A Comparison of Clinical Features of Youth with and without Rhinitis Signs and Symptoms Who Are Hospitalized for Headache
Abstract
1. Introduction
2. Materials and Methods
2.1. Cases and Data Collection
- Medical records
- Age
- Sex
- Body Mass Index (BMI)
- Headache-specific history: Time of onset, duration, and severity (numerical rating scale)
- Associated allergic disease: Atopic dermatitis, asthma, allergic conjunctivitis
- Symptoms of rhinitis: Nasal congestion, sneezing, itching, rhinorrhea
- Family history (headache, allergic disease)
- Medical background (headache and allergy medications)
- Treatment and clinical outcomes
- Examination data
- Laboratory results: White blood cell (WBC) count, hemoglobin (Hb), platelet (PLT), aspartate aminotransferase (AST), alanine aminotransferase (ALT), blood urea nitrogen (BUN), creatinine (Cre), sodium (Na), potassium (K), and total Immunoglobulin E (IgE) levels.
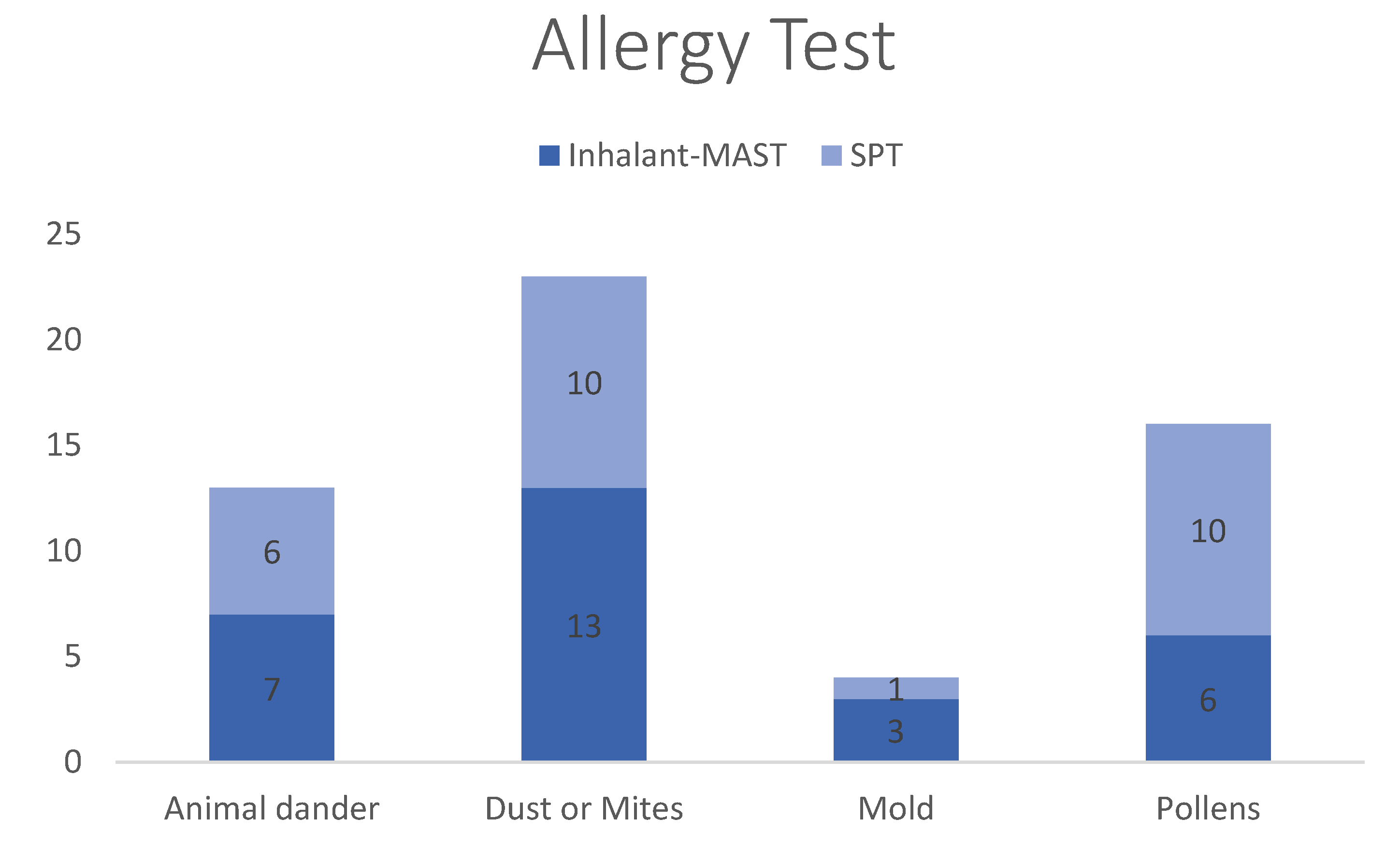
- Allergy test: skin prick test (SPT), inhalant multiple allergen simultaneous test (inhalant MAST), and screening for common allergens (animal dander, dust, mites, mold, and pollen).
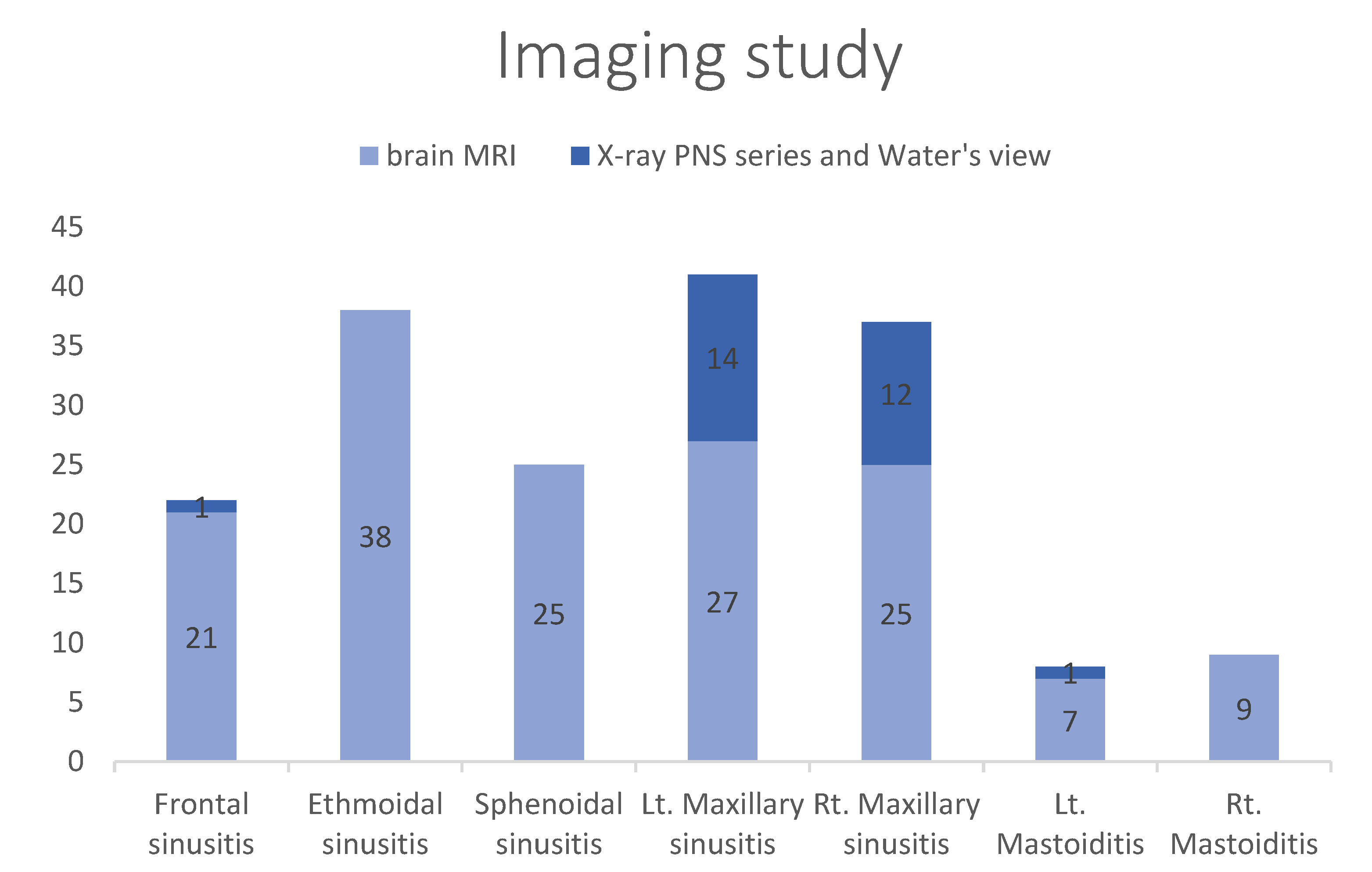
- Imaging data: Brain magnetic resonance imaging (MRI), brain computed tomography (CT), and X-ray paranasal sinus (PNS) series and water view.
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bille, B. A 40-Year Follow-up of School Children with Migraine. Cephalalgia 1997, 17, 488–491. [Google Scholar] [CrossRef]
- Roser, T.; Bonfert, M.; Ebinger, F.; Blankenburg, M.; Ertl-Wagner, B.; Heinen, F. Primary versus Secondary Headache in Children: A Frequent Diagnostic Challenge in Clinical Routine. Neuropediatrics 2013, 44, 34–39. [Google Scholar] [PubMed]
- Powers, S.W.; Patton, S.R.; Hommel, K.A.; Hershey, A.D. Quality of Life in Childhood Migraines: Clinical Impact and Comparison to Other Chronic Illnesses. Pediatrics 2003, 112, e1–e5. [Google Scholar] [CrossRef] [PubMed]
- Lateef, T.M.; Cui, L.; Nelson, K.B.; Nakamura, E.F.; Merikangas, K.R. Physical Comorbidity of Migraine and Other Headaches in US Adolescents. J. Pediatr. 2012, 161, 308–313. [Google Scholar] [CrossRef] [PubMed]
- Güvenç, I.A.; Acar, M.; Muluk, N.B.; Kucukcan, N.E.; Cingi, C. Is There an Association between Migraine and Allergic Rhinitis? Ear Nose Throat J. 2017, 96, E18–E23. [Google Scholar] [CrossRef] [PubMed]
- Şenbil, N.; Gürer, Y.K.; Üner, Ç.; Barut, Y. Sinusitis in Children and Adolescents with Chronic or Recurrent Headache: A Case–Control Study. J. Headache Pain 2008, 9, 33–36. [Google Scholar] [CrossRef]
- Gazerani, P.; Pourpak, Z.; Ahmadiani, A.; Hemmati, A.; Kazemnejad, A. A Correlation between Migraine, Histamine and Immunoglobulin E. Scand. J. Immunol. 2003, 57, 286–290. [Google Scholar] [CrossRef]
- Ku, M.; Silverman, B.; Prifti, N.; Ying, W.; Persaud, Y.; Schneider, A. Prevalence of Migraine Headaches in Patients with Allergic Rhinitis. Ann. Allergy Asthma Immunol. 2006, 97, 226–230. [Google Scholar] [CrossRef]
- Eross, E.; Dodick, D.; Eross, M. The Sinus, Allergy and Migraine Study (SAMS) CME. Headache J. Head Face Pain 2007, 47, 213–224. [Google Scholar] [CrossRef]
- Mehle, M.E. Allergy and Migraine: Is There a Connection? Curr. Opin. Otolaryngol. Head Neck Surg. 2008, 16, 265–269. [Google Scholar] [CrossRef]
- Wheatley, L.M.; Togias, A. Allergic Rhinitis. N. Engl. J. Med. 2015, 372, 456–463. [Google Scholar] [CrossRef] [PubMed]
- Manzoni, G.C.; Torelli, P. Chronic Headaches: A Clinician’s Experience of ICHD-3 Beta. Neurol. Sci. 2015, 36, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Bijur, P.E.; Latimer, C.T.; Gallagher, E.J. Validation of a Verbally Administered Numerical Rating Scale of Acute Pain for Use in the Emergency Department. Acad. Emerg. Med. 2003, 10, 390–392. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, A.M.; Stewart, R.E.; Köke, A.J.A.; Oosterwijk, R.F.A.; Swaan, J.L.; Schreurs, K.M.G.; Schiphorst Preuper, H.R. Cut-off Points for Mild, Moderate, and Severe Pain on the Numeric Rating Scale for Pain in Patients with Chronic Musculoskeletal Pain: Variability and Influence of Sex and Catastrophizing. Front. Psychol. 2016, 7, 1466. [Google Scholar] [CrossRef] [PubMed]
- Cady, R.K.; Schreiber, C.P. Sinus Headache: A Clinical Conundrum. Otolaryngol. Clin. N. Am. 2004, 37, 267–288. [Google Scholar] [CrossRef]
- Schankin, C.J.; Straube, A. Secondary Headaches: Secondary or Still Primary? J. Headache Pain 2012, 13, 263–270. [Google Scholar] [CrossRef]
- Gurkas, E.; Karalok, Z.S.; Taskın, B.D.; Aydogmus, U.; Yılmaz, C.; Bayram, G. Brain Magnetic Resonance Imaging Findings in Children with Headache. Arch. Argent. Pediatr. 2017, 115, e349–e355. [Google Scholar] [PubMed]
- Tran, N.P.; Vickery, J.; Blaiss, M.S. Management of Rhinitis: Allergic and Non-Allergic. Allergy. Asthma Immunol. Res. 2011, 3, 148–156. [Google Scholar] [CrossRef]
- Özge, A.; Öksüz, N.; Ayta, S.; Uluduz, D.; Yıldırım, V.; Toros, F.; Taşdelen, B. Atopic Disorders Are More Common in Childhood Migraine and Correlated Headache Phenotype. Pediatr. Int. 2014, 56, 868–872. [Google Scholar] [CrossRef]
- Ozturk, A.; Degirmenci, Y.; Tokmak, B.; Tokmak, A. Frequency of Migraine in Patients with Allergic Rhinitis. Pak. J. Med. Sci. 2013, 29, 528. [Google Scholar] [CrossRef]
- Gryglas, A. Allergic Rhinitis and Chronic Daily Headaches: Is There a Link? Curr. Neurol. Neurosci. Rep. 2016, 16, 1–8. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Blume, H.K. Childhood Headache: A Brief Review. Pediatr. Ann. 2017, 46, e155–e165. [Google Scholar] [CrossRef] [PubMed]
- Cady, R.K.; Dodick, D.W.; Levine, H.L.; Schreiber, C.P.; Eross, E.J.; Setzen, M.; Blumenthal, H.J.; Lumry, W.R.; Berman, G.D.; Durham, P.L. Sinus headache: A neurology, otolaryngology, allergy, and primary care consensus on diagnosis and treatment. Mayo Clinic Proc. 2005, 80, 908–916. [Google Scholar] [CrossRef] [PubMed]
- Saberi, A.; Nemati, S.; Shakib, R.J.; Kazemnejad, E.; Maleki, M. Association between Allergic Rhinitis and Migraine. J. Res. Med. Sci. Off. J. Isfahan Univ. Med. Sci. 2012, 17, 508. [Google Scholar]
- Shin, Y.; Park, H.; Shim, J.; Oh, M.; Kim, M. Seasonal Variation, Cranial Autonomic Symptoms, and Functional Disability in Migraine: A Questionnaire-based Study in Tertiary Care. Headache J. Head Face Pain 2015, 55, 1112–1123. [Google Scholar] [CrossRef] [PubMed]
- Macy, E. A Rhinitis Primer for Family Medicine. Perm. J. 2012, 16, 61. [Google Scholar] [CrossRef]
- Passali, F.M.; Spinosi, M.C.; Mignacco, G.; Cingi, C.; Rodriguez, H.A.; Passali, D. Influence of Allergic Rhinitis in Children and Adolescents with Recurrent Headache. Otolaryngol. Pol. 2018, 70, 50–59. [Google Scholar] [CrossRef]
- Scher, A.I.; Stewart, W.F.; Ricci, J.A.; Lipton, R.B. Factors Associated with the Onset and Remission of Chronic Daily Headache in a Population-Based Study. Pain 2003, 106, 81–89. [Google Scholar] [CrossRef]
- Bigal, M.E.; Tsang, A.; Loder, E.; Serrano, D.; Reed, M.L.; Lipton, R.B. Body Mass Index and Episodic Headaches: A Population-Based Study. Arch. Intern. Med. 2007, 167, 1964–1970. [Google Scholar] [CrossRef]
- Bigal, M.E.; Lipton, R.B.; Holland, P.R.; Goadsby, P.J. Obesity, Migraine, and Chronic Migraine: Possible Mechanisms of Interaction. Neurology 2007, 68, 1851–1861. [Google Scholar] [CrossRef]
- Kim, Y.H.; Yu, B.J.; Kim, W.J.; Kim, J.E.; Lee, G.-H.; Lee, K.-A.; Cho, J.H. Correlation between Skin Prick Test and MAST-Immunoblot Results in Patients with Chronic Rhinitis. Asian Pac. J. Allergy Immunol. 2013, 31, 20–25. [Google Scholar] [PubMed]
- Mehle, M.E. Migraine and Allergy: A Review and Clinical Update. Curr. Allergy Asthma Rep. 2012, 12, 240–245. [Google Scholar] [CrossRef] [PubMed]
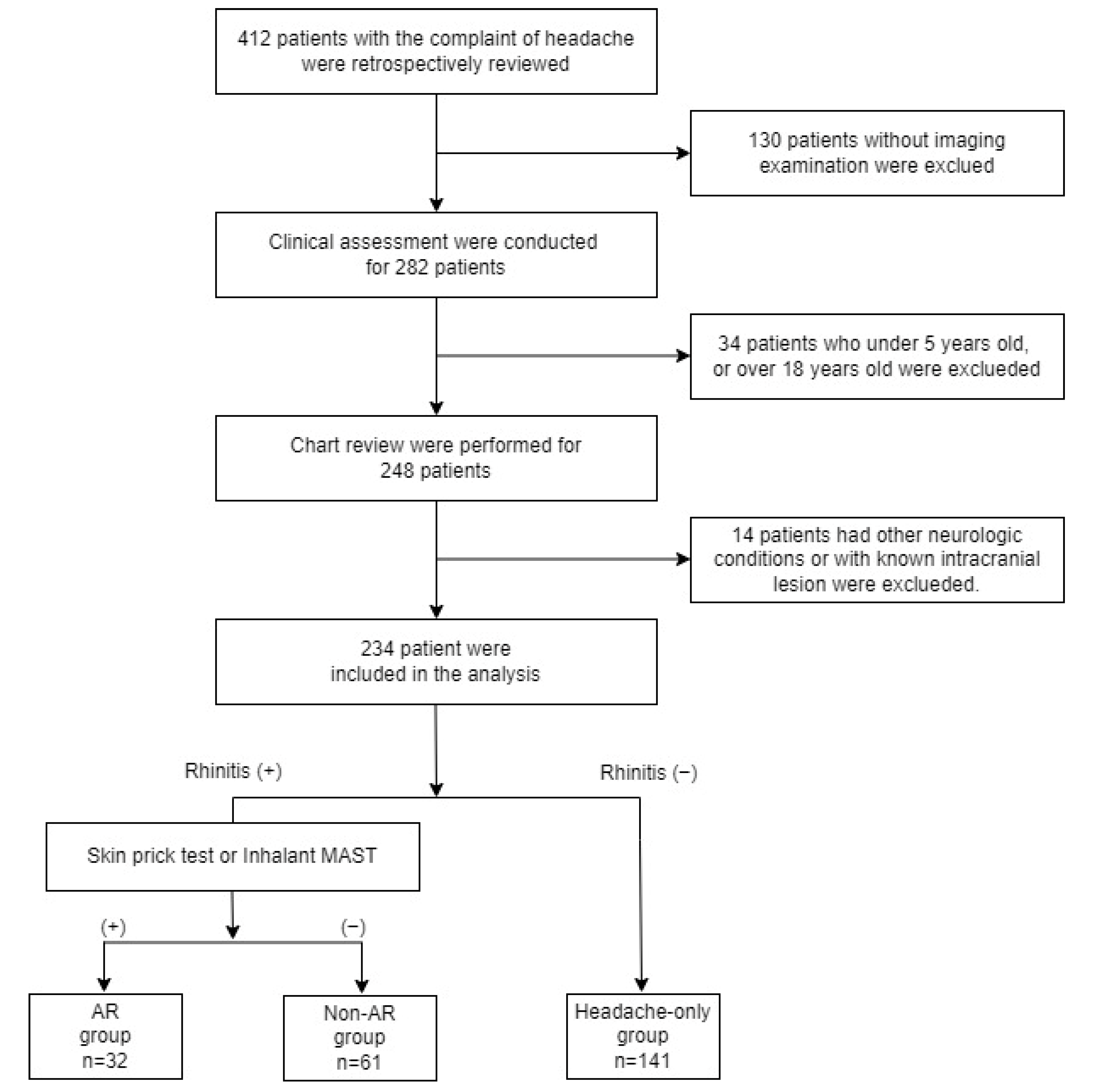
| Variable | AR Group | Non-AR Group | Headache-Only Group | p-Value |
|---|---|---|---|---|
| n = 32 (13.7%) | n = 61 (26.1%) | n = 141 (60.1%) | ||
| Age | 11.38 ± 4.00 | 11.16 ± 3.23 | 11.46 ± 3.56 | 0.861 |
| BMI | 22.19 ± 5.11 | 20.41 ± 3.42 | 20.17 ± 3.76 | 0.03 * |
| Variable | AR Group | Non-AR Group | Headache Group | p-Value |
|---|---|---|---|---|
| n = 32 (13.7%) | n = 61 (26.1%) | n = 141 (60.1%) | ||
| WBC (109/L) | 7.44 ± 2.66 | 8.12 ± 2.75 | 7.66 ± 2.44 | 0.424 |
| Hb (g/dL) | 13.49 ± 1.25 | 13.51 ± 0.87 | 13.55 ± 1.10 | 0.947 |
| PLT (109/L) | 310.35 ± 71.40 | 311.65 ± 83.74 | 304.53 ± 64.25 | 0.798 |
| ALT (IU/L) | 16.37 ± 9.35 | 21.15 ± 19.76 | 19.7 ± 39.88 | 0.812 |
| BUN (mg/dL) | 11.75 ± 2.89 | 11.7 ± 3.28 | 12.17 ± 3.53 | 0.642 |
| Cre (mg/dL) | 0.64 ± 0.21 | 0.56 ± 0.20 | 0.6 ± 0.24 | 0.243 |
| Na (mEq/L) | 140.27 ± 2.36 | 139.72 ± 1.65 | 140.26 ± 1.86 | 0.202 |
| K (mEq/L) | 4.1 ± 0.28 | 4.13 ± 0.28 | 4.18 ± 0.28 | 0.27 |
| AR Group | Non-AR Group | Headache Group | p-Value | ||
|---|---|---|---|---|---|
| (n = 32) | (n = 61) | (n = 141) | |||
| Emergency visit | Yes | 8 (16.3%) | 16 (32.7%) | 25 (51%) | 0.303 |
| No | 24 (13%) | 45 (24.3%) | 116 (62.7%) | ||
| Imaging Findings | Normal | 18 (11.3%) | 35 (21.9%) | 107 (66.9%) | 0.010 * |
| Sinusitis, Mastoditis | 14 (18.9%) | 26 (35.1%) | 34 (45.9%) | ||
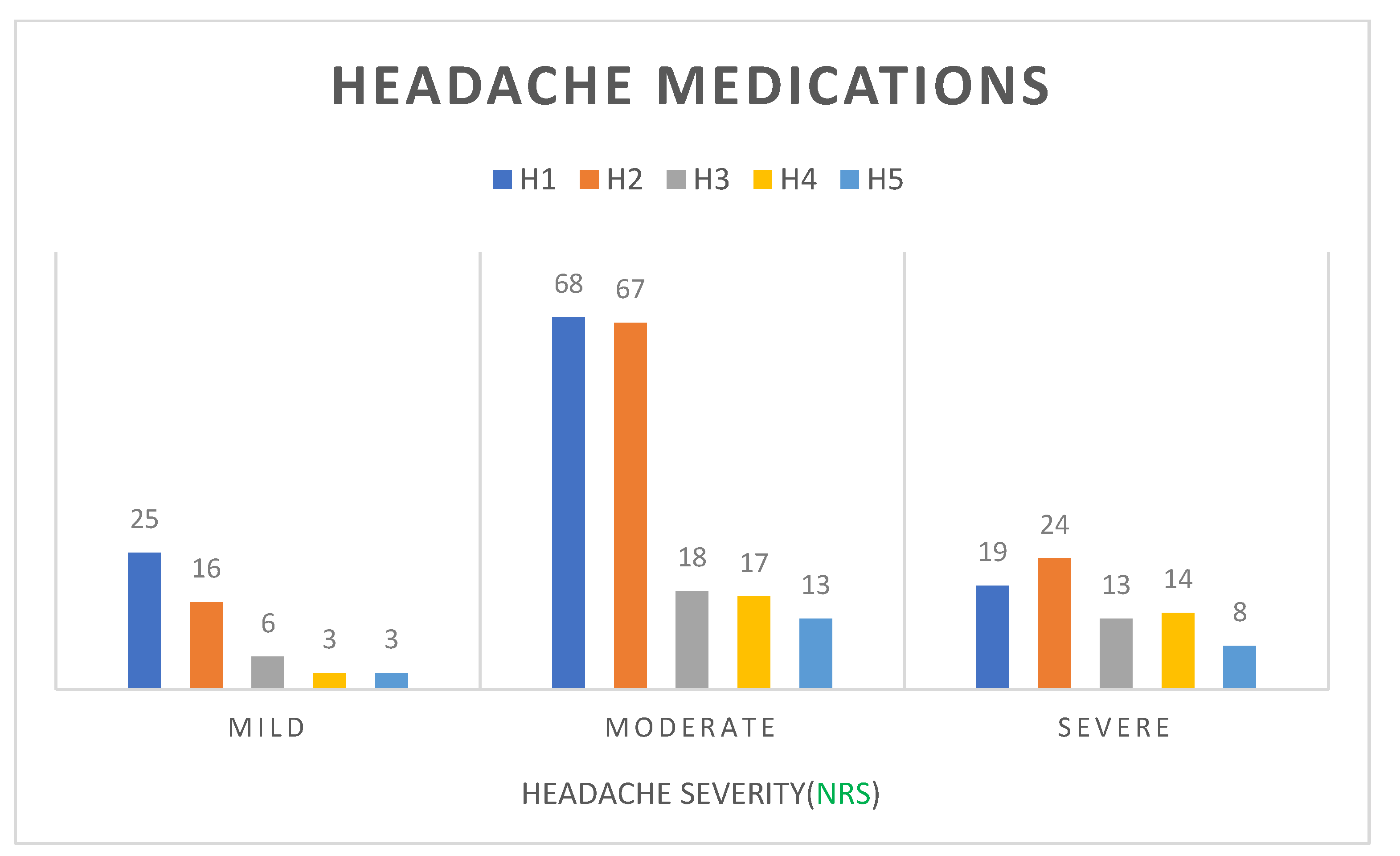
| NRS | Mild | Moderate | Severe | p-Value |
|---|---|---|---|---|
| n = 56 | n = 131 | n = 47 | ||
| BMI | 18.96 ± 3.62 | 21.35 ± 4.05 | 20.01 ± 3.35 | ˂0.001 * |
| Emergency visit | 7 (14.3%) | 32 (65.3%) | 10 (20.4%) | 0.183 |
| Abnormal Imaging Findings | 17 (23%) | 41 (55.4%) | 16 (21.6%) | 0.927 |
| AR Group | 8 (25%) | 21 (65.6%) | 3 (9.4%) | 0.522 |
| Headache Group | 14 (23%) | 32 (52.5%) | 15 (24.6%) | |
| Non-AR Group | 34 (24.1%) | 78 (55.3%) | 29 (20.6%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, S.-J.; Lee, H.; Cui, T.; Lee, J.M.; Ahn, J.Y.; Lee, S.; Kim, S. A Comparison of Clinical Features of Youth with and without Rhinitis Signs and Symptoms Who Are Hospitalized for Headache. Children 2022, 9, 1241. https://doi.org/10.3390/children9081241
Tang S-J, Lee H, Cui T, Lee JM, Ahn JY, Lee S, Kim S. A Comparison of Clinical Features of Youth with and without Rhinitis Signs and Symptoms Who Are Hospitalized for Headache. Children. 2022; 9(8):1241. https://doi.org/10.3390/children9081241
Chicago/Turabian StyleTang, Si-Jia, Heejin Lee, Tiantian Cui, Jae Min Lee, Ji Young Ahn, Sua Lee, and Saeyoon Kim. 2022. "A Comparison of Clinical Features of Youth with and without Rhinitis Signs and Symptoms Who Are Hospitalized for Headache" Children 9, no. 8: 1241. https://doi.org/10.3390/children9081241
APA StyleTang, S.-J., Lee, H., Cui, T., Lee, J. M., Ahn, J. Y., Lee, S., & Kim, S. (2022). A Comparison of Clinical Features of Youth with and without Rhinitis Signs and Symptoms Who Are Hospitalized for Headache. Children, 9(8), 1241. https://doi.org/10.3390/children9081241






