Bioelectrical Impedance Analysis-Derived Phase Angle and Body Composition Are Predictors of Health-Related Fitness in Children and Adolescents with Obesity
Abstract
1. Introduction
2. Materials and Methods
2.1. Anthropometric Measurements
2.2. Bioelectrical Impedance Analysis
2.3. Physical Fitness Assessment
- (1)
- HGS (in kg) was measured using a Dynex dynamometer (MD Systems Inc., Westerville, OH, USA) to assess the isometric strength of both arms. A pretest was done to allow the subject to become familiar with the instrument. Participants were asked to stand upright with their shoulder adducted and neutrally rotated, the elbow fully extended, and the forearm and wrist neutrally positioned. They performed three maximal contractions (each lasting 5 s) with each hand, with a 1 min rest between tests [35]. Maximum HGS was finally defined as the highest value of the six attempts (three for the dominant and three for the nondominant arm).
- (2)
- SBJ (in centimeters) was used to assess lower-body muscle strength [5]. Participants performed a two-foot take-off and landing (swinging of the arms and flexing of the knees allowed). Participants performed two attempts to jump as far as possible while landing on both feet and without falling backwards. Length was measured to the nearest point of contact. The best value was used for statistical analysis.
- (3)
- Five broad jump (FIVEBJ, in centimeters) was used to assess lower-body muscle strength and power. Participants performed a two-foot take-off and landing five times with swinging of the arms and flexing of the knees permitted to provide forward drive. Length was measured to the nearest point of contact of the landing at the end of the five jumps. The best value of two attempts was used for analysis.
- (4)
- Six-minute walking test (in meters) was performed indoors [36] along a corridor (length of 20 m) that was marked every 2 m with a brightly colored tape. Two cones were used to indicate the beginning and the end points of the walking course. Each participant was tested individually and was asked to walk the longest distance possible in 6 min. Only standardized phrases for encouragement (e.g., “keep going” and “you are doing well”) and announcement of time remaining were given.
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ganley, K.J.; Paterno, M.V.; Miles, C.; Stout, J.; Brawner, L.; Girolami, G.; Warren, M. Health-Related Fitness in Children and Adolescents. Pediatr. Phys. Ther. 2011, 23, 208–220. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Artero, E.G.; Ruiz, J.R.; Espana-Romero, V.; Jimenez-Pavon, D.; Vicente-Rodriguez, G.; Moreno, L.A.; Manios, Y.; Beghin, L.; Ottevaere, C.; et al. Physical Fitness Levels among European Adolescents: The HELENA Study. Br. J. Sport. Med. 2011, 45, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.R.; Castro-Pinero, J.; Artero, E.G.; Ortega, F.B.; Sjostrom, M.; Suni, J.; Castillo, M.J. Predictive Validity of Health-Related Fitness in Youth: A Systematic Review. Br. J. Sport. Med. 2009, 43, 909–923. [Google Scholar] [CrossRef] [PubMed]
- Raghuveer, G.; Hartz, J.; Lubans, D.R.; Takken, T.; Wiltz, J.L.; Mietus-Snyder, M.; Perak, A.M.; Baker-Smith, C.; Pietris, N.; Edwards, N.M.; et al. Cardiorespiratory Fitness in Youth: An Important Marker of Health: A Scientific Statement From the American Heart Association. Circulation 2020, 142, e101–e118. [Google Scholar] [CrossRef]
- Marques, A.; Henriques-Neto, D.; Peralta, M.; Martins, J.; Gomes, F.; Popovic, S.; Masanovic, B.; Demetriou, Y.; Schlund, A.; Ihle, A. Field-Based Health-Related Physical Fitness Tests in Children and Adolescents: A Systematic Review. Front. Pediatr. 2021, 9, 640028. [Google Scholar] [CrossRef]
- Ruiz, J.R.; Castro-Pinero, J.; Espana-Romero, V.; Artero, E.G.; Ortega, F.B.; Cuenca, M.M.; Jimenez-Pavon, D.; Chillon, P.; Girela-Rejon, M.J.; Mora, J.; et al. Field-Based Fitness Assessment in Young People: The ALPHA Health-Related Fitness Test Battery for Children and Adolescents. Br. J. Sport. Med. 2011, 45, 518–524. [Google Scholar] [CrossRef]
- Sacco, A.M.; Valerio, G.; Alicante, P.; Di Gregorio, A.; Spera, R.; Ballarin, G.; Scalfi, L. Raw Bioelectrical Impedance Analysis Variables (Phase Angle and Impedance Ratio) Are Significant Predictors of Hand Grip Strength in Adolescents and Young Adults. Nutrition 2021, 91–92, 111445. [Google Scholar] [CrossRef]
- Pezoa-Fuentes, P.; Cossio-Bolaños, M.; Urra-Albornoz, C.; Alvear-Vasquez, F.; Lazari, E.; Urzua-Alul, L.; de Campos, L.F.C.C.; Gomez-Campos, R. Fat-Free Mass and Maturity Status Are Determinants of Physical Fitness Performance in Schoolchildren and Adolescents. J. De Pediatr. 2022, 98, S0021755722000766. [Google Scholar] [CrossRef]
- Hermassi, S. The Associations Between Physical Performance and Anthropometric Characteristics in Obese and Non-Obese Schoolchild Handball Players. Front. Physiol. 2021, 11, 12. [Google Scholar] [CrossRef]
- Hsu, C.-Y.; Lin, R.-H.; Lin, Y.-C.; Chen, J.-Y.; Li, W.-C.; Lee, L.-A.; Liu, K.-H.; Chuang, H.-H. Are Body Composition Parameters Better than Conventional Anthropometric Measures in Predicting Pediatric Hypertension? Int. J. Environ. Res. Public Health 2020, 17, 5771. [Google Scholar] [CrossRef]
- Mendoza-Muñoz, M.; Adsuar, J.C.; Pérez-Gómez, J.; Muñoz-Bermejo, L.; Garcia-Gordillo, M.Á.; Carlos-Vivas, J. Influence of Body Composition on Physical Fitness in Adolescents. Medicina 2020, 56, 328. [Google Scholar] [CrossRef] [PubMed]
- Morinder, G.; Mattsson, E.; Sollander, C.; Marcus, C.; Larsson, U.E. Six-Minute Walk Test in Obese Children and Adolescents: Reproducibility and Validity. Physiother. Res. Int. 2009, 14, 91–104. [Google Scholar] [CrossRef] [PubMed]
- Valerio, G.; Gallarato, V.; D’Amico, O.; Sticco, M.; Tortorelli, P.; Zito, E.; Nugnes, R.; Mozzillo, E.; Franzese, A. Perceived Difficulty with Physical Tasks, Lifestyle, and Physical Performance in Obese Children. BioMed Res. Int. 2014, 2014, 735764. [Google Scholar] [CrossRef] [PubMed]
- Vandoni, M.; Calcaterra, V.; Carnevale Pellino, V.; De Silvestri, A.; Marin, L.; Zuccotti, G.V.; Tranfaglia, V.; Giuriato, M.; Codella, R.; Lovecchio, N. “Fitness and Fatness” in Children and Adolescents: An Italian Cross-Sectional Study. Children 2021, 8, 762. [Google Scholar] [CrossRef] [PubMed]
- Häcker, A.-L.; Bigras, J.-L.; Henderson, M.; Barnett, T.A.; Mathieu, M.-E. Motor Skills of Children and Adolescents With Obesity and Severe Obesity-A CIRCUIT Study. J. Strength Cond. Res. 2020, 34, 3577–3586. [Google Scholar] [CrossRef]
- Petrovics, P.; Sandor, B.; Palfi, A.; Szekeres, Z.; Atlasz, T.; Toth, K.; Szabados, E. Association between Obesity and Overweight and Cardiorespiratory and Muscle Performance in Adolescents. Int. J. Environ. Res. Public Health 2020, 18, 134. [Google Scholar] [CrossRef]
- Tsiros, M.D.; Tian, E.J.; Shultz, S.P.; Olds, T.; Hills, A.P.; Duff, J.; Kumar, S. Obesity, the New Childhood Disability? An Umbrella Review on the Association between Adiposity and Physical Function. Obes. Rev. 2020, 21, e13121. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Ramírez-Campillo, R.; Izquierdo, M. Is Muscular Fitness Associated with Future Health Benefits in Children and Adolescents? A Systematic Review and Meta-Analysis of Longitudinal Studies. Sports Med. 2019, 49, 1079–1094. [Google Scholar] [CrossRef]
- Carson, V.; Tremblay, M.S.; Chaput, J.-P.; Chastin, S.F.M. Associations between Sleep Duration, Sedentary Time, Physical Activity, and Health Indicators among Canadian Children and Youth Using Compositional Analyses. Appl. Physiol. Nutr. Metab. 2016, 41, S294–S302. [Google Scholar] [CrossRef]
- Valerio, G.; Licenziati, M.R.; Tortorelli, P.; Calandriello, L.F.; Alicante, P.; Scalfi, L. Lower Performance in the Six-Minute Walk Test in Obese Youth With Cardiometabolic Risk Clustering. Front. Endocrinol. 2018, 9, 701. [Google Scholar] [CrossRef]
- de Lima, T.R.; Martins, P.C.; Moreno, Y.M.F.; Chaput, J.-P.; Tremblay, M.S.; Sui, X.; Silva, D.A.S. Muscular Fitness and Cardiometabolic Variables in Children and Adolescents: A Systematic Review. Sports Med. 2022, 52, 1555–1575. [Google Scholar] [CrossRef] [PubMed]
- Cossio-Bolaños, M.; Vidal- Espinoza, R.; Albornoz, C.U.; Fuentes-Lopez, J.; Sánchez-Macedo, L.; Andruske, C.L.; Sulla-Torres, J.; Campos, R.G. Relationship between the Body Mass Index and the Ponderal Index with Physical Fitness in Adolescent Students. BMC Pediatr. 2022, 22, 231. [Google Scholar] [CrossRef] [PubMed]
- Palacio-Agüero, A.; Díaz-Torrente, X.; Quintiliano Scarpelli Dourado, D. Relative Handgrip Strength, Nutritional Status and Abdominal Obesity in Chilean Adolescents. PLoS ONE 2020, 15, e0234316. [Google Scholar] [CrossRef] [PubMed]
- Vincenzo, O.D.; Marra, M.; Sacco, A.M.; Pasanisi, F.; Scalfi, L. Bioelectrical Impedance (BIA)-Derived Phase Angle in Adults with Obesity: A Systematic Review. Clin. Nutr. 2021, 40, 5238–5248. [Google Scholar] [CrossRef] [PubMed]
- Ballarin, G.; Scalfi, L.; Monfrecola, F.; Alicante, P.; Bianco, A.; Marra, M.; Sacco, A.M. Body Composition and Bioelectrical-Impedance-Analysis-Derived Raw Variables in Pole Dancers. Int. J. Environ. Res. Public Health 2021, 18, 12638. [Google Scholar] [CrossRef]
- de Moraes, A.M.; Quinaud, R.T.; Ferreira, G.O.C.; Lima, A.B.; Carvalho, H.M.; Guerra-Júnior, G. Age-, Sex-, and Maturity-Associated Variation in the Phase Angle after Adjusting for Size in Adolescents. Front. Nutr. 2022, 9, 939714. [Google Scholar] [CrossRef]
- Kołodziej, M.; Czajka, K. Skeletal Muscle Quality in 6- and 7-y-Old Children Assessed Using Bioelectrical Impedance Analysis. Nutrition 2022, 96, 111568. [Google Scholar] [CrossRef]
- Orsso, C.E.; Gonzalez, M.C.; Maisch, M.J.; Haqq, A.M.; Prado, C.M. Using Bioelectrical Impedance Analysis in Children and Adolescents: Pressing Issues. Eur. J. Clin. Nutr. 2022, 76, 659–665. [Google Scholar] [CrossRef]
- Oliveira, L.D.A.; Hauschild, D.B.; Ventura, J.C.; Moreno, Y.M.F. Factors Associated with Phase Angle in Critically Ill Children. Pediatr. Crit. Care Med. 2018, 19, 16. [Google Scholar] [CrossRef]
- Martins, P.C.; de Lima, L.R.A.; Silva, A.M.; Petroski, E.L.; Moreno, Y.M.F.; Silva, D.A.S. Phase Angle Is Associated with the Physical Fitness of HIV-Infected Children and Adolescents. Scand. J. Med. Sci. Sports 2019, 29, 1006–1012. [Google Scholar] [CrossRef]
- Hetherington-Rauth, M.; Baptista, F.; Sardinha, L.B. BIA-Assessed Cellular Hydration and Muscle Performance in Youth, Adults, and Older Adults. Clin. Nutr. 2020, 39, 2624–2630. [Google Scholar] [CrossRef] [PubMed]
- Martins, P.C.; Hansen, F.; Silva, A.M.; Silva, D.A.S. Fluid Distribution and Cell Integrity Indicators Evaluated by Bioelectrical Impedance in University Athletes: Comparison between Team Sports and Individual Sports. Physiol. Meas. 2019, 40, 015004. [Google Scholar] [CrossRef] [PubMed]
- de Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO Growth Reference for School-Aged Children and Adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Haroun, D.; Taylor, S.J.C.; Viner, R.M.; Hayward, R.S.; Darch, T.S.; Eaton, S.; Cole, T.J.; Wells, J.C.K. Validation of Bioelectrical Impedance Analysis in Adolescents Across Different Ethnic Groups. Obesity 2010, 18, 1252–1259. [Google Scholar] [CrossRef] [PubMed]
- Roberts, H.C.; Denison, H.J.; Martin, H.J.; Patel, H.P.; Syddall, H.; Cooper, C.; Sayer, A.A. A Review of the Measurement of Grip Strength in Clinical and Epidemiological Studies: Towards a Standardised Approach. Age Ageing 2011, 40, 423–429. [Google Scholar] [CrossRef]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS Statement: Guidelines for the Six-Minute Walk Test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [CrossRef]
- Ballarin, G.; Monfrecola, F.; Alicante, P.; Di Gregorio, A.; Marra, M.; Sacco, A.; Scalfi, L. Raw Bioelectrical Impedance Analysis (BIA) Variables and Physical Fitness in Semi-Professional Basketball Players. In Proceedings of the 8th International Conference on Sport Sciences Research and Technology Support, Budapest, Hungary, 5–6 November 2020; pp. 133–138. [Google Scholar]
- Ulrich, S.; Hildenbrand, F.F.; Treder, U.; Fischler, M.; Keusch, S.; Speich, R.; Fasnacht, M. Reference Values for the 6-Minute Walk Test in Healthy Children and Adolescents in Switzerland. BMC Pulm. Med. 2013, 13, 49. [Google Scholar] [CrossRef]
- Vanhelst, J.; Fardy, P.S.; Salleron, J.; Béghin, L. The Six-Minute Walk Test in Obese Youth: Reproducibility, Validity, and Prediction Equation to Assess Aerobic Power. Disabil. Rehabil. 2013, 35, 479–482. [Google Scholar] [CrossRef]
- Tsiros, M.D.; Buckley, J.D.; Olds, T.; Howe, P.R.C.; Hills, A.P.; Walkley, J.; Wood, R.; Kagawa, M.; Shield, A.; Taylor, L.; et al. Impaired Physical Function Associated with Childhood Obesity: How Should We Intervene? Child. Obes. 2016, 12, 126–134. [Google Scholar] [CrossRef]
- Makni, E.; Elloumi, A.; Ben Brahim, M.; Moalla, W.; Tabka, Z.; Chamari, K.; Elloumi, M. Six-Minute Walk Distance Equation in Children and Adolescents with Obesity. Acta Paediatr. 2020, 109, 2729–2737. [Google Scholar] [CrossRef]
| Boys (n = 150) | Girls (n = 131) | p | |
|---|---|---|---|
| Age (yrs) | 11.0 (1.8) | 10.7 (1.9) | 0.197 |
| Weight (kg) | 63.9 (16.5) | 63.4 (17.3) | 0.793 |
| Weight Z-score | 2.83 (0.91) | 2.72 (0.96) | 0.318 |
| Height (cm) | 148.1 (11.2) | 145.9 (10.7) | 0.097 |
| Height Z-score | 0.70 (1.02) | 0.55 (1.02) | 0.243 |
| Body mass index—BMI (kg/m2) | 28.8 (4.0) | 29.2 (4.8) | 0.097 |
| BMI Z-score | 3.3 (0.8) | 3.0 (0.8) | 0.005 |
| Waist circumference—WC (cm) | 97.4 (11.3) | 97.0 (12.1) | 0.777 |
| WC/height—WCH | 0.66 (0.05) | 0.67 (0.07) | 0.344 |
| Fat-free mass—FFM (kg) | 40.4 (9.8) | 38.1 (9.7) | 0.053 |
| FFM index—FFMI (kg/m2) | 18.2 (2.3) | 17.7 (2.5) | 0.145 |
| Percentage of body fat (%) | 36.6 (7.4) | 38.7 (7.5) | 0.015 |
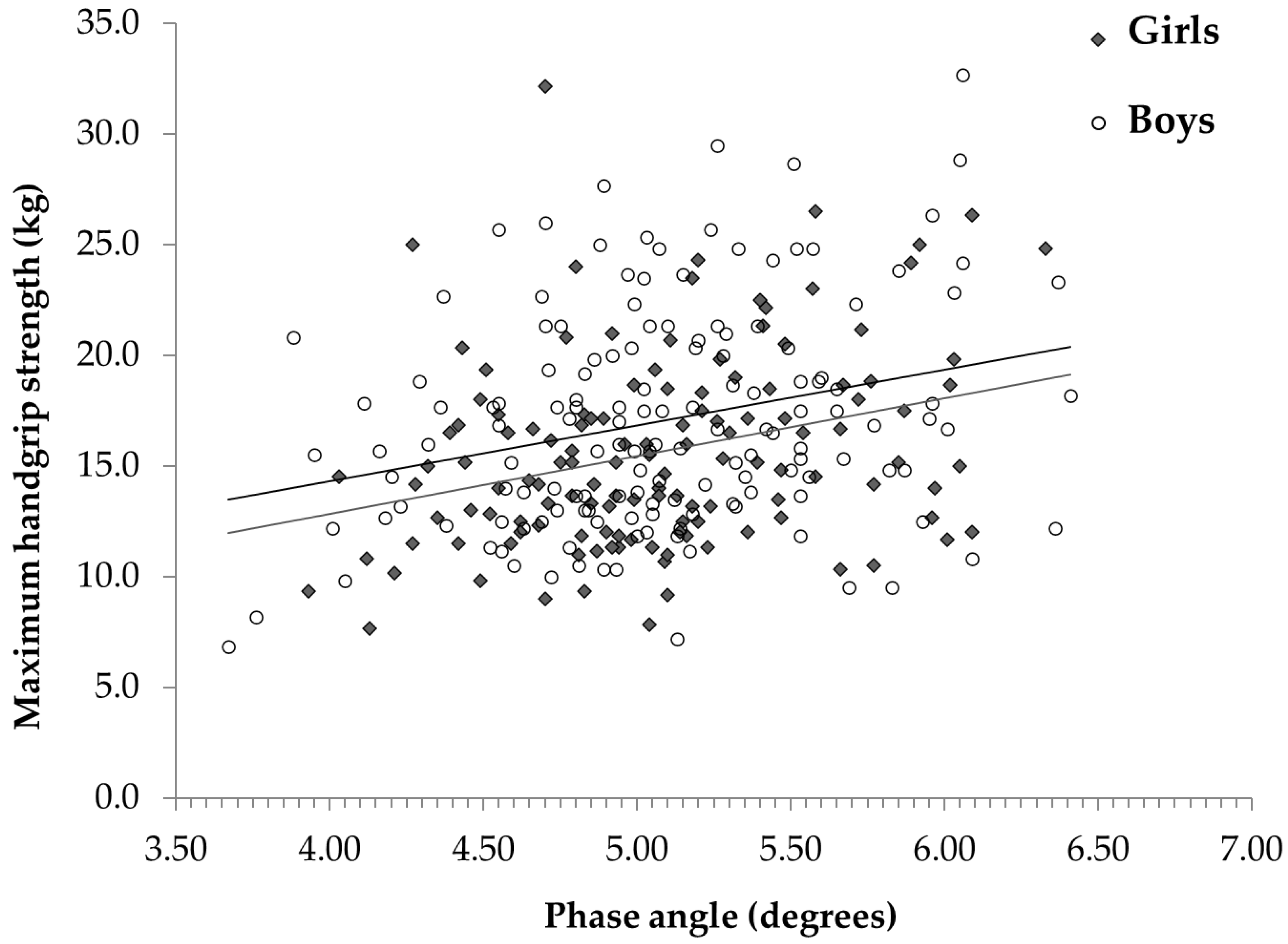
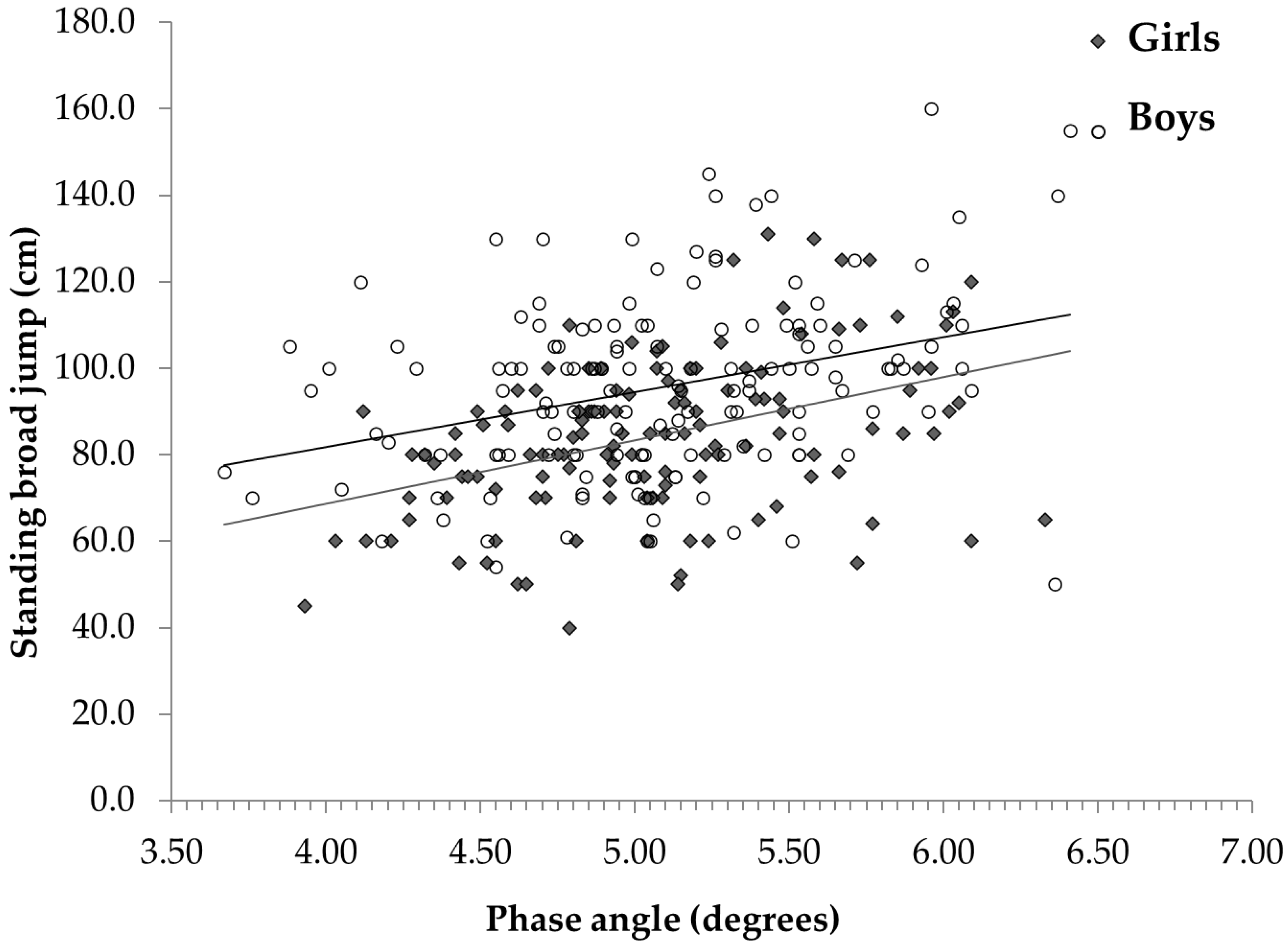
| Phase angle (degrees) | 5.09 (0.55) | 5.08 (0.54) | 0.961 |
| Handgrip strength (kg) | 17.1 (4.9) | 15.8 (4.4) | 0.015 |
| Standing broad jump (cm) | 95.8 (20.6) | 84.0 (19.4) | < 0.001 |
| Five broad jumps (cm) | 473.0 (86.5) | 424.1 (80.0) | < 0.001 |
| Six-minute walking distance (m) | 461 (45) | 457 (45) | 0.501 |
| HRF Tests | Height | Weight | BMI | BMI Z-Score | WHR | FFM | FFMI | %BF | PhA |
|---|---|---|---|---|---|---|---|---|---|
| Handgrip strength | 0.684 * | 0.661 * | 0.453 * | −0.086 | 0.084 | 0.720 * | 0.535 * | −0.036 | 0.285 * |
| Standing broad jump | 0.170 * | −0.020 | −0.194 * | −0.366 * | −0.343 * | 0.143 * | 0.075 | −0.327 * | 0.361 * |
| Five broad jumps | 0.163 * | −0.001 | −0.150 | −0.318 * | −0.293 * | 0.156 * | 0.103 | −0.302 * | 0.355 * |
| Six-minute walking distance | 0.160 * | 0.062 | −0.059 | −0.214 * | −0.155 * | 0.063 | −0.072 | −0.007 | 0.074 |
| Tertiles of Phase Angle | ||||||
|---|---|---|---|---|---|---|
| Boys | Girls | |||||
| 1st | 2nd | 3rd | 1st | 2nd | 3rd | |
| Handgrip test (kg) | 16.1 (4.7) | 17.4 (4.9) | 17.7 (5.3) | 15.1 (4.7) a | 14.8 (3.6) b | 17.1 (4.5) a,b |
| Standing broad jump (cm) | 89.7 (17.6) a | 95.0 (20.6) | 102.2 (22.5) a | 75.9 (14.2) | 85.1 (16.5) a | 91.8 (20.1) a,b |
| Five broad jumps (cm) | 445.5 (74.0) a | 473.0 (85.6) | 501.3 (92.9) a | 391.9 (62.9) | 418.7 (68.2) | 456.4 (91.1) a,b |
| Six-minute walking distance (m) | 464 (43) | 466 (46) | 461 (44) | 454 (39) | 458 (47) | 458 (46) |
| Sex | Age | Weight | Height | WHR | BMI Z-Score | FFM | %BF | PhA | R2 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Handgrip strength | Model 1 | 0.094 * | 0.241 ** | 0.252 ** | 0.116 ** | NS | NS | - | - | - | 0.507 |
| Model 2 | NS | 0.258 ** | NS | NS | NS | NS | 0.504 ** | NS | 0.150 ** | 0.568 | |
| Standing broad jump | Model 1 | 0.234 ** | 0.266 ** | NS | NS | −0.341 ** | NS | - | - | - | 0.242 |
| Model 2 | 0.214 ** | 0.236 ** | NS | NS | −0.242 ** | NS | NS | −0.171 ** | 0.273 ** | 0.349 | |
| Five broad jumps | Model 1 | 0.260 ** | 0.235 ** | NS | NS | −0.290 ** | NS | - | - | - | 0.208 |
| Model 2 | 0.346 ** | NS | NS | NS | NS | −0.364 ** | 0.119 * | NS | 0.336 ** | 0.331 | |
| Six-minute walking distance | Model 1 | NS | NS | NS | 0.149 * | NS | −0.154 * | - | - | - | 0.046 |
| Model 2 | NS | NS | NS | 0.149 * | NS | −0.154 * | NS | NS | NS | 0.046 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ballarin, G.; Licenziati, M.R.; Alicante, P.; Di Vincenzo, O.; Valerio, G.; Scalfi, L. Bioelectrical Impedance Analysis-Derived Phase Angle and Body Composition Are Predictors of Health-Related Fitness in Children and Adolescents with Obesity. Children 2022, 9, 1943. https://doi.org/10.3390/children9121943
Ballarin G, Licenziati MR, Alicante P, Di Vincenzo O, Valerio G, Scalfi L. Bioelectrical Impedance Analysis-Derived Phase Angle and Body Composition Are Predictors of Health-Related Fitness in Children and Adolescents with Obesity. Children. 2022; 9(12):1943. https://doi.org/10.3390/children9121943
Chicago/Turabian StyleBallarin, Giada, Maria Rosaria Licenziati, Paola Alicante, Olivia Di Vincenzo, Giuliana Valerio, and Luca Scalfi. 2022. "Bioelectrical Impedance Analysis-Derived Phase Angle and Body Composition Are Predictors of Health-Related Fitness in Children and Adolescents with Obesity" Children 9, no. 12: 1943. https://doi.org/10.3390/children9121943
APA StyleBallarin, G., Licenziati, M. R., Alicante, P., Di Vincenzo, O., Valerio, G., & Scalfi, L. (2022). Bioelectrical Impedance Analysis-Derived Phase Angle and Body Composition Are Predictors of Health-Related Fitness in Children and Adolescents with Obesity. Children, 9(12), 1943. https://doi.org/10.3390/children9121943









