Clinical Characteristics and Underlying Factors Related to Recovery from Severe Pneumonia in Under-Five Children with or without Malnutrition Treated at Health Care Facilities in Bangladesh
Abstract
1. Introduction
2. Materials and Methods
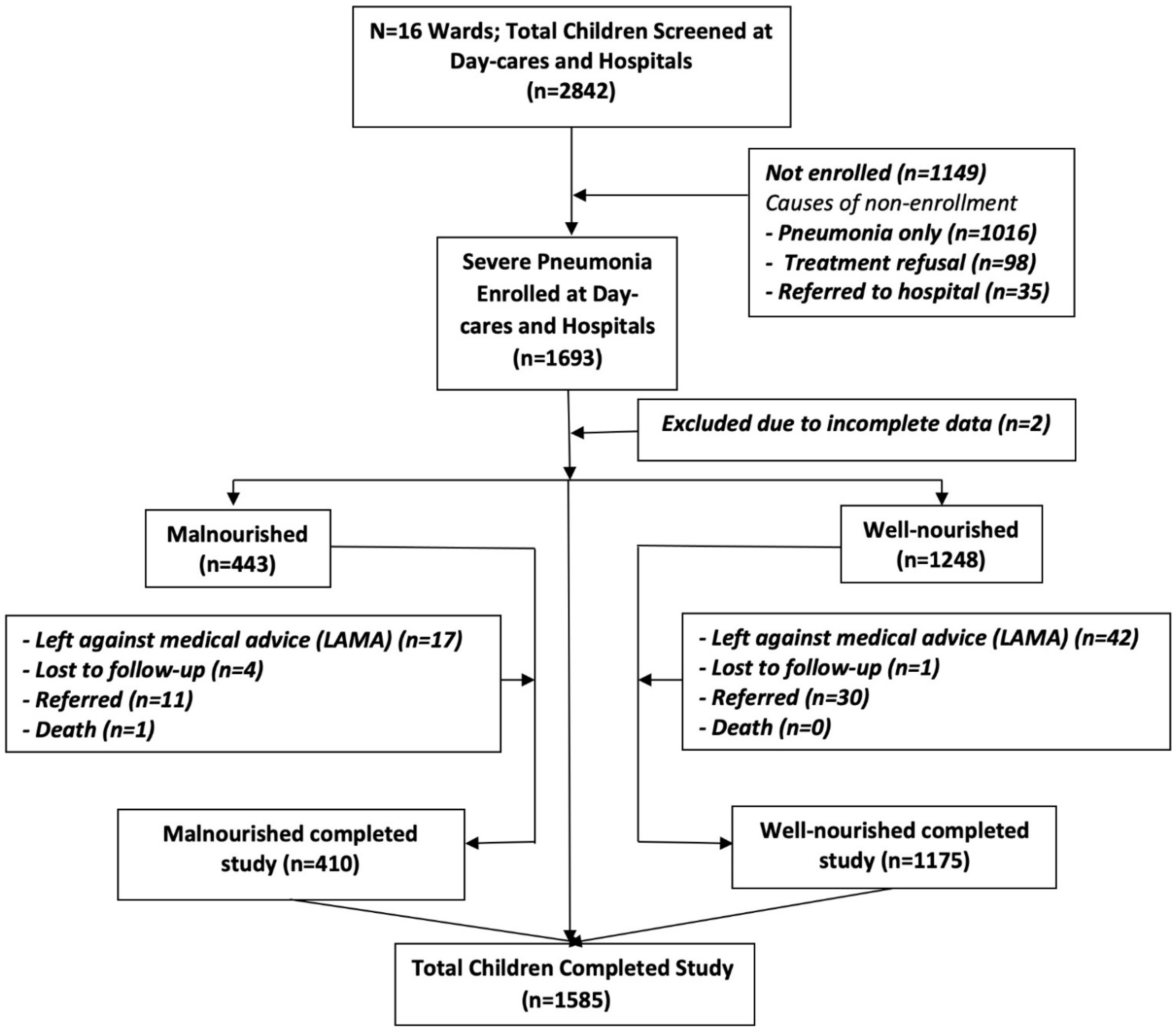
2.1. Study Population
2.2. Study Areas
2.3. Ethical Clearance
2.4. Study Procedures
2.5. Sample Size Calculations
2.6. Operational Definitions
2.7. Statistical Analysis
3. Results
4. Discussion
Limitations and Strengths of This Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations Children’s Fund (UNICEF). Childhood Pneumonia: Everything you Need to Know|UNICEF. 2020. Available online: https://www.unicef.org/stories/childhood-pneumonia-explained (accessed on 27 May 2021).
- Ibrahim, M.K.; Zambruni, M.; Melby, C.L.; Melby, P.C. Impact of childhood malnutrition on host defense and infection. Clin. Microbiol. Rev. 2017, 30, 919–971. [Google Scholar] [CrossRef]
- Black, R.E.; Allen, L.H.; Bhutta, Z.A.; Caulfield, L.E.; Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar] [CrossRef]
- Chisti, M.J.; Tebruegge, M.; La Vincente, S.; Graham, S.M.; Duke, T. Pneumonia in severely malnourished children in developing countries—mortality risk, aetiology and validity of WHO clinical signs: A systematic review. Trop. Med. Int. Health 2009, 14, 1173–1189. [Google Scholar] [CrossRef]
- Schwinger, C.; Golden, M.H.; Grellety, E.; Roberfroid, D.; Guesdon, B. Severe acute malnutrition and mortality in children in the community: Comparison of indicators in a multi-country pooled analysis. PLoS ONE 2019, 14, e0219745. [Google Scholar] [CrossRef] [PubMed]
- United Nations Children’s Fund (UNICEF). World Health Organization, International Bank for Reconstruction and Development/The World Bank. Levels and Trends in Child Malnutrition: Key Findings of the 2019 Edition of the Joint Child Malnutrition Estimates; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- World Health Organization (WHO). Nutrition. Malnutrition is a World Health Crisis. World Food Day. 2019. Available online: https://www.who.int/nutrition/topics/world-food-day-2019-malnutrition-world-health-crisis/en/ (accessed on 22 May 2021).
- Das, J.K.; Salam, R.A. Addressing childhood undernutrition and development through education and lipid-based supplements. Lancet Glob. Health 2019, 7, e1160–e1161. [Google Scholar] [CrossRef]
- United Nations. Sustainable Development Goals (SDGs). Goal 3: Ensure Healthy Lives and Promote Well-Being for All at All Ages. Goal 3 Targets. Available online: https://www.un.org/sustainabledevelopment/health/ (accessed on 1 May 2021).
- United Nations Children’s Fund (UNICEF). One Child Dies of Pneumonia Every 39 Seconds, Agencies Warn. Pneumonia—A Preventable Disease—Kills More Children than any Other Infection. One Child Dies of Pneumonia Every 39 Seconds, Agencies warn. 2019. Available online: https://www.unicef.org/press-releases/one-child-dies-pneumonia-every-39-seconds-agencies-warn (accessed on 9 January 2021).
- Global Nutrition Report 2020. Country Nutrition Profiles. Available online: https://globalnutritionreport.org/resources/nutrition-profiles/asia/southern-asia/bangladesh/ (accessed on 27 May 2021).
- Islam, M.R.; Rahman, M.S.; Rahman, M.M.; Nomura, S.; de Silva, A.; Lanerolle, P.; Jung, J.; Rahman, M.M. Reducing childhood malnutrition in Bangladesh: The importance of addressing socio-economic inequalities. Public Health Nutr. 2019, 23, 72–82. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Development Initiatives, 2018 Global Nutrition Report: Shining a Light to Spur Action on Nutrition; Development Initiatives: Bristol, UK, 2018; Available online: https://www.who.int/nutrition/globalnutritionreport/2018_Global_Nutrition_Report.pdf?ua=1 (accessed on 25 May 2021).
- Chisti, M.J.; Salam, M.A.; Ashraf, H.; Faruque, A.S.G.; Bardhan, P.K.; Shahid, A.S.M.S.B.; Shahunja, K.M.; Das, S.K.; Ahmed, T. Predictors and outcome of hypoxemia in severely malnourished children under five with pneumonia: A case control design. PLoS ONE 2013, 8, e51376. [Google Scholar] [CrossRef] [PubMed]
- Agweyu, A.; Lilford, R.J.; English, M.; for the Clinical Information Network Author Group. Appropriateness of clinical severity classification of new WHO childhood pneumonia guidance: A multi-hospital, retrospective, cohort study. Lancet Glob. Health 2018, 6, e74–e83. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Children: Reducing Mortality. 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality (accessed on 14 February 2021).
- McAllister, D.A.; Liu, L.; Shi, T.; Chu, Y.; Reed, C.; Burrows, J.; Adeloye, D.; Rudan, I.; Black, R.E.; Campbell, H.; et al. Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: A systematic analysis. Lancet Glob. Health 2019, 7, e47–e57. [Google Scholar] [CrossRef]
- Walson, J.L.; Berkley, J.A. The impact of malnutrition on childhood infections. Curr Opin Infect. Dis. 2018, 31, 231–236. [Google Scholar] [CrossRef]
- World Health Organization (WHO). United Nations Children’s Fund (UNICEF) & United States Agency for International Development (USAID). Improving Nutrition Outcomes with Better Water, Sanitation and Hygiene: Practical Solutions for policies and Programmes. 2015. Available online: https://www.unicef.org/media/files/IntegratingWASHandNut_WHO_UNICEF_USAID_Nov2015.pdf (accessed on 11 March 2021).
- World Health Organization (WHO). Revised WHO Classification and Treatment of Childhood Pneumonia at Health Facilities: Evidence Summaries. 2014. Available online: https://apps.who.int/iris/bitstream/handle/10665/137319/9789241507813_eng.pdf?sequence=1 (accessed on 14 February 2021).
- Nolan, T.; Angos, P.; Cunha, A.J.; Muhe, L.; Qazi, S.; Simoes, E.A.; Tamburlini, G.; Weber, M.; Pierce, N.F. Quality of hospital care for seriously ill children in less-developed countries. Lancet 2001, 357, 106–110. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Management of the Child with a Serious Infection or Severe Malnutrition. Guidelines for Care at the First-Referral Level in Developing Countries. WHO/FCH/CAH/00.1. 2000. Available online: https://apps.who.int/iris/bitstream/handle/10665/42335/WHO_FCH_CAH_00.1.pdf;jsessionid=BD9571B2F2D76061AF0A9780C995B336?sequence=1 (accessed on 18 February 2021).
- Ashraf, H.; Ahmed, T.; Hossain, M.I.; Alam, N.H.; Mahmud, R.; Kamal, S.M.; Salam, M.A.; Fuchs, G.J. Day-care management of children with severe malnutrition in an urban health clinic in Dhaka, Bangladesh. J. Trop. Pediatr. 2007, 53, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, H.; Alam, N.H.; Sultana, M.; Jahan, S.A.; Begum, N.; Farzana, S.; Chisti, M.J.; Kamal, M.; Shamsuzzaman, A.; Ahmed, T.; et al. Day clinic vs. hospital care of pneumonia and severe malnutrition in children under five: A randomised trial. Trop. Med. Int. Health 2019, 24, 922–931. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, H.; Jahan, S.A.; Alam, N.H.; Mahmud, R.; Kamal, S.M.; Salam, M.A.; Gyr, N. Day-care management of severe and very severe pneumonia, without associated co-morbidities such as severe malnutrition, in an urban health clinic in Dhaka, Bangladesh. Arch. Dis Child. 2008, 93, 490–494. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Global Database on Child Growth and Malnutrition. 2020. Available online: https://www.who.int/nutgrowthdb/about/introduction/en/index5.html (accessed on 30 January 2021).
- World Health Organization (WHO) 2014. IMCI Integrated Management of Childhood Illness. Available online: https://apps.who.int/iris/bitstream/handle/10665/104772/9789241506823_Module-3_eng.pdf?sequence=5&isAllowed=y (accessed on 3 September 2021).
- World Health Organization (WHO). Pocket Book of Hospital care for Children: Guidelines for the Management of Common Childhood Illness, 2nd ed.; World Health Organization: Geneva, Switzerland, 2013; Available online: https://apps.who.int/iris/handle/10665/81170 (accessed on 23 August 2021).
- Pneumonia Etiology Research for Child Health (PERCH) Study Group. Causes of severe pneumonia requiring hospital admission in children without HIV infection from Africa and Asia: The PERCH multi-country case-control study. Lancet 2019, 394, 757–779. [Google Scholar] [CrossRef]
- Ashraf, H.; Ahmed, S.; Fuchs, G.J.; Mahalanabis, D. Persistent diarrhoea: Associated infection and response to a low lactose diet. J. Trop. Pediatr. 2002, 48, 142–148. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Willson, D.F.; Landrigan, C.P.; Horn, S.D.; Smout, R.J. Complications in infants hospitalized for bronchiolitis or respiratory syncytial virus pneumonia. J. Pediatr. 2003, 143 (Suppl. 5), S142–S149. [Google Scholar] [CrossRef]
- Victora, C.G.; Wagstaff, A.; Schellenberg, J.A.; Gwatkin, D.; Claeson, M.; Habicht, J.P. Applying an equity lens to child health and mortality: More of the same is not enough. Lancet 2003, 362, 233–241. [Google Scholar] [CrossRef]
- Patel, K.A.; Langare, S.D.; Naik, J.D.; Rajderkar, S.S. Gender inequality and bio-social factors in nutritional status among under five children attending anganwadis in an urban slum of a town in Western Maharashtra, India. J. Res. Med. Sci. 2013, 18, 341–345. [Google Scholar]
- Nankinga, O.; Kwagala, B.; Walakira, E.J. Maternal employment and child nutritional status in Uganda. PLoS ONE 2019, 14, e0226720. [Google Scholar] [CrossRef] [PubMed]
- Department of Equity Poverty and Social Determinants of Health (EIP/EQH). A WHO Report on Inequities in Maternal and Child. Health Mozambique; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Jones, A.D.; Cruz Agudo, Y.; Galway, L.; Bentley, J.; Pinstrup-Andersen, P. Heavy agricultural workloads and low crop diversity are strong barriers to improving child feeding practices in the Bolivian Andes. Soc. Sci. Med. 2012, 75, 1673–1684. [Google Scholar] [CrossRef] [PubMed]
- Negash, C.; Whiting, S.J.; Henry, C.J.; Belachew, T.; Hailemariam, T.G. Association between maternal and child nutritional status in Hula, rural southern Ethiopia: A cross sectional study. PLoS ONE 2015, 10, e0142301. [Google Scholar] [CrossRef] [PubMed]
- Adekunle, L. The effect of family structure on a sample of malnourished urban Nigerian children. Food Nutr. Bull. 2005, 26, 230–233. [Google Scholar] [CrossRef] [PubMed]
- Bangladesh Bureau of Statistics (BBS), 2017. Preliminary Report on Household Income and Expenditure Survey 2016. Available online: https://catalog.ihsn.org/index.php/catalog/7399/related-materials (accessed on 17 May 2021).
- Tette, E.M.A.; Sifah, E.K.; Nartey, E.T. Factors affecting malnutrition in children and the uptake of interventions to prevent the condition. BMC Pediatr. 2015, 15, 189. [Google Scholar] [CrossRef]
- Tette, E.M.A.; Sifah, E.K.; Nartey, E.T.; Nuro-Ameyaw, P.; Tete-Donkor, P.; Biritwum, R.B. Maternal profiles and social determinants of malnutrition and the MDGs: What have we learnt? BMC Public Health 2016, 16, 214. [Google Scholar] [CrossRef] [PubMed]
- Morgan, G. What, if any, is the effect of malnutrition on immunological competence? Lancet 1997, 349, 1693–1695. [Google Scholar] [CrossRef]
- Chisti, M.J.; Ahmed, T.; Faruque, A.S.; Abdus Salam, M. Clinical and laboratory features of radiologic pneumonia in severely malnourished infants attending an urban diarrhea treatment center in Bangladesh. Pediatr. Infect. Dis. J. 2010, 29, 174–177. [Google Scholar] [CrossRef] [PubMed]
- Chisti, M.J.; Salam, M.A.; Ashraf, H.; Faruque, A.S.G.; Bardhan, P.K.; Das, S.K.; Shahunja, K.M.; Shahid, A.S.M.S.B.; Ahmed, T. Clinical signs of radiologic pneumonia in under-five hypokalemic diarrheal children admitted to an urban hospital in Bangladesh. PLoS ONE 2013, 8, e71911. [Google Scholar] [CrossRef] [PubMed]
- Falade, A.G.; Tschäppeler, H.; Greenwood, B.M.; Mulholland, E.K. Use of simple clinical signs to predict pneumonia in young Gambian children: The influence of malnutrition. Bull. World Health Organ. 1995, 73, 299–304. [Google Scholar] [PubMed]
- Jones, K.D.; Berkley, J.A. Severe acute malnutrition and infection. Paediatr. Int. Child. Health 2014, 34 (Suppl. 1), S1–S29. [Google Scholar] [CrossRef] [PubMed]
- Bourke, C.D.; Berkley, J.A.; Prendergast, A.J. Immune dysfunction as a cause and consequence of malnutrition. Trends Immunol. 2016, 37, 386–398. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Total (n = 1693) n (%) | Malnourished (n = 443) n (%) | Well-Nourished (n = 1248) n (%) | p-Value |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Child’s age in months | ||||
| Less than 12 months (Mean ± SD) 6.04 ± 1.46 | 1039 (61.4) | 221 (21.3) | 817 (78.7) | <0.001 |
| ≥12 months (Mean ± SD) 22.32 ± 9.58 | 654 (38.6) | 222 (34.0) | 431 (66.0) | |
| Sex of the children (male) | 1066 (63.0) | 291 (65.7) | 775 (62.1) | 0.215 |
| Maternal age in years, Mean (SD) | 24.7 (5.0) | 25.0 (5.3) | 24.6 (4.9) | 0.254 |
| Paternal age in years, Mean (SD) | 31.9 (6.4) | 32.1 (6.9) | 31.8 (6.2) | 0.351 |
| Maternal education (years of schooling) | ||||
| Illiterate (0 year); n (%) | 190 (11.2) | 81 (18.3) | 109 (8.7) | <0.001 |
| Primary (1–5 years); n (%) | 522 (30.8) | 149 (33.6) | 373 (29.9) | |
| Secondary (6–10 years); n (%) | 773 (45.7) | 181 (40.9) | 591 (47.4) | |
| Higher (≥11 years); n (%) | 207 (12.2) | 32 (7.2) | 174 (14.0) | |
| Paternal education (years of schooling) | ||||
| Illiterate (0 year); n (%) | 252 (14.9) | 91 (20.7) | 161 (12.9) | <0.001 |
| Primary (1–5 years); n (%) | 483 (28.5) | 143 (32.6) | 340 (27.3) | |
| Secondary (6–10 years); n (%) | 677 (40.0) | 160 (36.5) | 516 (41.5) | |
| Higher (≥11 years); n (%) | 274 (16.2) | 45 (10.3) | 228 (18.3) | |
| Maternal occupation | ||||
| Housewife | 1483 (87.6) | 371 (83.8) | 1110 (89.0) | 0.004 |
| Other (formal and informal) | 209 (12.3) | 72 (16.3) | 137 (11.0) | |
| Paternal occupation | ||||
| Day labor, Garment/Industry worker | 326 (19.3) | 102 (23.2) | 223 (17.9) | 0.006 |
| Skilled worker, Office Non-executive, Office executive | 455 (26.9) | 100 (22.8) | 355 (28.5) | |
| Business/Rickshaw/Push cart puller/Taxi/Bus/Tempo driver | 735 (43.4) | 194 (44.2) | 541 (43.4) | |
| Other (informal) | 169 (10.0) | 42 (9.6) | 126 (10.1) | |
| Number of family/household members | ||||
| <5 members; n (%) | 863 (51.0) | 243 (54.9) | 620 (49.7) | 0.063 |
| ≥5 members; n (%) | 829 (49.0) | 200 (45.2) | 627 (50.3) | |
| Number of siblings | ||||
| One or no; n (%) | 672 (39.7) | 169 (38.2) | 502 (40.3) | 0.586 |
| Two; n (%) | 665 (39.3) | 174 (39.3) | 490 (39.3) | |
| Three or more; n (%) | 355 (21.0) | 100 (22.6) | 255 (20.5) | |
| Household income (USD/month), Median (IQR) | USD 223 (165, 353) | USD 188 (141, 270) | USD 235 (165, 353) | <0.001 ¶ |
| Wealth tertiles | ||||
| Poor; n (%) | 565 (33.4) | 184 (41.5) | 380 (30.5) | <0.001 |
| Middle; n (%) | 597 (35.8) | 150 (33.9) | 447 (35.9) | |
| Rich; n (%) | 530 (31.3) | 109 (24.6) | 420 (33.7) | |
| Presence of clinical characteristics at recruitment in the health care facilities | ||||
| Rapid breathing; n (%) | 1682 (99.4) | 440 (99.3) | 1240 (99.4) | 0.935 |
| Lower chest wall in drawing; n (%) | 1651 (97.5) | 432 (97.5) | 1217 (97.5) | 0.999 |
| Hypoxemia (SPO2 < 90%); n (%) | 179 (10.6) | 39 (9.1) | 140 (11.6) | 0.168 |
| Nasal discharge; n (%) | 1470 (86.8) | 377 (85.1) | 1091 (87.4) | 0.215 |
| Fever; n (%) | 1436 (84.8) | 371 (83.8) | 1064 (85.3) | 0.446 |
| Resolution on Day Six after Admission into the Health Care Facilities | Malnourished Children n (%) | Well-Nourished Children n (%) | p-Value |
|---|---|---|---|
| No rapid breathing | 365 (86.5) N = 422 | 1077 (90.2) N = 1194 | 0.035 |
| No lower chest wall in-drawing | 382 (90.5) N = 422 | 1121 (93.9) N = 1194 | 0.019 |
| No hypoxemia | 404 (99.5) N = 406 | 1162 (99.5) N = 1168 | 1.000 |
| No nasal discharge | 319 (75.6) N = 422 | 874 (73.2) N = 1194 | 0.335 |
| No fever | 389 (92.2) N = 422 | 1137 (95.2) N = 1194 | 0.021 |
| Variables | Rapid Breathing (R² = 0.039) | Chest Wall in Drawing (R² = 0.031) | Hypoxemia (R² = 0.220) | Nasal Discharge (R² = 0.025) | Fever (R² = 0.040) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| AOR (95% CI) | p-Value | AOR (95% CI) | p-Value | AOR (95% CI) | p-Value | AOR (95% CI) | p-Value | AOR (95% CI) | p-Value | |
| Age | ||||||||||
| <1 year | ref. | ref. | ref. | ref. | ref. | |||||
| ≥1 year | 0.623 (0.438–0.887) | 0.009 | 0.766 (0.504–1.165) | 0.213 | 0.365 (0.063–2.106) | 0.260 | 0.695 (0.546–0.884) | 0.003 | 0.692 (0.432–1.109) | 0.126 |
| Sex | ||||||||||
| Male | ref. | ref. | ref. | ref. | ref. | |||||
| Female | 1.081 (0.775–1.506) | 0.648 | 0.935 (0.621–1.407) | 0.747 | 1.877 (0.442–7.977) | 0.393 | 1.295 (1.027–1.633) | 0.029 | 0.896 (0.565–1.420) | 0.639 |
| Father’s Education | ||||||||||
| Illiterate | ref. | ref. | ref. | ref. | ref. | |||||
| Primary | 1.022 (0.583–1.794) | 0.939 | 1.011 (0.525–1.947) | 0.973 | 0.000 (0.000–0.000) | 0.992 | 0.932 (0.633–1.375) | 0.724 | 1.612 (0.774–3.359) | 0.202 |
| Secondary | 1.361 (0.778–2.379) | 0.280 | 1.278 (0.664–2.461) | 0.463 | 0.455 (0.065–3.189) | 0.428 | 1.233 (0.837–1.816) | 0.290 | 1.007 (0.460–2.204) | 0.986 |
| Higher | 1.862 (0.918–3.775) | 0.085 | 1.928 (0.832–4.469) | 0.126 | 1.424 (0.142–14.331) | 0.764 | 1.168 (0.706–1.932) | 0.546 | 0.870 (0.309–2.448) | 0.792 |
| Father’s Occupation | ||||||||||
| Day labor, Garment/Industry worker | ref. | ref. | ref. | ref. | ref. | |||||
| Skilled worker, Office non-executive & executive | 0.918 (0.547–1.542) | 0.747 | 0.987 (0.517–1.886) | 0.969 | 1.384 (0.102–18.812) | 0.807 | 1.092 (0.764–1.562) | 0.629 | 1.019 (0.496–2.095) | 0.959 |
| Business/Rickshaw/Push cart puller/Taxi/Bus/Tempo driver | 1.010 (0.639–1.597) | 0.966 | 1.241 (0.709–2.172) | 0.449 | 2.009 (0.217–18.615) | 0.539 | 0.969 (0.703–1.338) | 0.850 | 1.309 (0.701–2.443) | 0.398 |
| Other (informal) | 1.339 (0.730–2.456) | 0.345 | 1.648 (0.793–3.424) | 0.181 | 0.000 (0.000–0.000) | 0.995 | 1.060 (0.675–1.664) | 0.800 | 1.346 (0.565–3.208) | 0.502 |
| Mother’s Education | ||||||||||
| Illiterate | ref. | ref. | ref. | ref. | ref. | |||||
| Primary | 0.568 (0.320–1.009) | 0.054 | 0.790 (0.399–1.565) | 0.499 | 1.088 (0.081–14.646) | 0.949 | 1.078 (0.702–1.654) | 0.732 | 0.471 (0.226–0.980) | 0.044 |
| Secondary | 0.761 (0.432–1.340) | 0.344 | 0.880 (0.441–1.755) | 0.716 | 2.836 (0.193–41.778) | 0.448 | 1.161 (0.752–1.794) | 0.500 | 0.664 (0.327–1.350) | 0.258 |
| Higher | 0.738 (0.342–1.592) | 0.438 | 0.602 (0.225–1.609) | 0.311 | 0.000 (0.000–0.000) | 0.995 | 1.177 (0.664–2.084) | 0.577 | 0.862 (0.312–2.384) | 0.775 |
| Mother’s Occupation | ||||||||||
| Housewife | ref. | ref. | ref. | ref. | ref. | |||||
| Others | 0.641 (0.354–1.158) | 0.14 | 0.686 (0.342–1.377) | 0.289 | 2.265 (0.377–13.603) | 0.371 | 1.148 (0.804–1.639) | 0.447 | 1.135 (0.571–2.256) | 0.718 |
| Household Members | ||||||||||
| <5 members | ref. | ref. | ref. | ref. | ref. | |||||
| ≥5 members | 0.980 (0.674–1.427) | 0.918 | 1.494 (0.953–2.343) | 0.080 | 0.593 (0.060–5.883) | 0.655 | 0.984 (0.756–1.281) | 0.906 | 0.693 (0.409–1.172) | 0.171 |
| Number of Siblings | ||||||||||
| One or no | ref. | ref. | ref. | ref. | ref. | |||||
| Two | 1.111 (0.774–1.595) | 0.568 | 0.931 (0.595–1.456) | 0.753 | 0.936 (0.128–6.830) | 0.948 | 1.174 (0.910–1.514) | 0.218 | 1.066 (0.659–1.726) | 0.793 |
| Three or more | 1.064 (0.636–1.780) | 0.814 | 0.882 (0.489–1.591) | 0.677 | 4.996 (0.412–60.646) | 0.207 | 1.064 (0.742–1.526) | 0.736 | 0.912 (0.431–1.933) | 0.811 |
| Wealth Tertiles | ||||||||||
| Poor | ref. | ref. | ref. | ref. | ref. | |||||
| Middle | 1.143 (0.765–1.710) | 0.514 | 0.829 (0.514–1.337) | 0.443 | 0.217 (0.022–2.184) | 0.195 | 1.002 (0.748–1.341) | 0.990 | 1.647 (0.937–2.894) | 0.083 |
| Rich | 0.767 (0.482–1.221) | 0.264 | 0.609 (0.350–1.057) | 0.078 | 0.730 (0.118–4.500) | 0.734 | 1.205 (0.880–1.649) | 0.244 | 1.505 (0.801–2.826) | 0.204 |
| Nutrition Status | ||||||||||
| Well-nourished | ref. | ref. | ref. | ref. | ref. | |||||
| Malnourished | 1.636 (1.150–2.328) | 0.006 | 1.698 (1.113–2.590) | 0.014 | 1.098 (0.195–6.167) | 0.916 | 1.012 (0.776–1.320) | 0.932 | 1.700 (1.066–2.710) | 0.026 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huq, K.A.T.M.E.; Moriyama, M.; Matsuyama, R.; Chisti, M.J.; Rahman, M.M.; Alam, N.H. Clinical Characteristics and Underlying Factors Related to Recovery from Severe Pneumonia in Under-Five Children with or without Malnutrition Treated at Health Care Facilities in Bangladesh. Children 2021, 8, 778. https://doi.org/10.3390/children8090778
Huq KATME, Moriyama M, Matsuyama R, Chisti MJ, Rahman MM, Alam NH. Clinical Characteristics and Underlying Factors Related to Recovery from Severe Pneumonia in Under-Five Children with or without Malnutrition Treated at Health Care Facilities in Bangladesh. Children. 2021; 8(9):778. https://doi.org/10.3390/children8090778
Chicago/Turabian StyleHuq, K. A. T. M. Ehsanul, Michiko Moriyama, Ryota Matsuyama, Mohammod Jobayer Chisti, Md Moshiur Rahman, and Nur Haque Alam. 2021. "Clinical Characteristics and Underlying Factors Related to Recovery from Severe Pneumonia in Under-Five Children with or without Malnutrition Treated at Health Care Facilities in Bangladesh" Children 8, no. 9: 778. https://doi.org/10.3390/children8090778
APA StyleHuq, K. A. T. M. E., Moriyama, M., Matsuyama, R., Chisti, M. J., Rahman, M. M., & Alam, N. H. (2021). Clinical Characteristics and Underlying Factors Related to Recovery from Severe Pneumonia in Under-Five Children with or without Malnutrition Treated at Health Care Facilities in Bangladesh. Children, 8(9), 778. https://doi.org/10.3390/children8090778






