Knowledge, Attitudes and Professional Behavior of Silver Diamine Fluoride among Dental Personnel: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Study Selection and Extraction
2.4. Assessment of Quality
3. Results
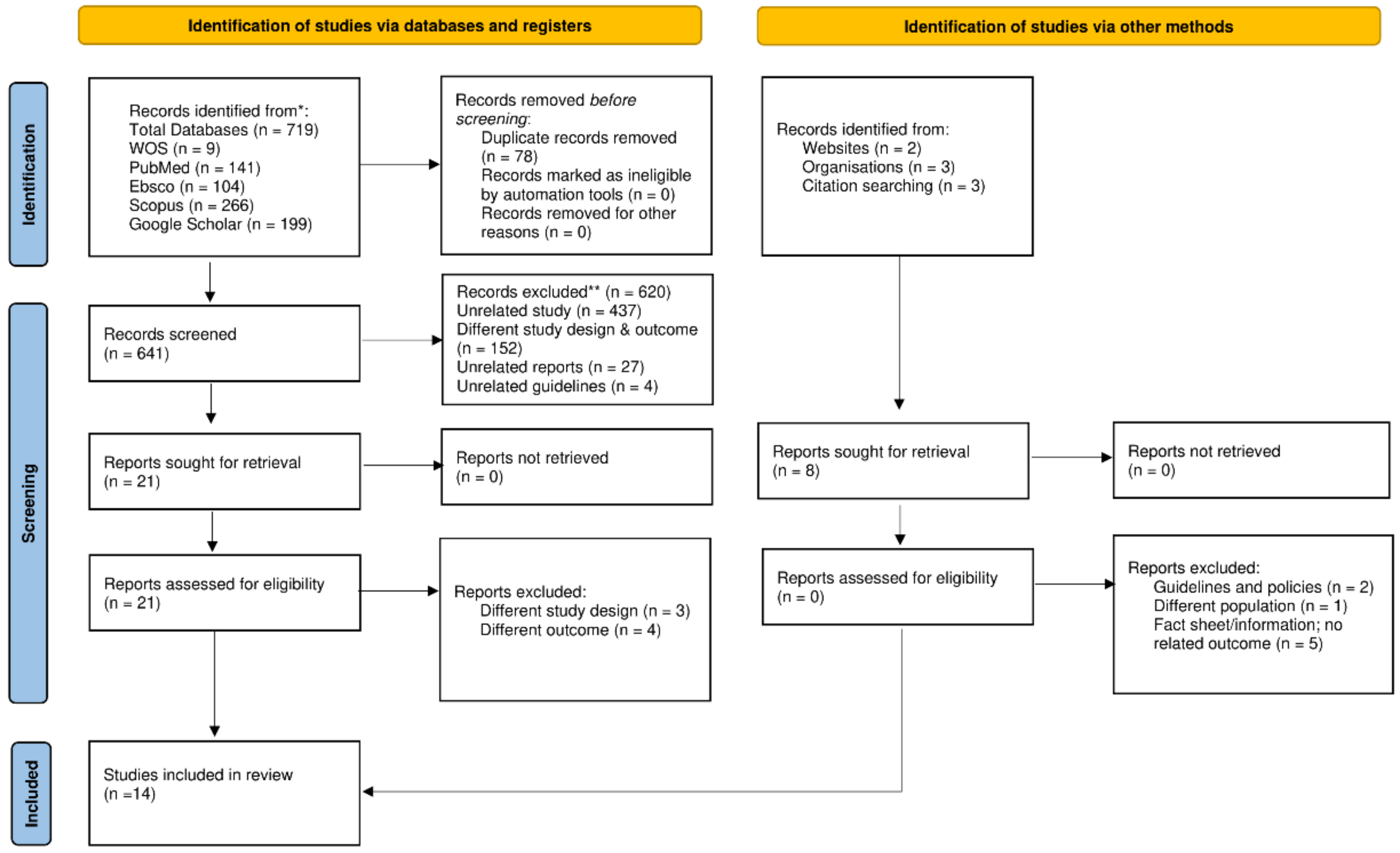
3.1. Study Selection
3.2. General Characteristics of Studies Included and Main Demographics of Studied Population
3.3. Quality Assessment of Selected Studies
3.4. Main Outcomes
3.4.1. Knowledge/Awareness Related to Silver Diamine Fluoride and Related Association Factors
3.4.2. Attitude, Professional Behavior/Usage of Silver Diamine Fluoride, and Related Associated Factors
3.4.3. Perceptions/Perceived Barriers or Advantages of Silver Diamine Fluoride and Related Associated Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| No. | Concept | Search String | Number |
|---|---|---|---|
| #1 | Silver diamine fluoride | ((((((((silver diamine fluoride) OR (diamine silver fluoride)) OR (ammoniacal silver fluoride)) OR (silver ammonia fluoride)) OR (silver fluoride)) OR (quaternary ammonium compounds)) OR (saforide)) OR (Riva Star)) OR (silver nitrate + caries) | 115,098 |
| #2 | Knowledge Awareness Attitude Professional Usage Barrier | ((((knowledge) OR (awareness)) OR (attitude)) OR (professional usage)) OR (barrier) | 1,840,208 |
| #3 | Dental personnel | ((((((((dental personnel) OR (general dentist)) OR (dental therapist)) OR (specialist)) OR (dental specialist)) OR (pediatric)) OR (dental professional)) OR (dentist)) OR (dental nurse) | 1,254,895 |
| #4 | Limited to English | #1 AND #2 AND #3 | 141 |
| No. | Concept | Search String | Number |
|---|---|---|---|
| #1 | Silver diamine fluoride | ((((((((silver diamine fluoride) OR (diamine silver fluoride)) OR (ammoniacal silver fluoride)) OR (silver ammonia fluoride)) OR (silver fluoride)) OR (quaternary ammonium compounds)) OR (saforide)) OR (Riva Star)) OR (silver nitrate + caries) | 134,085 |
| #2 | Knowledge Awareness Attitude Professional Usage Barrier | ((((knowledge) OR (awareness)) OR (attitude)) OR (professional usage)) OR (barrier) | 8,913,542 |
| #3 | Dental personnel | ((((((((dental personnel) OR (general dentist)) OR (dental therapist)) OR (specialist)) OR (dental specialist)) OR (pediatric)) OR (dental professional)) OR (dentist)) OR (dental nurse) | 3,535,596 |
| #4 | Limited to English | #1 AND #2 AND #3 | 1324 |
| #5 | Limited to English and dentistry | #1 AND #2 AND #3 | 266 |
| No. | Concept | Search String | Number |
|---|---|---|---|
| #1 | Silver diamine fluoride | ((((((((silver diamine fluoride) OR (diamine silver fluoride)) OR (ammoniacal silver fluoride)) OR (silver ammonia fluoride)) OR (silver fluoride)) OR (quaternary ammonium compounds)) OR (saforide)) OR (Riva Star)) OR (silver nitrate + caries) | 44,072 |
| #2 | Knowledge Awareness Attitude Professional Usage Barrier | ((((knowledge) OR (awareness)) OR (attitude)) OR (professional usage)) OR (barrier) | 3,283,655 |
| #3 | Dental personnel | ((((((((dental personnel) OR (general dentist)) OR (dental therapist)) OR (specialist)) OR (dental specialist)) OR (pediatric)) OR (dental professional)) OR (dentist)) OR (dental nurse) | 820,839 |
| #4 | Limited to English | #1 AND #2 AND #3 | 1055 |
| #5 | Limited to English and dentistry | #1 AND #2 AND #3 | 104 |
| No. | Concept | Search String | Number |
|---|---|---|---|
| #1 | Silver diamine fluoride | ((((((((silver diamine fluoride) OR (diamine silver fluoride)) OR (ammoniacal silver fluoride)) OR (silver ammonia fluoride)) OR (silver fluoride)) OR (quaternary ammonium compounds)) OR (saforide)) OR (Riva Star)) OR (silver nitrate + caries) | 7900 |
| #2 | Knowledge Awareness Attitude Professional Usage Barrier | ((((knowledge) OR (awareness)) OR (attitude)) OR (professional usage)) OR (barrier) | 3,200,272 |
| #3 | Dental personnel | ((((((((dental personnel) OR (general dentist)) OR (dental therapist)) OR (specialist)) OR (dental specialist)) OR (pediatric)) OR (dental professional)) OR (dentist)) OR (dental nurse) | 488,974 |
| #4 | Limited to English | #1 AND #2 AND #3 | 13 |
| #5 | Limited to English and dentistry | #1 AND #2 AND #3 | 9 |
- GOOGLE SCHOLAR
- 2.
- Other sources
Appendix B
| Study NIH Checklist for | Antonioni et al., 2019 [21] | Chen et al., 2019 [22] | Chhokar et al., 2017 [23] | Dang et al., 2020 [24] | Pizano JM, 2017 [25] | Al Ashwal et al., 2020 [26] | Alajlan et al., 2020 [27] | Azzawi et al., 2021 [28] | Ezzeldin et al., 2021 [29] | Alshammari et al., 2021 [30] | Vollu et al., 2020 [31] | Schroë et al., 2022 [17] | Abbas et al., 2021 [32] | Mehlawat et al., 2022 [33] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Was the research question or objective in this paper clearly stated? | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| 2. Was the study population clearly specified and defined? | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| 3. Was the participation rate of eligible persons at least 50%? | X | X | X | √ | X | NR | √ | √ | X | √ | X | X | NR | √ |
| 4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| 5. Was a sample size justification, a power description, or variance and effect estimates provided? | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| 6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| 7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| 8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as a continuous variable)? | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 9. Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? | √ | NR | √ | √ | √ | NR | √ | √ | NR | √ | NR | √ | √ | √ |
| 10. Was the exposure(s) assessed more than once over time? | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| 12. Were the outcome assessors blinded to the exposure status of participants? | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 13. Was loss to follow-up after baseline 20% or less? | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| 14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? | √ | X | √ | √ | √ | √ | √ | √ | X | √ | √ | X | √ | X |
| CD = cannot determine; NA = not applicable; NR = not reported. | ||||||||||||||
| √, Yes; X, No. |
References
- GBD Oral Disorders Collaborators; Bernabe, E.; Marcenes, W.; Hernandez, C.; Bailey, J.; Abreu, L.; Alipour, V.; Amini, S.; Arabloo, J.; Arefi, Z. Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: A systematic analysis for the global burden of disease 2017 study. J. Dent. Res. 2020, 99, 362–373. [Google Scholar]
- World Health Organization. Sugars and Dental Caries (No. WHO/NMH/NHD/17.12); World Health Organization: Geneva, Switzerland, 2017; Available online: https://apps.who.int/iris/handle/10665/259413 (accessed on 1 October 2022).
- Petersen, P.E.; Ogawa, H. Prevention of dental caries through the use of fluoride–the WHO approach. Community Dent Health 2016, 33, 66–68. [Google Scholar]
- Seifo, N.; Robertson, M.; MacLean, J.; Blain, K.; Grosse, S.; Milne, R.; Seeballuck, C.; Innes, N. The use of silver diamine fluoride (SDF) in dental practice. Br. Dent. J. 2020, 228, 75–81. [Google Scholar] [CrossRef]
- Innes, N.; Chu, C.; Fontana, M.; Lo, E.; Thomson, W.; Uribe, S.; Heiland, M.; Jepsen, S.; Schwendicke, F. A century of change towards prevention and minimal intervention in cariology. J. Dent. Res. 2019, 98, 611–617. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.; Zhao, I.; Hiraishi, N.; Duangthip, D.; Mei, M.; Lo, E.; Chu, C. Clinical trials of silver diamine fluoride in arresting caries among children: A systematic review. JDR Clin. Transl. Res. 2016, 1, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Contreras, V.; Toro, M.J.; Elías-Boneta, A.R.; Encarnación-Burgos, M.A. Effectiveness of silver diamine fluoride in caries prevention and arrest: A systematic literature review. Gen. Dent. 2017, 65, 22. [Google Scholar]
- Rosenblatt, A.; Stamford, T.; Niederman, R. Silver diamine fluoride: A caries “silver-fluoride bullet”. J. Dent. Res. 2009, 88, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, A. A clinical study of effect of diamine silver fluoride on recurrent caries. J. Osaka Univ. Dent. Sch. 1976, 16, 103–109. [Google Scholar]
- Horst, J.A.; Ellenikiotis, H.; Milgrom, P.M.; Committee, U.S.C.A. UCSF protocol for caries arrest using silver diamine fluoride: Rationale, indications, and consent. J. Calif. Dent. Assoc. 2016, 44, 16. [Google Scholar] [PubMed]
- Seto, J.; Horst, J.A.; Parkinson, D.Y.; Frachella, J.C.; DeRisi, J.L. Enhanced Tooth Structure Via Silver Microwires Following Treatment with 38 Percent Silver Diamine Fluoride. Pediatric Dent. 2020, 42, 226–231. [Google Scholar]
- Woolfolk, S.K.; Cloyd, A.K.; Ye, Q.; Boone, K.; Spencer, P.; Snead, M.L.; Tamerler, C. Peptide-Enabled Nanocomposites Offer Biomimetic Reconstruction of Silver Diamine Fluoride-Treated Dental Tissues. Polymers 2022, 14, 1368. [Google Scholar] [CrossRef]
- Seifo, N.; Cassie, H.; Radford, J.R.; Innes, N.P. Silver diamine fluoride for managing carious lesions: An umbrella review. BMC Oral Health 2019, 19, 145. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.S.; Zhang, S.; Mei, M.L.; Lo, E.C.-M.; Chu, C.-H. Caries remineralisation and arresting effect in children by professionally applied fluoride treatment—A systematic review. BMC Oral Health 2016, 16, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Chaffin, J.; Gold, J.; Vidone, L. Silver diamine fluoride: Overview and perspective for payers. Beacon 2016, 2, 14–18. [Google Scholar]
- Gao, S.S.; Amarquaye, G.; Arrow, P.; Bansal, K.; Bedi, R.; Campus, G.; Chen, K.J.; Chibinski, A.C.R.; Chinzorig, T.; Crystal, Y.O.; et al. Global Oral Health Policies and Guidelines: Using Silver Diamine Fluoride for Caries Control. Front. Oral Health 2021, 2, 685557. [Google Scholar] [CrossRef]
- Schroë, S.C.; Bonifacio, C.C.; Bruers, J.J.; Innes, N.P.; Hesse, D. General and Paediatric Dentists’ Knowledge, Attitude and Practices Regarding the use of Silver Diammine Fluoride for the Management of Dental Caries: A National Survey in the Netherlands. BMC Oral Health 2022, 22, 458. [Google Scholar] [CrossRef]
- Seifo, N.; Cassie, H.; Radford, J.; Innes, N. “It’s really no more difficult than putting on fluoride varnish”: A qualitative exploration of dental professionals’ views of silver diamine fluoride for the management of carious lesions in children. BMC Oral Health 2020, 20, 257. [Google Scholar] [CrossRef]
- Timms, L.; Graham, A.; Gallacher, N.; Large, J.; Simpson, S.; Johnson, R.; Gallichan, N.; Oliver, R.; Morgan, E.; Hardwick, C. Paediatric dentists’ views on the use of silver diammine fluoride: A UK perspective. Fac. Dent. J. 2021, 12, 114–119. [Google Scholar] [CrossRef]
- NIH. Study Quality Assessment Tools. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 4 July 2022).
- Antonioni, M.B.; Fontana, M.; Salzmann, L.B.; Inglehart, M.R. Pediatric Dentists’ Silver Diamine Fluoride Education, Knowledge, Attitudes, and Professional Behavior: A National Survey. J. Dent. Educ. 2019, 83, 173–182. [Google Scholar] [CrossRef]
- Chen, Y.-S. Evaluating the Knowledge and Opinions of Army Dentists Regarding Silver Diamine Fluoride. Master’s Thesis, Uniformed Services University of The Health Sciences , Bethesda, MD, USA, 2019. [Google Scholar]
- Chhokar, S.K.; Laughter, L.; Rowe, D.J. Perceptions of Registered Dental Hygienists in Alternative Practice Regarding Silver Diamine Fluoride. J. Dent. Hyg. 2017, 91, 53–60. [Google Scholar] [PubMed]
- Dang, C.; Comnick, C.L.; Tabrizi, M.; Kaufman, L.; Soto, A.; Smith, B.M.; Ribeiro, A.P.D.; Tobey, T.; Capin, O.R.; Scully, A. Assessment of knowledge and perception about silver diamine fluoride (SDF) for treating older adults among graduating dental students. J. Dent. Educ. 2020, 84, 1210–1218. [Google Scholar] [CrossRef] [PubMed]
- Pizano, J.M. Opinions and Current Practices of General Dentists, Pediatric Dentists, and Pediatricians of Ohio Regarding Silver Diamine Fluoride. Master’s Thesis, The Ohio State University, Columbus, OH, USA, 2017. [Google Scholar]
- Al Ashwal, L.A.; Al Kharan, M.I. Assessment of knowledge about silver diamine fluoride in Riyadh Elm University among students (levels 11 and 12) and interns. Int. J. Med. Dev. Ctries. 2020, 4, 1831–1836. [Google Scholar]
- Alajlan, G.; Alshaikh, H.; Alshamrani, L.; Alanezi, M.; Alarfaj, S.; AlSwayyed, T. Knowledge on and Attitude toward Silver Diamine Fluoride among Saudi Dental Practitioners in Riyadh Public Hospitals. Clin. Cosmet. Investig. Dent. 2020, 12, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Azzawi, B.Y.; Abushanab, R.; Nadeem, R.; Almotairi, D.; Alghtani, M.; Wali, O.; Vanka, S.; Vanka, A. Knowledge, attitudes, and practices of pediatric dentists towards silver di amine fluoride. Ann. Dent. Spec. 2021, 9, 1–6. [Google Scholar] [CrossRef]
- Ezzeldin, T.; Al-Awasi, K.A.; Bader, R.M.; Alshaikhi, A.Y.; Hakami, A.H.; Siddiqui, I.A.; Almulhim, A.A.; Alsubaie, T.M. A Study to assess the awareness and use of Silver Diammine Fluoride and Hall Technique among dental professionals and dental students in the Eastern Province. Saudi Dent. J. 2021, 33, 1166–1173. [Google Scholar] [CrossRef] [PubMed]
- Alshammari, A.F.; Alenzi, R.H.; Alanezi, A.A.; Enizy, A.S.; Aldakhil, A.M.; Alkurdi, K.A. Knowledge and Attitude of Dentists toward Silver Diamine Fluoride in Saudi Arabia. Int. J. Clin. Pediatr. Dent. 2021, 14, 662–665. [Google Scholar] [CrossRef]
- Vollu, A.L.; Moreira, J.P.D.; Luiz, R.R.; Barja-Fidalgo, F.; Fonseca-Goncalves, A. Survey of Knowledge, Attitudes and Practices of Brazilian Dentists Regarding Silver Diamine Fluoride. Pesqui. Bras. Odontopediatria Clínica Integr. 2020, 20, 7. [Google Scholar] [CrossRef]
- Abbas, B.; Aamer, S.; Anwar, F.S.; Farhan, F.; Wajahat, M.; Khurshid, Z. Perception, Knowledge, and Professional Behavior of Dentists about Silver Diamine Flouride: A Nationwide Survey. Eur. J. Gen. Dent. 2022, 11, 032–037. [Google Scholar] [CrossRef]
- Mehlawat, J.; Marya, C.; Nagpal, R.; Kataria, S.; Taneja, P. Dentists’ knowledge, attitudes, and professional behavior regarding silver diamine fluoride: A cross-sectional questionnaire study. J. Indian Assoc. Public Health Dent. 2022, 20, 188–192. [Google Scholar] [CrossRef]
- World Health Organization. WHO Expert Consultation on Public Health Intervention against Early Childhood Caries: Report of a Meeting, Bangkok, Thailand, 26–28 January 2016; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Crystal, Y.O.; Janal, M.N.; Yim, S.; Nelson, T. Teaching and utilization of silver diamine fluoride and Hall-style crowns in US pediatric dentistry residency programs. J. Am. Dent. Assoc. 2020, 151, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Crystal, Y.O.; Marghalani, A.A.; Ureles, S.D.; Wright, J.T.; Sulyanto, R.; Divaris, K.; Fontana, M.; Graham, L. Use of silver diamine fluoride for dental caries management in children and adolescents, including those with special health care needs. Pediatric Dent. 2017, 39, 135E–145E. [Google Scholar]
- Horst, J. Silver fluoride as a treatment for dental caries. Adv. Dent. Res. 2018, 29, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Arheiam, A.; Bankia, I.; Ingafou, M. Perceived competency towards preventive dentistry among dental graduates: The need for curriculum change. Libyan J. Med. 2015, 10, 26666. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, T.; Tandon, S.; Chand, S.; Bhargava, A. Knowledge, attitude and practice towards preventive dental care-A KAP study. J. Glob. Oral Health 2019, 2, 36–40. [Google Scholar] [CrossRef]
- Patil, R.U.; Sahu, A.; Kambalimath, H.V.; Panchakshari, B.K.; Jain, M. Knowledge, Attitude and Practice among Dental Practitioners Pertaining to Preventive Measures in Paediatric Patients. J. Clin. Diagn. Res. 2016, 10, ZC71–ZC75. [Google Scholar] [CrossRef]
- Michie, S.; Van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 1–12. [Google Scholar] [CrossRef]
- Crystal, Y.O.; Niederman, R. Evidence-based dentistry update on silver diamine fluoride. Dent. Clin. 2019, 63, 45–68. [Google Scholar] [CrossRef]
- Crystal, Y.O.; Janal, M.N.; Hamilton, D.S.; Niederman, R. Parental perceptions and acceptance of silver diamine fluoride staining. J. Am. Dent. Assoc. 2017, 148, 510–518.e514. [Google Scholar] [CrossRef]
- Duangthip, D.; Fung, M.; Wong, M.; Chu, C.; Lo, E. Adverse effects of silver diamine fluoride treatment among preschool children. J. Dent. Res. 2018, 97, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Nelson, T.; Scott, J.M.; Crystal, Y.O.; Berg, J.H.; Milgrom, P. Silver Diamine Fluoride in Pediatric Dentistry Training Programs: Survey of Graduate Program Directors. Pediatr. Dent. 2016, 38, 212–217. [Google Scholar]
- American Academy of Pediatric Dentistry. Policy on the Use of Silver Diamine Fluoride for Pediatric Dental Patients. Pediatr. Dent. 2017, 39, 51–53. [Google Scholar]
- Association of State and Territorial Dental Directors (ASTDD). Silver Diamine Fluoride (SDF) Fact Sheet; Association of State and Territorial Dental Directors (ASTDD): Reno, NV, USA, 2017; Available online: https://www.astdd.org/www/docs/sdf-fact-sheet-09-07-2017.pdf (accessed on 1 October 2022).
| Author/Year | Country | Type of Study | Data Collection | Measured Outcome |
|---|---|---|---|---|
| Antonioni et al., 2019 [21] | United States of America | Cross-sectional | Web-based survey, validated questionnaire | Knowledge, attitudes, SDF usage |
| Chen et al., 2019 [22] | United States of America | Cross-sectional | Online survey (distributed via email, validation of questionnaire not mentioned) | Knowledge, attitudes, perceived barriers |
| Chhokar et al., 2017 [23] | United States of America | Cross-sectional | Online survey distributed via email, pre-test carried out with 12 dental personnel (dental hygienists and dentists) | Knowledge, perceptions, SDF usage |
| Dang et al., 2020 [24] | United States of America | Cross-sectional | Paper distribution, content validation | Knowledge, perceptions, SDF usage |
| Pizano, 2017 [25] | United States of America | Cross-sectional | Online survey distributed via email, questions developed by a group of experts and pilot tested | Knowledge, attitudes, perceptions, barriers, SDF usage |
| Al Ashwal et al., 2020 [26] | Saudi Arabia | Cross-sectional | Papers and online survey, validation of questionnaire not mentioned | Knowledge, perceived barriers to SDF, professional usage |
| Alajlan et al., 2020 [27] | Saudi Arabia | Cross-sectional | Online survey, validated and published questionnaire | Knowledge, attitudes, perceived barriers, SDF usage |
| Azzawi et al., 2021 [28] | Saudi Arabia | Cross-sectional | Online survey (Google Form), pretested questionnaire | Knowledge, perceive barriers, SDF usage |
| Ezzeldin et al., 2021 [29] | Saudi Arabia | Cross-sectional | Online survey, distributed via WhatsApp message, validation of questionnaire not mentioned | Knowledge/awareness, SDF usage |
| Alshammari et al., 2021 [30] | Saudi Arabia | Cross-sectional | Online survey using a pretested questionnaire | Knowledge, perceived barriers, SDF usage |
| Vollu et al., 2020 [31] | Brazil | Cross-sectional | Online survey distributed via email, validation of questionnaire not mentioned | Knowledge, perceived barriers, SDF usage |
| Schroë et al., 2022 [17] | The Netherlands | Cross-sectional | Paper questionnaire or online survey, pretested | Knowledge, attitudes, SDF usage |
| Abbas et al., 2021 [32] | Pakistan | Cross-sectional | Survey (not reported on paper or online), pretested questionnaire | Knowledge, attitudes |
| Mehlawat et al., 2022 [33] | India | Cross-sectional | Online survey distributed via WhatsApp group, pretested questionnaire | Knowledge, attitudes, SDF usage |
| Author/Year | Study Population | Sample Size and Response Rate (%) | Gender | Age | Years in Practice (Practitioner/Student) |
|---|---|---|---|---|---|
| Antonioni et al., 2019 [21] | Pediatric dentists | 582 (9.34%) | Male 53% Female 47% | Mean age 45.68 ± 12.71 years (range 26–79 years) | Graduation year Degree 1997 ± 13.08 years (range 1964–2015) Specialist 2001 ± 12.92 years (range 1968–2016) |
| Chen et al., 2019 [22] | Army dentists (general dentists, comprehensive dentists, pediatric dentists) | 237 (31.73%) | Male 70.89% Female 28.27% | NR | <2 years 26.16% 2–5 years 37.97% 6–9 years 15.19% 10–13 years 8.02% 14–17 years 4.22% ≥18 years 8.44% |
| Chhokar et al., 2017 [23] | Dental hygienists | 103 (46.0%) | NR | NR | <1 year 12.0% 1–3 years 27.0% 4–6 years 21.0% 7–10 years 26.0% >10 years 14.0% |
| Dang et al., 2020 [24] | Dental students | 386 (55.0%) | NR | Median age 27 ± 4.2 years (range 23–47 years | Graduating dental students |
| Pizano, 2017 [25] | Dentists, pediatric dentists | 455 (11.3%) | Pediatric dentists Male 60.0% Female 40.0% Dentists Male 65.0% Female 35.0% Pediatrician Male 15.0% Female 85.0% | Pediatric dentists 20–40 years 50.0% 41–60 years 31.0% ≥61 years 19.0% Dentists 20–40 years 37.0% 41–60 years 37.0% >61 years 26.0% | Pediatric dentists 1–10 years 45.0% 11–20 years 17.0% >20 years 38.0% Dentists 1–10 years 33.0% 11–20 years 15.0% >20 years 52.0% |
| Al Ashwal et al., 2020 [26] | Dental students and interns | 252 (Response rate was not mentioned) | Male 39.7% Female 60.3% | ≤25 years 79.4% >25 years 20.6% | Level 11 33.7% Level 12 42.9% Intern 23.4% |
| Alajlan et al., 2020 [27] | Dental practitioners in public hospitals | 278 (100%) | Male 39.93% Female 60.07% | 24– 35 years 75.0% 36–45 years 17.27% >45 years 7.55% | NR |
| Azzawi et al., 2021 [28] | Pediatric dentists | 58 (58.0%) | Male 27.6% Female 72.4% | 25–40 years 62.4% >40 years 27.6% | Not stated |
| Ezzeldin et al., 2021 [29] | Dental students, dentists, and specialists | 312 (22.8%) | Students Male 30.6% Female 69.4% Dentists Male 33.8% Female 66.2% Specialists Male 43.1% Female 56.9% | Students 20–25 years 89.9% 25–45 years 10.1% Dentists 20–35 years 90.9% 36–45 years 7.7% >50 years 1.4% Specialists 20–35 years 54.2% 36–45 years 27.7% >50 years 18.1% | Students ≤1 year 100.0%% Dentists ≤1 year 43.2% 2–5 years 24.5% 6–10 years 24.5% 11–20 years 5.1% >20 years 2.9% Specialists ≤1 year 9.9% 2–5 years 23.9% 6–10 years 18.3% 11–20 years 29.6% >20 years 18.3% |
| Alshammari et al., 2021 [30] | Dentists | 150 (83.3%) | Male 62.0% Female 38.0% | 25–35 years 98.7% 35–45 years 1.3% | Not stated |
| Vollu et al., 2020 [31] | Dentists | 409 (3.89%) | NR | NR | Mean 16.83 ± 11.64 years |
| Schroë et al., 2022 [17] | Dentists, pediatric dentists | 167 (25.0%) | Dentists Male 46.0% Female 54.0% Pediatric dentists Male 15.0% Female 85.0% | Dentists <35 years 41.0% 35–50 years 25.0% >51 years 34.0% Pediatric dentists <35 years 4.0% 35–50 years 70.0% >51 years 26.0% | Dentists <1 year 1.0% 1–5 years 30.0% 6–10 years 11.0% >10 years 58.0% Pediatric dentists 1–5 years 4.0% 6–10 years 4.0% >10 years 92.0% |
| Abbas et al., 2021 [32] | Dentists | 223 (Response rate not mentioned) | Male 21.2% Female 78.8% | 20–30 years 63.2% 31–40 years 30.0% 41–50 years 6.7% | NR |
| Mehlawat et al., 2022 [33] | Dentists | 127 (63.5%) | Male 24.8% Female 75.2% | NR | NR |
| Author/Year | Knowledge/Awareness | Attitude/Consideration | Perception/Perceived Barrier or Advantage | Practice/Professional Usage | Associated Factor |
|---|---|---|---|---|---|
| Antonioni et al., 2019 [21] | • General SDF knowledge Mean 3.63 • Cavitated-lesion knowledge Mean 4.11 • Non-cavitated-lesion knowledge Mean 3.88 • SDF use prior to all restorative treatment Mean 1.94 (Range 1.00–5.00) | • Patient-related indications for SDF usage Mean 4.24 • Cost-related indications for SDF usage Mean 3.74 • Considerations to treatment not in aesthetic zone Mean 4.07 • Considerations to treatment in aesthetic zone Mean 2.66 (Range 1.00–5.00) | NR | Office use of SDF Mean 2.46 (Range 1.00–5.00) • 67.0% used SDF to arrest carious lesions in primary teeth • 87.0% expected to increase their SDF use in the future | Knowledge ↑ • SDF professional development education SDF usage ↑ • Positive SDF related attitude SDF usage ↓ • Older age |
| Chen et al., 2019 [22] | • Had heard of SDF 87.76% • Knows that SDF arrests caries in the dentin 94.51% • Knows how to apply SDF 47.68% | • Want to know more about SDF in clinical use after reading the summary of SDF 91.38% • Interested in making SDF available in military clinics 73.28% • Would consider using SDF if provided 95.3% • Would use SDF on an adult patient (permanent teeth) if it was a posterior tooth and the patient was fully aware regarding the staining after caries are arrested 87.93% | • SDF may weaken bonding strength for resin restorations 2.59% • Prefer to use other materials for cavity prevention and remineralization 8.19% • SDF is a technique-sensitive procedure that is not simple to apply 3.02% • Do not believe in the effectiveness of SDF 2.16% | NR | NR |
| Chhokar et al., 2017 [23] | • Had never heard of SDF 32% • Had heard of SDF but not sure what it is used for 22% • Aware of what SDF is used for 43% • Had observed SDF being used 1% | NR | • Alternative treatment to removing tooth structure with a dental drill 82% • Less expensive 82% • Applied like a varnish and therefore is time efficient 86% • Does not require the use of LA 91% • Reduced acceptance from parents/patients due to the permanent black staining 56% • SDF advantages > disadvantages to the patients I am accustomed to treating as a dental hygienist 95% | • Used SDF once 0% • Used SDF a few times 0% • Use SDF occasionally 1% • Use SDF frequently 1% | SDF advantages > disadvantages • Intention to offer SDF to patient Perception |
| Dang et al., 2020 [24] | • SDF properties Average score 4 average Range 0–6 • SDF indication Average score 1 average Range 0–2 | NR | • SDF usefulness Median score 3 (SD = 1.25, range: −4–4) • SDF appropriateness Median score 2 (SD = 2.48, range: −6–6) • Students’ willingness to use SDF Median score 1 (SD = 0.74, range: −2–2), • Patients’ willingness to use SDF Median score 1 (SD = 0.86, range: −2–2) | Clinical experiences using SDF for older adults 54.8% | “SDF usefulness,” “SDF appropriateness,” and “SDF patient willingness to use” were significantly associated with higher perception scores of student willingness to use SDF |
| Pizano JM, 2017 [25] | Patients indicated for SDF treatment: • Uncooperative 0–3 years old patients Pediatric dentists 76% Dentists 73% • Patients with special health care needs Pediatric dentists 71% Dentists 73% | • Appropriate for treatment on primary posterior teeth Pediatric dentists 81% Dentists 94% | • Pediatric dentists Aesthetics 83% Not covered by insurance 55% Multiple appointments are needed 38% • Dentists Aesthetics 86% Lack of training 54% Not covered by insurance 46% | • Currently using SDF in practice Pediatric dentists 45% Dentists 15% | • Willingness to provide SDF Fewer years in practice, younger age |
| Al Ashwal et al., 2020 [26] | • 54.8% did not know anything about SDF • 52.8% did not know the primary function • Knowledge among students and interns was low; 57.9% had little awareness of SDF | NR | • Stains 50.4% • Metallic taste 51.2% | 67% did not know SDF application technique | Knowledge • Reading about SDF • Knowing SDF’s primary function |
| Alajlan et al., 2020 [27] | Average level with mean of 3.12 (out of 5) | Average level with mean of 3.39 (out of 5) | Mean of 4.37 • Permanent black discoloration on the tooth after treatment 55.39% • SDF treatment does not restore natural tooth anatomy and function if it is not followed by a restoration 51.08% • Concern over patient’s satisfaction with SDF treatment 37.41% | • 61.87% had never used SDF to prevent caries • 60.43% had never used SDF to arrest dental caries in primary and 61.51% in permanent teeth. • 34.53% expected that SDF usage would increase a little in the future | Knowledge • Dental specialties Attitude • Dental specialties • Clinical titles |
| Azzawi et al., 2021 [28] | • Knowledge regarding SDF use in dentistry > 60%. • Knowledge of general indications of SDF * Medically compromised children 74% * Behavioral issues and anxiety 73% • Knowledge of specific indications and practices of SDF * Cavitated lesions 65% * Non-aesthetic zone of primary teeth 62% | NR | Barriers: • Not enough knowledge 31% • Not well trained in its use 27% • Aesthetic is poor 28% • Patient satisfaction is lower 35% • Insufficient amount of evidence 22% • Insurance does not cover SDF 25% • SDF is not readily available commercially 49% | Had used/currently use SDF in clinical practice 56.9% | Usage of SDF ↑ • Knowledge on how to use SDF |
| Ezzeldin et al., 2021 [29] | • Awareness of SDF Students 29.6% Dentists 54.6% Specialists 73.6% • Efficacy of SDF Significant proportion of specialists and graduates described: SDF application to be trouble-free, cost effective, reduces the need of GA/sedation to treat pediatric patients, application does not require LA or drilling • Cosmetic outcome of SDF Significant proportion of specialists agreed: Parents’ acceptance of the tooth discoloration Parents non-acceptance of SDF usage on anterior teeth | NR | NR | Use SDF in practice Students 8.6% Dentists 8.8% Specialists 25.0% | NR |
| Alshammari et al., 2021 [30] | Had heard of SDF 62.7% Dentists who answered correctly for all knowledge-based questions 14.89% | NR | Advantages of using SDF • Arresting caries 55.3% SDF disadvantages • Staining the tooth 47.9% • Irritation of pulp 27.7% • Low pH 14.9% | Future implementation of SDF replacing traditional methods 72.0% | No statistically significant difference with knowledge • Gender • Age • Work sector |
| Vollu et al., 2020 [31] | • Had not heard of/did not know about SDF 19.7% • Indication for SDF: Non-compliant patients 75.9% Care in places with no infrastructure 68.5% Patients with no capacity for collaboration 66.7% Primary dentition 75.9% Anterior and posterior teeth 59.3% Posterior teeth 35.2% | NR | Reported barriers among: • Those that did not use SDF Lack of scientific knowledge 58.3% Tooth staining 27.6% • Those who used SDF tooth staining 90.7% Parental acceptance 64.8% | Currently using SDF 13.2% | • Dental specialties Pediatric dentists, showing a 6.76 times higher chance of using SDF than other specialties • Workplace Dentists working at universities had a 2.29 times higher chance of using SDF than those working at private offices |
| Schroë et al., 2022 [17] | Mean overall knowledge items (tooth indication, patient indication, mode of action, toxicity) • Dentists 6.7 • Pediatric dentists 7.4 (out of 15) | Mean score for overall attitude of the respondents • Dentists 14.35 • Pediatric dentists 16.65 | • SDF users Parental acceptance, not knowing the billing code, and the risk of staining clothing/ surfaces • SDF non-users Inadequate knowledge of SDF, parental acceptance, and not knowing the legislation around SDF | Dentists • Current use 16.0% • Future use 50.0% Pediatric dentist • Current use 74% • Future use 74% | NR |
| Abbas et al., 2021 [32] | • Aware of SDF use in dentistry 76.2% • Aware of SDF use in tooth-hypersensitivity treatment 79.3% • Aware of SDF use for the treatment of pediatric dental caries 92.8% • Aware of SDF use in adult dental caries 68.6% • Aware of the advantages of SDF treatment over traditional dental treatment 29.1% • Aware of potential problems associated with the use of SDF 26.5% | • A better alternative treatment for children with behavioral issues 28.7% • A better treatment option for medically fragile patients 33.2% • Alternative treatment for patients with dental anxiety 35.4% • A good treatment option for patients who have recently received chemotherapy or radiation therapy 36.8% • Can be used in patients on bisphosphate treatment 38.6% • Can be used in patients requiring GA • Can be used in patients with microstomia 20.6% • Good treatment option for primary teeth not in the aesthetic zone 59.6% | NR | NR | Professional status (consultant) was found to be significantly associated with knowledge and attitude regarding SDF |
| Mehlawat et al., 2022 [33] | • Had good/very good knowledge of SDF use in dentistry 14.4% • Had good/very good knowledge of the advantages SDF treatment can have over traditional dental treatments 13.6% • Knew SDF is used for treatment of tooth hypersensitivity 9.6% • Knew how SDF is used to treat dental caries among pediatric 24.8% and adult patients 12.0% | • Infected soft dentin must be removed before applying SDF 34.4% • A good treatment for arresting caries when it is not possible to restore all lesions in one appointment 34.4% • Can be used to arrest cavitated lesions in enamel 58.4%, dentin 46.4%, and root-cavity lesions 31.2% • A good treatment alternative among the children with behavioral issues 40.8%, medically fragile patients 41.6%, patients with severe dental anxiety 36%, and patients undergoing or who have recently undergone radiation therapy or chemotherapy 32% | NR | SDF usage in the future Increase a lot 21.6% Increase a little 53.6% Primary teeth • Had never used SDF for treating dental caries 34.4% • Used it often in their offices 10.4% Permanent teeth • Had never used SDF 38.4% • Used it often in their offices 8% | NR |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohammed, I.E.; Shariff, N.; Mohd Hanim, M.F.; Mohd Yusof, M.Y.P.; Md Sabri, B.A.; Md Bohari, N.F.; Venkiteswaran, A. Knowledge, Attitudes and Professional Behavior of Silver Diamine Fluoride among Dental Personnel: A Systematic Review. Children 2022, 9, 1936. https://doi.org/10.3390/children9121936
Mohammed IE, Shariff N, Mohd Hanim MF, Mohd Yusof MYP, Md Sabri BA, Md Bohari NF, Venkiteswaran A. Knowledge, Attitudes and Professional Behavior of Silver Diamine Fluoride among Dental Personnel: A Systematic Review. Children. 2022; 9(12):1936. https://doi.org/10.3390/children9121936
Chicago/Turabian StyleMohammed, Intan Elliayana, Nursharhani Shariff, Muhammad Faiz Mohd Hanim, Mohd Yusmiaidil Putera Mohd Yusof, Budi Aslinie Md Sabri, Nor Faezah Md Bohari, and Annapurny Venkiteswaran. 2022. "Knowledge, Attitudes and Professional Behavior of Silver Diamine Fluoride among Dental Personnel: A Systematic Review" Children 9, no. 12: 1936. https://doi.org/10.3390/children9121936
APA StyleMohammed, I. E., Shariff, N., Mohd Hanim, M. F., Mohd Yusof, M. Y. P., Md Sabri, B. A., Md Bohari, N. F., & Venkiteswaran, A. (2022). Knowledge, Attitudes and Professional Behavior of Silver Diamine Fluoride among Dental Personnel: A Systematic Review. Children, 9(12), 1936. https://doi.org/10.3390/children9121936








