Brain-Directed Care: Why Neuroscience Principles Direct PICU Management beyond the ABCs
Abstract
1. Introduction
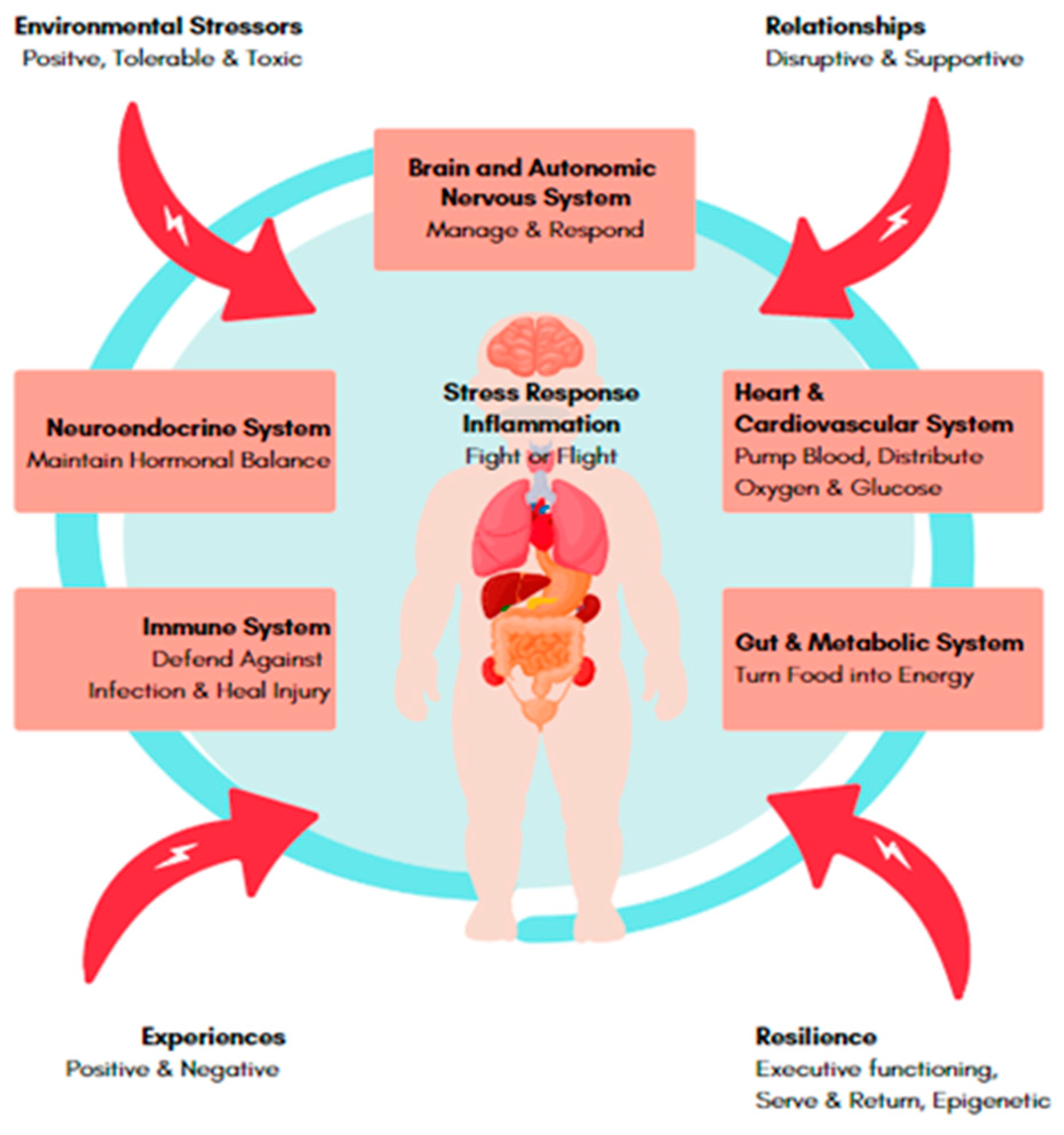
2. Neuroscience: Building Health Brains
2.1. Brains Are Built, Not Born
2.2. Experiences Shape Our Brains
2.3. The Importance of Human Relationships
2.4. Resilience Is Fundamental for Fostering and Advancing Neurodevelopment
3. Impact of Hospitalization and Critical Illness on Child Health
3.1. Hospitalization in Childhood
3.2. Chronic Illness
3.3. Critical Illness
4. Approaches to Reducing the Burden of Adverse Childhood Hospitalization and Illness Experiences
4.1. Trauma-Informed Care
4.2. PICU Liberation
4.3. Parental Education and Psychosocial Support
4.4. Early Screening and Intervention
5. Embracing Neuroscience in the PICU
- Develop and invest in care and services that give young children the best start in life. This might include mandatory TIC training for all staff and carers.
- Make family-friendly early childhood development policies a PICU priority. This might include open visitation, parental presence during procedures and rounds, and neurodevelopmental cares.
- Collect data on essential indicators of early childhood development and track progress. This might include social determinants, adverse childhood events, pre-morbid child development, pre-PICU parent functioning, and post-PICU outcomes.
- Provide leadership for early childhood development programs. This might include Brain Story Certification, and the embedding of core brain story concepts into curriculum.
- Continue to advocate for early childhood development services that families can access. This might include parenting programs, care coordination, post-PICU child and family psychosocial interventions, and PICU follow-up services.
6. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Tierney, A.L.; Nelson, C.A., III. Brain development and the role of experience in the early years. Zero Three 2009, 30, 9. [Google Scholar] [PubMed]
- Thompson, R.A. Stress and child development. Future Child. 2014, 24, 41–59. [Google Scholar] [CrossRef] [PubMed]
- Johnston, M.V. Plasticity in the developing brain: Implications for rehabilitation. Dev. Disabil. Res. Rev. 2009, 15, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Fox, S.E.; Levitt, P.; Nelson, C.A., III. How the timing and quality of early experiences influence the development of brain architecture. Child Dev. 2010, 81, 28–40. [Google Scholar] [CrossRef]
- Hensch, T.K.; Bilimoria, P.M. Re-opening windows: Manipulating critical periods for brain development. In Cerebrum: The Dana Forum on Brain Science; Dana Foundation: New York, NY, USA, 2012. [Google Scholar]
- Nelson, C.A., III; Gabard-Durnam, L.J. Early adversity and critical periods: Neurodevelopmental consequences of violating the expectable environment. Trends Neurosci. 2020, 43, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Jensen, S.K.; Bouhouch, R.R.; Walson, J.L.; Daelmans, B.; Bahl, R.; Darmstadt, G.L.; Dua, T. Enhancing the child survival agenda to promote, protect, and support early child development. In Seminars in Perinatology; Elsevier: Amsterdam, The Netherlands, 2015; pp. 373–386. [Google Scholar]
- Branchi, I.; Cirulli, F. Early experiences: Building up the tools to face the challenges of adult life. Dev. Psychobiol. 2014, 56, 1661–1674. [Google Scholar] [CrossRef] [PubMed]
- Brito, N.H.; Noble, K.G. Socioeconomic status and structural brain development. Front. Neurosci. 2014, 8, 276. [Google Scholar] [CrossRef]
- Knudsen, E.I. Sensitive periods in the development of the brain and behavior. J. Cogn. Neurosci. 2004, 16, 1412–1425. [Google Scholar] [CrossRef]
- Newport, E.L.; Bavelier, D.; Neville, H.J. Critical thinking about critical periods: Perspectives on a critical period for language acquisition. In Language, Brain and Cognitive Development: Essays in Honor of Jacques Mehler; MIT Press: Cambridge, MA, USA, 2001; pp. 481–502. [Google Scholar]
- Gunnar, M.; Quevedo, K. The neurobiology of stress and development. Annu. Rev. Psychol. 2007, 58, 145–173. [Google Scholar] [CrossRef] [PubMed]
- Felitti, V.; Anda, R.; Nordenberg, D.; Williamson, D. Adverse childhood experiences and health outcomes in adults: The Ace study. J. Fam. Consum. Sci. 1998, 90, 31. [Google Scholar]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Kong, J.; Liu, Y.; Goldberg, J.; Almeida, D.M. Adverse childhood experiences amplify the longitudinal associations of adult daily stress and health. Child Abus. Negl. 2021, 122, 105337. [Google Scholar] [CrossRef] [PubMed]
- Leiva, L.; Torres-Cortés, B.; Antivilo-Bruna, A. Adverse Childhood Experiences and Mental Health: When Well-Being Matters. Child Indic. Res. 2022, 15, 631–655. [Google Scholar] [CrossRef]
- Crandall, A.; Miller, J.R.; Cheung, A.; Novilla, L.K.; Glade, R.; Novilla, M.L.B.; Magnusson, B.M.; Leavitt, B.L.; Barnes, M.D.; Hanson, C.L. ACEs and counter-ACEs: How positive and negative childhood experiences influence adult health. Child Abus. Negl. 2019, 96, 104089. [Google Scholar] [CrossRef]
- Kosterman, R.; Mason, W.A.; Haggerty, K.P.; Hawkins, J.D.; Spoth, R.; Redmond, C. Positive childhood experiences and positive adult functioning: Prosocial continuity and the role of adolescent substance use. J. Adolesc. Health 2011, 49, 180–186. [Google Scholar] [CrossRef]
- Narayan, A.J.; Rivera, L.M.; Bernstein, R.E.; Harris, W.W.; Lieberman, A.F. Positive childhood experiences predict less psychopathology and stress in pregnant women with childhood adversity: A pilot study of the benevolent childhood experiences (BCEs) scale. Child Abus. Negl. 2018, 78, 19–30. [Google Scholar] [CrossRef]
- Poole, J.C.; Dobson, K.S.; Pusch, D. Childhood adversity and adult depression: The protective role of psychological resilience. Child Abus. Negl. 2017, 64, 89–100. [Google Scholar] [CrossRef]
- Sege, R.D.; Browne, C.H. Responding to ACEs with HOPE: Health outcomes from positive experiences. Acad. Pediatr. 2017, 17, S79–S85. [Google Scholar] [CrossRef]
- Skodol, A.E.; Bender, D.S.; Pagano, M.E.; Shea, M.T.; Yen, S.; Sanislow, C.A.; Grilo, C.M.; Daversa, M.T.; Stout, R.L.; Zanarini, M.C. Positive childhood experiences: Resilience and recovery from personality disorder in early adulthood. J. Clin. Psychiatry 2007, 68, 14724. [Google Scholar] [CrossRef]
- Slopen, N.; Chen, Y.; Guida, J.L.; Albert, M.A.; Williams, D.R. Positive childhood experiences and ideal cardiovascular health in midlife: Associations and mediators. Prev. Med. 2017, 97, 72–79. [Google Scholar] [CrossRef]
- Hanson, J.L.; Nacewicz, B.M.; Sutterer, M.J.; Cayo, A.A.; Schaefer, S.M.; Rudolph, K.D.; Shirtcliff, E.A.; Pollak, S.D.; Davidson, R.J. Behavioral problems after early life stress: Contributions of the hippocampus and amygdala. Biol. Psychiatry 2015, 77, 314–323. [Google Scholar] [CrossRef] [PubMed]
- Baker, L.M.; Williams, L.M.; Korgaonkar, M.S.; Cohen, R.A.; Heaps, J.M.; Paul, R.H. Impact of early vs. late childhood early life stress on brain morphometrics. Brain Imaging Behav. 2013, 7, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Salminen, L.E.; Morey, R.A.; Riedel, B.C.; Jahanshad, N.; Dennis, E.L.; Thompson, P.M. Adaptive identification of cortical and subcortical imaging markers of early life stress and posttraumatic stress disorder. J. Neuroimaging 2019, 29, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Molet, J.; Maras, P.M.; Avishai-Eliner, S.; Baram, T.Z. Naturalistic rodent models of chronic early-life stress. Dev. Psychobiol. 2014, 56, 1675–1688. [Google Scholar] [CrossRef]
- Clark, C.; Crombie, R.; Head, J.; Van Kamp, I.; Van Kempen, E.; Stansfeld, S.A. Does traffic-related air pollution explain associations of aircraft and road traffic noise exposure on children’s health and cognition? A secondary analysis of the United Kingdom sample from the RANCH project. Am. J. Epidemiol. 2012, 176, 327–337. [Google Scholar] [CrossRef]
- Clark, C.; Martin, R.; Van Kempen, E.; Alfred, T.; Head, J.; Davies, H.W.; Haines, M.M.; Barrio, I.L.; Matheson, M.; Stansfeld, S.A. Exposure-effect relations between aircraft and road traffic noise exposure at school and reading comprehension: The RANCH project. Am. J. Epidemiol. 2006, 163, 27–37. [Google Scholar] [CrossRef]
- Gupta, A.; Gupta, A.; Jain, K.; Gupta, S. Noise pollution and impact on children health. Indian J. Pediatr. 2018, 85, 300–306. [Google Scholar] [CrossRef]
- Stansfeld, S.A.; Berglund, B.; Clark, C.; Lopez-Barrio, I.; Fischer, P.; Öhrström, E.; Haines, M.M.; Head, J.; Hygge, S.; Van Kamp, I. Aircraft and road traffic noise and children’s cognition and health: A cross-national study. Lancet 2005, 365, 1942–1949. [Google Scholar] [CrossRef]
- Ravi, M.; Miller, A.H.; Michopoulos, V. The immunology of stress and the impact of inflammation on the brain and behaviour. BJPsych Adv. 2021, 27, 158–165. [Google Scholar] [CrossRef]
- Agorastos, A.; Pervanidou, P.; Chrousos, G.P.; Baker, D.G. Developmental trajectories of early life stress and trauma: A narrative review on neurobiological aspects beyond stress system dysregulation. Front. Psychiatry 2019, 118. [Google Scholar] [CrossRef]
- Black, M.M.; Behrman, J.R.; Daelmans, B.; Prado, E.L.; Richter, L.; Tomlinson, M.; Trude, A.C.; Wertlieb, D.; Wuermli, A.J.; Yoshikawa, H. The principles of Nurturing Care promote human capital and mitigate adversities from preconception through adolescence. BMJ Glob. Health 2021, 6, e004436. [Google Scholar] [CrossRef] [PubMed]
- Britto, P.R.; Singh, M.; Dua, T.; Kaur, R.; Yousafzai, A.K. What implementation evidence matters: Scaling-up nurturing interventions that promote early childhood development. Ann. N. Y. Acad. Sci. 2018, 1419, 5–16. [Google Scholar] [CrossRef] [PubMed]
- Shonkoff, J.P. Breakthrough impacts: What science tells us about supporting early childhood development. YC Young Children 2017, 72, 8–16. [Google Scholar]
- Shonkoff, J.P.; Richmond, J.B. Investment in Early Childhood Development Lays the Foundation for a Prosperous and Sustainable Society; Encyclopedia on Early Childhood Development. Available online: https://www.child-encyclopedia.com/importance-early-childhood-development/according-experts/investment-early-childhood-development-lays (accessed on 5 December 2022).
- Dosani, A.; Creighton, D.; Lodha, A.K. Late Preterm Infants and Neurodevelopmental Outcomes: Why Do I Need to Serve and Return? In Late Preterm Infants; Springer: Cham, Switzerland, 2019; pp. 115–134. [Google Scholar]
- Goodman, J.H. Perinatal depression and infant mental health. Arch. Psychiatr. Nurs. 2019, 33, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Feldman, R. What is resilience: An affiliative neuroscience approach. World Psychiatry 2020, 19, 132–150. [Google Scholar] [CrossRef]
- de Silva, A.; Neel, M.L.; Maitre, N.; Busch, T.; Taylor, H.G. Resilience and vulnerability in very preterm 4-year-olds. Clin. Neuropsychol. 2021, 35, 904–924. [Google Scholar] [CrossRef]
- Holz, N.E.; Tost, H.; Meyer-Lindenberg, A. Resilience and the brain: A key role for regulatory circuits linked to social stress and support. Mol. Psychiatry 2020, 25, 379–396. [Google Scholar] [CrossRef]
- Howell, K.H.; Miller-Graff, L.E.; Martinez-Torteya, C.; Napier, T.R.; Carney, J.R. Charting a course towards resilience following adverse childhood experiences: Addressing intergenerational trauma via strengths-based intervention. Children 2021, 8, 844. [Google Scholar] [CrossRef]
- Hughes, C.; Devine, R.T. For better or for worse? Positive and negative parental influences on young children’s executive function. Child Dev. 2019, 90, 593–609. [Google Scholar] [CrossRef]
- Priel, A.; Zeev-Wolf, M.; Djalovski, A.; Feldman, R. Maternal depression impairs child emotion understanding and executive functions: The role of dysregulated maternal care across the first decade of life. Emotion 2020, 20, 1042. [Google Scholar] [CrossRef]
- Masten, A.S.; Barnes, A.J. Resilience in children: Developmental perspectives. Children 2018, 5, 98. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, X.; Zhang, L.; Guo, C. Executive function and resilience as mediators of adolescents’ perceived stressful life events and school adjustment. Front. Psychol. 2019, 10, 446. [Google Scholar] [CrossRef] [PubMed]
- Niinomi, K.; Fukui, M. Children’s psychosocial and behavioural consequences during their siblings’ hospitalisation: A qualitative content analysis from caregivers’ perspectives. J. Clin. Nurs. 2022, 31, 2219–2226. [Google Scholar] [CrossRef] [PubMed]
- Eiser, C. The psychological impact of chronic illness on children’s development. In The Education of Children with Medical Conditions; Routledge: London, UK, 2013; pp. 27–37. [Google Scholar]
- Shea, T.; Athanasakos, E.; Cleeve, S.; Croft, N.; Gibbs, D. Pediatric medical traumatic stress: A scoping review. J. Child Life: Psychosoc. Theory Pract. 2021, 2, 42–54. [Google Scholar]
- Rzucidlo, S.E.; Campbell, M. Beyond the physical injuries: Child and parent coping with medical traumatic stress after pediatric trauma. J. Trauma Nurs. JTN 2009, 16, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Brosbe, M.S.; Faust, J.; Gold, S.N. Complex traumatic stress in the pediatric medical setting. J. Trauma Dissociation 2013, 14, 97–112. [Google Scholar] [CrossRef]
- Long, D.; Gibbons, K.; Le Brocque, R.; Schults, J.A.; Kenardy, J.; Dow, B. Midazolam exposure in the paediatric intensive care unit predicts acute post-traumatic stress symptoms in children. Aust. Crit. Care 2022, 35, 408–414. [Google Scholar] [CrossRef]
- Rennick, J.E.; Morin, I.; Kim, D.; Johnston, C.C.; Dougherty, G.; Platt, R. Identifying children at high risk for psychological sequelae after pediatric intensive care unit hospitalization. Pediatr. Crit. Care Med. 2004, 5, 358–363. [Google Scholar] [CrossRef]
- Sheridan, R.L.; Stoddard, F.J.; Kazis, L.E.; Lee, A.; Li, N.-C.; Kagan, R.J.; Palmieri, T.L.; Meyer, W.J., III; Nicolai, M.; Stubbs, T.K. Long-term posttraumatic stress symptoms vary inversely with early opiate dosing in children recovering from serious burns: Effects durable at 4 years. J. Trauma Acute Care Surg. 2014, 76, 828–832. [Google Scholar] [CrossRef]
- Vinall, J.; Miller, S.P.; Bjornson, B.H.; Fitzpatrick, K.P.; Poskitt, K.J.; Brant, R.; Synnes, A.R.; Cepeda, I.L.; Grunau, R.E. Invasive procedures in preterm children: Brain and cognitive development at school age. Pediatrics 2014, 133, 412–421. [Google Scholar] [CrossRef]
- Pineda, R.G.; Neil, J.; Dierker, D.; Smyser, C.D.; Wallendorf, M.; Kidokoro, H.; Reynolds, L.C.; Walker, S.; Rogers, C.; Mathur, A.M. Alterations in brain structure and neurodevelopmental outcome in preterm infants hospitalized in different neonatal intensive care unit environments. J. Pediatr. 2014, 164, 52–60.e52. [Google Scholar] [CrossRef] [PubMed]
- Douglas, W. Early hospital admissions and later disturbances of behaviour and learning. Dev. Med. Child Neurol. 1975, 17, 456–480. [Google Scholar] [CrossRef] [PubMed]
- Quinton, D.; Rutter, M. Early hospital admissions and later disturbances of behaviour: An attempted replication of Douglas’ findings. Dev. Med. Child Neurol. 1976, 18, 447–459. [Google Scholar] [CrossRef] [PubMed]
- Mrazek, D.A. Effects of hospitalization on early child development. In Continuities and Discontinuities in Development; Emde, R.N., Harmon, R.J., Eds.; Plenum Press: New York, NY, USA, 1984; pp. 211–225. [Google Scholar]
- Schaffer, H.; Callender, W. Psychologic effects of hospitalization in infancy. Pediatrics 1959, 24, 528–539. [Google Scholar] [CrossRef] [PubMed]
- Clemens, J. Fostering Resilience in Hospitalized Children. Pediatr. Nurs. 2020, 46, 204–206. [Google Scholar]
- Silva, V.L.S.D.; França, G.V.A.D.; Munhoz, T.N.; Santos, I.S.; Barros, A.J.; Barros, F.C.; Matijasevich, A. Hospitalization in the First Years of Life and Development of Psychiatric Disorders at Age 6 and 11: A Birth Cohort Study in Brazil; Cadernos de Saúde Pública: Rio de Janeiro, RJ, Brazil, 2018; Volume 34. [Google Scholar] [CrossRef]
- Perrin, E.C.; Gerrity, P.S. Development of children with a chronic illness. Pediatr. Clin. N. Am. 1984, 31, 19–31. [Google Scholar] [CrossRef]
- Turkel, S.; Pao, M. Late consequences of chronic pediatric illness. Psychiatr. Clin. N. Am. 2007, 30, 819–835. [Google Scholar] [CrossRef]
- Bell, M.F.; Bayliss, D.M.; Glauert, R.; Harrison, A.; Ohan, J.L. Chronic illness and developmental vulnerability at school entry. Pediatrics 2016, 137, e20152475. [Google Scholar] [CrossRef]
- Goldfeld, S.; O’Connor, M.; Sayers, M.; Moore, T.; Oberklaid, F. Prevalence and correlates of special health care needs in a population cohort of Australian children at school entry. J. Dev. Behav. Pediatr. 2012, 33, 319–327. [Google Scholar] [CrossRef]
- Forrest, C.B.; Bevans, K.B.; Riley, A.W.; Crespo, R.; Louis, T.A. School outcomes of children with special health care needs. Pediatrics 2011, 128, 303–312. [Google Scholar] [CrossRef]
- Manning, J.C.; Pinto, N.P.; Rennick, J.E.; Colville, G.; Curley, M.A. Conceptualizing post intensive care syndrome in children—The PICS-p framework. Pediatr. Crit. Care Med. 2018, 19, 298–300. [Google Scholar] [CrossRef] [PubMed]
- Als, L.C.; Tennant, A.; Nadel, S.; Cooper, M.; Pierce, C.M.; Garralda, M.E. Persistence of neuropsychological deficits following pediatric critical illness. Crit. Care Med. 2015, 43, e312–e315. [Google Scholar] [CrossRef] [PubMed]
- Colville, G. The psychologic impact on children of admission to intensive care. Pediatr. Clin. N. Am. 2008, 55, 605–616. [Google Scholar] [CrossRef] [PubMed]
- Colville, G.A.; Pierce, C.M. Children’s self-reported quality of life after intensive care treatment. Pediatr. Crit. Care Med. 2013, 14, e85–e92. [Google Scholar] [CrossRef]
- Davydow, D.S.; Richardson, L.P.; Zatzick, D.F.; Katon, W.J. Psychiatric morbidity in pediatric critical illness survivors: A comprehensive review of the literature. Arch. Pediatr. Adolesc. Med. 2010, 164, 377–385. [Google Scholar] [CrossRef]
- Knoester, H.; Bronner, M.B.; Bos, A.P. Surviving pediatric intensive care: Physical outcome after 3 months. Intensive Care Med. 2008, 34, 1076–1082. [Google Scholar] [CrossRef]
- Namachivayam, P.; Taylor, A.; Montague, T.; Moran, K.; Barrie, J.; Delzoppo, C.; Butt, W. Long-stay children in intensive care: Long-term functional outcome and quality of life from a 20-yr institutional study. Pediatr. Crit. Care Med. 2012, 13, 520–528. [Google Scholar] [CrossRef]
- Nelson, L.P.; Gold, J.I. Posttraumatic stress disorder in children and their parents following admission to the pediatric intensive care unit: A review. Pediatr. Crit. Care Med. 2012, 13, 338–347. [Google Scholar] [CrossRef]
- Procter, C.; Morrow, B.; Pienaar, G.; Shelton, M.; Argent, A. Outcomes following admission to paediatric intensive care: A systematic review. J. Paediatr. Child Health 2021, 57, 328–358. [Google Scholar] [CrossRef]
- Rennick, J.E.; Rashotte, J. Psychological outcomes in children following pediatric intensive care unit hospitalization: A systematic review of the research. J. Child Health Care 2009, 13, 128–149. [Google Scholar] [CrossRef]
- Woolf, C.; Muscara, F.; Anderson, V.A.; McCarthy, M.C. Early traumatic stress responses in parents following a serious illness in their child: A systematic review. J. Clin. Psychol. Med. Settings 2016, 23, 53–66. [Google Scholar] [CrossRef] [PubMed]
- Ko, M.S.M.; Poh, P.-F.; Heng, K.Y.C.; Sultana, R.; Murphy, B.; Ng, R.W.L.; Lee, J.H. Assessment of long-term psychological outcomes after pediatric intensive care unit admission: A systematic review and meta-analysis. JAMA Pediatr. 2022, 176, e215767. [Google Scholar] [CrossRef] [PubMed]
- Geneslaw, A.S.; Lu, Y.; Miles, C.H.; Hua, M.; Cappell, J.; Smerling, A.J.; Olfson, M.; Edwards, J.D.; Ing, C. Long-term increases in mental disorder diagnoses after invasive mechanical ventilation for severe childhood respiratory disease: A propensity matched observational cohort study. Pediatr. Crit. Care Med. 2021, 22, 1013–1025. [Google Scholar] [CrossRef] [PubMed]
- Tomaszewski, W.; Ablaza, C.; Straney, L.; Taylor, C.; Millar, J.; Schlapbach, L.J. Educational Outcomes of Childhood Survivors of Critical Illness—A Population-Based Linkage Study. Crit. Care Med. 2022, 50, 901–912. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.C.; Gutovich, J.; Smyser, C.; Pineda, R.; Newnham, C.; Tjoeng, T.H.; Vavasseur, C.; Wallendorf, M.; Neil, J.; Inder, T. Neonatal intensive care unit stress is associated with brain development in preterm infants. Ann. Neurol. 2011, 70, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Nist, M.D.; Harrison, T.M.; Steward, D.K. The biological embedding of neonatal stress exposure: A conceptual model describing the mechanisms of stress-induced neurodevelopmental impairment in preterm infants. Res. Nurs. Health 2019, 42, 61–71. [Google Scholar] [CrossRef]
- Dow, B.L.; Kenardy, J.A.; Le Brocque, R.M.; Long, D.A. The utility of the Children’s Revised Impact of Event Scale in screening for concurrent PTSD following admission to intensive care. J. Trauma. Stress 2012, 25, 602–605. [Google Scholar] [CrossRef]
- Duffee, J.; Szilagyi, M.; Forkey, H.; Kelly, E.T. Trauma-informed care in child health systems. Pediatrics 2021, 148, e2021052579. [Google Scholar] [CrossRef]
- Sanders, M.; Hall, S. Trauma-informed care in the newborn intensive care unit: Promoting safety, security and connectedness. J. Perinatol. 2018, 38, 3–10. [Google Scholar] [CrossRef]
- Cutuli, J.; Alderfer, M.A.; Marsac, M.L. Introduction to the special issue: Trauma-informed care for children and families. Psychol. Serv. 2019, 16, 1. [Google Scholar] [CrossRef]
- Marsac, M.L.; Kassam-Adams, N.; Hildenbrand, A.K.; Nicholls, E.; Winston, F.K.; Leff, S.S.; Fein, J. Implementing a trauma-informed approach in pediatric health care networks. JAMA Pediatr. 2016, 170, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Salley, C.; Axelrad, M.; Fischer, E.; Steuer, K. But parents need help! Pathways to caregiver mental health care in pediatric hospital settings. Palliat. Support. Care, 2022; in press. [Google Scholar] [CrossRef] [PubMed]
- Garner, A.; Yogman, M.; Child, C.O.P.A.O.; Health, F. Preventing childhood toxic stress: Partnering with families and communities to promote relational health. Pediatrics 2021, 148, e2021052582. [Google Scholar] [CrossRef] [PubMed]
- Frosch, C.A.; Schoppe-Sullivan, S.J.; O’Banion, D.D. Parenting and child development: A relational health perspective. Am. J. Lifestyle Med. 2021, 15, 45–59. [Google Scholar] [CrossRef] [PubMed]
- Darling Rasmussen, P.; Storebø, O.J.; Løkkeholt, T.; Voss, L.G.; Shmueli-Goetz, Y.; Bojesen, A.B.; Simonsen, E.; Bilenberg, N. Attachment as a core feature of resilience: A systematic review and meta-analysis. Psychol. Rep. 2019, 122, 1259–1296. [Google Scholar] [CrossRef] [PubMed]
- Unick, G.J.; Bassuk, E.L.; Richard, M.K.; Paquette, K. Organizational trauma-informed care: Associations with individual and agency factors. Psychol. Serv. 2019, 16, 134. [Google Scholar] [CrossRef]
- Fleishman, J.; Kamsky, H.; Sundborg, S. Trauma-informed nursing practice. OJIN Online J. Issues Nurs. 2019, 24. [Google Scholar] [CrossRef]
- Isokääntä, S.; Koivula, K.; Honkalampi, K.; Kokki, H. Resilience in children and their parents enduring pediatric medical traumatic stress. Pediatr. Anesth. 2019, 29, 218–225. [Google Scholar] [CrossRef]
- Trauma-Informed Care Training Center. Available online: www.traumainformedcaretraining.com (accessed on 3 October 2022).
- Mental Health Coordinating Council. Trauma-Informed Care and Practice Organisational Toolkit (TICPOT). Available online: https://www.health.nsw.gov.au/mentalhealth/psychosocial/principles/Pages/trauma-informed.aspx (accessed on 3 October 2022).
- The Children’s Hospital of Philadelphia. After the Injury: Information for Healthcare Professionals. Available online: https://www.aftertheinjury.org/for-professionals (accessed on 3 October 2022).
- Purewal, S.K.; Bucci, M.; Gutiérrez Wang, L.; Koita, K.; Silvério Marques, S.; Oh, D.; Burke Harris, N. Screening for adverse childhood experiences (ACEs) in an integrated pediatric care model. Zero Three 2016, 37, 10–17. [Google Scholar]
- Rodenbough, A.; Opolka, C.; Wang, T.; Gillespie, S.; Ververis, M.; Fitzpatrick, A.M.; Grunwell, J.R. Adverse Childhood Experiences and Patient-Reported Outcome Measures in Critically Ill Children. Front. Pediatr. 2022, 10, 923118. [Google Scholar] [CrossRef]
- Cheung, C.; La Count, S.; Jarvis, J.; McClusky, C.; O’Leary, D.; Gunn, S.; Hall, A.; Schneck, J.; Fink, E. 806: Prevalence of Adverse Social Determinants of Health in Families of Children With Critical Illness. Crit. Care Med. 2021, 49, 399. [Google Scholar] [CrossRef]
- Demers, L.A.; Wright, N.M.; Kopstick, A.J.; Niehaus, C.E.; Hall, T.A.; Williams, C.N.; Riley, A.R. Is Pediatric Intensive Care Trauma-Informed? A Review of Principles and Evidence. Children 2022, 9, 1575. [Google Scholar] [CrossRef] [PubMed]
- Kudchadkar, S.R. Healing Environments for Critically Ill Children: Development of a Multidisciplinary and Integrated Approach to Sleep, Sedation, Delirium and Early Mobilization. Ph.D. Thesis, Johns Hopkins University, Baltimore, MD, USA, 2018. [Google Scholar]
- Nagle, K.; Griffiths, N.; Hetherington, B.; Jatana, V.; Leutert, K.; Swift, L.; Thompson, K.; Ward, L. Implementing Neurodevelopmental Care Strategies in the Paediatric Intensive Care Unit. Aust. Crit. Care 2019, 32, S15. [Google Scholar] [CrossRef]
- Dalei, S.R.; Nayak, G.R.; Pradhan, R. Effect of art therapy and play therapy on anxiety among hospitalized preschool children. J. Biomed. Sci. 2020, 7, 71–76. [Google Scholar] [CrossRef]
- Ibrahim, H.A.; Amal, A.A. The Effectiveness of Play Therapy in Hospitalized Children with Cancer: Systematic Review. J. Nurs. Pract. 2020, 3, 233–243. [Google Scholar] [CrossRef]
- Pun, B.T.; Balas, M.C.; Barnes-Daly, M.A.; Thompson, J.L.; Aldrich, J.M.; Barr, J.; Byrum, D.; Carson, S.S.; Devlin, J.W.; Engel, H.J. Caring for critically ill patients with the ABCDEF bundle: Results of the ICU liberation collaborative in over 15,000 adults. Crit. Care Med. 2019, 47, 3. [Google Scholar] [CrossRef]
- Barnes-Daly, M.A.; Phillips, G.; Ely, E. Improving hospital survival and reducing brain dysfunction at seven California community hospitals: Implementing PAD guidelines via the ABCDEF bundle in 6064 patients. Crit. Care Med. 2017, 45, 171–178. [Google Scholar] [CrossRef]
- Waak, M.; Harnischfeger, J.; Ferguson, A.; Gibbons, K.; Nguyen, K.; Long, D. Every child, every day, back to play: The PICUstars protocol-implementation of a nurse-led PICU liberation program. BMC Pediatr. 2022, 22, 1–18. [Google Scholar] [CrossRef]
- Di Nardo, M.; Boldrini, F.; Broccati, F.; Cancani, F.; Satta, T.; Stoppa, F.; Genuini, L.; Zampini, G.; Perdichizzi, S.; Bottari, G. The LiberAction Project: Implementation of a Pediatric Liberation Bundle to Screen Delirium, Reduce Benzodiazepine Sedation, and Provide Early Mobilization in a Human Resource-Limited Pediatric Intensive Care Unit. Front. Pediatr. 2021, 9, 788997. [Google Scholar] [CrossRef]
- Lin, J.; Srivastava, A.; Traube, C.; Kawai, Y.; Kudchadkar, S.; Hielsberg, C.; Kumar, V.; Aghamohammadi, S.; Arteaga, G.; Smith, H. 861: Caring for critically ill children with the ABCDEF bundle: The PICU Liberation Collaborative. Crit. Care Med. 2022, 50, 426. [Google Scholar] [CrossRef]
- Arteaga, G.; Kawai, Y.; Rowekamp, D.; Rohlik, G.; Matzke, N.; Fryer, K.; Feigal, S.; Neu, L.; Graner, K.; Olson, A. 1289: The pediatric ICU liberation project impact on patient outcomes: The Mayo experience. Crit. Care Med. 2018, 46, 628. [Google Scholar] [CrossRef]
- Simone, S.; Edwards, S.; Lardieri, A.; Walker, L.K.; Graciano, A.L.; Kishk, O.A.; Custer, J.W. Implementation of an ICU bundle: An interprofessional quality improvement project to enhance delirium management and monitor delirium prevalence in a single PICU. Pediatr. Crit. Care Med. 2017, 18, 531–540. [Google Scholar] [CrossRef] [PubMed]
- Alzawad, Z.; Lewis, F.M.; Ngo, L.; Thomas, K. Exploratory model of parental stress during children’s hospitalisation in a paediatric intensive care unit. Intensive Crit. Care Nurs. 2021, 67, 103109. [Google Scholar] [CrossRef] [PubMed]
- Stremler, R.; Haddad, S.; Pullenayegum, E.; Parshuram, C. Psychological outcomes in parents of critically ill hospitalized children. J. Pediatr. Nurs. 2017, 34, 36–43. [Google Scholar] [CrossRef]
- Le Brocque, R.M.; Dow, B.L.; McMahon, H.; Crothers, A.L.; Kenardy, J.A.; Williams, T.J.; Long, D.A. The course of posttraumatic stress in children: Examination of symptom trajectories and predictive factors following admission to pediatric intensive care. Pediatr. Crit. Care Med. 2020, 21, e399–e406. [Google Scholar] [CrossRef]
- Geiger, J.M.; Schelbe, L. The Handbook on Child Welfare Practice; Springer: Cham, Switzerland, 2021. [Google Scholar]
- Le Brocque, R.M.; Hendrikz, J.; Kenardy, J.A. Parental response to child injury: Examination of parental posttraumatic stress symptom trajectories following child accidental injury. J. Pediatr. Psychol. 2010, 35, 646–655. [Google Scholar] [CrossRef]
- McQuillan, M.E.; Bates, J.E. Parental stress and child temperament. In Parental Stress and Early Child Development; Springer: Cham, Switzerland, 2017; pp. 75–106. [Google Scholar]
- Mustard, J.F. Experience-based brain development: Scientific underpinnings of the importance of early child development in a global world. Paediatr. Child Health 2006, 11, 571–572. [Google Scholar] [CrossRef]
- Lebel, C.; Deoni, S. The development of brain white matter microstructure. Neuroimage 2018, 182, 207–218. [Google Scholar] [CrossRef]
- Keenan, H.T.; Presson, A.P.; Clark, A.E.; Cox, C.S.; Ewing-Cobbs, L. Longitudinal developmental outcomes after traumatic brain injury in young children: Are infants more vulnerable than toddlers? J. Neurotrauma 2019, 36, 282–292. [Google Scholar] [CrossRef]
- Aspesberro, F.; Mangione-Smith, R.; Zimmerman, J.J. Health-related quality of life following pediatric critical illness. Intensive Care Med. 2015, 41, 1235–1246. [Google Scholar] [CrossRef]
- Yagiela, L.M.; Carlton, E.F.; Meert, K.L.; Odetola, F.O.; Cousino, M.K. Parent medical traumatic stress and associated family outcomes after pediatric critical illness: A systematic review. Pediatr. Crit. Care Med. 2019, 20, 759–768. [Google Scholar] [CrossRef] [PubMed]
- Melnyk, B.M.; Alpert-Gillis, L.; Feinstein, N.F.; Crean, H.F.; Johnson, J.; Fairbanks, E.; Small, L.; Rubenstein, J.; Slota, M.; Corbo-Richert, B. Creating opportunities for parent empowerment: Program effects on the mental health/coping outcomes of critically ill young children and their mothers. Pediatrics 2004, 113, e597–e607. [Google Scholar] [CrossRef] [PubMed]
- Nelson, L.P.; Lachman, S.E.; Li, S.W.; Gold, J.I. The Effects of Family Functioning on the Development of Posttraumatic Stress in Children and their Parents following Admission to the Pediatric Intensive Care Unit. Pediatr. Crit. Care Med. 2019, 20, e208. [Google Scholar] [CrossRef] [PubMed]
- Rothschild, C.B.; Rychlik, K.L.; Goodman, D.M.; Charleston, E.; Brown, M.L.; Michelson, K.N.; Investigators, N.S. Association between resilience and psychological morbidity in parents of critically ill children. Pediatr. Crit. Care Med. 2020, 21, e177–e185. [Google Scholar] [CrossRef] [PubMed]
- Jakobsen, L.; Kristensen, K.K.; Laerkner, E. Parents’ experiences during and after their child’s stay in the paediatric intensive care unit–A qualitative interview study. Intensive Crit. Care Nurs. 2021, 67, 103089. [Google Scholar] [CrossRef]
- Suleman, Z.; Evans, C.; Manning, J.C. Parents’ and carers’ experiences of transition and aftercare following a child’s discharge from a paediatric intensive care unit to an in-patient ward setting: A qualitative systematic review. Intensive Crit. Care Nurs. 2019, 51, 35–44. [Google Scholar] [CrossRef]
- Fang, Y.; Boelens, M.; Windhorst, D.A.; Raat, H.; van Grieken, A. Factors associated with parenting self-efficacy: A systematic review. J. Adv. Nurs. 2021, 77, 2641–2661. [Google Scholar] [CrossRef]
- Albanese, A.M.; Russo, G.R.; Geller, P.A. The role of parental self-efficacy in parent and child well-being: A systematic review of associated outcomes. Child: Care Health Dev. 2019, 45, 333–363. [Google Scholar] [CrossRef]
- Edwards, J.D. Anticipatory guidance on the risks for unfavorable outcomes among children with medical complexity. J. Pediatr. 2017, 180, 247–250. [Google Scholar] [CrossRef]
- Thompson, A.L.; Young-Saleme, T.K. Anticipatory guidance and psychoeducation as a standard of care in pediatric oncology. Pediatr. Blood Cancer 2015, 62, S684–S693. [Google Scholar] [CrossRef]
- Pittard, W.B., III. Well Child Care Parental Anticipatory Guidance in the Preschool Years: Clinical Effectiveness. In Well Child Care in Infancy: Promoting Readiness for Life; AuthorHouse: Bloomington, IL, USA, 2013; pp. 93–118. [Google Scholar]
- Petteys, A.R.; Adoumie, D. Mindfulness-based neurodevelopmental care: Impact on NICU parent stress and infant length of stay; A randomized controlled pilot study. Adv. Neonatal Care 2018, 18, E12–E22. [Google Scholar] [CrossRef] [PubMed]
- Chan, N.; Neece, C.L. Mindfulness-based stress reduction for parents of children with developmental delays: A follow-up study. Evid. Based Pract. Child Adolesc. Ment. Health 2018, 3, 16–29. [Google Scholar] [CrossRef]
- Burgdorf, V.; Szabó, M.; Abbott, M.J. The effect of mindfulness interventions for parents on parenting stress and youth psychological outcomes: A systematic review and meta-analysis. Front. Psychol. 2019, 10, 1336. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Kumar, A. The mediating role of positive perceptions on coping strategies and psychological well-being among mothers of children with intellectual disabilities. Adv Ment. Health Intellect. Disabil. 2020, 14, 263–272. [Google Scholar] [CrossRef]
- Vernhet, C.; Dellapiazza, F.; Blanc, N.; Cousson-Gélie, F.; Miot, S.; Roeyers, H.; Baghdadli, A. Coping strategies of parents of children with autism spectrum disorder: A systematic review. Eur. Child Adolesc. Psychiatry 2019, 28, 747–758. [Google Scholar] [CrossRef] [PubMed]
- Hurley, D.; Allen, M.S.; Swann, C.; Vella, S.A. A matched control trial of a mental health literacy intervention for parents in community sports clubs. Child Psychiatry Hum. Dev. 2021, 52, 141–153. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Huang, F.; Koesters, M.; Staiger, T.; Becker, T.; Thornicroft, G.; Ruesch, N. Effectiveness of interventions to promote help-seeking for mental health problems: Systematic review and meta-analysis. Psychol. Med. 2018, 48, 2658–2667. [Google Scholar] [CrossRef]
- Melnyk, B.M.; Feinstein, N.; Fairbanks, E. Two decades of evidence to support implementation of the COPE program as standard practice with parents of young unexpectedly hospitalized/critically ill children and premature infants. Pediatr. Nurs. 2006, 32, 475. [Google Scholar] [PubMed]
- Muscara, F.; McCarthy, M.C.; Rayner, M.; Nicholson, J.M.; Dimovski, A.; McMillan, L.; Hearps, S.J.; Yamada, J.; Burke, K.; Walser, R. Effect of a Videoconference-Based Online Group Intervention for traumatic stress in parents of children with life-threatening illness: A randomized clinical trial. JAMA Netw. Open 2020, 3, e208507. [Google Scholar] [CrossRef]
- Baker, S.C.; Gledhill, J.A. Systematic review of interventions to reduce psychiatric morbidity in parents and children after PICU admissions. Pediatr. Crit. Care Med. 2017, 18, 343–348. [Google Scholar] [CrossRef]
- Johnston, C.C.; Rennick, J.E.; Filion, F.; Campbell-Yeo, M.; Goulet, C.; Bell, L.; Tucci, M.; Ranger, M. Maternal touch and talk for invasive procedures in infants and toddlers in the pediatric intensive care unit. J. Pediatr. Nurs. 2012, 27, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Azoulay, E.; Pochard, F.; Kentish-Barnes, N.; Chevret, S.; Aboab, J.; Adrie, C.; Annane, D.; Bleichner, G.; Bollaert, P.E.; Darmon, M. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am. J. Respir. Crit. Care Med. 2005, 171, 987–994. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, M.L.; Courtney, M. Reducing family members’ anxiety and uncertainty in illness around transfer from intensive care: An intervention study. Intensive Crit. Care Nurs. 2004, 20, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Dow, B.; De Young, A.; Schaefer, G.; Scott, G.; Long, D. Feasibility and acceptability of PICU-CARE to prevent persistent traumatic stress reactions in young children admitted to intensive care: Protocol for a pilot study of early intervention. Nurs. Crit. Care 2022. [Google Scholar] [CrossRef]
- Lipkin, P.H.; Macias, M.M.; Norwood, K.W.; Brei, T.J.; Davidson, L.F.; Davis, B.E.; Ellerbeck, K.A.; Houtrow, A.J.; Hyman, S.L.; Kuo, D.Z. Promoting optimal development: Identifying infants and young children with developmental disorders through developmental surveillance and screening. Pediatrics 2020, 145, e20193449. [Google Scholar] [CrossRef]
- Hirai, A.H.; Kogan, M.D.; Kandasamy, V.; Reuland, C.; Bethell, C. Prevalence and variation of developmental screening and surveillance in early childhood. JAMA Pediatr. 2018, 172, 857–866. [Google Scholar] [CrossRef]
- Long, D.A.; Fink, E.L. Transitions from short to long-term outcomes in pediatric critical care: Considerations for clinical practice. Transl. Pediatr. 2021, 10, 2858. [Google Scholar] [CrossRef]
- Long, D.; Gibbons, K.; Dow, B.; Best, J.; Webb, K.-L.; Liley, H.G.; Stocker, C.; Thoms, D.; Schlapbach, L.J.; Wharton, C. Effectiveness–implementation hybrid-2 randomised trial of a collaborative Shared Care Model for Detecting Neurodevelopmental Impairments after Critical Illness in Young Children (DAISY): Pilot study protocol. BMJ Open 2022, 12, e060714. [Google Scholar] [CrossRef]
- Williams, C.N.; Kirby, A.; Piantino, J. If you build it, they will come: Initial experience with a multi-disciplinary pediatric neurocritical care follow-up clinic. Children 2017, 4, 83. [Google Scholar] [CrossRef]
- Bele, S.; Chugh, A.; Mohamed, B.; Teela, L.; Haverman, L.; Santana, M.J. Patient-reported outcome measures in routine pediatric clinical care: A systematic review. Front. Pediatr. 2020, 8, 364. [Google Scholar] [CrossRef]
- Anderson, L.M.; Papadakis, J.L.; Vesco, A.T.; Shapiro, J.B.; Feldman, M.A.; Evans, M.A.; Weissberg-Benchell, J. Patient-reported and parent proxy-reported outcomes in pediatric medical specialty clinical settings: A systematic review of implementation. J. Pediatr. Psychol. 2020, 45, 247–265. [Google Scholar] [CrossRef] [PubMed]
- Ishaque, S.; Karnon, J.; Chen, G.; Nair, R.; Salter, A.B. A systematic review of randomised controlled trials evaluating the use of patient-reported outcome measures (PROMs). Qual. Life Res. 2019, 28, 567–592. [Google Scholar] [CrossRef] [PubMed]
- Anthony, L.; Hilder, A.; Newcomb, D.; Webb, K.-L.; Best, J.; Stocker, C.; Long, D. General practitioner perspectives on a shared-care model for paediatric patients post-intensive care: A cross-sectional survey. Aust. Crit. Care 2022. [Google Scholar] [CrossRef] [PubMed]
- Paul, R.; Roth, F.P. Characterizing and Predicting Outcomes of Communication Delays in Infants and Toddlers: Implications for Clinical Practice. Lang. Speech. Hear. Serv. Sch. 2011, 42, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Letourneau, N.; Drummond, J.; Fleming, D.; Kysela, G.; McDonald, L.; Stewart, M. Supporting parents: Can intervention improve parent-child relationships? J. Fam. Nurs. 2001, 7, 159–187. [Google Scholar] [CrossRef]
- Hansen, L. Empowering parents in PICUs-What are the barriers? Pediatr. Crit. Care Med. 2014, 15, 40–41. [Google Scholar] [CrossRef]
- Osher, D.; Cantor, P.; Berg, J.; Steyer, L.; Rose, T. Drivers of human development: How relationships and context shape learning and development1. Appl. Dev. Sci. 2020, 24, 6–36. [Google Scholar] [CrossRef]
- Sanders, M.R.; Turner, K.M.; Metzler, C.W. Applying self-regulation principles in the delivery of parenting interventions. Clin. Child Fam. Psychol. Rev. 2019, 22, 24–42. [Google Scholar] [CrossRef]
- Hoffman, M.F.; Karpyn, A.; Christofferson, J.; Neely, T.; McWhorter, L.G.; Demianczyk, A.C.; James, R.; Hafer, J.; Kazak, A.E.; Sood, E. Fathers of children with congenital heart disease: Sources of stress and opportunities for intervention. Pediatr. Crit. Care Med. 2020, 21, e1002. [Google Scholar] [CrossRef]
- Nagy, E.; Moore, S.; Silveira, P.P.; Meaney, M.J.; Levitan, R.D.; Dubé, L. Low socioeconomic status, parental stress, depression, and the buffering role of network social capital in mothers. J. Ment. Health 2022, 31, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Vreeland, A.; Gruhn, M.A.; Watson, K.H.; Bettis, A.H.; Compas, B.E.; Forehand, R.; Sullivan, A.D. Parenting in context: Associations of parental depression and socioeconomic factors with parenting behaviors. J. Child Fam. Stud. 2019, 28, 1124–1133. [Google Scholar] [CrossRef]
- Palix Foundation. Alberta Family Wellness Initiative. Available online: https://www.albertafamilywellness.org/training/ (accessed on 28 August 2022).
- Gagnon, M.L. The Alberta Family Wellness Initiative: Catalyzing Positive Change Based on Brain Story Understanding and Documenting the Difference It Can Make. In Handbook of Child Maltreatment; Springer: Cham, Switzerland, 2022; pp. 429–444. [Google Scholar]
- UNICEF. Early Moments Matter. Available online: https://www.unicef.org/early-moments (accessed on 28 August 2022).
- Victora, C.G.; Wagstaff, A.; Schellenberg, J.A.; Gwatkin, D.; Claeson, M.; Habicht, J.-P. Applying an equity lens to child health and mortality: More of the same is not enough. Lancet 2003, 362, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Guralnick, M.J. Why early intervention works: A systems perspective. Infants Young Child. 2011, 24, 6. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Nurturing Care for Early Childhood Development: A Framework for Helping Children Survive and Thrive to Transform Health and Human Potential. 2018. Available online: https://nurturing-care.org/handbook/ (accessed on 28 August 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Long, D.A.; Waak, M.; Doherty, N.N.; Dow, B.L. Brain-Directed Care: Why Neuroscience Principles Direct PICU Management beyond the ABCs. Children 2022, 9, 1938. https://doi.org/10.3390/children9121938
Long DA, Waak M, Doherty NN, Dow BL. Brain-Directed Care: Why Neuroscience Principles Direct PICU Management beyond the ABCs. Children. 2022; 9(12):1938. https://doi.org/10.3390/children9121938
Chicago/Turabian StyleLong, Debbie A., Michaela Waak, Nicola N. Doherty, and Belinda L. Dow. 2022. "Brain-Directed Care: Why Neuroscience Principles Direct PICU Management beyond the ABCs" Children 9, no. 12: 1938. https://doi.org/10.3390/children9121938
APA StyleLong, D. A., Waak, M., Doherty, N. N., & Dow, B. L. (2022). Brain-Directed Care: Why Neuroscience Principles Direct PICU Management beyond the ABCs. Children, 9(12), 1938. https://doi.org/10.3390/children9121938






