Pediatric Minimally Invasive Surgery—A Bibliometric Study on 30 Years of Research Activity
Abstract
:1. Introduction
2. Materials and Methods
3. Results
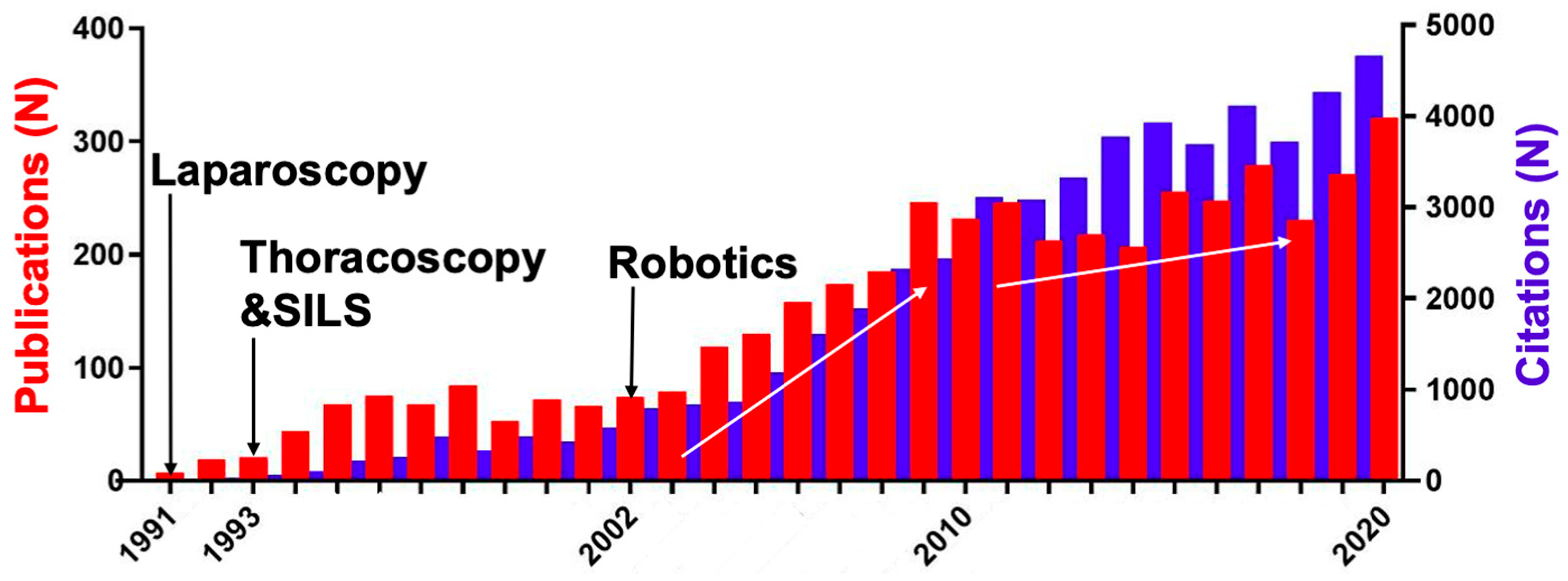
3.1. Overall Trends
3.2. 50 Most Cited Publications on MIS
3.3. Top Cited Journals and Impact Factor
3.4. Evidence Levels
3.5. Hot Topics
4. Discussion
4.1. Scientific Quality of the Top 50 Citations
4.2. Hot Topics of the Top 50 Citations
4.3. Establishing New Techniques in Pediatric MIS
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alain, J.L.; Grousseau, D.; Terrier, G. Extramucosal pyloromyotomy by laparoscopy. Surg. Endosc. 1991, 5, 174–175. [Google Scholar] [CrossRef] [PubMed]
- Alain, J.L.; Grousseau, D.; Terrier, G. Extramucosal pylorotomy by laparoscopy. J. Pediatr. Surg. 1991, 26, 1191–1192. [Google Scholar] [CrossRef]
- Blinman, T.; Ponsky, T. Pediatric minimally invasive surgery: Laparoscopy and thoracoscopy in infants and children. Pediatrics 2012, 130, 539–549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meinzer, A.; Alkatout, I.; Krebs, T.F.; Baastrup, J.; Reischig, K.; Meiksans, R.; Bergholz, R. Advances and Trends in Pediatric Minimally Invasive Surgery. J. Clin. Med. 2020, 9, 3999. [Google Scholar] [CrossRef]
- Holcomb, G.W.; Olsen, D.O.; Sharp, K.W. Laparoscopic cholecystectomy in the pediatric patient. J. Pediatr. Surg. 1991, 26, 1186–1190. [Google Scholar] [CrossRef]
- Shalev, E.; Mann, S.; Romano, S.; Rahav, D. Laparoscopic detorsion of adnexa in childhood: A case report. J. Pediatr. Surg. 1991, 26, 1193–1194. [Google Scholar] [CrossRef]
- Kern, J.A.; Rodgers, B.M. Thoracoscopy in the management of empyema in children. J. Pediatr. Surg. 1993, 28, 1128–1132. [Google Scholar] [CrossRef]
- Lobe, T.E.; Rothenberg, S.; Waldschmidt, J.; Stroedter, L. Thoracoscopic Repair of Esophageal Atresia in an Infant: A Surgical First. Pediatr. Endosurg. Innov. Technol. 1999, 3, 141–148. [Google Scholar] [CrossRef]
- Heller, K.; Gutt, C.; Schaeff, B.; Beyer, P.A.; Markus, B. Use of the robot system Da Vinci for laparoscopic repair of gastro-oesophageal reflux in children. Eur. J. Pediatr. Surg. 2002, 12, 239–242. [Google Scholar] [CrossRef]
- Cui, X.; He, Y.-B.; Huang, W.-H.; Chen, L.; Chen, J.-C.; Zhou, C.-M. Mini-laparoscopic pyeloplasty to treat UPJO in infants. Minim. Invasive Ther. Allied Technol. 2022, 31, 473–478. [Google Scholar] [CrossRef]
- Lacher, M.; Kuebler, J.F.; Dingemann, J.; Ure, B.M. Minimal invasive surgery in the newborn: Current status and evidence. Semin. Pediatr. Surg. 2014, 23, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Sham, G.T.W.; Chung, P.H.Y.; Chan, I.M.C.; Leung, W.C.; Wong, K.K.Y. Thoracoscopic removal of a displaced thoracoamniotic shunt in a newborn with antenatal pleural effusion-a case report. Transl. Pediatr. 2020, 9, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Bishay, M.; Giacomello, L.; Retrosi, G.; Thyoka, M.; Garriboli, M.; Brierley, J.; Harding, L.; Scuplak, S.; Cross, K.M.; Curry, J.I.; et al. Hypercapnia and acidosis during open and thoracoscopic repair of congenital diaphragmatic hernia and esophageal atresia: Results of a pilot randomized controlled trial. Ann. Surg. 2013, 258, 895–900. [Google Scholar] [CrossRef]
- Aziz, O.; Athanasiou, T.; Tekkis, P.P.; Purkayastha, S.; Haddow, J.; Malinovski, V.; Paraskeva, P.; Darzi, A. Laparoscopic versus open appendectomy in children: A meta-analysis. Ann. Surg. 2006, 243, 17–27. [Google Scholar] [CrossRef] [PubMed]
- La Torre, G.; Sciarra, I.; Chiappetta, M.; Monteduro, A. New bibliometric indicators for the scientific literature: An evolving panorama. Clin. Ter. 2017, 168, e65–e71. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Martynov, I.; Suttkus, A.; Lacher, M.; Mayer, S. Publication Trends and Global Collaborations on Esophageal Atresia Research: A Bibliometric Study. Eur. J. Pediatr. Surg. 2020, 31, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Gerdsri, N.; Kongthon, A. Identify Potential Opportunity for Research Collaboration Using Bibliometrics. Int. J. Bus. 2018, 23, 248–260. [Google Scholar]
- Cashin, M.S.; Kelley, S.P.; Douziech, J.R.; Varghese, R.A.; Hamilton, Q.P.; Mulpuri, K. The levels of evidence in pediatric orthopaedic journals: Where are we now? J. Pediatr. Orthop. 2011, 31, 721–725. [Google Scholar] [CrossRef]
- GF, B. Appendectomy in children by simple port laparoscopy. Chir. Endosc. 1993, 2, 6–9. [Google Scholar]
- Lee, R.S.; Retik, A.B.; Borer, J.G.; Peters, C.A. Pediatric robot assisted laparoscopic dismembered pyeloplasty: Comparison with a cohort of open surgery. J. Urol. 2006, 175, 683–687. [Google Scholar] [CrossRef]
- Georgeson, K.E.; Inge, T.H.; Albanese, C.T. Laparoscopically assisted anorectal pull-through for high imperforate anus—A new technique. J. Pediatr. Surg. 2000, 35, 927–931. [Google Scholar] [CrossRef] [PubMed]
- Hall, N.J.; Pacilli, M.; Eaton, S.; Reblock, K.; Gaines, B.A.; Pastor, A.; Langer, J.C.; Koivusalo, A.I.; Pakarinen, M.P.; Stroedter, L.; et al. Recovery after open versus laparoscopic pyloromyotomy for pyloric stenosis: A double-blind multicentre randomised controlled trial. Lancet 2009, 373, 390–398. [Google Scholar] [CrossRef]
- Friedmacher, F.; Ford, K.; Davenport, M. Biliary atresia: A scientometric analysis of the global research architecture and scientific developments. J. Hepatobiliary Pancreat. Sci. 2019, 26, 201–210. [Google Scholar] [CrossRef]
- Martynov, I.; Feng, X.; Duess, J.W.; Gosemann, J.-H.; Lacher, M.; Mayer, S. Global Development of Research on Anorectal Malformations over the Last Five Decades: A Bibliometric Analysis. Children 2022, 9, 253. [Google Scholar] [CrossRef]
- Ence, A.K.; Cope, S.R.; Holliday, E.B.; Somerson, J.S. Publication Productivity and Experience: Factors Associated with Academic Rank Among Orthopaedic Surgery Faculty in the United States. J. Bone Joint Surg. Am. 2016, 98, e41. [Google Scholar] [CrossRef]
- Ramos, M.B.; Koterba, E.; Rosi Júnior, J.; Teixeira, M.J.; Figueiredo, E.G. A Bibliometric Analysis of the Most Cited Articles in Neurocritical Care Research. Neurocrit. Care 2019, 31, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Damodar, D.; Plotsker, E.; Greif, D.; Rizzo, M.G.; Baraga, M.G.; Kaplan, L.D. The 50 Most Cited Articles in Meniscal Injury Research. Orthop. J. Sport. Med. 2021, 9, 2325967121994909. [Google Scholar] [CrossRef]
- Rodwin, M.A. Reforming pharmaceutical industry-physician financial relationships: Lessons from the United States, France, and Japan. J. Law. Med. Ethics 2011, 39, 662–670. [Google Scholar] [CrossRef]
- Huo, Y.-Q.; Pan, X.-H.; Li, Q.-B.; Wang, X.-Q.; Jiao, X.-J.; Jia, Z.-W.; Wang, S.-J. Fifty top-cited classic papers in orthopedic elbow surgery: A bibliometric analysis. Int. J. Surg. 2015, 18, 28–33. [Google Scholar] [CrossRef]
- He, L.; Fang, H.; Wang, X.; Wang, Y.; Ge, H.; Li, C.; Chen, C.; Wan, Y.; He, H. The 100 most-cited articles in urological surgery: A bibliometric analysis. Int. J. Surg. 2020, 75, 74–79. [Google Scholar] [CrossRef]
- Qureshi, N.Q.; Mufarrih, S.H.; Bloomfield, G.S.; Tariq, W.; Almas, A.; Mokdad, A.H.; Bartlett, J.; Nisar, I.; Siddiqi, S.; Bhutta, Z.; et al. Disparities in Cardiovascular Research Output and Disease Outcomes among High-, Middle- and Low-Income Countries—An Analysis of Global Cardiovascular Publications over the Last Decade (2008–2017). Glob. Heart 2021, 16, 4. [Google Scholar] [CrossRef] [PubMed]
- Tas, F. An analysis of the most-cited research papers on oncology: Which journals have they been published in? Tumour Biol. 2014, 35, 4645–4649. [Google Scholar] [CrossRef] [PubMed]
- Tao, T.; Zhao, X.; Lou, J.; Bo, L.; Wang, F.; Li, J.; Deng, X. The top cited clinical research articles on sepsis: A bibliometric analysis. Crit. Care 2012, 16, R110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heath, G.W.; Parra, D.C.; Sarmiento, O.L.; Andersen, L.B.; Owen, N.; Goenka, S.; Montes, F.; Brownson, R.C. Lancet Physical Activity Series Working Group Evidence-based intervention in physical activity: Lessons from around the world. Lancet 2012, 380, 272–281. [Google Scholar] [CrossRef] [Green Version]
- Miltenburg, D.M.; Nuchtern, J.G.; Jaksic, T.; Kozinetiz, C.; Brandt, M.L. Laparoscopic evaluation of the pediatric inguinal hernia--a meta-analysis. J. Pediatr. Surg. 1998, 33, 874–879. [Google Scholar] [CrossRef]
- Allahabadi, S.; Feeley, S.E.; Lansdown, D.A.; Pandya, N.K.; Feeley, B.T. Influential Articles on Pediatric and Adolescent Anterior Cruciate Ligament Injuries: A Bibliometric Analysis. Orthop. J. Sport. Med. 2021, 9, 23259671211010772. [Google Scholar] [CrossRef] [PubMed]
- Allahabadi, S.; Eftekhari, A.; Feeley, S.E.; Feeley, B.T.; Lansdown, D.A. Influential and Highest Cited Shoulder Instability Articles: A Bibliometric Analysis. Orthop. J. Sport. Med. 2021, 9, 2325967121992577. [Google Scholar] [CrossRef]
- Talari, K.; Goyal, M. Retrospective studies—Utility and caveats. J. R. Coll. Physicians Edinb. 2020, 50, 398–402. [Google Scholar] [CrossRef]
- Euser, A.M.; Zoccali, C.; Jager, K.J.; Dekker, F.W. Cohort studies: Prospective versus retrospective. Nephron. Clin. Pract. 2009, 113, c214-7. [Google Scholar] [CrossRef] [Green Version]
- Hariton, E.; Locascio, J.J. Randomised controlled trials—The gold standard for effectiveness research: Study design: Randomised controlled trials. BJOG 2018, 125, 1716. [Google Scholar] [CrossRef] [Green Version]
- Kohno, M.; Ogawa, T.; Kojima, Y.; Sakoda, A.; Johnin, K.; Sugita, Y.; Nakane, A.; Noguchi, M.; Moriya, K.; Hattori, M.; et al. Pediatric congenital hydronephrosis (ureteropelvic junction obstruction): Medical management guide. Int. J. Urol. 2020, 27, 369–376. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Liu, C.; Li, Y.; Sun, C.; Li, X. Determination of the Need for Surgical Intervention in Infants Diagnosed with Fetal Hydronephrosis in China. Med. Sci. Monit. 2016, 22, 4210–4217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, H.L.; Roberts, J.P. Laparoscopic dismembered pyeloplasty in children: Preliminary results. Br. J. Urol. 1996, 77, 909–913. [Google Scholar] [CrossRef]
- Huang, Y.; Wu, Y.; Shan, W.; Zeng, L.; Huang, L. An updated meta-analysis of laparoscopic versus open pyeloplasty for ureteropelvic junction obstruction in children. Int. J. Clin. Exp. Med. 2015, 8, 4922–4931. [Google Scholar] [PubMed]
- Schmedding, A.; Rolle, U. Decentralized Rather than Centralized Pediatric Surgery Care in Germany. Eur. J. Pediatr. Surg. 2017, 27, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Knoedler, J.; Han, L.; Granberg, C.; Kramer, S.; Chow, G.; Gettman, M.; Kimball, B.; Moriarty, J.; Kim, S.; Husmann, D. Population-based comparison of laparoscopic and open pyeloplasty in paediatric pelvi-ureteric junction obstruction. BJU Int. 2013, 111, 1141–1147. [Google Scholar] [CrossRef] [PubMed]
- Goetz, G.; Klora, M.; Zeidler, J.; Eberhard, S.; Bassler, S.; Mayer, S.; Gosemann, J.-H.; Lacher, M. Surgery for Pediatric Ureteropelvic Junction Obstruction-Comparison of Outcomes in Relation to Surgical Technique and Operating Discipline in Germany. Eur. J. Pediatr. Surg. 2019, 29, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.-J.; Chen, J.Y.-C.; Hsu, C.-K.; Chuang, F.-C.; Yang, S.S.-D. The incidence of inguinal hernia and associated risk factors of incarceration in pediatric inguinal hernia: A nation-wide longitudinal population-based study. Hernia 2016, 20, 559–563. [Google Scholar] [CrossRef]
- Ponsky, T.A.; Nalugo, M.; Ostlie, D.J. Pediatric laparoscopic inguinal hernia repair: A review of the current evidence. J. Laparoendosc. Adv. Surg. Technol. A 2014, 24, 183–187. [Google Scholar] [CrossRef]
- Kostov, G.G.; Dimov, R.S. Total extra peritoneal inguinal hernia repair: A single-surgeon preliminary findings report. Folia Med. 2021, 63, 183–188. [Google Scholar] [CrossRef]
- Schier, F. Laparoscopic inguinal hernia repair-a prospective personal series of 542 children. J. Pediatr. Surg. 2006, 41, 1081–1084. [Google Scholar] [CrossRef] [PubMed]
- Montupet, P.; Esposito, C. Laparoscopic treatment of congenital inguinal hernia in children. J. Pediatr. Surg. 1999, 34, 420–423. [Google Scholar] [CrossRef]
- Morini, F.; Dreuning, K.M.A.; Janssen Lok, M.J.H.; Wester, T.; Derikx, J.P.M.; Friedmacher, F.; Miyake, H.; Zhu, H.; Pio, L.; Lacher, M.; et al. Surgical Management of Pediatric Inguinal Hernia: A Systematic Review and Guideline from the European Pediatric Surgeons’ Association Evidence and Guideline Committee. Eur. J. Pediatr. Surg. 2022, 32, 219–232. [Google Scholar] [CrossRef]
- Lee, S.R. Efficacy of laparoscopic herniorrhaphy for treating incarcerated pediatric inguinal hernia. Hernia 2018, 22, 671–679. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.R.; Park, P.J. Laparoscopic reoperation for pediatric recurrent inguinal hernia after previous laparoscopic repair. Hernia 2019, 23, 663–669. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Yu, C.; Lu, J.; Wei, Y.; Long, C.; Shen, L.; Lin, T.; He, D.; Wei, G.; Kou, L.; et al. Laparoscopic versus open inguinal hernia repair in children: A systematic review. J. Minim. Access Surg. 2019, 18, 12–19. [Google Scholar] [CrossRef]
- Lee, S. Basic Knowledge of Tracheoesophageal Fistula and Esophageal Atresia. Adv. Neonatal Care 2018, 18, 14–21. [Google Scholar] [CrossRef]
- Dingeldein, M. Congenital Diaphragmatic Hernia: Management & Outcomes. Adv. Pediatr. 2018, 65, 241–247. [Google Scholar] [CrossRef]
- Stocker, L.J.; Wellesley, D.G.; Stanton, M.P.; Parasuraman, R.; Howe, D.T. The increasing incidence of foetal echogenic congenital lung malformations: An observational study. Prenat. Diagn. 2015, 35, 148–153. [Google Scholar] [CrossRef]
- Becmeur, F.; Jamali, R.R.; Moog, R.; Keller, L.; Christmann, D.; Donato, L.; Kauffmann, I.; Schwaab, C.; Carrenard, G.; Sauvage, P. Thoracoscopic treatment for delayed presentation of congenital diaphragmatic hernia in the infant. A report of three cases. Surg. Endosc. 2001, 15, 1163–1166. [Google Scholar] [CrossRef]
- Bax, K.M.; van Der Zee, D.C. Feasibility of thoracoscopic repair of esophageal atresia with distal fistula. J. Pediatr. Surg. 2002, 37, 192–196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, S.M.; Grace, N.; Edwards, M.J.; Woo, R.; Puapong, D. Thoracoscopic segmentectomy for treatment of congenital lung malformations. J. Pediatr. Surg. 2011, 46, 2265–2269. [Google Scholar] [CrossRef] [PubMed]
- Gosemann, J.-H.; Lange, A.; Zeidler, J.; Blaser, J.; Dingemann, C.; Ure, B.M.; Lacher, M. Appendectomy in the pediatric population-a German nationwide cohort analysis. Langenbeck’s Arch. Surg. 2016, 401, 651–659. [Google Scholar] [CrossRef]
- Costerus, S.; Zahn, K.; van de Ven, K.; Vlot, J.; Wessel, L.; Wijnen, R. Thoracoscopic versus open repair of CDH in cardiovascular stable neonates. Surg. Endosc. 2016, 30, 2818–2824. [Google Scholar] [CrossRef] [Green Version]
- Thakkar, H.; Mullassery, D.M.; Giuliani, S.; Blackburn, S.; Cross, K.; Curry, J.; De Coppi, P. Thoracoscopic oesophageal atresia/tracheo-oesophageal fistula (OA/TOF) repair is associated with a higher stricture rate: A single institution’s experience. Pediatr. Surg. Int. 2021, 37, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Barroso, C.; Correia-Pinto, J. Perioperative Complications of Congenital Diaphragmatic Hernia Repair. Eur. J. Pediatr. Surg. 2018, 28, 141–147. [Google Scholar] [CrossRef]
- Uecker, M.; Kuebler, J.F.; Ure, B.M.; Schukfeh, N. Minimally Invasive Pediatric Surgery: The Learning Curve. Eur. J. Pediatr. Surg. 2020, 30, 172–180. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Huskić, D.; Čohadžić, T.; Jukić, M.; Šušnjar, T. Learning Curve for Laparoscopic Repair of Pediatric Inguinal Hernia Using Percutaneous Internal Ring Suturing. Children 2021, 8, 294. [Google Scholar] [CrossRef]
- Esparaz, J.R.; Jeziorczak, P.M.; Mowrer, A.R.; Chakraborty, S.R.; Nierstedt, R.T.; Zumpf, K.B.; Munaco, A.J.; Robertson, D.J.; Pearl, R.H.; Aprahamian, C.J. Adopting Single-Incision Laparoscopic Appendectomy in Children: Is It Safe During the Learning Curve? J. Laparoendosc. Adv. Surg. Technol. A 2019, 29, 1306–1310. [Google Scholar] [CrossRef]
- Tasian, G.E.; Wiebe, D.J.; Casale, P. Learning curve of robotic assisted pyeloplasty for pediatric urology fellows. J. Urol. 2013, 190, 1622–1626. [Google Scholar] [CrossRef] [Green Version]
- Binet, A.; Bastard, F.; Meignan, P.; Braïk, K.; Le Touze, A.; Villemagne, T.; Morel, B.; Robert, M.; Klipfel, C.; Lardy, H. Laparoscopic Pyloromyotomy: A Study of the Learning Curve. Eur. J. Pediatr. Surg. 2018, 28, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, P.; Martynov, I.; Perger, L.; Scholz, S.; Lacher, M. 20 Years of Single-Incision-Pediatric-Endoscopic-Surgery: A Survey on Opinion and Experience Among International Pediatric Endosurgery Group Members. J. Laparoendosc. Adv. Surg. Technol. A 2021, 31, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Navarrete-Arellano, M. Robotic-Assisted Minimally Invasive Surgery in Children. In Medical Robotics [Working Title]; IntechOpen: Vienna, Austria, 2021. [Google Scholar]
- Denning, N.-L.; Kallis, M.P.; Prince, J.M. Pediatric Robotic Surgery. Surg. Clin. N. Am. 2020, 100, 431–443. [Google Scholar] [CrossRef] [PubMed]





| “thoracoscopy” OR “thoracoscopic” OR “thoracoscopically” OR “laparoscopy” OR “laparoscopic” OR “laparoscopically” OR “minimal invasive surgery” OR “minimally invasive surgery” OR “robot assisted” |
| AND |
| “neonate” OR “neonates” OR “neonatal” OR “infant” OR “infants” OR “infancy” OR “preterm” OR “preterms” OR “newborn” OR “newborns” OR “pediatric” OR “pediatrics” OR “children” OR “child” OR “boy” OR “girl” OR “boys” OR “girls” OR “adolescent” OR “congenital” OR “atresia” OR “tracheoesophageal fistula” OR “necrotizing enterocolitis” OR “Hirschsprung disease” OR “anorectal malformation” OR “neuroblastoma” OR “hepatoblastoma” OR “nephroblastoma” OR “wilms” OR “orchidopexy” OR “pyloromyotomy” OR “Kasai” OR “imperforate anus” |
| NOT |
| “CHD” OR “patent ductus arteriosus” OR “PDA” OR “neurosurgery” OR “thalamic astrocytomas” OR “GAIT” OR “Palsy” OR “stereoelectroencephalography” OR “ASD” OR “Autism” OR “brain” OR “brainstem” OR “neuromotor” OR “attention-deficit hyperactivity disorder” OR “ADHD” OR “idiopathic scoliosis” OR “spinal” OR “spine” |
| Publication First Author | Journal | Total Citations (n) | Year | Impact Index | Impact Factor (2020) | Evidence Level | Country | |
|---|---|---|---|---|---|---|---|---|
| 1 | Pediatric robot assisted laparoscopic dismembered pyeloplasty: Comparison with a cohort of open surgery | |||||||
| Lee RS | J Urol | 221 | 2006 | 6.3 | 5.9 | retrospective | USA | |
| 2 | Laparoscopically assisted anorectal pull-through for high imperforate anus—A new technique | |||||||
| Georgeson KE | J Pediatr Surg | 220 | 2000 | 9.1 | 1.9 | retrospective | USA | |
| 3 | Primary laparoscopic pull-through for hirschsprungs-disease in infants and children | |||||||
| Georgeson KE | J Pediatr Surg | 212 | 1995 | 11.8 | 1.9 | case report | USA | |
| 4 | Laparoscopic versus open appendectomy in children—A meta-analysis | |||||||
| Aziz O | Ann Surg | 205 | 2006 | 6.8 | 10.1 | meta analysis | UK | |
| 5 | Pediatric laparoscopic dismembered pyeloplasty | |||||||
| Peters CA | J Urol | 193 | 1995 | 13.0 | 5.9 | case report | USA | |
| 6 | Single-port laparoscopic surgery: initial experience in children for varicocelectomy | |||||||
| Kaouk JH | BJU Int | 182 | 2008 | 6.6 | 4.8 | case report | USA | |
| 7 | Thoracoscopic repair of esophageal atresia and tracheoesophageal fistula—A multi-institutional analysis | |||||||
| Holcomb GW | Ann Surg | 182 | 2005 | 8.2 | 10.1 | retrospective | USA | |
| 8 | Congenital choledochal cyst: video-guided laparoscopic treatment | |||||||
| Farello GA | Surg Laparosc Endosc | 167 | 1995 | 15.0 | 1.4 | case report | Italy | |
| 9 | Laparoscopic inguinal herniorrhaphy in children: A three-center experience with 933 repairs | |||||||
| Schier F | J Pediatr Surg | 164 | 2002 | 11.0 | 1.9 | retrospective | Germany | |
| 10 | Thoracoscopic decortication vs. tube thoracostomy with fibrinolysis for empyema in children: a prospective, randomized trial | |||||||
| St Peter SD | J Pediatr Surg | 157 | 2009 | 7.0 | 1.9 | RCT | USA | |
| 11 | Laparoscopic inguinal hernia repair—a prospective personal series of 542 children | |||||||
| Schier F | J Pediatr Surg | 155 | 2006 | 9.0 | 1.9 | prospective | Germany | |
| 12 | Laparoscopic Anderson-Hynes dismembered pyeloplasty in children | |||||||
| Tan HL | J Urol | 151 | 1999 | 13.9 | 5.9 | retrospective | UK | |
| 13 | Laparoscopic percutaneous extraperitoneal closure for inguinal hernia in children: clinical outcome of 972 repairs done in 3 pediatric surgical institutions | |||||||
| Takehara H | J Pediatr Surg | 149 | 2006 | 9.4 | 1.9 | retrospective | Japan | |
| 14 | Early Experience with Single-Port Laparoscopic Surgery in Children | |||||||
| Ponsky TA | J Laparoendosc Adv Surg Tech A | 141 | 2009 | 7.8 | 1.4 | retrospective | USA | |
| 15 | Laparoscopic vesicoureteroplasty in children: initial case reports | |||||||
| Ehrlich RM | Urology | 136 | 1994 | 19.1 | 1.9 | case report | USA | |
| 16 | A multi-institutional analysis of laparoscopic orchidopexy | |||||||
| Baker LA | BJU Int | 129 | 2001 | 14.7 | 4.8 | retrospective | USA | |
| 17 | Laparoscopic treatment of congenital inguinal hernia in children | |||||||
| Montupet P | J Pediatr Surg | 126 | 1999 | 16.7 | 1.9 | retrospective | Italy | |
| 18 | Open versus laparoscopic pyloromyotomy for pyloric stenosis—A prospective, randomized trial | |||||||
| St Peter SD | Ann Surg | 124 | 2006 | 11.3 | 10.1 | RCT | USA | |
| 19 | Prospective, randomized, single-center, single-blind comparison of laparoscopic vs. open repair of pediatric inguinal hernia | |||||||
| Chan KL | Surg Endosc | 123 | 2005 | 12.2 | 3.1 | RCT | Peoples R China | |
| 20 | Initial comparison of robotic-assisted laparoscopic versus open pyeloplasty in children | |||||||
| Yee DS | Urology | 120 | 2006 | 11.7 | 1.9 | retrospective | USA | |
| 21 | Recovery after open versus laparoscopic pyloromyotomy for pyloric stenosis: A double-blind multicentre randomised controlled trial | |||||||
| Hall NJ | Lancet | 113 | 2009 | 9.7 | 60.4 | RCT | UK | |
| 22 | Retroperitoneal laparoscopic versus open pyeloplasty in children | |||||||
| Bonnard A | J Urol | 112 | 2005 | 13.4 | 6 | retrospective | France | |
| 23 | Laparoscopic Sleeve Gastrectomy in 108 Obese Children and Adolescents Aged 5 to 21 Years | |||||||
| Alqahtani AR | Ann Surg | 111 | 2012 | 7.2 | 10.1 | retrospective | Saudi Arabia | |
| 24 | Experience with 220 consecutive laparoscopic Nissen fundoplications in infants and children | |||||||
| Rothenberg SS | J Pediatr Surg | 110 | 1998 | 20.0 | 1.9 | retrospective | USA | |
| 25 | Laparoscopic renal surgery via a retroperitoneal approach in children | |||||||
| El-Ghoneimi A | J Urol | 110 | 1998 | 20.0 | 5.9 | retrospective | France | |
| 26 | Is there a role for laparoscopic appendectomy in pediatric surgery? | |||||||
| Gilchrist BF | J Pediatr Surg | 109 | 1992 | 25.7 | 1.9 | prospective | USA | |
| 27 | Thoracoscopic repair of tracheoesophageal fistula in newborns | |||||||
| Rothenberg SS | J Pediatr Surg | 108 | 2002 | 16.7 | 1.9 | retrospective | USA | |
| 28 | Laparoscopic dismembered pyeloplasty by a retroperitoneal approach in children | |||||||
| El-Ghoneimi A | BJU Int | 108 | 2003 | 15.7 | 4.8 | retrospective | France | |
| 29 | Robotic assisted laparoscopic pyeloplasty in children | |||||||
| Atug F | J Urol | 108 | 2005 | 13.9 | 5.9 | retrospective | USA | |
| 30 | Laparoscopic evaluation of the pediatric inguinal hernia—A meta-analysis | |||||||
| Miltenburg DW | J Pediatr Surg | 109 | 1998 | 21.0 | 1.9 | meta analysis | USA | |
| 31 | Pediatric laparoscopic splenectomy | |||||||
| Tulman S | J Pediatr Surg | 103 | 1993 | 26.2 | 1.9 | case report | USA | |
| 32 | Thoracoscopy in the management of empyema in children | |||||||
| Kern JA | J Pediatr Surg | 103 | 1993 | 26.2 | 1.9 | retrospective | USA | |
| 33 | Robotic Assisted Laparoscopic Ureteral Reimplantation in Children: Case Matched Comparative Study With Open Surgical Approach | |||||||
| Marchini Giovanni S | J Urol | 101 | 2011 | 8.9 | 5.9 | retrospective | USA | |
| 34 | Laparoscopic splenic procedures in children—Experience in 231 children | |||||||
| Rescorla FJ | Ann Surg | 100 | 2007 | 13.0 | 10.1 | retrospective | USA | |
| 35 | Thoracoscopy Versus Thoracotomy Improves Midterm Musculoskeletal Status and Cosmesis in Infants and Children | |||||||
| Lawal Taiwo A | Ann Thorac Surg | 100 | 2009 | 11.0 | 3.6 | retrospective | Germany | |
| 36 | Laparoscopic heminephroureterectomy in pediatric patients | |||||||
| Janetschek G | J Urol | 100 | 1997 | 23.0 | 5.9 | retrospective | Austria | |
| 37 | Laparoscopic transabdominal pyeloplasty in children is feasible irrespective of age | |||||||
| Metzelder ML | J Urol | 99 | 2006 | 14.1 | 5.9 | retrospective | Germany | |
| 38 | Hypercapnia and Acidosis During Open and Thoracoscopic Repair of Congenital Diaphragmatic Hernia and Esophageal Atresia Results of a Pilot Randomized Controlled Trial | |||||||
| Bishay M | Ann Surg | 97 | 2013 | 7.2 | 10.1 | RCT | Canada | |
| 39 | Neonatal thoracoscopic repair of congenital diaphragmatic hernia: Selection criteria for successful outcome | |||||||
| Yang EY | J Pediatr Surg | 95 | 2005 | 15.8 | 1.9 | retrospective | USA | |
| 40 | Extramucosal pyloromyotomy by laparoscopy | |||||||
| Alain JL | Surg Endosc | 94 | 1991 | 30.9 | 3.1 | retrospective | France | |
| 41 | Retroperitoneal laparoscopic vs. open partial nephroureterectomy in children | |||||||
| El-Ghoneimi A | BJU Int | 93 | 2003 | 18.3 | 4.8 | retrospective | France | |
| 42 | Laparoscopic pyloromyotomy for hypertrophic pyloric stenosis: A prospective, randomized controlled trial | |||||||
| Leclair MD | J Pediatr Surg | 92 | 2007 | 14.1 | 1.9 | RCT | France | |
| 43 | Single-blind randomized clinical trial of laparoscopic versus open appendicectomy in children | |||||||
| Lintula H | Br J Surg | 91 | 2001 | 24.2 | 5.7 | RCT | Finland | |
| 44 | Laparoscopic herniorrhaphy in girls | |||||||
| Schier F | J Pediatr Surg | 91 | 1998 | 20.9 | 1.9 | retrospective | Germany | |
| 45 | One-trocar transumbilical laparoscopic-assisted appendectomy in children: Our experience | |||||||
| D’Alessio A | Eur J Pediatr Surg | 91 | 2002 | 19.8 | 2.3 | retrospective | Italy | |
| 46 | Experience with Modified Single-Port Laparoscopic Procedures in Children | |||||||
| Rothenberg SS | J Laparoendosc Adv Surg Tech A | 90 | 2009 | 12.2 | 1.4 | retrospective | USA | |
| 47 | Complications in pediatric urological laparoscopy: Results of a survey | |||||||
| Peters CA | J Urol | 90 | 1996 | 26.7 | 5.9 | retrospective | USA | |
| 48 | Laparoscopic pyeloplasty in the infant younger than 6 months—Is it technically possible? | |||||||
| Kutikov A | J Urol | 90 | 2006 | 15.6 | 5.9 | retrospective | USA | |
| 49 | Initial experience with laparoscopic transvesical ureteral reimplantation at the Children’s Hospital of Philadelphia | |||||||
| Kutikov A | J Urol | 90 | 2006 | 15.6 | 5.9 | retrospective | USA | |
| 50 | Should laparoscopic appendectomy be avoided for complicated appendicitis in children? | |||||||
| Horwitz JR | J Pediatr Surg | 90 | 1997 | 25.6 | 1.9 | retrospective | USA | |
| Publication First Author | Journal | Total Citations (n) | Year | Impact Index | Impact Factor (2020) | Evidence Level | Country | |
|---|---|---|---|---|---|---|---|---|
| 1 | Pediatric Robot Assisted Laparoscopic Dismembered Pyeloplasty: Comparison with a Cohort of Open Surgery | |||||||
| Lee RS | J Urol | 221 | 2006 | 6.3 | 5.9 | retrospective | USA | |
| 2 | Single-Port Laparoscopic Surgery: Initial Experience in Children for Varicocelectomy | |||||||
| Kaouk JH | BJU Int | 182 | 2008 | 6.6 | 4.8 | case report | USA | |
| 3 | Laparoscopic Versus Open Appendectomy in Children—A Meta-Analysis | |||||||
| Aziz O | Ann Surg | 205 | 2006 | 6.8 | 10.1 | meta-analysis | UK | |
| 4 | Thoracoscopic Decortication Vs. Tube Thoracostomy with Fibrinolysis for Empyema in Children: A Prospective, Randomized Trial | |||||||
| St Peter SD | J Pediatr Surg | 157 | 2009 | 7 | 1.9 | RCT | USA | |
| 5 | Laparoscopic Sleeve Gastrectomy in 108 Obese Children and Adolescents Aged 5 to 21 Years | |||||||
| Alqahtani AR | Ann Surg | 111 | 2012 | 7.2 | 10.1 | retrospective | Saudi Arabia | |
| 6 | Hypercapnia and Acidosis During Open and Thoracoscopic Repair of Congenital Diaphragmatic Hernia and Esophageal Atresia Results of a Pilot Randomized Controlled Trial | |||||||
| Bishay M | Ann Surg | 97 | 2013 | 7.2 | 10.1 | RCT | Canada | |
| 7 | Early Experience with Single-Port Laparoscopic Surgery in Children | |||||||
| Ponsky TA | J Laparoendosc Adv Surg Tech A | 141 | 2009 | 7.8 | 1.4 | retrospective | USA | |
| 8 | Thoracoscopic Repair of Esophageal Atresia and Tracheoesophageal Fistula—A Multi-Institutional Analysis | |||||||
| Holcomb GW | Ann Surg | 182 | 2005 | 8.2 | 10.1 | retrospective | USA | |
| 9 | Robotic Assisted Laparoscopic Ureteral Reimplantation in Children: Case Matched Comparative Study with Open Surgical Approach | |||||||
| Marchini Giovanni S | J Urol | 101 | 2011 | 8.9 | 5.9 | retrospective | USA | |
| 10 | Laparoscopic Inguinal Hernia Repair—A Prospective Personal Series of 542 Children | |||||||
| Schier F | J Pediatr Surg | 155 | 2006 | 9 | 1.9 | prospective | Germany | |
| 11 | Laparoscopically Assisted Anorectal Pull-Through for High Imperforate Anus—A New Technique | |||||||
| Georgeson KE | J Pediatr Surg | 220 | 2000 | 9.1 | 1.9 | retrospective | USA | |
| 12 | Laparoscopic Percutaneous Extraperitoneal Closure for Inguinal Hernia in Children: Clinical Outcome Of 972 Repairs Done In 3 Pediatric Surgical Institutions | |||||||
| Takehara H | J Pediatr Surg | 149 | 2006 | 9.4 | 1.9 | retrospective | Japan | |
| 13 | Recovery After Open Versus Laparoscopic Pyloromyotomy for Pyloric Stenosis: A Double-Blind Multicentre Randomised Controlled Trial | |||||||
| Hall NJ | Lancet | 113 | 2009 | 9.7 | 60.4 | RCT | UK | |
| 14 | Laparoscopic Inguinal Herniorrhaphy In Children: A Three-Center Experience With 933 Repairs | |||||||
| Schier F | J Pediatr Surg | 164 | 2002 | 11 | 1.9 | retrospective | Germany | |
| 15 | Thoracoscopy Versus Thoracotomy Improves Midterm Musculoskeletal Status and Cosmesis in Infants And Children | |||||||
| Lawal Taiwo A | Ann Thorac Surg | 100 | 2009 | 11 | 3.6 | retrospective | Germany | |
| 16 | Open Versus Laparoscopic Pyloromyotomy for Pyloric Stenosis—A Prospective, Randomized Trial | |||||||
| St Peter SD | Ann Surg | 124 | 2006 | 11.3 | 10.1 | RCT | USA | |
| 17 | Initial Comparison Of Robotic-Assisted Laparoscopic Versus Open Pyeloplasty in Children | |||||||
| Yee DS | Urology | 120 | 2006 | 11.7 | 1.9 | retrospective | USA | |
| 18 | Primary Laparoscopic Pull-Through for Hirschsprungs-Disease In Infants and Children | |||||||
| Georgeson KE | J Pediatr Surg | 212 | 1995 | 11.8 | 1.9 | case report | USA | |
| 19 | Prospective, Randomized, Single-Center, Single-Blind Comparison of Laparoscopic Vs. Open Repair of Pediatric Inguinal Hernia | |||||||
| Chan KL | Surg Endosc | 123 | 2005 | 12.2 | 3.1 | RCT | Peoples R China | |
| 20 | Experience with Modified Single-Port Laparoscopic Procedures in Children | |||||||
| Rothenberg SS | J Laparoendosc Adv Surg Tech A | 90 | 2009 | 12.2 | 1.4 | retrospective | USA | |
| 21 | Pediatric Laparoscopic Dismembered Pyeloplasty | |||||||
| Peters CA | J Urol | 193 | 1995 | 13 | 5.9 | case report | USA | |
| 22 | Laparoscopic Splenic Procedures in Children—Experience in 231 Children | |||||||
| Rescorla FJ | Ann Surg | 100 | 2007 | 13 | 10.1 | retrospective | USA | |
| 23 | Retroperitoneal Laparoscopic Versus Open Pyeloplasty in Children | |||||||
| Bonnard A | J Urol | 112 | 2005 | 13.4 | 6 | retrospective | France | |
| 24 | Laparoscopic Anderson-Hynes Dismembered Pyeloplasty in Children | |||||||
| Tan HL | J Urol | 151 | 1999 | 13.9 | 5.9 | retrospective | UK | |
| 25 | Robotic Assisted Laparoscopic Pyeloplasty in Children | |||||||
| Atug F | J Urol | 108 | 2005 | 13.9 | 5.9 | retrospective | USA | |
| 26 | Laparoscopic Transabdominal Pyeloplasty in Children Is Feasible Irrespective of Age | |||||||
| Metzelder ML | J Urol | 99 | 2006 | 14.1 | 5.9 | retrospective | Germany | |
| 27 | Laparoscopic Pyloromyotomy for Hypertrophic Pyloric Stenosis: A Prospective, Randomized Controlled Trial | |||||||
| Leclair MD | J Pediatr Surg | 92 | 2007 | 14.1 | 1.9 | RCT | France | |
| 28 | A Multi-Institutional Analysis of Laparoscopic Orchidopexy | |||||||
| Baker LA | BJU Int | 129 | 2001 | 14.7 | 4.8 | retrospective | USA | |
| 29 | Congenital Choledochal Cyst: Video-Guided Laparoscopic Treatment | |||||||
| Farello GA | Surg Laparosc Endosc | 167 | 1995 | 15 | 1.4 | case report | Italy | |
| 30 | Laparoscopic pyeloplasty in the infant younger than 6 months—Is it technically possible? | |||||||
| Kutikov A | J Urol | 90 | 2006 | 15.6 | 5.9 | retrospective | USA | |
| 31 | Initial experience with laparoscopic transvesical ureteral reimplantation at the Children’s Hospital of Philadelphia | |||||||
| Kutikov A | J Urol | 90 | 2006 | 15.6 | 5.9 | retrospective | USA | |
| 32 | Laparoscopic Dismembered Pyeloplasty by a Retroperitoneal Approach in Children | |||||||
| El-Ghoneimi A | BJU Int | 108 | 2003 | 15.7 | 4.8 | retrospective | France | |
| 33 | Neonatal Thoracoscopic Repair of Congenital Diaphragmatic Hernia: Selection Criteria for Successful Outcome | |||||||
| Yang EY | J Pediatr Surg | 95 | 2005 | 15.8 | 1.9 | retrospective | USA | |
| 34 | Laparoscopic Treatment of Congenital Inguinal Hernia in Children | |||||||
| Montupet P | J Pediatr Surg | 126 | 1999 | 16.7 | 1.9 | retrospective | Italy | |
| 35 | Thoracoscopic Repair of Tracheoesophageal Fistula in Newborns | |||||||
| Rothenberg SS | J Pediatr Surg | 108 | 2002 | 16.7 | 1.9 | retrospective | USA | |
| 36 | Retroperitoneal Laparoscopic Vs. Open Partial Nephroureterectomy in Children | |||||||
| El-Ghoneimi A | BJU Int | 93 | 2003 | 18.3 | 4.8 | retrospective | France | |
| 37 | Laparoscopic Vesicoureteroplasty in Children: Initial Case Reports | |||||||
| Ehrlich RM | Urology | 136 | 1994 | 19.1 | 1.9 | case report | USA | |
| 38 | One-Trocar Transumbilical Laparoscopic-Assisted Appendectomy in Children: Our Experience | |||||||
| D’Alessio A | Eur J Pediatr Surg | 91 | 2002 | 19.8 | 2.3 | retrospective | Italy | |
| 39 | Experience with 220 Consecutive Laparoscopic Nissen Fundoplications in Infants and Children | |||||||
| Rothenberg SS | J Pediatr Surg | 110 | 1998 | 20 | 1.9 | retrospective | USA | |
| 40 | Laparoscopic Renal Surgery Via a Retroperitoneal Approach in Children | |||||||
| El-Ghoneimi A | J Urol | 110 | 1998 | 20 | 5.9 | retrospective | France | |
| 41 | Laparoscopic Herniorrhaphy in Girls | |||||||
| Schier F | J Pediatr Surg | 91 | 1998 | 20.9 | 1.9 | retrospective | Germany | |
| 42 | Laparoscopic Evaluation of the Pediatric Inguinal Hernia—A Meta-Analysis | |||||||
| Miltenburg DW | J Pediatr Surg | 109 | 1998 | 21 | 1.9 | meta-analysis | USA | |
| 43 | Laparoscopic heminephroureterectomy in pediatric patients | |||||||
| Janetschek G | J Urol | 100 | 1997 | 23.0 | 5.9 | retrospective | Austria | |
| 44 | Single-Blind Randomized Clinical Trial of Laparoscopic Versus Open Appendicectomy in Children | |||||||
| Lintula H | Br J Surg | 91 | 2001 | 24.2 | 5.7 | RCT | Finland | |
| 45 | Should Laparoscopic Appendectomy Be Avoided for Complicated Appendicitis in Children? | |||||||
| Horwitz JR | J Pediatr Surg | 90 | 1997 | 25.6 | 1.9 | retrospective | USA | |
| 46 | Is There a Role For Laparoscopic Appendectomy in Pediatric Surgery? | |||||||
| Gilchrist BF | J Pediatr Surg | 109 | 1992 | 25.7 | 1.9 | prospective | USA | |
| 47 | Pediatric Laparoscopic Splenectomy | |||||||
| Tulman S | J Pediatr Surg | 103 | 1993 | 26.2 | 1.9 | case report | USA | |
| 48 | Thoracoscopy in the Management of Empyema in Children | |||||||
| Kern JA | J Pediatr Surg | 103 | 1993 | 26.2 | 1.9 | retrospective | USA | |
| 49 | Complications In Pediatric Urological Laparoscopy: Results of a Survey | |||||||
| Peters CA | J Urol | 90 | 1996 | 26.7 | 5.9 | retrospective | USA | |
| 50 | Extramucosal Pyloromyotomy by Laparoscopy | |||||||
| Alain JL | Surg Endosc | 94 | 1991 | 30.9 | 3.1 | retrospective | France | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shu, B.; Feng, X.; Martynov, I.; Lacher, M.; Mayer, S. Pediatric Minimally Invasive Surgery—A Bibliometric Study on 30 Years of Research Activity. Children 2022, 9, 1264. https://doi.org/10.3390/children9081264
Shu B, Feng X, Martynov I, Lacher M, Mayer S. Pediatric Minimally Invasive Surgery—A Bibliometric Study on 30 Years of Research Activity. Children. 2022; 9(8):1264. https://doi.org/10.3390/children9081264
Chicago/Turabian StyleShu, Boshen, Xiaoyan Feng, Illya Martynov, Martin Lacher, and Steffi Mayer. 2022. "Pediatric Minimally Invasive Surgery—A Bibliometric Study on 30 Years of Research Activity" Children 9, no. 8: 1264. https://doi.org/10.3390/children9081264
APA StyleShu, B., Feng, X., Martynov, I., Lacher, M., & Mayer, S. (2022). Pediatric Minimally Invasive Surgery—A Bibliometric Study on 30 Years of Research Activity. Children, 9(8), 1264. https://doi.org/10.3390/children9081264







