Comparative Study of Refraction between Wave Front-Based Refraction and Autorefraction without and with Cycloplegia in Children and Adolescents
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Procedures
2.3. Spherocylindrical Refraction
2.4. Statistical Analysis
3. Results
3.1. Comparison of Refractive Components with and without Cycloplegia
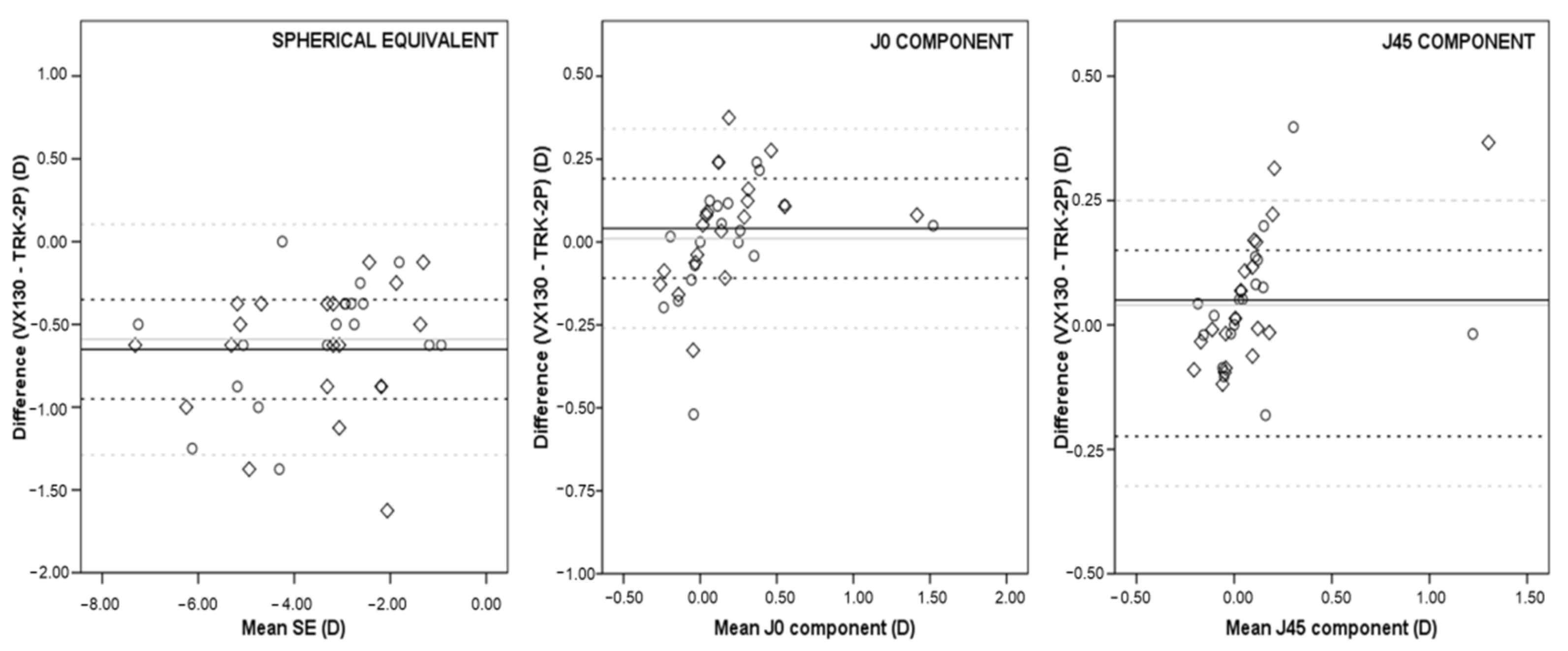
3.2. Comparison between Instruments without Cycloplegia
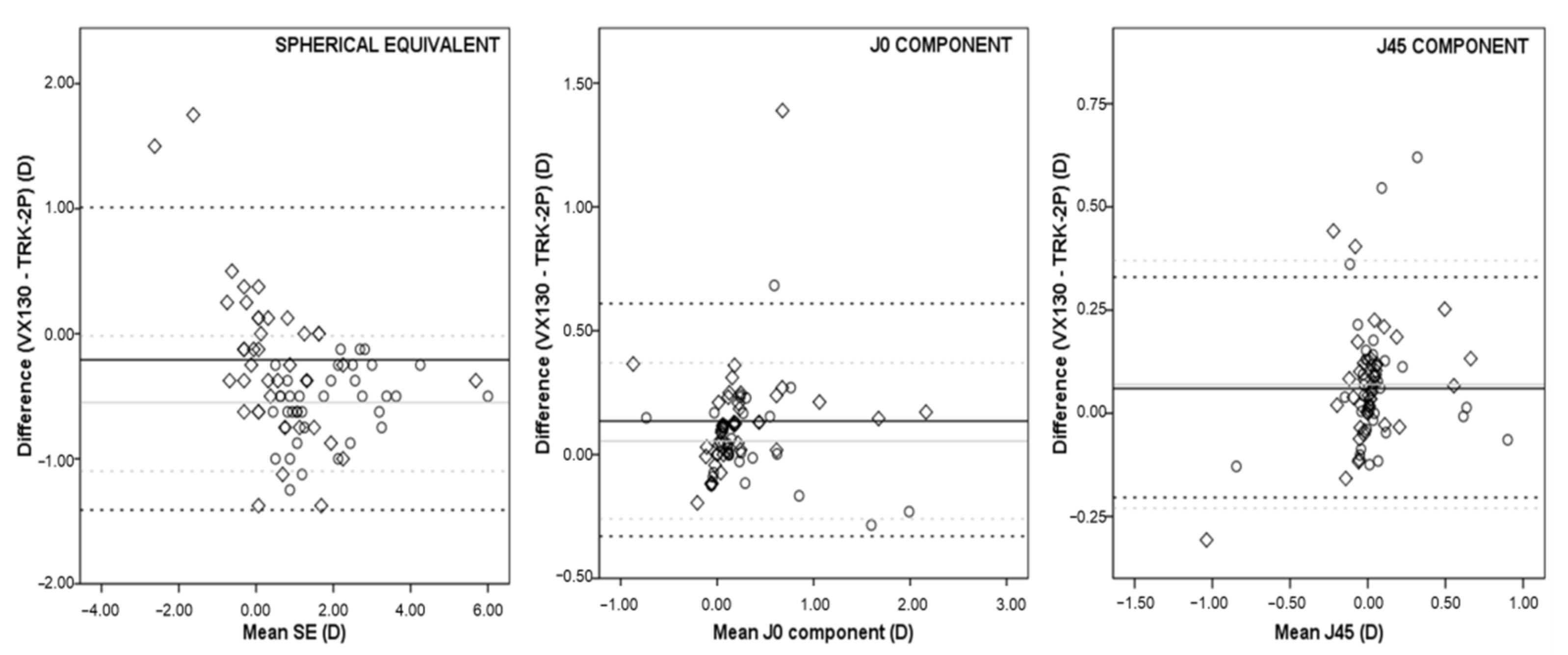
3.3. Comparison between Instruments with Cycloplegia
4. Discussion
4.1. Comparison of Refractive Components with and without Cycloplegia
4.2. Agreement between Instruments without Cycloplegia
4.3. Agreement between Instruments with Cycloplegia
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.; Resnikoff, S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.M.; Verhoeven, V.; Cumberland, P.M.; Bertelsen, G.; Wolfram, C.; Buitendijk, G.H.S.; Hofman, A.; Van Duijn, C.M.; Vingerling, J.R.; Kuijpers, R.W.A.M.; et al. Prevalence of refractive error in Europe: The European Eye Epidemiology (E3) Consortium. Eur. J. Epidemiol. 2015, 30, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.M.; Bertelsen, G.; Cumberland, P.; Wolfram, C.; Verhoeven, V.; Anastasopoulos, E.; Buitendijk, G.H.; Cougnard-Grégoire, A.; Creuzot-Garcher, C.; Erke, M.G.; et al. Increasing prevalence of myopia in Europe and the impact of education. Ophthalmology 2015, 122, 1489–1497. [Google Scholar] [CrossRef]
- Packwood, E.A.; Cruz, O.A.; Rychwalski, P.J.; Keech, R.V. The psychosocial effects of amblyopia study. J. AAPOS 1999, 3, 15–17. [Google Scholar] [CrossRef]
- Williams, W.R.; Latif, A.H.; Hannington, L.; Watkins, D.R. Hyperopia and educational attainment in a primary school cohort. Arch. Dis. Child. 2005, 90, 150–153. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.Y.; Ferreira, A.; Hughes, R.; Carter, G.; Mitchell, P. Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: An evidence based systematic review. Am. J. Ophthalmol. 2014, 157, 9–25.e12. [Google Scholar] [CrossRef]
- Flitcroft, D.L. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog. Retin. Eye Res. 2012, 31, 622–660. [Google Scholar] [CrossRef]
- Buch, H.; Vinding, T.; de la Cour, M.D.; Appleyard, M.; Jensen, G.B.; Nielsen, N.V. Prevalence and causes of visual impairment and blindness among 9980 Scandinavian adults. Ophthalmology 2004, 111, 53–61. [Google Scholar] [CrossRef]
- Franklin, A. Subjective refraction: Principles and techniques for the correction of spherical ametropia. In Clinical Optics and Refraction: A Guide for Optometrist, Contact Lens Opticians and Dispensing Opticians; Elsevier: Philadelphia, PA, USA, 2007. [Google Scholar]
- Hernández-Moreno, L.; Vallelado-Alvarez, A.; Martin, R. Repeatability of ARK-30 in a pediatric population. Indian J. Ophthalmol. 2018, 66, 1262–1267. [Google Scholar]
- Harvey, E.M.; Miller, J.M.; Wagner, L.K.; Dobson, V. Reproducibility and accuracy of measurements with a hand held autorefractor in children. Br. J. Ophthalmol. 1997, 81, 941–948. [Google Scholar] [CrossRef]
- Tuncer, I.; Zengin, M.O.; Karahan, E. Comparison of the Retinomax hand-held autorefractor versus table-top autorefractor and retinoscopy. Int. J. Ophthalmol. 2014, 7, 491–495. [Google Scholar]
- Choong, Y.F.; Chen, A.H.; Goh, P.P. A comparison of autorefraction and subjective refraction with and without cycloplegia in primary school children. Am. J. Ophthalmol. 2006, 142, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Kara, C.; Petriçli, İ.S. Inability of Open-Field Autorefraction to Eliminate Accommodation in Preschoolers. J. Pediatr. Ophthalmol. Strabismus 2017, 54, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Rotsos, T.; Grigoriou, D.; Kokkolaki, A.; Manios, N. A comparison of manifest refractions, cycloplegic refractions and retinoscopy on the RMA-3000 autorefractometer in children aged 3 to 15 years. Clin. Ophthalmol. 2009, 3, 429–431. [Google Scholar] [CrossRef] [PubMed]
- Krishnacharya, P.S. Study on accommodation by autorefraction and dynamic refraction in children. J. Optom. 2014, 7, 193–202. [Google Scholar] [CrossRef]
- Mimouni, M.; Zoller, L.; Horowitz, J.; Wygnanski-Jaffe, T.; Morad, Y.; Mezer, E. Cycloplegic autorefraction in young adults: Is it mandatory? Graefe’s Arch. Clin. Exp. Ophthalmol. 2016, 254, 395–398. [Google Scholar] [CrossRef]
- Saxena, R.; Vashist, P.; Tandon, R.; Pandey, R.M.; Bhardawaj, A.; Menon, V.; Mani, K. Prevalence of myopia and its risk factors in urban school children in Delhi: The North India Myopia Study (NIM Study). PLoS ONE 2015, 10, e0117349. [Google Scholar] [CrossRef]
- Fotedar, R.; Rochtchina, E.; Morgan, I.; Wang, J.J.; Mitchell, P.; Rose, K.A. Necessity of cycloplegia for assessing refractive error in 12-year-old children: A population-based study. Am. J. Ophthalmol. 2007, 144, 307–309. [Google Scholar] [CrossRef]
- Thibos, L.N.; Wheeler, W.; Horner, D. Power vectors: An application of Fourier analysis to the description and statistical analysis of refractive error. Optom. Vis. Sci. 1997, 474, 367–375. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- McAlinden, C.; Khadka, J.; Pesudovs, K. Statistical methods for conducting agreement (comparison of clinical tests) and precision (repeteability or repfroducibility) studies in optometry and ophthalmology. Ophthalmic Physiol. Opt. 2011, 31, 330–338. [Google Scholar] [CrossRef]
- Supuk, E.; Alderson, A.; Davey, C.J.; Green, C.; Litvin, N.; Scally, A.J.; Elliott, D.B. Dizziness, but not falls rate, improves after routine cataract surgery: The role of refractive and spectacle changes. Ophthalmic Physiol. Opt. 2016, 36, 183–190. [Google Scholar] [CrossRef]
- Shetty, N.; Dadachanji, Z.; Narasimhan, R.; Kundu, G.; Khamar, P.; Ahuja, P.; Kumar, V.; Kumar, V.; Shetty, R.; Nuijts, R.M.; et al. Status of residual refractive error, ocular aberrations, and accommodation after myopic LASIK, SMILE, and TransPRK. J. Refract. Surg. 2019, 35, 624–631. [Google Scholar] [CrossRef]
- Chen, J.; Xie, A.; Hou, L.; Su, Y.; Lu, F.; Thorn, F. Cycloplegic and noncycloplegic refractions of Chinese neonatal infants. Investig. Ophthalmol. Vis. Sci. 2011, 52, 2456–2461. [Google Scholar] [CrossRef]
- Smith, T.S.T.; Frick, K.D.; Holden, B.A.; Fricke, T.R.; Naidoo, K.S. Potential lost productivity resulting from the global burden of uncorrected refractive error. Bull. World Health Organ. 2009, 87, 431–437. [Google Scholar] [CrossRef]
- Resnikoff, S.; Pascolini, D.; Mariotti, S.P.; Pokharel, G.P. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull. World Health Organ. 2008, 86, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Suryakumar, R.; Bobier, W.R. The manifestation of noncycloplegic refractive state in pre-school children is dependent on autorefractor design. Optom. Vis. Sci. 2007, 80, 578–586. [Google Scholar] [CrossRef] [PubMed]
- Wesemann, W.; Dick, B. Accuracy and accommodation capability of a handheld autorefractor. J. Cataract. Refract. Surg. 2000, 26, 62–70. [Google Scholar] [CrossRef]
- Morgan, I.G.; Ohno-Matsui, K.; Saw, S.M. Myopia. Lancet 2012, 379, 1739–1748. [Google Scholar] [CrossRef]
- Mutti, D.O.; Mitchell, G.L.; Moeschberger, M.L.; Jones, L.A.; Zadnik, K. Parental myopia, near work, school achievement, and children’s refractive error. Investig. Ophthalmol. Vis. Sci. 2001, 43, 3633–3640. [Google Scholar]
- Wang, B.; Ciuffreda, K.J. Depth-of-focus of the human eye: Theory and clinical implications. Surv. Opththalmol. 2006, 51, 75–85. [Google Scholar] [CrossRef]
- Millodot, M. The effect of refractive error on the accommodative response gradient: A summary and update. Ophthalmic Physiol. Opt. 2015, 35, 607–612. [Google Scholar] [CrossRef]
- Shneor, E.; Millodot, M.; Avraham, O.; Amar, S.; Gordon-Shaag, A. Clinical evaluation of the L80 autorefractometer. Clin. Exp. Optom. 2012, 95, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Salmon, T.O.; West, R.W.; Gasser, W.; Kenmore, A.T. Measurement of refractive errors in young myopes using the COAS Shack-Hartmann aberrometer. Optom. Vis. Sci. 2003, 80, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Sankaridurg, P.; He, X.; Naduvilath, T.; Lv, M.; Ho, A.; Smith III, E.; Erickson, P.; Zhu, J.; Zou, H.; Xu, X. Comparison of noncycloplegic and cycloplegic autorefraction in categorizing refractive error data in children. Acta Ophthalmol. 2017, 95, e633–e640. [Google Scholar] [CrossRef]
- Hashemi, H.; Khabazkhoob, M.; Asharlous, A.; Yekta, A.; Emamiam, M.H. Overestimation of hyperopia with autorefraction compared with retinoscopy under cycloplegia in school-age children. Br. J. Ophthalmol. 2018, 102, 1717–1722. [Google Scholar] [CrossRef] [PubMed]
- Rajavy, R.; Sabbaghi, H.; Baghini, A.S.; Yaseri, M.; Sheibani, K.; Norouzi, G. Accuracy and repeatability of refractive error measurements by photorefractometry. J. Ophthalmic Vis. Res. 2015, 10, 221–228. [Google Scholar]
- Yassa, E.T.; Únlú, C. Comparison of autorefraction and photorefraction with and without cycloplegia using 1% tropicamide in preschool children. J. Ophthalmol. 2019, 2019, 1487013. [Google Scholar] [CrossRef]
- Saini, V.; Raina, U.K.; Gupta, A.; Goyal, J.L.; Anjum, R.; Saini, P.; Gupta, S.K.; Sharma, P. Comparison of Plusoptix S12R photoscreener with cycloplegic retinoscopy and autorefraction in pediatric age group. Indian J. Ophthalmol. 2019, 67, 1555–1559. [Google Scholar] [CrossRef]
- Payerols, A.; Eliaou, C.; Trezeguet, V.; Villain, M.; Daien, V. Accuracy of Plusoptix a09 distance refraction in pediatric myopia and hyperopia. BMC Ophthalmol. 2016, 16, 72. [Google Scholar] [CrossRef]
- Prabakaran, S.; Dirani, M.; Chia, A.; Gazzard, G.; Fan, Q.; Leo, S.-W.; Ling, Y.; Eong, K.-G.A.; Wong, T.-Y.; Saw, S.-M. Cycloplegic refraction in preschool children: Comparisons between the hand-held autorefractor, table-mounted autorefractor and retinoscopy. Ophthalmic Physiol. Opt. 2009, 29, 422–426. [Google Scholar] [CrossRef] [PubMed]
- Oral, Y.; Gunaydin, N.; Ozgur, O.; Arsan, A.K.; Oskan, S. A comparison of different autorefractors with retinoscopy in children. J. Pediatr. Ophthalmol. Strabismus 2012, 49, 370–377. [Google Scholar] [CrossRef]
- Guha, S.; Shah, S.; Shah, K.; Hurakadli, P.; Majee, D.; Gandhi, S. A comparison of cycloplegia autorefraction and retinoscopy in Indian children. Clin. Exp. Optom. 2017, 100, 73–78. [Google Scholar] [CrossRef]
- Wilson, L.B.; Melia, M.; Kraker, R.T.; VanderVeen, D.K.; Hutchinson, A.K.; Pineles, S.L.; Galvin, J.A.; Lambert, S.R. Accuracy of autorefraction in children: A report by the American Academy of Ophthalmology. Ophthalmology 2020, 127, 1259–1267. [Google Scholar] [CrossRef] [PubMed]
- McCullough, S.J.; Little, J.; Breslin, K.M.; Saunders, K.J. Comparison of refractive error measures by the IRX3 aberrometer and autorefraction. Optom. Vis. Sci. 2014, 91, 1183–1190. [Google Scholar] [CrossRef] [PubMed]
| Refractive Error | Parameters (Mean ± SD) | Pre-Cycloplegia | Post-Cycloplegia | p |
|---|---|---|---|---|
| Myopia (n = 20) | Sphere (D) | −3.04 ± 1.71 | −2.88 ± 1.66 | 0.137 |
| Cylinder (D) | −0.55 ± 0.74 | −0.60 ± 0.81 | 0.163 | |
| SE (D) | −3.32 ± 1.68 | −3.18 ± 1.59 | 0.209 | |
| J0 (D) | 0.15 ± 0.34 | 0.18 ± 0.36 | 0.098 | |
| J45 (D) | 0.07 ± 0.27 | 0.08 ± 0.30 | 0.541 | |
| Hyperopia (n = 40) | Sphere (D) | 0.86 ± 1.79 | 2.43 ± 1.54 | <0.001 |
| Cylinder (D) | −0.57 ± 0.96 | −0.65 ± 0.96 | 0.074 | |
| SE (D) | 0.58 ± 1.49 | 2.10 ± 1.18 | <0.001 | |
| J0 (D) | 0.16 ± 0.48 | 0.22 ± 0.47 | 0.002 | |
| J45 (D) | −0.23 ± 0.23 | 0.01 ± 0.25 | 0.005 |
| Refractive Error | Parameters (Mean ± SD) | Pre-Cycloplegia | Post-Cyclolegia | p |
|---|---|---|---|---|
| Myopia (n = 20) | Sphere (D) | −3.54 ± 1.74 | −3.37 ± 1.77 | 0.019 |
| Cylinder (D) | −0.85 ± 0.82 | −0.82 ± 0.79 | 0.420 | |
| SE (D) | −3.96 ± 1.73 | −3.78 ± 1.72 | 0.012 | |
| J0 (D) | 0.19 ± 0.41 | 0.19 ± 0.42 | 0.967 | |
| J45 (D) | 0.12 ± 0.36 | 0.12 ± 0.31 | 0.905 | |
| Hyperopia (n = 40) | Sphere (D) | 0.82 ± 1.47 | 1.94 ± 1.57 | <0.001 |
| Cylinder (D) | −0.88 ± 1.02 | −0.79 ± 0.87 | 0.014 | |
| SE (D) | 0.37 ± 1.18 | 1.54 ± 1.27 | <0.001 | |
| J0 (D) | 0.30 ± 0.54 | 0.28 ± 0.43 | 0.407 | |
| J45 (D) | 0.04 ± 0.28 | 0.09 ± 0.27 | 0.009 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calvo-Maroto, A.M.; Llorente-González, S.; Bezunartea-Bezunartea, J.; Hurtado-Ceña, F.J.; Berrozpe-Villabona, C.; Bilbao-Malavé, V.; Piñero, D.P.; Barrio-Barrio, J.; Recalde-Maestre, S. Comparative Study of Refraction between Wave Front-Based Refraction and Autorefraction without and with Cycloplegia in Children and Adolescents. Children 2022, 9, 88. https://doi.org/10.3390/children9010088
Calvo-Maroto AM, Llorente-González S, Bezunartea-Bezunartea J, Hurtado-Ceña FJ, Berrozpe-Villabona C, Bilbao-Malavé V, Piñero DP, Barrio-Barrio J, Recalde-Maestre S. Comparative Study of Refraction between Wave Front-Based Refraction and Autorefraction without and with Cycloplegia in Children and Adolescents. Children. 2022; 9(1):88. https://doi.org/10.3390/children9010088
Chicago/Turabian StyleCalvo-Maroto, Ana M, Sara Llorente-González, Jaione Bezunartea-Bezunartea, Francisco Javier Hurtado-Ceña, Clara Berrozpe-Villabona, Valentina Bilbao-Malavé, David P Piñero, Jesús Barrio-Barrio, and Sergio Recalde-Maestre. 2022. "Comparative Study of Refraction between Wave Front-Based Refraction and Autorefraction without and with Cycloplegia in Children and Adolescents" Children 9, no. 1: 88. https://doi.org/10.3390/children9010088
APA StyleCalvo-Maroto, A. M., Llorente-González, S., Bezunartea-Bezunartea, J., Hurtado-Ceña, F. J., Berrozpe-Villabona, C., Bilbao-Malavé, V., Piñero, D. P., Barrio-Barrio, J., & Recalde-Maestre, S. (2022). Comparative Study of Refraction between Wave Front-Based Refraction and Autorefraction without and with Cycloplegia in Children and Adolescents. Children, 9(1), 88. https://doi.org/10.3390/children9010088







