Metronidazole-Induced Encephalopathy in a 16-Year-Old Girl with Crohn’s Disease: Case Report and Review of the Pediatric Literature
Abstract
1. Introduction
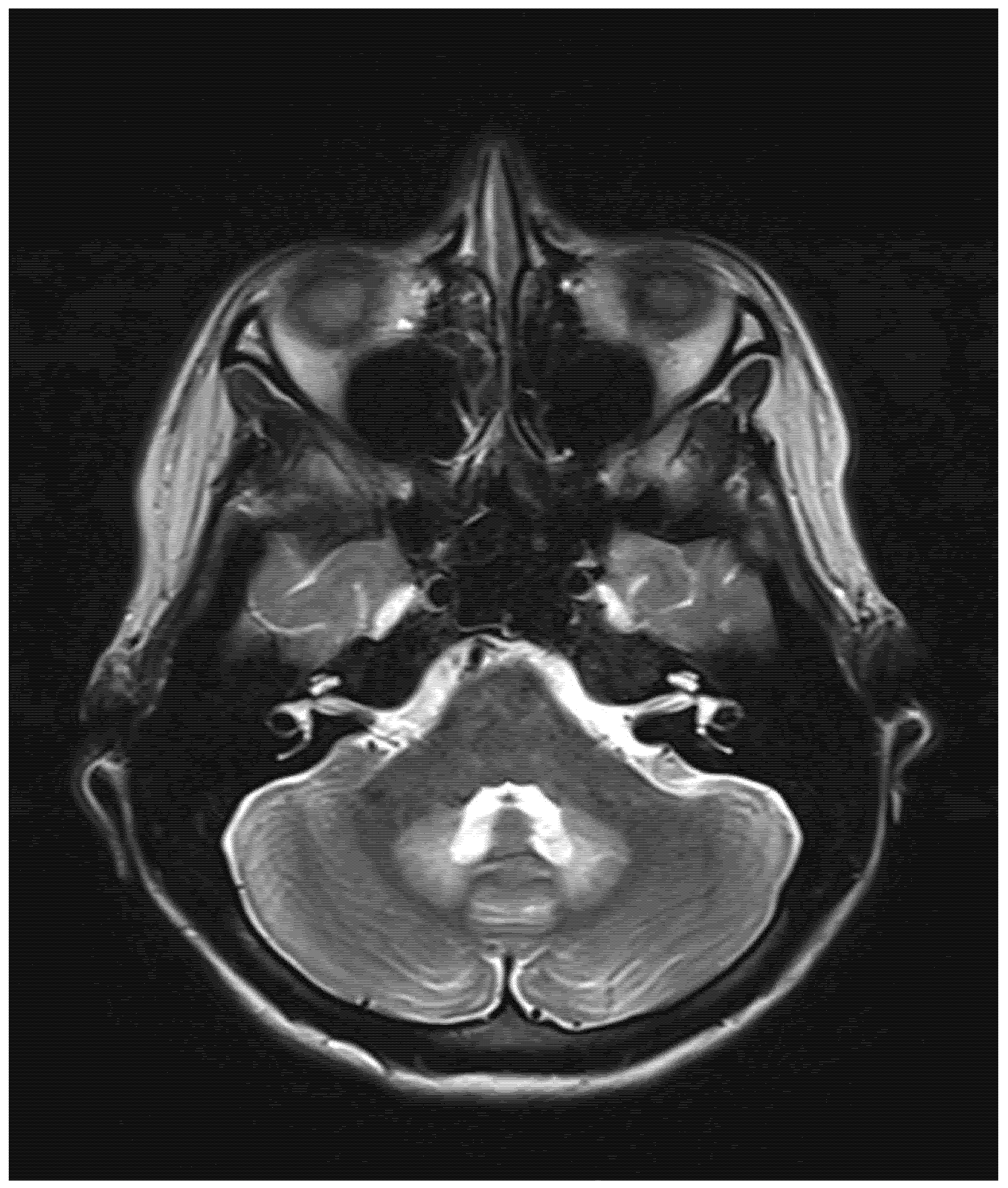
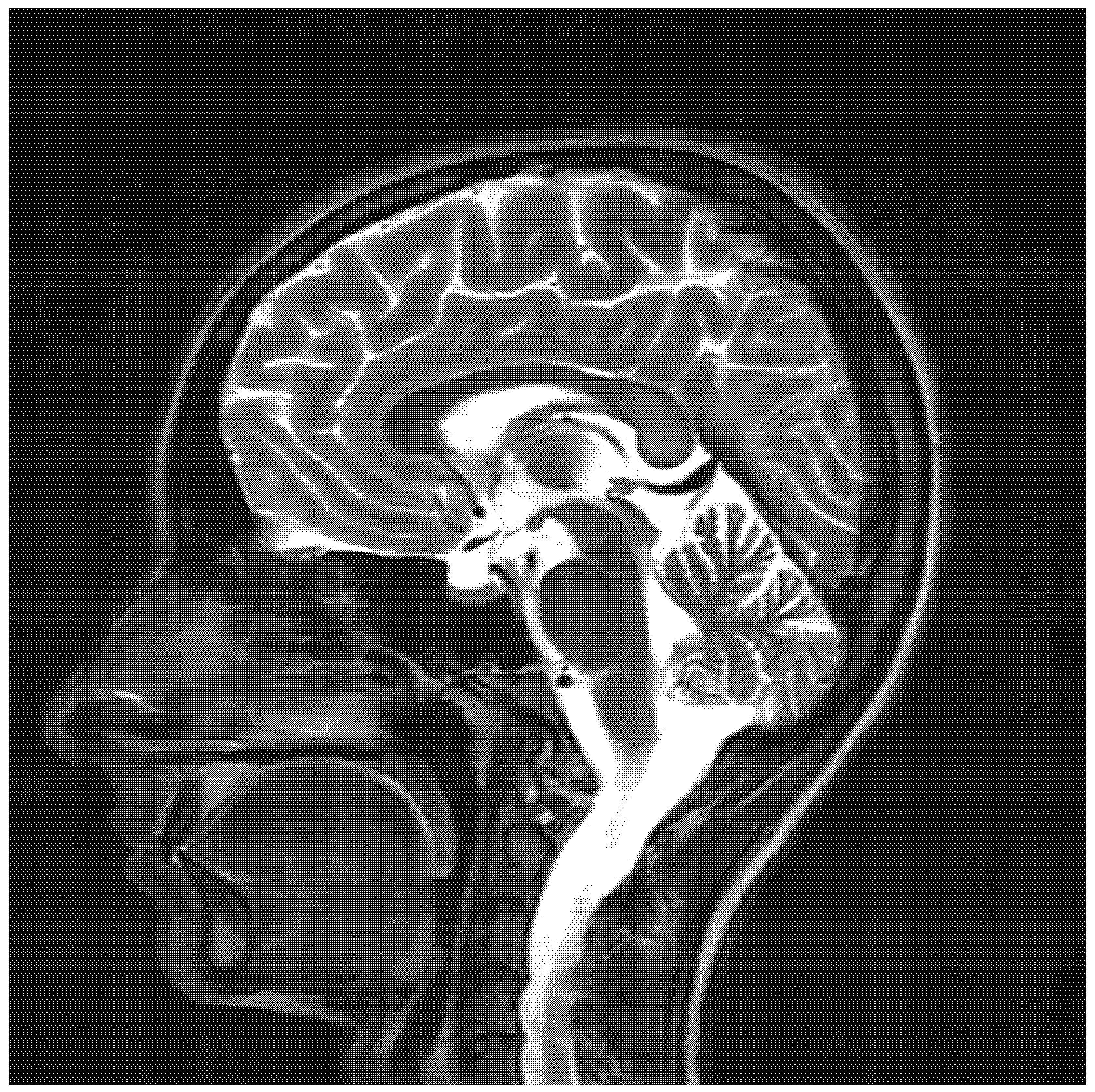
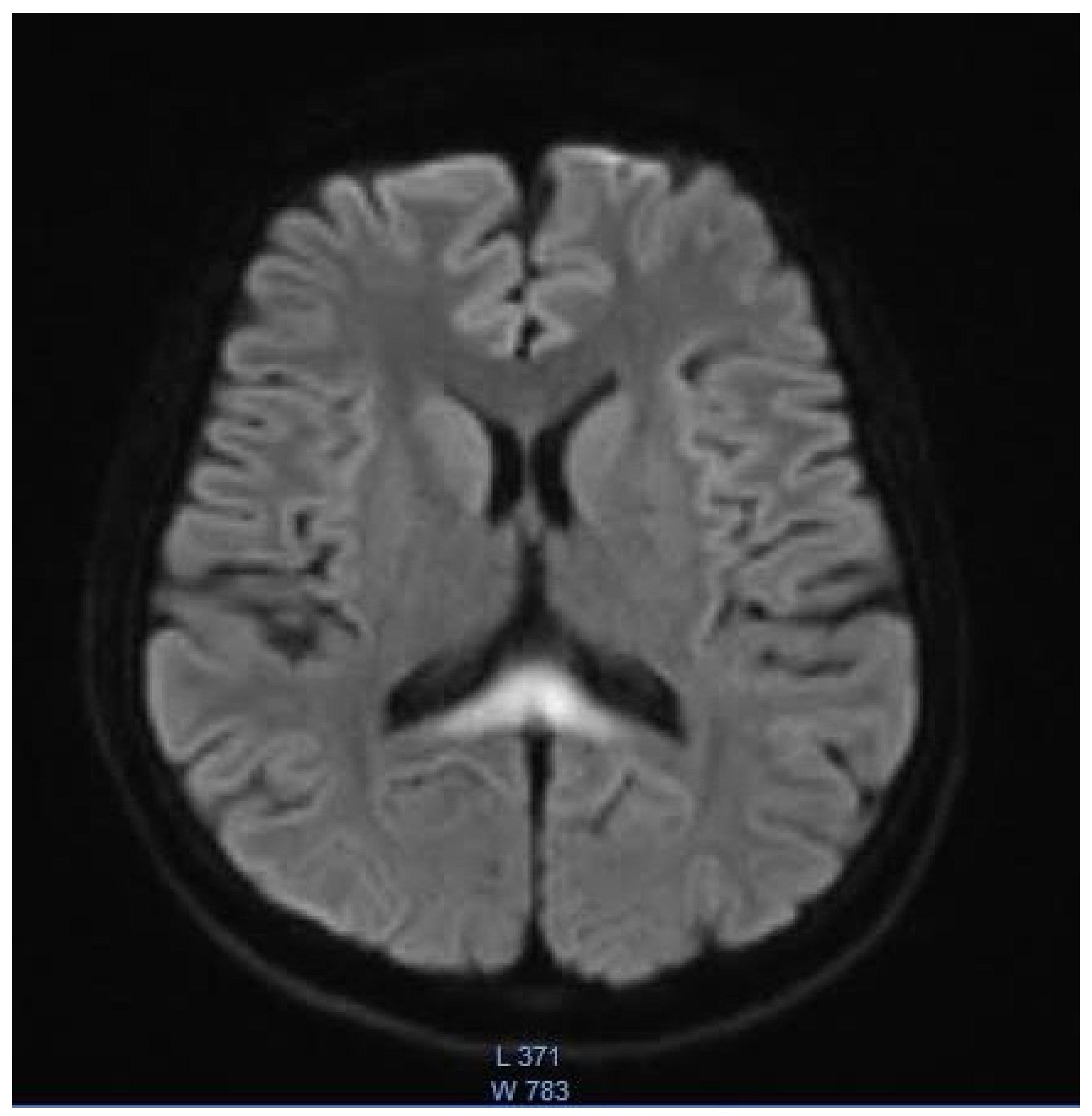
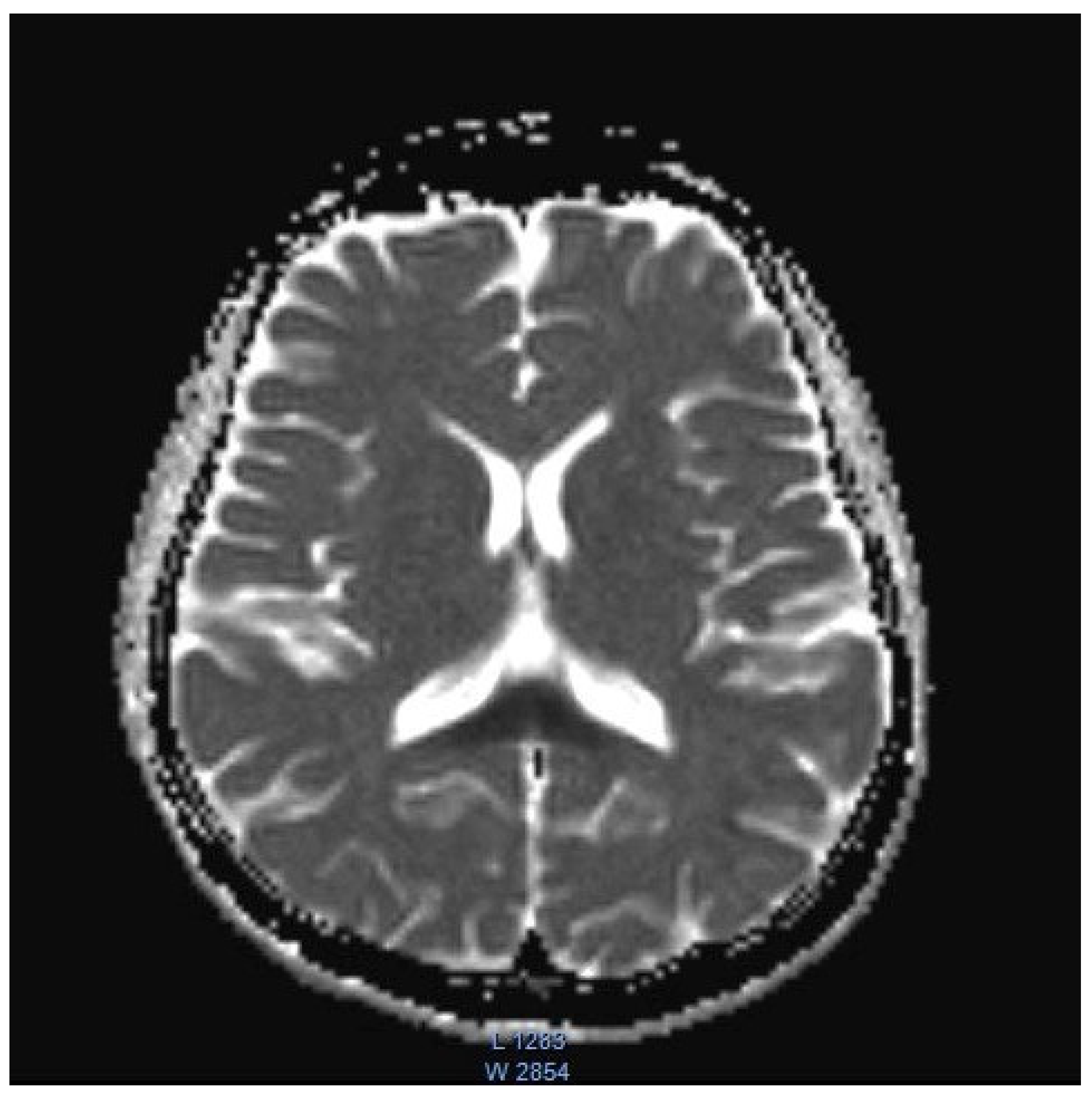
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bailes, J.; Willis, J.; Priebe, C.; Strub, R. Encephalopathy With Metronidazole in a Child. Arch. Pediatr. Adolesc. Med. 1983, 137, 290–291. [Google Scholar] [CrossRef] [PubMed]
- Bates, J.E.; Almast, J.; Augustine, E.F. Neonatal dentate nucleus T2 hyperintensity after in utero metronidazole exposure. Neurology 2015, 85, 1006. [Google Scholar] [CrossRef] [PubMed]
- Cecil, K.M.; Halsted, M.J.; Schapiro, M.; Dinopoulos, A.; Jones, B.V. Reversible MR Imaging and MR Spectroscopy Abnormalities in Association with Metronidazole Therapy. J. Comput. Assist. Tomogr. 2002, 26, 948–951. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.Y.; Borchert, M.S. Cortical Visual Impairment Treated by Plasmapheresis in a Child With Metronidazole-Induced Encephalopathy. J. Neuro-Ophthalmol. 2019, 41, e66–e68. [Google Scholar] [CrossRef] [PubMed]
- Chatzkel, J.A.; Vossough, A. Metronidazole-induced cerebellar toxicity. Pediatr. Radiol. 2009, 40, 1453. [Google Scholar] [CrossRef]
- Gaye, A.; Sanghavi, A. Metronidazole-Induced Encephalopathy in a Pediatric Patient. J. Allergy Clin. Immunol. 2007, 119, S38. [Google Scholar] [CrossRef]
- Kafadar, I.; Moustafa, F.; Yalçn, K.; Klç, B.A. A Rare Adverse Effect of Metronidazole. Pediatr. Emerg. Care 2013, 29, 751–752. [Google Scholar] [CrossRef]
- Omrani, A.; Rohani, M.; Hosseinpour, S.; Tavasoli, A.R. Persistent dystonia and basal ganglia involvement following metronidazole induced encephalopathy. Neurol. Sci. 2019, 41, 957–959. [Google Scholar] [CrossRef]
- Patel, L.; Batchala, P.; Almardawi, R.; Morales, R.; Raghavan, P. Acute metronidazole-induced neurotoxicity: An update on MRI findings. Clin. Radiol. 2019, 75, 202–208. [Google Scholar] [CrossRef]
- Starrs, M.E.; Yenigun, O.M. Metronidazole, an Uncommon Cause of Dizziness and Ataxia in the Emergency Department: A Case Report. Clin. Pract. Cases Emerg. Med. 2021, 2, 239–241. [Google Scholar] [CrossRef]
- Garg, A.; Sudan, Y.S.; Gupta, R.; Bansal, A.R. Headphone sign: Metronidazole-induced encephalopathy. Neurol. India 2016, 64, 1374–1376. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Overby, P.J.; Mehta, H. Case 271: Metronidazole-induced Encephalopathy. Radiology 2019, 293, 473–479. [Google Scholar] [CrossRef] [PubMed]
- Yazdani, R.M.; Kayfan, S.; Cao, J.; Clarke, R.L.; Pfeifer, C.M. MRI findings of metronidazole neurotoxicity in a pediatric patient with chronic diarrhea. Radiol. Case Rep. 2018, 14, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Van Rheenen, P.F.; Aloi, M.; Assa, A.; Bronsky, J.; Escher, J.C.; Fagerberg, U.L.; Gasparetto, M.; Gerasimidis, K.; Griffiths, A.; Henderson, P.; et al. The Medical Management of Paediatric Crohn’s Disease: An ECCO-ESPGHAN Guideline Update. J. Crohn’s Coliti 2021, 15, 171–194. [Google Scholar] [CrossRef] [PubMed]
- Turner, D.; Ricciuto, A.; Lewis, A.; D’Amico, F.; Dhaliwal, J.; Griffiths, A.M.; Bettenworth, D.; Sandborn, W.J.; Sands, B.E.; Reinisch, W.; et al. STRIDE-II: An Update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) Initiative of the International Organization for the Study of IBD (IOIBD): Determining Therapeutic Goals for Treat-to-Target strategies in IBD. Gastroenterology 2021, 160, 1570–1583. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, C.G.; Karlsson, W.K.; Amin, F.M.; Lindelof, M. Metronidazole-induced encephalopathy: A systematic review. J. Neurol. 2018, 267, 1–13. [Google Scholar] [CrossRef]
- Kuriyama, A.; Jackson, J.L.; Doi, A.; Kamiya, T. Metronidazole-Induced Central Nervous System Toxicity. Clin. Neuropharmacol. 2011, 34, 241–247. [Google Scholar] [CrossRef]
- Dainer, M.J. Untoward reaction to Flagyl (metronidazole). Am. J. Obstet. Gynecol. 1979, 133, 939–940. [Google Scholar] [CrossRef]
- Roy, U. Clinical and Neuroradiological Spectrum of Metronidazole Induced Encephalopathy: Our Experience and the Review of Literature. J. Clin. Diagn. Res. 2016, 10, OE01. [Google Scholar] [CrossRef]
- Bergogne-Berezin, E.; Bryskier, A. The suppository form of antibiotic administration: Pharmacokinetics and clinical application. J. Antimicrob. Chemother. 1999, 43, 177–185. [Google Scholar] [CrossRef][Green Version]
- Mathew, R.P.; Kunhimohammed, S.P.; Joseph, M. A Case of Topical Metronidazole–Induced Encephalopathy. JAMA Neurol. 2020, 77, 1318–1319. [Google Scholar] [CrossRef] [PubMed]
- Sechi, G.; Serra, A. Wernicke’s encephalopathy: New clinical settings and recent advances in diagnosis and management. Lancet Neurol. 2007, 6, 442–455. [Google Scholar] [CrossRef]
- Oudman, E.; Wijnia, J.W.; Oey, M.J.; van Dam, M.; Postma, A. Wernicke-Korsakoff syndrome despite no alcohol abuse: A summary of systematic reports. J. Neurol. Sci. 2021, 426, 117482. [Google Scholar] [CrossRef] [PubMed]
- Hahn, J.S.; Berquist, W.; Alcorn, D.M.; Chamberlain, L.; Bass, D. Wernicke Encephalopathy and Beriberi During Total Parenteral Nutrition Attributable to Multivitamin Infusion Shortage. Pediatrics 1998, 101, e10. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, L.; Bezerra, F.R.; Monteiro, M.; Silva, M.L.; De Oliveira, F.R.; Lima, R.R.; Fontes-Júnior, E.A.; Maia, C.S.F. Thiamine deficiency, oxidative metabolic pathways and ethanol-induced neurotoxicity: How poor nutrition contributes to the alcoholic syndrome, as Marchiafava–Bignami disease. Eur. J. Clin. Nutr. 2017, 71, 580–586. [Google Scholar] [CrossRef]
- Bhattacharyya, S.; Darby, R.R.; Raibagkar, P.; Castro, L.N.G.; Berkowitz, A.L. Antibiotic-associated encephalopathy. Neurology 2016, 86, 963–971. [Google Scholar] [CrossRef]
- Ferro, J.M.; Santos, M.O. Neurology of inflammatory bowel disease. J. Neurol. Sci. 2021, 424, 117426. [Google Scholar] [CrossRef]
- Bond, K.; Brinjikji, W.; Eckel, L.; Kallmes, D.; McDonald, R.; Carr, C. Dentate Update: Imaging Features of Entities That Affect the Dentate Nucleus. Am. J. Neuroradiol. 2017, 38, 1467–1474. [Google Scholar] [CrossRef]
- Couce, M.; Ramos, F.; Bueno, M.; Díaz, J.; Meavilla, S.; Bóveda, M.; Fernández-Marmiesse, A.; García-Cazorla, A. Evolution of maple syrup urine disease in patients diagnosed by newborn screening versus late diagnosis. Eur. J. Paediatr. Neurol. 2015, 19, 652–659. [Google Scholar] [CrossRef]
- Kohlschütter, A.; Eichler, F. Childhood leukodystrophies: A clinical perspective. Expert Rev. Neurother. 2011, 11, 1485–1496. [Google Scholar] [CrossRef]
- Wang, Q.; Li, X.; Ding, Y.; Liu, Y.; Song, J.; Yang, Y. Clinical and mutational spectra of 23 Chinese patients with glutaric aciduria type 1. Brain Dev. 2014, 36, 813–822. [Google Scholar] [CrossRef] [PubMed]
- Khadilkar, S.; Jaggi, S.; Patel, B.; Yadav, R.; Hanagandi, P.; Amaral, L.F.D. A practical approach to diseases affecting dentate nuclei. Clin. Radiol. 2015, 71, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Boy, N.; Contributors, A.I.; Mühlhausen, C.; Maier, E.M.; Heringer, J.; Assmann, B.; Burgard, P.; Dixon, M.; Fleissner, S.; Rockman-Greenberg, C.; et al. Proposed recommendations for diagnosing and managing individuals with glutaric aciduria type I: Second revision. J. Inherit. Metab. Dis. 2016, 40, 75–101. [Google Scholar] [CrossRef] [PubMed]
- Baertling, F.; Rodenburg, R.J.; Schaper, J.; Smeitink, J.A.; Koopman, W.J.H.; Mayatepek, E.; Morava, E.; Distelmaier, F. A guide to diagnosis and treatment of Leigh syndrome. J. Neurol. Neurosurg. Psychiatry 2013, 85, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Tang, X.; Li, W.; Liang, S.; Zhu, Q.; Wu, M. A case of methylprednisolone treatment for metronidazole-induced encephalopathy. BMC Neurol. 2019, 19, 49. [Google Scholar] [CrossRef] [PubMed]
| Author, Year, Country | Age (Years), Sex | Indication | Cumulative Dose of Metronidazole | Days to First Symptoms; Total Duration of Treatment | Symptoms and Clinical Findings | MRI Findings | Follow Up MRI | Outcome |
|---|---|---|---|---|---|---|---|---|
| Bailes, 1983, USA [1] | 12, M | Perforated appendicitis | 4 g | 4; 4 | Altered mental status; seizures | N/A | N/A | Resolution |
| Bates, 2015, USA [2] | 36-day-old, M | Mother’s vaginosis (utero exposure) | N/A | N/A; N/A | Hypothermia; bradycardia; failure to thrive; decreased tone and strength | T2: symmetrical hyperintensity in the dentate nuclei | Not done | Resolution |
| Cecil, 2002, USA [3] | 17, M | Crohn’s disease | N/A | N/A; N/A | Gait instability; Polyneuropathy; visual disturbance; tremor | T2: Symmetrical hyperintensity in the substantia nigra, red nucleus, globus pallidus, the putamen, caudate body, caudate heads and medial thalami | Near complete resolution | Near complete resolution |
| Chang, 2021, USA [4] | 14, M | Clostridium difficile enterocolitis | N/A | N/A; N/A | Altered mental status; stiffening of 4 extremities; visual disturbance; slurred speech; gait instability | T2: symmetrical hyperintensity with corresponding diffusion restriction on DWI in posterior frontal, parietal, and occipital periventricular white matter and splenium of the corpus callosum | Near complete resolution | Near complete resolution |
| Chatzkel, 2010, USA [5] | 15, F | Crohn’s disease | N/A | 7; N/A | Ataxia; dysmetria | T2: Symmetrical hyperintensity in the dentate nuclei | Resolution | N/A |
| Gaye, USA, 2007 [6] | Teenager, M | appendectomy | N/A | N/A; N/A | Unresponsiveness; respiratory distress; decerebrate posturing | Left parietal flair signal | N/A | Resolution |
| Kafadar, 2013, Turkey [7] | 3, M | amoebiasis diarrhea | N/A | 14; N/A | Loss of vision; ataxia, dizziness | Normal | N/A | Resolution |
| Omrani, Iran, 2020 [8] | 11, M | Febrile bloody diarrhea | 12 g | N/A; N/A | Tinnitus; hearing loss; aggressive behavior; generalized dystonia; generalized tonic-clonic seizure; decreased level of consciousness. | T2: Symmetrical hyperintensity in dentate nuclei, substantia nigra, globus pallidi, splenium of the corpus callosum, and centrum semiovale | Improvement | Partial improvement |
| Patel, USA, 2020 [9] | 8, M | Prophylaxis after small bowel transplantation | 1378.8 g | Three years; three years | Ataxia | T2: Symmetrical hyperintensity in the dentate nuclei, inferior olivary nuclei, putamen, and corpus callosum | Resolution | Resolution |
| Starrs, 2021, USA [10] | 12, M | Clostridium deficile infection | N/A | 75; 75 | Vertigo; nausea; vomiting; ataxia; gait instability | T2: Symmetrical hyperintensity in the dentate nuclei | N/A | Resolution |
| Sudan, 2016, India [11] | 14, M | Acute abdominal pain | N/A | 3; 5 | Dysarthria; altered mental status; seizures. | T2: symmetrical hyperintensity in the optic tracts, dorsal midbrain, inferior olivary nuclei, peri-aqueductal white matter, superior and inferior colliculi, superior cerebellar peduncle, dentate nuclei, medulla oblongata, and cervical spinal cord segment extending from the cervicomedullary junction to C6-C7 level DWI: restricted diffusion in the splenium of the corpus callosum | N/A | Resolution |
| Sun, 2019, USA [12] | 11, M | Fusobacterium menigitis | N/A | 3 months; N/A | Vomiting; dizziness; vertigo; gait instability; bilateral lower extremity paresthesia | T2: Symmetrical hyperintensity in the dentate nuclei, dorsal pons, and medulla. DWI: no restricted diffusion | Resolution | Resolution |
| Yazdani, 2019, USA [13] | 17, M | Chronic diarrhea | N/A | N/A | Gait instability; abnormal unilateral lean | T2: Symmetrical signal hyperintensity in dorsal pons, dentate nuclei, dorsal medulla | Improvement | Resolution |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rybak, K.; Warchoł, A.; Drobczyński, Ł.; Banaszkiewicz, A. Metronidazole-Induced Encephalopathy in a 16-Year-Old Girl with Crohn’s Disease: Case Report and Review of the Pediatric Literature. Children 2022, 9, 1408. https://doi.org/10.3390/children9091408
Rybak K, Warchoł A, Drobczyński Ł, Banaszkiewicz A. Metronidazole-Induced Encephalopathy in a 16-Year-Old Girl with Crohn’s Disease: Case Report and Review of the Pediatric Literature. Children. 2022; 9(9):1408. https://doi.org/10.3390/children9091408
Chicago/Turabian StyleRybak, Karolina, Aleksandra Warchoł, Łukasz Drobczyński, and Aleksandra Banaszkiewicz. 2022. "Metronidazole-Induced Encephalopathy in a 16-Year-Old Girl with Crohn’s Disease: Case Report and Review of the Pediatric Literature" Children 9, no. 9: 1408. https://doi.org/10.3390/children9091408
APA StyleRybak, K., Warchoł, A., Drobczyński, Ł., & Banaszkiewicz, A. (2022). Metronidazole-Induced Encephalopathy in a 16-Year-Old Girl with Crohn’s Disease: Case Report and Review of the Pediatric Literature. Children, 9(9), 1408. https://doi.org/10.3390/children9091408





