access the app easily, not complicated. |
| Reliability | Consistency of the app operation under various conditions. |
| Response Times | How fast the response time of the app from the user request to the response time. |
| Ease of learning | Users can easily learn how to assess falls risk and how to solve them. |
| Satisfaction | Users evaluate the overall satisfaction of the app. |
| End-user outcomes | |
| The occurrence of overall and indoor fall events within the past year | Falls and the details of any falls from the past year are collected. Data included the fall place, circumstances of the fall, injury, and treatment. Participants are interviewed by researchers. |
| The score from the 44-question Thai-HFHAT | Participants’ indoor home environments are evaluated using a 44-item checklist. |
| The score from the Stay Independent Brochure (SIB) | Participants assessed themselves using the SIB checklist. |
| Time Up and Go test (TUG) | Used to assess the risk of falls. Participants are evaluated by researchers. |
2.6. Data Collection
2.6.1. Phase I
2.6.2. Phase II
2.7. Statistical and Data Analysis
- (1)
- The quantitative data were analyzed using descriptive statistics, reporting the result as frequency and percentage.
- (2)
- The qualitative data were analyzed from open questions using thematic analysis. The qualitative data were read, re-read, then coded and collated under the items related to acceptability: ease of use, reliability, response times, ease of learning, and satisfaction with the app. A second researcher confirmed the coding.
- (3)
- The test–retest reliability was analyzed using statistics Intraclass Correlation Coefficient model 3, 1 (ICC3, 1). Reliability was interpreted according to standard criteria, with ICC values ≥ 0.75 indicating good reliability.
- (4)
- The correlation between the number of falls in the past year and the time from the TUG test was analyzed with the score from SIB (Thai-version) and the score from the 44-question Thai-HFHAT. Prior to correlation analysis, the normality of continuous data was assessed using the Shapiro–Wilk test. Since the data did not meet normal distribution assumptions, non-parametric methods were applied. Spearman’s rank correlation coefficient was used to examine the association between the number of falls in the past year, TUG test time, and scores from the SIB (Thai-version) and 44-item Thai-HFHAT. A significance level (α) of 0.05 was applied, and p-values < 0.05 were considered statistically significant.
3. Results
3.1. Phase 1: Application Development
3.1.1. The Characteristics of Healthcare Professionals
3.1.2. System Usability Evaluation
3.1.3. Performance Analytics and User Behavior
3.1.4. Health Professional Satisfaction and Suggestion
- (1)
- Some older adults may experience vision or reading difficulties, suggesting the need for an audio-assisted feature to read questions aloud.
- (2)
- An example should be provided, or a video with images and audio should be included to guide users.
- (3)
- There is a spelling error.
- (4)
- Part 2 requires clearer instructions to guide users on the intended actions.
- (5)
- The letters are too small, and the font color should be adjusted to be different from the background.
3.2. Phase 2: Applying Application to Older Adults
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Report on Falls Prevention in Older Age; WHO: Geneva, Switzerland, 2007. [Google Scholar]
- World Health Organization. Ageing and Health Fact Sheet; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Srichang, N.; Kawee, L. Fall Forecast Report for Elderly (Aged 60 Years and Over) in Thailand, 2017–2021; Division of Non-Communicable Diseases, Department of Disease Control, Ministry of Public Health: Bangkok, Thailand, 2017.
- Kallin, K.; Lundin-Olsson, L.; Jensen, J.; Nyberg, L.; Gustafson, Y. Predisposing and precipitating factors for falls among older people in residential care. Public. Health 2002, 116, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Kitkumhang, V.; Kittimanon, N.; Pannarunothai, S. Risk factors of fall in elderly in the community. J. Health Sci. 2006, 15, 787–799. (In Thai) [Google Scholar]
- Sophonratanapokin, B.; Sawangdee, Y.; Soonthorndhada, K. Effect of the living environment on falls among the elderly in Thailand. Southeast Asian J. Trop. Med. Public. Health 2012, 43, 1537–1547. [Google Scholar]
- National Institute for Health and Care Excellence. Clinical Guideline 21, Falls: The Assessment and Prevention of Falls in Older People; NICE: London, UK, 2004. [Google Scholar]
- Pynoos, J.; Steinman, B.A.; Nguyen, A.Q. Environmental assessment and modification as fall-prevention strategies for older adults. Clin. Geriatr. Med. 2010, 26, 633–644. [Google Scholar] [CrossRef]
- Loonlawong, S.; Limroongreungrat, W.; Jiamjarasrangsi, W. The Stay Independent Brochure as a screening evaluation for fall risk in an elderly Thai population. Clin. Interv. Aging 2019, 14, 2155–2162. [Google Scholar] [CrossRef] [PubMed]
- Lektip, C.; Lapmanee, S.; Rattananupong, T.; Lohsoonthorn, V.; Vorayingyong, A.; Woratanarat, T.; Sirisuk, K.-O.; Suttanon, P.; Petsirasan, R.; Kitidumrongsuk, P.; et al. Predictive validity of three home fall hazard assessment tools for older adults in Thailand. PLoS ONE 2020, 15, e0244729. [Google Scholar] [CrossRef] [PubMed]
- NCES. Global Digital Population as of April 2021 (in Millions) Statista: The Statistics Portal. Available online: https://www.statista.com/statistics/617136/digital-population-worldwide/ (accessed on 20 January 2023).
- NCES. Number of Smartphone Users Worldwide from 2016 to 2020 (in Billions) Statista: The Statistics Portal. Available online: https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/ (accessed on 20 January 2023).
- United Nations Thailand. Social Impact Assessment of COVID-19 in Thailand; United Nations Thailand: Bangkok, Thailand, 2020. (In Thai) [Google Scholar]
- Institute for Population and Social Research. Situation of the Thai Elderly 2017; Mahidol University: Nakhon Pathom, Thailand, 2018. (In Thai) [Google Scholar]
- Bitar, H.; Alismail, S. The role of eHealth, telehealth, and telemedicine for chronic disease patients during COVID-19 pandemic: A rapid systematic review. Digit. Health 2021, 7, 20552076211009396. [Google Scholar] [CrossRef]
- Hong, Y.; Lee, S.H. Effectiveness of tele-monitoring by patient severity and intervention type in chronic obstructive pulmonary disease patients: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2019, 92, 1–15. [Google Scholar] [CrossRef]
- Omboni, S.; Ballatore, T.; Rizzi, F.; Tomassini, F.; Panzeri, E.; Campolo, L. Telehealth at scale can improve chronic disease management in the community during a pandemic: An experience at the time of COVID-19. PLoS ONE 2021, 16, e0258015. [Google Scholar] [CrossRef]
- Pech, M.; Sauzeon, H.; Yebda, T.; Benois-Pineau, J.; Amieva, H. Falls Detection and Prevention Systems in Home Care for Older Adults: Myth or Reality? JMIR Aging 2021, 4, e29744. [Google Scholar] [CrossRef]
- Delbaere, K.; Valenzuela, T.; Lord, S.R.; Clemson, L.; Zijlstra, G.A.R.; Close, J.C.T.; Lung, T.; Woodbury, A.; Chow, J.; McInerney, G.; et al. E-health StandingTall balance exercise for fall prevention in older people: Results of a two year randomised controlled trial. BMJ 2021, 373, n740. [Google Scholar] [CrossRef]
- Subramaniam, S.; Faisal, A.I.; Deen, M.J. Wearable Sensor Systems for Fall Risk Assessment: A Review. Front. Digit. Health 2022, 4, 921506. [Google Scholar] [CrossRef]
- Hsieh, K.L.; Chen, L.; Sosnoff, J.J. Mobile Technology for Falls Prevention in Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2023, 78, 861–868. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The Timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Dennison, L.; Morrison, L.; Conway, G.; Yardley, L. Opportunities and challenges for smartphone applications in supporting health behavior change: Qualitative study. J. Med. Internet Res. 2013, 15, e86. [Google Scholar] [CrossRef]
- Yardley, L.; Beyer, N.; Hauer, K.; Kempen, G.; Piot-Ziegler, C.; Todd, C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005, 34, 614–619. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Holden, R.J.; Karsh, B.T. The technology acceptance model: Its past and its future in health care. J. Biomed. Inform. 2010, 43, 159–172. [Google Scholar] [CrossRef]
- Mitzner, T.L.; Boron, J.B.; Fausset, C.B.; Adams, A.E.; Charness, N.; Czaja, S.J.; Dijkstra, K.; Fisk, A.D.; Rogers, W.A.; Sharit, J. Older adults talk technology: Technology usage and attitudes. Comput. Human. Behav. 2010, 26, 1710–1721. [Google Scholar] [CrossRef]
- Wittayapun, Y.; Nawarat, J.; Lapmanee, S.; Mackenzie, L.; Lektip, C. Reliability of the 44-question Home Fall Hazard Assessment Tool and demographic characteristics associated with home hazards among the Thai elderly. F1000Research 2023, 12, 8. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Hendrickson, A.R.; Massey, P.D.; Cronan, T.P. On the Test-Retest Reliability of Perceived Usefulness and Perceived Ease of Use Scales. MIS Q. 1993, 17, 227–230. [Google Scholar] [CrossRef]
- Vu, T.V.; Mackenzie, L. The inter-rater and test-retest reliability of the Home Falls and Accidents Screening Tool. Aust. Occup. Ther. J. 2012, 59, 235–242. [Google Scholar] [CrossRef]
- Thiamwong, L.; Thamarpirat, J.; Maneesriwongul, W.; Jitapunkul, S. Thai falls risk assessment test (Thai-FRAT) developed for community-dwelling Thai elderly. J. Med. Assoc. Thai 2008, 91, 1823–1831. [Google Scholar]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go test. Phys. Ther. 2000, 80, 896–903. [Google Scholar]
- Lustria, M.L.; Cortese, J.; Noar, S.M.; Glueckauf, R.L. Computer-tailored health interventions delivered over the web: Review and analysis of key components. Patient Educ. Couns. 2009, 74, 156–173. [Google Scholar] [CrossRef]
- Krebs, P.; Prochaska, J.O.; Rossi, J.S. A meta-analysis of computer-tailored interventions for health behavior change. Prev. Med. 2010, 51, 214–221. [Google Scholar] [CrossRef]
- de Vries, H.; Brug, J. Computer-tailored interventions motivating people to adopt health promoting behaviours: Introduction to a new approach. Patient Educ. Couns. 1999, 36, 99–195. [Google Scholar]
- Hawkins, R.P.; Kreuter, M.; Resnicow, K.; Fishbein, M.; Dijkstra, A. Understanding tailoring in communicating about health. Health Educ. Res. 2008, 23, 454–466. [Google Scholar] [CrossRef]

| Health Professionals (n) | Gender (Female %) | Age (mean ± SD) | Year of Service (mean ± SD) |
|---|---|---|---|
| Doctors (2) | 50 | 41.50 ± 4.90 | 7.00 ± 1.41 |
| Physical therapists (10) | 50 | 31.90 ± 4.01 | 7.50 ± 3.92 |
| Occupational therapists (5) | 80 | 32.40 ± 5.50 | 7.80 ± 2.58 |
| Nurse (5) | 100 | 38.40 ± 11.01 | 11.40 ± 7.20 |
| Public health technical officers (3) | 100 | 29.67 ± 2.51 | 5.67 ± 2.52 |
| Village health volunteers (5) | 60 | 54.80 ± 11.08 | 12.40 ± 5.59 |
| Items | Number of Health Professionals (%) | ||||
|---|---|---|---|---|---|
| 5 | 4 | 3 | 2 | 1 | |
| |||||
| 26.67 | 53.33 | 20.00 | 0 | 0 |
| 13.33 | 50.00 | 36.67 | 0 | 0 |
| 53.33 | 40.00 | 6.67 | 0 | 0 |
| 40.00 | 32.50 | 27.50 | 0 | 0 |
| 43.33 | 43.33 | 13.34 | 0 | 0 |
| |||||
| 56.67 | 33.33 | 10.00 | 0 | 0 |
| |||||
| 60.00 | 36.67 | 3.33 | 0 | 0 |
| |||||
| 20.00 | 63.33 | 16.67 | 0 | 0 |
| 43.33 | 50.00 | 6.67 | 0 | 0 |
| Demographic Characteristics | Non Falling (n = 43) | Falling (n = 24) | p-Value |
|---|---|---|---|
| n (%) | n (%) | ||
| Age (years) | 0.554 | ||
| Mean ± SD | 67.98 ± 6.09 | 68.79 ± 5.98 | |
| Min–Max | 60–90 | 59–80 | |
| Gender | 0.405 | ||
| Male | 13 (30.23) | 5 (20.83) | |
| Female | 30 (69.77) | 19 (79.17) | |
| BMI (kg/m2) | 0.122 | ||
| Mean ± SD | 25.13 ± 3.63 | 24.32 ± 2.74 | |
| Min–Max | 17.71–32.46 | 19.82–29.49 | |
| Educations Level | 0.471 | ||
| Primary education | 18 (41.86) | 13 (54.17) | |
| Above primary education | 25 (58.14) | 11 (45.83) | |
| Marital Status | 0.116 | ||
| Single | 5 (11.63) | 2 (8.34) | |
| Married/Living Together | 32 (74.42) | 11 (45.83) | |
| Divorced/Separated/Widowed | 6 (13.95) | 11 (45.83) | |
| Occupation | 0.261 | ||
| Unemployed/Housewife | 12 (27.91) | 2 (8.34) | |
| Trade/Laborer | 10 (23.25) | 3 (12.50) | |
| Retired Government Official | 7 (16.28) | 5 (20.83) | |
| Farmer | 14 (32.56) | 14 (58.33) | |
| Congenital disease | 0.867 | ||
| No chronic disease | 5 (11.63) | 2 (8.34) | |
| Diabetes | 12 (27.90) | 6 (25.00) | |
| Hypertension | 20 (46.52) | 9 (37.50) | |
| High blood cholesterol | 4 (9.30) | 4 (16.66) | |
| Others (e.g., heart disease, gout, rheumatoid arthritis | 2 (4.65) | 3 (12.50) | |
| Number of falling | |||
| Mean ± SD | 1.46 ± 0.93 | ||
| Min–Max | 1–5 | ||
| 1 times | 17 (70.83) | ||
| 2 times | 5 (20.83) | ||
| 3 times | 1 (4.17) | ||
| 5 times | 1 (4.17) | ||
| Variable | Correlation Coefficient | p-Value |
|---|---|---|
| SIB Score (Thai-version) | 0.657 | <0.001 |
| 44-question Thai-HFHAT Score | 0.709 | <0.001 |
| Variable | Correlation Coefficient | p-Value |
|---|---|---|
| SIB Score (Thai-version) | 0.656 | <0.001 |
| 44-question Thai-HFHAT Score | 0.632 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lektip, C.; Jiamjarasrangsi, W.; Kaewrat, C.; Nawarat, J.; Rungruangbaiyok, C.; Mackenzie, L.; Somsak, V.; Wannaprom, N. The Development and Evaluation of the Application for Assessing the Fall Risk Factors and the Suggestion to Prevent Falls in Older Adults. Informatics 2025, 12, 53. https://doi.org/10.3390/informatics12020053
Lektip C, Jiamjarasrangsi W, Kaewrat C, Nawarat J, Rungruangbaiyok C, Mackenzie L, Somsak V, Wannaprom N. The Development and Evaluation of the Application for Assessing the Fall Risk Factors and the Suggestion to Prevent Falls in Older Adults. Informatics. 2025; 12(2):53. https://doi.org/10.3390/informatics12020053
Chicago/Turabian StyleLektip, Charupa, Wiroj Jiamjarasrangsi, Charlee Kaewrat, Jiraphat Nawarat, Chadapa Rungruangbaiyok, Lynette Mackenzie, Voravuth Somsak, and Nipaporn Wannaprom. 2025. "The Development and Evaluation of the Application for Assessing the Fall Risk Factors and the Suggestion to Prevent Falls in Older Adults" Informatics 12, no. 2: 53. https://doi.org/10.3390/informatics12020053
APA StyleLektip, C., Jiamjarasrangsi, W., Kaewrat, C., Nawarat, J., Rungruangbaiyok, C., Mackenzie, L., Somsak, V., & Wannaprom, N. (2025). The Development and Evaluation of the Application for Assessing the Fall Risk Factors and the Suggestion to Prevent Falls in Older Adults. Informatics, 12(2), 53. https://doi.org/10.3390/informatics12020053








