Disc Displacement of the Temporomandibular Joint and Facial Asymmetry in Children and Adolescents: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Procedure and Enrollment
2.2. Standards for Selection
2.3. Resources of Knowledge
2.4. Methodology for Selection
2.5. Recruitment Procedure
2.6. Technique for Data Gathering
2.7. Critical Evaluation of Each Study
2.8. Synthesis Methods
2.9. Identification of Bias
3. Results
3.1. Selection of Sources of Evidence
3.2. Features of Research
3.3. Results of Syntheses
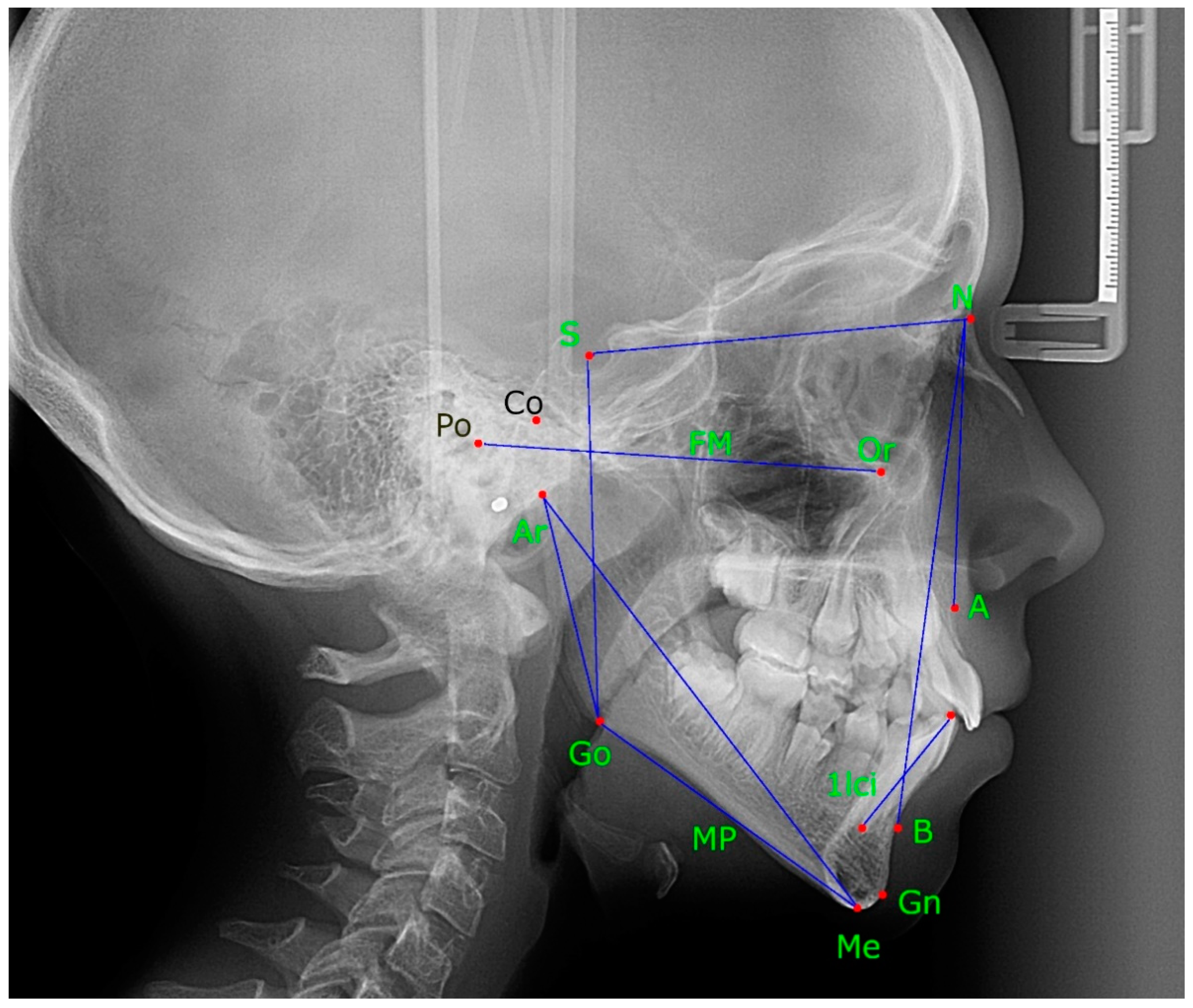
3.3.1. Distance from Menton to Midline (Mandibular Lateral Asymmetry, or Displacement)
3.3.2. Distance from Articulare to Gonion (Mandible Ramus Height)
3.3.3. Distance from Articulare to Menton (Total Mandibular Length)
3.3.4. Distance from Sella to Gonion (Overall Posterior Jawline Dimension)
3.3.5. Other Cephalogram Measurements
3.4. Investigation’s Potential Bias
4. Discussion
4.1. Scientific Proof Synopsis
4.2. Strengths and Weaknesses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Estomaguio, G.A.; Yamada, K.; Saito, I. Unilateral Condylar Bone Change, Inclination of the Posterior Slope of the Articular Eminence and Craniofacial Morphology. Orthod. Waves 2008, 67, 113–119. [Google Scholar] [CrossRef]
- Khojastepour, L.; Omidi, M.; Vojdani, M.; Bagheri, K. Investigating Possible Correlation between Condylar Asymmetry and Clinical Dysfunction Indices in Patients with Temporomandibular Dysfunction Using Cone-Beam Computed Tomographic. J. Cranio-Maxillofac. Surg. 2019, 47, 438–442. [Google Scholar] [CrossRef] [PubMed]
- Guercio-Monaco, E.; De Stefano, A.; Impellizzeri, A.; Galluccio, G. Association between the Temporomandibular Joint Disc Position on Magnetic Resonance Imaging and the Mandibular Deviation on Posteroanterior Cephalogram: A Cross-Sectional Study in Adolescents. Clin. Ter. 2020, 171, e509–e516. [Google Scholar] [CrossRef] [PubMed]
- Xie, Q.; Yang, C.; He, D.; Cai, X.; Ma, Z.; Shen, Y.; Abdelrehem, A. Will Unilateral Temporomandibular Joint Anterior Disc Displacement in Teenagers Lead to Asymmetry of Condyle and Mandible? A Longitudinal Study. J. Craniomaxillofac. Surg. 2016, 44, 590–596. [Google Scholar] [CrossRef] [PubMed]
- Santana-Mora, U.; López-Cedrún, J.; Suárez-Quintanilla, J.; Varela-Centelles, P.; Mora, M.J.; Da Silva, J.L.; Figueiredo-Costa, F.; Santana-Penín, U. Asymmetry of Dental or Joint Anatomy or Impaired Chewing Function Contribute to Chronic Temporomandibular Joint Disorders. Ann. Anat. Anat. Anz. 2021, 238, 151793. [Google Scholar] [CrossRef]
- Toh, A.Q.J.; Chan, J.L.H.; Leung, Y.Y. Mandibular Asymmetry as a Possible Etiopathologic Factor in Temporomandibular Disorder: A Prospective Cohort of 134 Patients. Clin. Oral. Investig. 2021, 25, 4445–4450. [Google Scholar] [CrossRef]
- Uy-Co, E.T.; Yamada, K.; Hanada, K.; Hayashi, T.; Ito, J. Condylar Bony Change and Mandibular Deviation in Orthodontic Patients—Using Helical CT and MRI. Clin. Orthod. Res. 2000, 3, 132–143. [Google Scholar] [CrossRef]
- Ikeda, M.; Miyamoto, J.J.; Takada, J.; Moriyama, K. Association between 3-Dimensional Mandibular Morphology and Condylar Movement in Subjects with Mandibular Asymmetry. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 324–334. [Google Scholar] [CrossRef]
- Kilic, N.; Kiki, A.; Oktay, H. Condylar Asymmetry in Unilateral Posterior Crossbite Patients. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 382–387. [Google Scholar] [CrossRef]
- Ooi, K.; Inoue, N.; Matsushita, K.; Mikoya, T.; Minowa, K.; Kawashiri, S.; Tei, K. Relations between Anterior Disc Displacement and Maxillomandibular Morphology in Skeletal Anterior Open Bite with Changes to the Mandibular Condyle. Br. J. Oral Maxillofac. Surg. 2020, 58, 1084–1090. [Google Scholar] [CrossRef]
- Zhang, Y.-L.; Song, J.-L.; Xu, X.-C.; Zheng, L.-L.; Wang, Q.-Y.; Fan, Y.-B.; Liu, Z. Morphologic Analysis of the Temporomandibular Joint Between Patients with Facial Asymmetry and Asymptomatic Subjects by 2D and 3D Evaluation: A Preliminary Study. Medicine 2016, 95, e3052. [Google Scholar] [CrossRef]
- Zhuo, Z.; Cai, X.; Xie, Q. Is Anterior Disc Displacement Without Reduction Associated with Temporomandibular Joint Condylar Height in Juvenile Patients Younger Than 20 Years? J. Oral Maxillofac. Surg. 2015, 73, 843–849. [Google Scholar] [CrossRef]
- Oguri, Y.; Yamada, K.; Fukui, T.; Hanada, K.; Kohno, S. Mandibular Movement and Frontal Craniofacial Morphology in Orthognathic Surgery Patients with Mandibular Deviation and Protrusion: Mandibular Movement in Patients with Mandibular Deviation and Protrusion. J. Oral Rehabil. 2003, 30, 392–400. [Google Scholar] [CrossRef]
- Nicot, R.; Chung, K.; Vieira, A.R.; Raoul, G.; Ferri, J.; Sciote, J.J. Condyle Modeling Stability, Craniofacial Asymmetry and ACTN3 Genotypes: Contribution to TMD Prevalence in a Cohort of Dentofacial Deformities. PLoS ONE 2020, 15, e0236425. [Google Scholar] [CrossRef]
- Pawlaczyk-Kamieńska, T.; Kulczyk, T.; Pawlaczyk-Wróblewska, E.; Borysewicz-Lewicka, M.; Niedziela, M. Limited Mandibular Movements as a Consequence of Unilateral or Asymmetrical Temporomandibular Joint Involvement in Juvenile Idiopathic Arthritis Patients. J. Clin. Med. 2020, 9, E2576. [Google Scholar] [CrossRef]
- Bernini, J.M.; Kellenberger, C.J.; Eichenberger, M.; Eliades, T.; Papageorgiou, S.N.; Patcas, R. Quantitative Analysis of Facial Asymmetry Based on Three-Dimensional Photography: A Valuable Indicator for Asymmetrical Temporomandibular Joint Affection in Juvenile Idiopathic Arthritis Patients? Pediatr. Rheumatol. Online J. 2020, 18, 10. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Corporation for Digital Scholarship Zotero 6.0.6. Available online: https://www.zotero.org/ (accessed on 25 July 2022).
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. Ottawa Hospital Research Institute. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 29 April 2022).
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series; John Wiley & Sons: Chichester, UK, 2008. [Google Scholar]
- Schwarzer, G. Meta: General Package for Meta-Analysis 2022. Available online: https://cran.r-project.org/web/packages/meta/meta.pdf (accessed on 25 July 2022).
- R Core Team. A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Bastos, L.V.W.; Tesch, R.d.S.; Denardin, O.V.P. Cephalometric Deviations Present in Children and Adolescents with Temporomandibular Joint Disorders. Dental Press J. Orthod. 2012, 17, 74–84. [Google Scholar] [CrossRef]
- Nebbe, B. Adolescent Female Craniofacial Morphology Associated with Advanced Bilateral TMJ Disc Displacement. Eur. J. Orthod. 1998, 20, 701–712. [Google Scholar] [CrossRef] [Green Version]
- Trpkova, B.; Major, P.; Nebbe, B.; Prasad, N. Craniofacial Asymmetry and Temporomandibular Joint Internal Derangement in Female Adolescents: A Posteroanterior Cephalometric Study. Angle Orthod. 2000, 70, 81–88. [Google Scholar] [CrossRef]
- Shi, J.-J.; Zhang, F.; Zhou, Y.-Q.; Gu, Z.-Y. The Relationship between Partial Disc Displacement and Mandibular Dysplasia in Female Adolescents. Med. Sci. Monit. 2010, 16, CR283-8. [Google Scholar]
- Nakagawa, S.; Sakabe, J.; Nakajima, I.; Akasaka, M. Relationship between Functional Disc Position and Mandibular Displacement in Adolescent Females: Posteroanterior Cephalograms and Magnetic Resonance Imaging Retrospective Study. J. Oral. Rehabil. 2002, 29, 417–422. [Google Scholar] [CrossRef]
- Xie, Q.; Yang, C.; He, D.; Cai, X.; Ma, Z. Is Mandibular Asymmetry More Frequent and Severe with Unilateral Disc Displacement? J. Cranio-Maxillofac. Surg. 2015, 43, 81–86. [Google Scholar] [CrossRef]
- Jeon, D.-M.; Jung, W.-S.; Mah, S.-J.; Kim, T.-W.; Ahn, S.-J. The Effects of TMJ Symptoms on Skeletal Morphology in Orthodontic Patients with TMJ Disc Displacement. Acta Odontol. Scand. 2014, 72, 776–782. [Google Scholar] [CrossRef]
- Jung, W.-S.; Kim, H.; Jeon, D.-M.; Mah, S.-J.; Ahn, S.-J. Magnetic Resonance Imaging-Verified Temporomandibular Joint Disk Displacement in Relation to Sagittal and Vertical Jaw Deformities. Int. J. Oral Maxillofac. Surg. 2013, 42, 1108–1115. [Google Scholar] [CrossRef]
- Şakar, O.; Çalişir, F.; Marşan, G.; Öztaş, E. Evaluation of the Effects of Temporomandibular Joint Disc Displacement and Its Progression on Dentocraniofacial Morphology in Symptomatic Patients Using Posteroanterior Cephalometric Analysis. CRANIO® 2013, 31, 23–31. [Google Scholar] [CrossRef]
- Liu, Z.; Xie, Q.; Yang, C.; Chen, M.; Bai, G.; Abdelrehem, A. The Effect of Arthroscopic Disc Repositioning on Facial Growth in Juvenile Patients with Unilateral Anterior Disc Displacement. J. Craniomaxillofac. Surg. 2020, 48, 765–771. [Google Scholar] [CrossRef]






| Author, Year | Aim | Study Population | DD Classification | Asymmetry | Radiographic Evaluation | Findings | Conclusions |
|---|---|---|---|---|---|---|---|
| Nebbe, 1998 [25] | to test the hypothesis of no difference in facial cephalometric measurements in adolescents with DD | study group: bilateral DD 17 teenage girls, 13.65 years on average Control group: ND position 17 teenage girls, 13.53 years on average | MRI | study group: lower overall posterior height (S-Go) reduced mandibular ramus length (Co-Go, Ar-Go) shortened posterior facial height (S-Ar) increase in the distance from S-N to the palatal plane increase in the distance from S-N to a line tangent to the inferior border of the mandible’s body posterior displacement of Gn related to anterior structures of the face posterior rotation of the mandible Control group: higher mandibular lateral displacement inclined frontal occlusal plane | lateral cephalogram | mean differences (95% CI): Ar-Go (mm) 4.18 (0.69–7.68); Ar-Me 4.33 (mm) (−0.01–8.68); Ar-Go-Me (degrees) 0.46 (−4.18–3.27); FH/MP 3.80 (degrees) (−8.02–0.42); S-Go (mm) 5.57 (1.96–9.18); N-Me (mm) 1.07 (−5.54–3.40) | bilateral DD: posterior vertical facial height diminished; Juvenile disc position aberrations are not within the range of typical physiologic diversity. |
| Trpkova, 2000 [26] | if TMJ ID (DD) is associated with craniofacial asymmetry | 80 females (average age, 13.20 ± 1.7) bilateral normal TMJ: 42 unilateral right TMJ ID: 13 unilateral left TMJ ID: 10 bilateral TMJ ID: 15 | MRI TMJ ID: disc displacement and disc length | the longitudinal imbalance in the area of AGo differed substantially | posteroanterior cephalograms lateral cephalograms | increased asymmetry of the AGo with a shorter mandible ramus in bilateral TMJ ID | women with symmetrical TMJ ID experienced higher vertical mandible asymmetry |
| Nakagawa, 2002 [28] | to determine the relationship between LMD, VMD, DD, and mandible growth | 54 female adolescents (average age: 15.7 ± 3.0) Group 1: bilateral ND position: 23 subjects (average age: 14.9 ± 3.4); Group 2: unilateral /bilateral DD (=partial DD): 12 subjects (average age: 15.9 ± 2.9) Group 3: unilateral /bilateral disc dislocation (=complete DD): 19 subjects (mean age: 16.4 ± 2.4 years) | MRI | right and left mandibular height (VMD) LMD | posteroanterior cephalograms | mandible deviation is linked to DD and disc dislocation Group 1: VMD (AGo-zygomatic line): mean 0.89 ± 0.74 mm LMD (MeX) mean 1.33 ± 1.23 mm Group 2: VMD mean 3.2 ± 1.51 mm LMD mean 3.01 ± 2.51 mm Group 3: VMD mean 3.13 ± 2.3 mm LMD mean 3.72 ± 2.42 mm | DD disturbs normal mandible growth VMD was not related to age LMD was related to age DD was related to LMD and VMD |
| Shi, 2010 [27] | to evaluate the relationship between partial DD and mandibular dysplasia | 46 female adolescents aged 10.1–12.8 years. DD group (n = 26), ND group (n = 20) | MRI | the displaced group exhibited a reduced length of the mandible (Go-Po), sharper mandible plane (MP/FH), and steep mandible inclination (Ar-Go-Me) | lateral cephalograms | DD vs. ND: SNA(°) 79.31 ± 3.40 vs. 80.15 ± 4.79, p = 0.489; SNB(°) 74.31 3.06 vs. 75.25 5.09, p = 0.440; ANB(°) 6 ± 1.45 vs. 6 ± 1.02, p = 1; Ar-Go(mm) 45.42 ± 4.59 vs. 47.75 ± 6.50, p = 0.162; Ar-Me(mm) 95.73 ± 4.68 vs. 99.05 ± 6.95, p = 0.060; Go-Po(mm) 69.00 ± 3.96 vs. 72.00 ± 3.54, p = 0.011 *; Ar-Go-Me (°) 118.77 ± 5.03 vs. 115.75 ± 2.78, p = 0.020 *; MP/FH (°) 31.23 ± 3.85 vs. 26.80 ± 5.54, p = 0.003; S-Go(mm) 74.50 ± 3.26 vs. 76.50 ± 5.57, p = 0.134; N-Me(mm) 116.12 ± 4.22 vs. 116.30 ± 4.96, p = 0.892 | partial DD may be related to horizontal jaw impairments but not longitudinal abnormalities |
| Bastos, 2012 [24] | to evaluate differences between the cephalometric variables for facial growth patterns in children and adolescents with articular TMD and control group | Experimental group 30 patients with articular TMD. Control group: 30 volunteers without TMD, matched | RDC/ TMD | the analysis of the post-peak of pubertal growth spurt showed that the experimental group had mean values for SNA and SNB angles decreased, and the facial axis angle (SN.Gn) and lower incisor inclination (1-NB) increased with the mean values found in the control group, revealing statistically significant differences | lateral cephalograms | DD vs. ND:Pre-peak: S.N.A (°) 82.05 ± 3.03 vs. 81.39 ± 4.34, p = 0.611; S.N.B (°) 4.30 ± 1.91 vs. 3.98 ± 4.63, p = 0.799; A.N.B (°) 4.3 ± 1.91 vs. 3.98 ± 4.63, p = 0.799; Ar-Go (mm) 39.22 ± 3.86 vs. 39.46 ± 3.50, p = 0.853; Ar.Go.Me (°) 129.66 ± 6.75 vs. 126.15 ± 5.37, p = 0.104; S-Go (mm) 68.25 ± 6.10 vs. 67.23 ± 5.68, p = 0.619; N-Me (mm) 110.40 ± 7.96 vs. 110.24 ± 7.69, p = 0.952; post-peak: S.N.A (°) 78.25 ± 3.55 vs. 82.90 ± 4.53, p = 0.008; S.N.B (°) 74.69 ± 3.63 vs. 79.26 ± 4.75, p = 0.011; A.N.B (°) 3.55 ± 2.98 vs. 3.71 ± 2.89, p = 0.891; Ar-Go (mm) 42.18 ± 3.53 vs. 43.12 ± 3.99, p = 0.532; Ar.Go.Me (°) 125.76 ± 5.59 vs. 128.02 ± 4.42, p = 0.265; S-Go (mm) 73.42 ± 6.42 vs. 72.99 ± 4.36, p = 0.842; N-Me (mm) 121.26 ± 9.21 vs. 115.37 ± 7.58, p = 0.088 | changes in morphometric parameters were detected in youngsters with joint TMD |
| Xie, 2015 [29] | to determine the amount of MA in asymmetric ADD individuals | study goup: average age 16.74 years vs. average age 16.21 years in the control group (165 patients with ADD (101 left, 64 right), 156 controls without ADD | MRI | of 119 MA patients in ADD group, 73 with left ADD, 46 with right ADD, | posteroanterior cephalograms | in the ADD group, category 27.88% had no MA, mean MeX: 5.62 mm in the control group, 25.64% had MA, mean MeX: 4.19 mm | MA is more unilateral ADD teenagers The greater the DD, the shorter the condyle and higher the jaw irregularity |
| Xie, 2016 [4] | to observe the influence of ADD and to analyze its effect on the symmetry of the mandible | average age 16.31 28 females, 16 males The average follow-up period was 12.22 months | MRI | first evaluation 86.36% MA follow-up: 93.18% MA | posteroanterior cephalograms | the correlation coefficient between condyle height disparity and MeX (CC = 0.681, p < 0.05) the increase of menton deviation was significantly related to the age of patients at the initial visit (correlation coefficient = −0.760, p < 0.05). the average MeX was 5.58 mm at the initial visit, while it was 7.74 mm after follow-up | in adolescents, MA was secondary or fostered by UJADD |
| Guercio-Monaco, 2020 [3] | to analyze the association between TMJ disc position evaluated by MRI and the mandible deviation evaluated by PA in adolescents | 53 adolescents (37 females and 16 males, mean age 14.28 ± 2.46 years; 11–18) and 106 TMJs group I Same disc position bilateral (n = 23); group II DD is more severe ipsilateral (n = 17); group III DD more severe contralateral (n = 13) | MRI | significant differences between the mean of group II (4.4 ± 2.2) with groups I and III (p = 0.016 and p = 0.036 respectively), with a greater menton deviation concerning the rest of the groups a statistical association between DD and gender was observed (p = 0.002), with more frequent DD in females | posteroanterior cephalograms | MeX menton deviation: Same disc position bilateral 2.17 ± 1.93; DD more severe ipsilateral 4.40 ± 2.26; DD more severe contralateral 2.10 ± 1.70 | the menton deviation was related to unilateral or bilateral cases TMJ DD the menton tended to exhibit more deflection to the side more affected |
| Characteristic, Effect Size Type | Number of Studies | Effect Size (95% CI) | p-Value | I2 (95% CI) | p-Value | Egger Test | Studies | Leave One Out |
|---|---|---|---|---|---|---|---|---|
| MeX (mm) mean difference | 2 | −1.75 (−2.43–−1.07) | <0.001 | NC | NC | Nakagawa, 2002 [28]; Xie, 2015 [29] | -Nakagawa, 2002: −1.43 (−2.37–−0.49), p = 0.003, I2 = NA%; -Xie, 2015: −2.12 (−3.11–−1.12), p ≤ 0.001, I2 = NA% | |
| Ar-Go (mm) mean difference | 3 | 1.98 (−0.11–4.08) | 0.063 | 42.3 (0–82.6) | 0.177 | 0.265 | Nebbe, 1998 [25]; Shi, 2010 [27]; Bastos, 2012 [24] | -Nebbe, 1998: 1.02 (−0.71–2.76), p = 0.248, I2 = 0%; -Shi, 2010: 2.11 (−1.42–5.63), p = 0.242, I2 = 70%; -Bastos, 201: 3.25 (0.88–5.63), p = 0.007, I2 = 0% |
| Go-Po (mm) mean difference | 2 | 1.3 (−2.37–4.97) | 0.487 | NC | NC | Shi, 2010 [27]; Bastos, 2012 [24] | -Shi, 2010: −0.76 (−3.93–2.41), p = 0.636, I2 = NA%; -Bastos, 2: 3 (0.83–5.17), p = 0.007, I2 = NA% | |
| Ar-Me (mm) mean difference | 2 | 3.74 (1.04–6.44) | 0.007 | NC | NC | Nebbe, 1998 [25]; Shi, 2010 [27] | -Nebbe, 1998: 3.32 (−0.22–6.86), p = 0.066, I2 = NA%; -Shi, 2010: 4.33 (0.15–8.51), p = 0.042, I2 = NA% | |
| S-Go (mm) mean difference | 2 | 4.15 (−0.32–8.63) | 0.069 | NC | NC | Nebbe, 1998 [25]; Shi, 2010 [27] | -Nebbe, 1998: 2 (−0.73–4.73), p = 0.151, I2 = NA%; -Shi, 2010: 6.57 (3.1–10.04), p ≤ 0.001, I2 = NA% | |
| N-Me (mm) mean difference | 3 | −0.19 (−2.24–1.86) | 0.859 | 0 (0–89.6) | 0.471 | 0.721 | Nebbe, 1998 [25]; Shi, 2010 [27]; Bastos, 2012 [24] | -Nebbe, 1998: −0.61 (−3.09–1.87), p = 0.631, I2 = 8%; -Shi, 2010: −0.7 (−4.34–2.93), p = 0.705, I2 = 26%; -Bastos, 201: 0.43 (−1.86–2.73), p = 0.711, I2 = 0% Supplementary Figure S10 |
| SNA (deg) mean difference | 2 | 1.31 (−0.28–2.9) | 0.105 | NC | NC | Shi, 2010 [27]; Bastos, 2012 [24] | -Shi, 2010: 1.64 (−0.43–3.71), p = 0.12, I2 = NA%; -Bastos, 2: 0.84 (−1.63–3.31), p = 0.506, I2 = NA% | |
| SNB (deg) mean difference | 2 | 2.82 (−0.74–6.37) | 0.12 | NC | NC | Shi, 2010 [27]; Bastos, 2012 [24] | -Shi, 2010: 4.57 (2.43–6.71), p ≤ 0.001, I2 = NA%; -Bastos, 2: 0.94 (−1.58–3.46), p = 0.465, I2 = NA% | |
| ANB (deg) mean difference | 2 | −0.02 (−0.67–0.64) | 0.958 | NC | NC | Shi, 2010 [27]; Bastos, 2012 [24] | -Shi, 2010: −0.11 (−1.76–1.53), p = 0.894, I2 = NA%; -Bastos, 2: 0 (−0.71–0.71), p = 1, I2 = NA% | |
| MP/FH (deg) mean difference | 2 | −0.45 (−8.51–7.61) | 0.913 | NC | NC | Nebbe, 1998 [25]; Shi, 2010 [27] | -Nebbe, 1998: −4.43 (−7.27–−1.59), p = 0.002, I2 = NA%; -Shi, 2010: 3.8 (−0.26–7.86), p = 0.067, I2 = NA% | |
| Ar-Go-Me (deg) mean difference | 3 | −1.55 (−3.52–0.41) | 0.121 | 30.8 (0–92.8) | 0.236 | 0.06 | Nebbe, 1998 [25]; Shi, 2010 [27]; Bastos, 2012 [24] | -Nebbe, 1998: −2.23 (−4.15–−0.31), p = 0.023, I2 = 11%; -Shi, 2010: −0.42 (−2.69–1.84), p = 0.715, I2 = 0%; -Bastos, 201: −1.57 (−4.93–1.8), p = 0.362, I2 = 61% Supplementary Figure S9 |
| Researcher and Release Year | Case Definition Sustainability | Cases’ Representativeness | Controls Selecting | Controls Defining | Cases and Controls Comparability | Exposure Assessment |
|---|---|---|---|---|---|---|
| Nebbe, 1998 [25] | * | * | * | * | * | |
| Trpkova, 2000 [26] | * | * | * | * | * | |
| Nakagawa, 2002 [28] | * | * | * | * | * | |
| Shi, 2010 [27] | * | * | * | * | * | |
| Bastos, 2012 [24] | * | ** | * | |||
| Xie, 2015 [29] | * | * | * | * | * | |
| Xie, 2016 [4] | * | * | * | * | NA | * |
| Guercio-Monaco, 2020 [3] | * | * | * | * | * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almășan, O.; Leucuța, D.-C.; Buduru, S. Disc Displacement of the Temporomandibular Joint and Facial Asymmetry in Children and Adolescents: A Systematic Review and Meta-Analysis. Children 2022, 9, 1297. https://doi.org/10.3390/children9091297
Almășan O, Leucuța D-C, Buduru S. Disc Displacement of the Temporomandibular Joint and Facial Asymmetry in Children and Adolescents: A Systematic Review and Meta-Analysis. Children. 2022; 9(9):1297. https://doi.org/10.3390/children9091297
Chicago/Turabian StyleAlmășan, Oana, Daniel-Corneliu Leucuța, and Smaranda Buduru. 2022. "Disc Displacement of the Temporomandibular Joint and Facial Asymmetry in Children and Adolescents: A Systematic Review and Meta-Analysis" Children 9, no. 9: 1297. https://doi.org/10.3390/children9091297
APA StyleAlmășan, O., Leucuța, D.-C., & Buduru, S. (2022). Disc Displacement of the Temporomandibular Joint and Facial Asymmetry in Children and Adolescents: A Systematic Review and Meta-Analysis. Children, 9(9), 1297. https://doi.org/10.3390/children9091297








