Early Intervention in Unilateral Cerebral Palsy: Let’s Listen to the Families! What Are Their Desires and Perspectives? A Preliminary Family-Researcher Co-Design Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
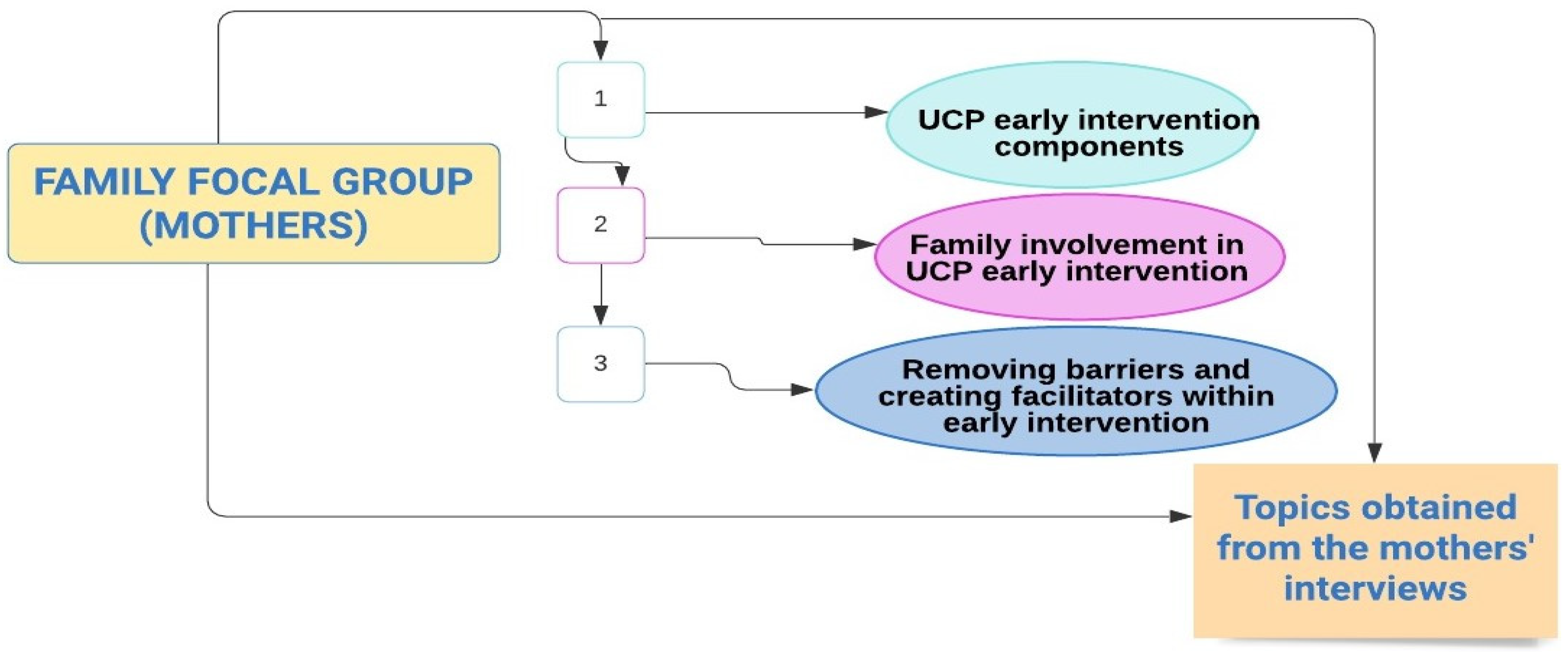
2.2. Study Design
2.3. Data Analysis
3. Results
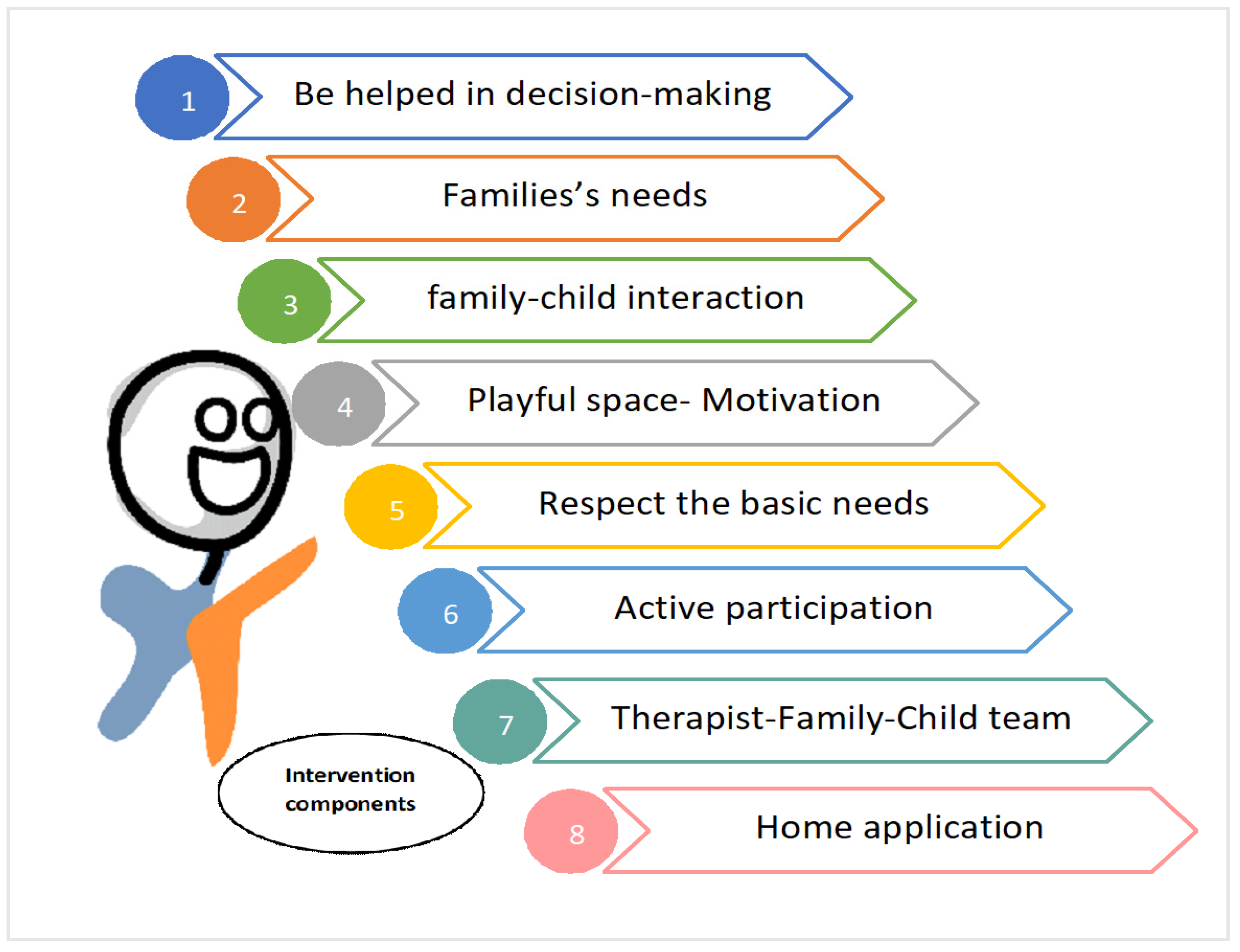
3.1. UCP Early Intervention Components
3.2. Family Involvement in UCP Early Intervention
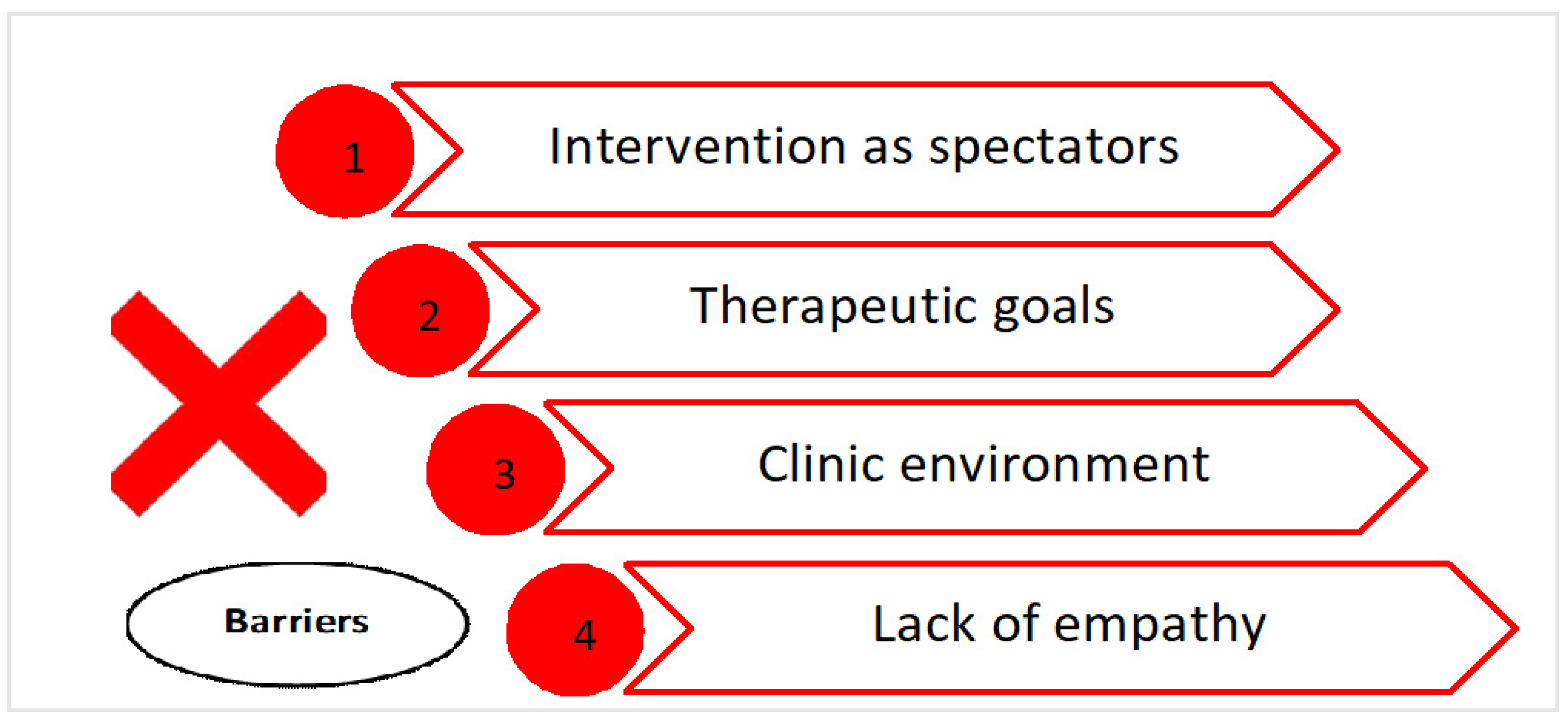
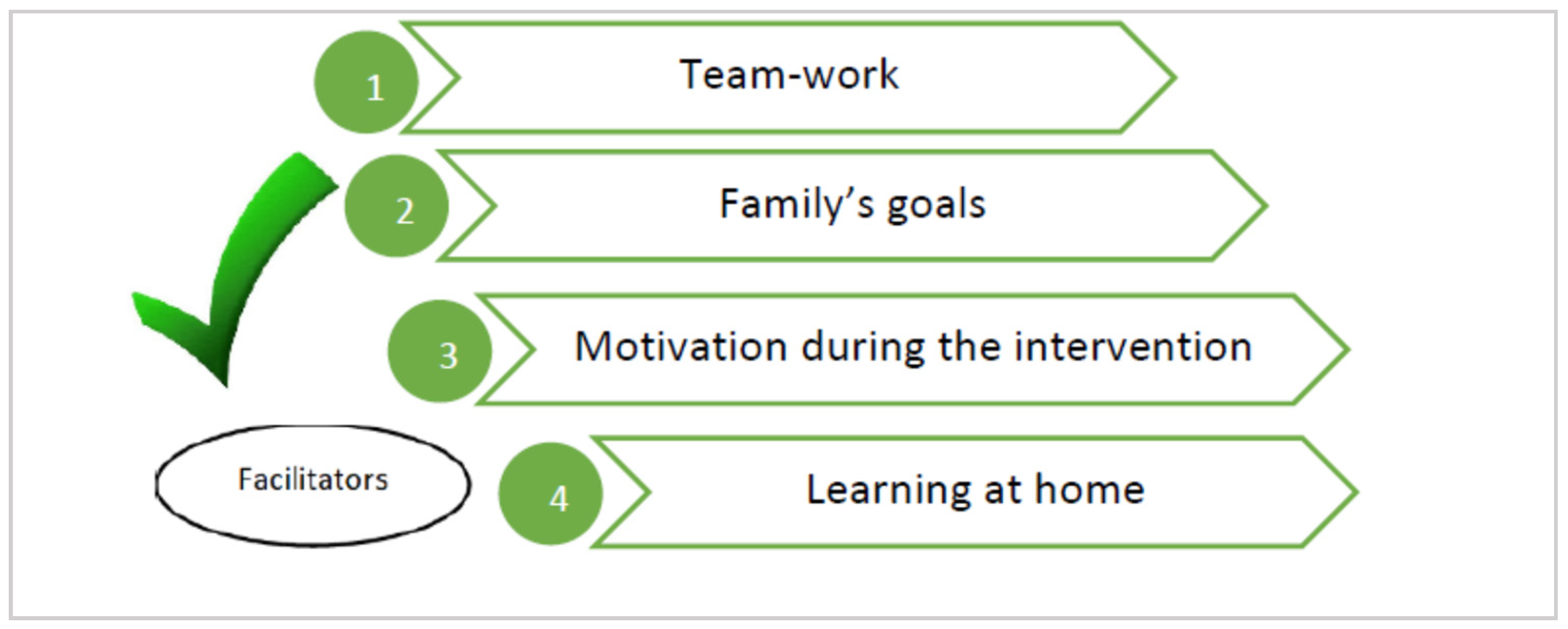
3.3. Removing Barriers and Creating Facilitators within Early Intervention
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child. Neurol. Suppl. 2007, 109, 8–14. [Google Scholar] [PubMed]
- Hadzagic-Catibusic, F.; Avdagic, E.; Zubcevic, S.; Uzicanin, S. Brain Lesions in Children with Unilateral Spastic Cerebral Palsy. Med. Arch. 2017, 71, 7–11. [Google Scholar] [CrossRef]
- Houwink, A.; Aarts, P.B.; Geurts, A.C.; Steenbergen, B. A neurocognitive perspective on developmental disregard in children with hemiplegic cerebral palsy. Res. Dev. Disabil. 2011, 32, 2157–2163. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.-C.; Chen, Y.-J.; Chien, C.-L.; Kashima, H.; Lin, K.-C. Constraint-induced movement therapy as a paradigm of translational research in neurorehabilitation: Reviews and prospects. Am. J. Transl. Res. 2010, 3, 48–60. [Google Scholar] [PubMed]
- Eyre, J.A.; Taylor, J.P.; Villagra, F.; Smith, M.; Miller, S. Evidence of activity-dependent withdrawal of corticospinal projections during human development. Neurology 2001, 57, 1543–1554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrari, F.; Plessi, C.; Lucaccioni, L.; Bertoncelli, N.; Bedetti, L.; Ori, L.; Berardi, A.; Della Casa, E.; Iughetti, L.; D’Amico, R. Motor and Postural Patterns Concomitant with General Movements Are Associated with Cerebral Palsy at Term and Fidgety Age in Preterm Infants. J. Clin. Med. 2019, 8, 1189. [Google Scholar] [CrossRef] [Green Version]
- Novak, I.; Morgan, C.; Adde, L.; Blackman, J.; Boyd, R.N.; Brunstrom-Hernandez, J.; Cioni, G.; Damiano, D.; Darrah, J.; Eliasson, A.-C.; et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy. JAMA Pediatr. 2017, 171, 897–907. [Google Scholar] [CrossRef]
- Martin, J.H.; Chakrabarty, S.; Friel, K.M. Harnessing activity-dependent plasticity to repair the damaged corticospinal tract in an animal model of cerebral palsy. Dev. Med. Child. Neurol. 2011, 53, 9–13. [Google Scholar] [CrossRef] [Green Version]
- Morgan, C.; Darrah, J.; Gordon, A.; Harbourne, R.; Spittle, A.; Johnson, R.E.; Fetters, L. Effectiveness of motor interventions in infants with cerebral palsy: A systematic review. Dev. Med. Child. Neurol. 2016, 58, 900–909. [Google Scholar] [CrossRef] [Green Version]
- Romeo, D.; Cioni, M.; Scoto, M.; Mazzone, L.; Palermo, F.; Romeo, M.G. Neuromotor development in infants with cerebral palsy investigated by the Hammersmith Infant Neurological Examination during the first year of age. Eur. J. Paediatr. Neurol. 2008, 12, 24–31. [Google Scholar] [CrossRef]
- Palomo-Carrión, R.; Romero-Galisteo, R.; Romay-Barrero, H.; Martínez-Galán, I.; Lirio-Romero, C.; Pinero-Pinto, E. How Does the Cause of Infantile Hemiparesis Influence Other Conditioning Factors? A Preliminary Study in a Spanish Population. Children 2021, 8, 323. [Google Scholar] [CrossRef]
- Clarke-Steffen, L. Waiting and Not Knowing: The Diagnosis of Cancer in a Child. J. Pediatr. Oncol. Nurs. 1993, 10, 146–153. [Google Scholar] [CrossRef]
- Landolt, M.A.; Nuoffer, J.M.; Steinmann, B.; Superti-Furga, A. Quality of life and psychologic adjustment in children and ad-olescents with early treated phenylketonuria can be normal. J. Pediatrics 2002, 140, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Wallander, J.L.; Varni, J.W. Effects of pediatric chronic physical disorders on child and family adjustment. J. Child. Psychol. Psychiatry Allied Discip. 1998, 39, 29–46. [Google Scholar] [CrossRef]
- Dunst, C.J.; Trivette, C.M.; Hamby, D.W. Meta-Analysis of family-centered help giving practices research. Ment. Retard. Dev. Disabil. Res. Rev. 2007, 13, 370–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spittle, A.; Orton, J.; Anderson, P.J.; Boyd, R.; Doyle, L.W. Early developmental intervention programmes provided post hospi-tal discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database Syst. Rev. 2015, 11, CD005495. [Google Scholar]
- Basu, A.P.; Pearse, J.E.; Baggaley, J.; Watson, R.M.; Rapley, T. Participatory design in the development of an early therapy in-tervention for perinatal stroke. BMC Pediatrics 2017, 17, 33. [Google Scholar] [CrossRef] [Green Version]
- Dirks, T.; Hadders-Algra, M. The role of the family in intervention of infants at high risk of cerebral palsy: A systematic analysis. Dev. Med. Child. Neurol. 2011, 53, 62–67. [Google Scholar] [CrossRef]
- Akhbari Ziegler, S.; Mitteregger, E.; Hadders-Algra, M. Caregivers’ experiences with the new family-centred paediatric physiotherapy programme COPCA: A qualitative study. Child. Care Health Dev. 2020, 46, 28–36. [Google Scholar] [CrossRef] [Green Version]
- Lord, C.; Rapley, T.; Marcroft, C.; Pearse, J.; Basu, A. Determinants of parent-delivered therapy interventions in children with cerebral palsy: A qualitative synthesis and checklist. Child. Care Health Dev. 2018, 44, 659–669. [Google Scholar] [CrossRef] [Green Version]
- Hemmingson, H.; Borell, L. Environmental barriers in mainstream schools. Child. Care Health Dev. 2002, 28, 57–63. [Google Scholar] [CrossRef]
- Goodwin, J.; Lecouturier, J.; Smith, J.; Crombie, S.; Basu, A.; Parr, J.R.; Howel, D.; McColl, E.; Roberts, A.; Miller, K.; et al. Understanding frames: A qualitative exploration of standing frame use for young people with cerebral palsy in educa-tional settings. Child. Care Health Dev. 2019, 45, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Blauw-Hospers, C.H.; Dirks, T.; Hulshof, L.J.; Bos, A.F.; Hadders-Algra, M. Pediatric physical therapy in infancy: From night-mare to dream? A two-arm randomized trial. Phys. Ther. 2011, 91, 1323–1338. [Google Scholar] [CrossRef] [Green Version]
- Hutchon, B.; Gibbs, D.; Harniess, P.; Jary, S.; Crossley, S.; Moffat, J.V.; Basu, N.; Basu, A.P. Early intervention programmes for infants at high risk of atypical neurodevelopmental outcome. Dev. Med. Child. Neurol. 2019, 61, 1362–1367. [Google Scholar] [CrossRef]
- Ennis, L.; Wykes, T. Impact of patient involvement in mental health research: Longitudinal study. Br. J. Psychiatry 2013, 203, 381–386. [Google Scholar] [CrossRef] [Green Version]
- Mulvaney-Day, N.E.; Rappaport, N.; Alegría, M.; Codianne, L.M. Developing systems interventions in a school setting: An application of community-based participatory research for mental health. Ethn. Dis. 2006, 16, S107–S117. [Google Scholar] [PubMed]
- Pullmann, M.D. Participatory Research in Systems of Care for Children’s Mental Health. Am. J. Community Psychol. 2009, 44, 43–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Federación Estatal de Asociaciones de Profesionales de la Atención Temprana (GAT). White Papel on Early Intervention; Real Patronato sobre Discapacidad, Ministerio de Sanidad, Política Social e Igualdad: Madrid, Spain, 2005. [Google Scholar]
- Robles-Bello, M.A.; Sánchez-Teruel, D. Atención infantil temprana en España. Pap. Psicólogo 2013, 34, 132–143. [Google Scholar]
- Graneheim, U.; Lundman, B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ. Today 2004, 24, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Coad, J.; Evans, R. Reflections on Practical Approaches to Involving Children and Young People in the Data Analysis Process. Child. Soc. 2007, 22, 41–52. [Google Scholar] [CrossRef]
- Curtis, J.R.; Engelberg, R.A.; Wenrich, M.D.; Shannon, S.E.; Treece, P.D.; Rubenfeld, G.D. Missed opportunities during family con-ferences about end-of-life care in the intensive care unit. Am. J. Respir. Crit. Care Med. 2005, 171, 844–849. [Google Scholar] [CrossRef] [PubMed]
- Cox, E.D.; Jacobsohn, G.C.; Rajamanickam, V.P.; Carayon, P.; Kelly, M.; Wetterneck, T.B.; Rathouz, P.J.; Brown, R.L. A Family-Centered Rounds Checklist, Family Engagement, and Patient Safety: A Randomized Trial. Pediatrics 2017, 139, e20161688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, S.; Davis, N.; Tyson, S.F. A scoping review of the needs of children and other family members after a child’s traumatic injury. Clin. Rehabil. 2017, 32, 501–511. [Google Scholar] [CrossRef] [Green Version]
- Woodgate, R.L.; Edwards, M.; Ripat, J.D.; Borton, B.L.; Rempel, G. Intense parenting: A qualitative study detailing the experiences of parenting children with complex care needs. BMC Pediatr. 2015, 15, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dirik, A.; Sandhu, S.; Giacco, D.; Barrett, K.; Bennison, G.; Collinson, S.; Priebe, S. Why involve families in acute mental healthcare? A collaborative conceptual review. BMJ Open 2017, 7, e017680. [Google Scholar] [CrossRef] [Green Version]
- Puurveen, G.; Baumbusch, J.; Gandhi, P. From Family Involvement to Family Inclusion in Nursing Home Settings: A Critical Interpretive Synthesis. J. Fam. Nurs. 2018, 24, 60–85. [Google Scholar] [CrossRef]
- Whittingham, K.; Sanders, M.R.; McKinlay, L.; Boyd, R.N. Parenting Intervention Combined With Acceptance and Commitment Therapy: A Trial with Families of Children with Cerebral Palsy. J. Pediatr. Psychol. 2016, 41, 531–542. [Google Scholar] [CrossRef] [Green Version]
- Huang, H.-H.; Huang, H.-W.; Chen, Y.-M.; Hsieh, Y.-H.; Shih, M.-K.; Chen, C.-L. Modified ride-on cars and mastery motivation in young children with disabilities: Effects of environmental modifications. Res. Dev. Disabil. 2018, 83, 37–46. [Google Scholar] [CrossRef]
- Wang, P.-J.; Hwang, A.-W.; Liao, H.-F.; Chen, P.-C.; Hsieh, W.-S. The stability of mastery motivation and its relationship with home environment in infants and toddlers. Infant Behav. Dev. 2011, 34, 434–442. [Google Scholar] [CrossRef]
- Piggot, J.; Paterson, J.; Hocking, C. Participation in Home Therapy Programs for Children with Cerebral Palsy: A Compelling Challenge. Qual. Health Res. 2002, 12, 1112–1129. [Google Scholar] [CrossRef]
- Brotherson, M.J.; Cook, C.C.; Erwin, E.J.; Weigel, C. Understanding self-determination and families of young children with disabili-ties in home environ ments. J. Early Interv. 2008, 31, 22–43. [Google Scholar] [CrossRef]
- Health Resources and Services Administration. Designated Health Professional Shortage Areas Statistics; US Department of Health and Human Services, Health Resources and Services Administration: Rockville, MD, USA, 2016.
- Smalley, K.B.; Yancey, C.T.; Warren, J.C.; Naufel, K.; Ryan, R.; Pugh, J.L. Rural mental health and psychological treatment: A review for practitioners. J. Clin. Psychol. 2010, 66, 479–489. [Google Scholar] [CrossRef]
- Angold, A.; Erkanli, A.; Farmer, E.M.Z.; Fairbank, J.A.; Burns, B.J.; Keeler, G.; Costello, E.J. Psychiatric Disorder, Impairment, and Service Use in Rural African American and White Youth. Arch. Gen. Psychiatry 2002, 59, 893–901. [Google Scholar] [CrossRef]
- Skinner, A.C.; Slifkin, R.T. Rural/Urban Differences in Barriers to and Burden of Care for Children with Special Health Care Needs. J. Rural. Heal. 2007, 23, 150–157. [Google Scholar] [CrossRef]
- Olsen, J.M. Health Coaching: A Concept Analysis. Nurs. Forum 2013, 49, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Huffman, M.H. Health coaching: A fresh, new approach to improve quality outcomes and compliance for patients with chronic conditions. Home Health Nurse 2009, 27, 490–496. [Google Scholar] [CrossRef]
- Dirks, T.; Blauw-Hospers, C.H.; Hulshof, L.J.; Hadders-Algra, M. Differences between the family-centered ‘COPCA’ program and traditional infant physical therapy based on neurodevelopmental treatment principles. Phys. Ther. 2011, 91, 1303–1322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nyante, G.G.; Carpenter, C. The experience of carers of children with cerebral palsy living in rural areas of Ghana who have received no rehabilitation services: A qualitative study. Child. Care Health Dev. 2019, 45, 815–822. [Google Scholar] [CrossRef]
- Morgan, F.; Tan, B.K. Rehabilitation for children with cerebral palsy in rural Cambodia: Parental perceptions of family-centred practices. Child. Care Health Dev. 2011, 37, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Koçak, F.A.; Koçak, Y.; Şaş, S.; Kurt, E.E.; Erdem, H.R.; Tuncay, F. The evaluation of opinions of the parents of children with cerebral palsy on exercise therapy applied in Special Education and Rehabilitation Centers in rural areas. Turk. J. Phys. Med. Rehabil. 2018, 64, 369–370. [Google Scholar] [CrossRef] [PubMed]

| Open Questions in the Interview | Responses from Mothers during the Interview |
|---|---|
| What components should early intervention have for the baby diagnosed with UCP? | Mother 1. “Coaching families to understand how to handle the child at different times of the day”. Mother 2. “Increasing the functionality of our children. Respecting the periods of time in which the child is not attentive or is tired”. Mother 3. “Not generating frustration for the child or the family, that the child does not cry all the time and playing happens”. Mother 4. “That there is communication between the therapist and the family”. Mother 5. “For therapists to spend time with the family to listen to their problems because it is not easy to manage the situation of diagnosis and treatment”. Mother 6. “That families are able to make decisions together with therapists”. Mother 7. “Proposing targets that are not only those of the therapist”. Mother 8. “For the sessions not to be therapist–child, but for the family to be also a member”. Mother 9. “For families to understand what they want to do with our children”. Mother 10. “For their development to be promoted as best as possible and that there is not continuous crying during the intervention”. |
| What components should early intervention have for the family? | Mother 1. “Involving the family throughout the treatment process, not just telling them what to do”. Mother 2. “Reflecting together on what is best for our children, that we play an active role”. Mother 3. “We know our children, so we must be actively involved. We need to feel that what we do is okay and achieve satisfaction through common goals, not just the therapist”. Mother 4. “Allowing a pleasant situation to be created for the family and that frustration is not generated; our stress levels are very high; we do not know what will happen to our children”. Mother 5. An interaction to be established between the therapist (and) us as a family and to have an impact on our children with training in their management”. Mother 6. “For the intervention to be designed at home so that our time can be respected, with a follow-up by the therapist”. Mother 7. “For us to be able to accompany and decide on the treatment of our children and to not be judged”. Mother 8. “For us to be able to make use of our home as a means for the development of our children and to be taught some strategies to make correct use of them”. Mother 9. “For our needs to be understood, for the therapist to give us security in the handling of our children”. Mother 10. “For us to be able to design strategies or tools that are useful to improve the functionality of our children and to feel useful in the process”. |
| What should be the involvement of the family in early intervention? | Mother 1. “To be able to decide on the different tools or interventions that are going to be carried out with our children”. Mother 2. “We can guide the treatment from home to be able to use the moments when the child is calm”. Mother 3. “We know our children, and we need training to be able to offer them learning through our games”. Mother 4. “Deciding together with the professionals what to do, not just listening”. Mother 5. “To include ourselves in our children’s therapy and to learn to give them what they need from home, where they spend more time and with us”. Mother 6. “To have a say and not just listen to what the therapist tells us to do, establishing a joint dialogue for the betterment of our children”. Mother 7. “To be heard to plan the intervention from home and together”. Mother 8. “To use the knowledge we have of our children to promote their development and learning in a stable environment, such as home”. Mother 9. “It would be very good if a therapist–family team was created so that everyone’s well-being is enhanced and for it to be founded in a playful place”. Mother 10. “Our involvement must be active, not just listening because we know how to calm our children; we would need coaching to better interact with our children and to achieve the goals that we always set ourselves with motivation for all”. |
| What barriers included in early intervention should be removed? | Mother 1. “The clinical setting sometimes does not provide an opportunity for the family to participate”. Mother 2. “The clinical environment does not allow us to make use of our moments of greater tranquility and the hours and waits become very burdensome”. Mother 3. “The clinical environment and the therapists when they impose their own knowledge and do not give you the opportunity for dialogue”. Mother 4. “The therapist who does not listen to you and is in a clinical environment that is not motivating at all”. Mother 5. “Treatment at home may be better than in the hospital as it [hospital] does not offer many times when families can feel comfortable or calm”. Mother 6. “The lack of empathy of many professionals and their distance from families within the practice or hospital”. Mother 7. “Not being able to say what my son needs, the goals we want, and that this distance becomes greater at the practice”. Mother 8. “That the therapist is always the one who determines the moment in which the intervention should be carried out according to his goals in the hospital”. Mother 9. “The lack of empathy of the professionals who believe that they know everything at the hospital and are unaware of our problems, without giving us the opportunity to participate”. Mother 10. “Set goals to work at the hospital, but what happens at home? That stage ends, and we have to face a very difficult path without support”. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palomo-Carrión, R.; Romay-Barrero, H.; Pinero-Pinto, E.; Romero-Galisteo, R.-P.; López-Muñoz, P.; Martínez-Galán, I. Early Intervention in Unilateral Cerebral Palsy: Let’s Listen to the Families! What Are Their Desires and Perspectives? A Preliminary Family-Researcher Co-Design Study. Children 2021, 8, 750. https://doi.org/10.3390/children8090750
Palomo-Carrión R, Romay-Barrero H, Pinero-Pinto E, Romero-Galisteo R-P, López-Muñoz P, Martínez-Galán I. Early Intervention in Unilateral Cerebral Palsy: Let’s Listen to the Families! What Are Their Desires and Perspectives? A Preliminary Family-Researcher Co-Design Study. Children. 2021; 8(9):750. https://doi.org/10.3390/children8090750
Chicago/Turabian StylePalomo-Carrión, Rocío, Helena Romay-Barrero, Elena Pinero-Pinto, Rita-Pilar Romero-Galisteo, Purificación López-Muñoz, and Inés Martínez-Galán. 2021. "Early Intervention in Unilateral Cerebral Palsy: Let’s Listen to the Families! What Are Their Desires and Perspectives? A Preliminary Family-Researcher Co-Design Study" Children 8, no. 9: 750. https://doi.org/10.3390/children8090750
APA StylePalomo-Carrión, R., Romay-Barrero, H., Pinero-Pinto, E., Romero-Galisteo, R.-P., López-Muñoz, P., & Martínez-Galán, I. (2021). Early Intervention in Unilateral Cerebral Palsy: Let’s Listen to the Families! What Are Their Desires and Perspectives? A Preliminary Family-Researcher Co-Design Study. Children, 8(9), 750. https://doi.org/10.3390/children8090750








