Is Longstanding Congenital Muscular Torticollis Provoking Pelvic Malalignment Syndrome?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Subjects
2.3. Outcome Measurements
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Yim, S.Y.; Yoon, D.; Park, M.C.; Lee, I.J.; Kim, J.H.; Lee, M.A.; Kwack, K.S.; Lee, J.D.; Lee, J.H.; Soh, E.Y.; et al. Integrative analysis of congenital muscular torticollis: From gene expression to clinical significance. BMC Med. Genom. 2013, 6 (Suppl. 2), S10. [Google Scholar] [CrossRef] [Green Version]
- Kaplan, S.L.; Coulter, C.; Fetters, L. Physical therapy management of congenital muscular torticollis: An evidence-based clinical practice guideline: From the Section on Pediatrics of the American Physical Therapy Association. Pediatric Phys. Ther. 2013, 25, 348–394. [Google Scholar] [CrossRef]
- Blythe, W.R.; Logan, T.C.; Holmes, D.K.; Drake, A.F. Fibromatosis Colli: A common cause of neonatal torticollis. Am. Fam. Physician 1996, 54, 1965–1967. [Google Scholar]
- Stassen, L.F.; Kerawala, C.J. New surgical technique for the correction of congenital muscular torticollis (wry neck). Br. J. Oral Maxillofac. Surg. 2000, 38, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Hollier, L.; Kim, J.; Grayson, B.H.; McCarthy, J.G. Congenital muscular torticollis and the associated craniofacial changes. Plast. Reconstr. Surg. 2000, 105, 827–835. [Google Scholar] [CrossRef] [PubMed]
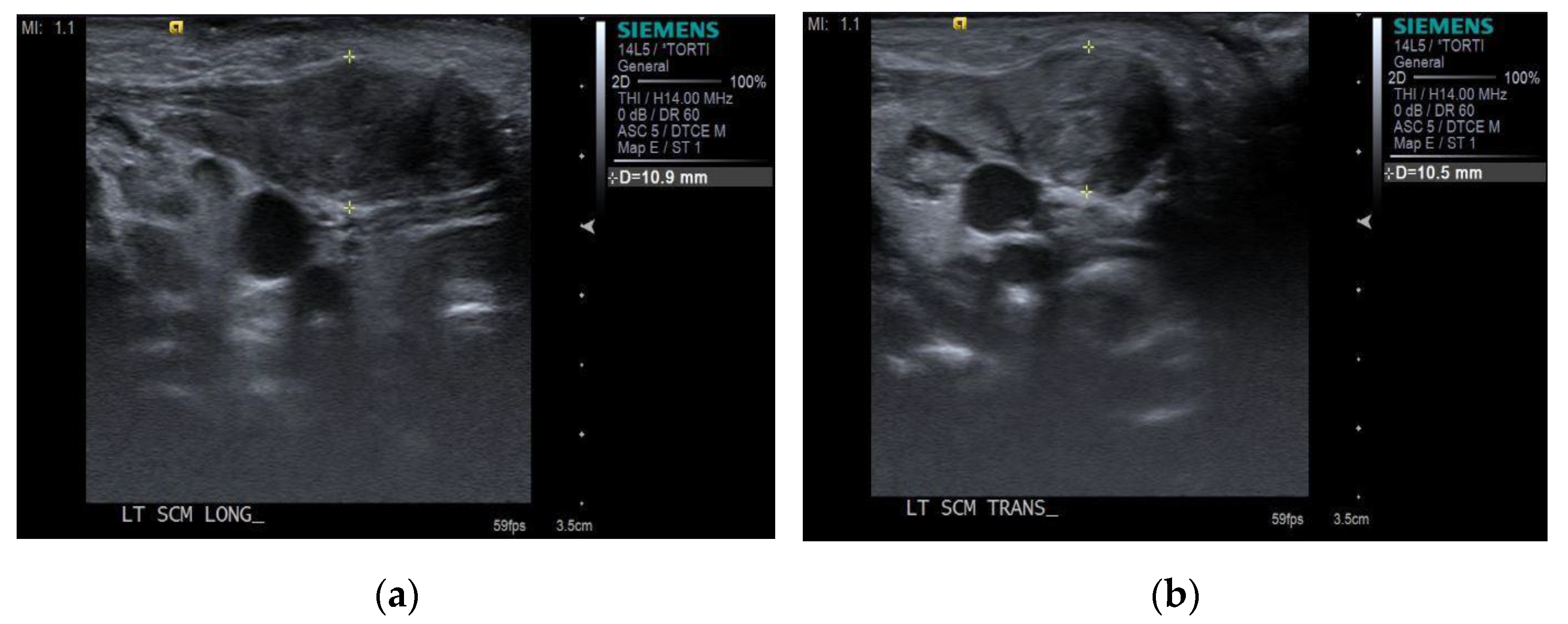
- Han, M.H.; Kang, J.Y.; Do, H.J.; Park, H.S.; Noh, H.J.; Cho, Y.H.; Jang, D.H. Comparison of Clinical Findings of Congenital Muscular Torticollis Between Patients With and Without Sternocleidomastoid Lesions as Determined by Ultrasonography. J. Pediatric Orthop. 2019, 39, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Canale, S.T.; Griffin, D.W.; Hubbard, C.N. Congenital muscular torticollis. A long-term follow-up. J. Bone Jt. Surg. Am. 1982, 64, 810–816. [Google Scholar] [CrossRef]
- Ballock, R.T.; Song, K.M. The prevalence of nonmuscular causes of torticollis in children. J. Pediatric Orthop. 1996, 16, 500–504. [Google Scholar] [CrossRef]
- Kim, J.H.; Yum, T.H.; Shim, J.S. Secondary Cervicothoracic Scoliosis in Congenital Muscular Torticollis. Clin. Orthop. Surg. 2019, 11, 344–351. [Google Scholar] [CrossRef]
- Seo, S.J.; Yim, S.Y.; Lee, I.J.; Han, D.H.; Kim, C.S.; Lim, H.; Park, M.C. Is craniofacial asymmetry progressive in untreated congenital muscular torticollis? Plast. Reconstr. Surg. 2013, 132, 407–413. [Google Scholar] [CrossRef]
- Seo, S.J.; Kim, J.H.; Joh, Y.H.; Park, D.H.; Lee, I.J.; Lim, H.; Park, M.C. Change of Facial Asymmetry in Patients With Congenital Muscular Torticollis After Surgical Release. J. Craniofac. Surg. 2016, 27, 64–69. [Google Scholar] [CrossRef]
- Ta, J.H.; Krishnan, M. Management of congenital muscular torticollis in a child: A case report and review. Int. J. Pediatric Otorhinolaryngol. 2012, 76, 1543–1546. [Google Scholar] [CrossRef]
- Sargent, B.; Kaplan, S.L.; Coulter, C.; Baker, C. Congenital Muscular Torticollis: Bridging the Gap Between Research and Clinical Practice. Pediatrics 2019, 144, e20190582. [Google Scholar] [CrossRef]
- Hussein, M.A.; Yun, I.S.; Lee, D.W.; Park, H.; Oock, K.Y. Cervical Spine Dysmorphism in Congenital Muscular Torticollis. J. Craniofac. Surg. 2018, 29, 925–929. [Google Scholar] [CrossRef]
- Hussein, M.A.; Yun, I.S.; Park, H.; Kim, Y.O. Cervical Spine Deformity in Long-Standing, Untreated Congenital Muscular Torticollis. J. Craniofac. Surg. 2017, 28, 46–50. [Google Scholar] [CrossRef]
- Ahn, A.R.; Rah, U.W.; Woo, J.E.; Park, S.; Kim, S.; Yim, S.Y. Craniovertebral Junction Abnormalities in Surgical Patients With Congenital Muscular Torticollis. J. Craniofac. Surg. 2018, 29, e327–e331. [Google Scholar] [CrossRef]
- Schamberger, W. Malalignment Syndrome in Runners. Phys. Med. Rehabil. Clin. 2016, 27, 237–317. [Google Scholar] [CrossRef] [PubMed]
- Schamberger, W. The Malalignment Syndrome, 2nd ed.; Churchill Livingstone: Vancouver, BC, Canada, 2012. [Google Scholar]
- Hwang, D.; Shin, Y.J.; Choi, J.Y.; Jung, S.J.; Yang, S.S. Changes in muscle stiffness in infants with congenital muscular torticollis. Diagnostics 2019, 9, 8290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cho, J.H.; Lee, C.S.; Joo, Y.; Park, J.; Hwang, C.J.; Lee, D. Association between Sacral Slanting and Adjacent Structures in Patients with Adolescent Idiopathic Scoliosis. Clin. Orthop. Surg. 2017, 9, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Sandstrom, S.; Pettersson, H.; Akerman, K. The WHO Manual of Diagnostic Imaging: Radiographic Technique and Projections; WHO: Geneva, Switzerland, 2003. [Google Scholar]
- Kaplan, S.L.; Coulter, C.; Sargent, B. Physical Therapy Management of Congenital Muscular Torticollis: A 2018 Evidence-Based Clinical Practice Guideline From the APTA Academy of Pediatric Physical Therapy. Pediatric Phys. Ther. 2018, 30, 240–290. [Google Scholar] [CrossRef]
- Cheng, J.C.; Tang, S.P.; Chen, T.M.; Wong, M.W.; Wong, E.M. The clinical presentation and outcome of treatment of congenital muscular torticollis in infants–A study of 1086 cases. J. Pediatric Surg. 2000, 35, 1091–1109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vallen, H.; Xi, T.; Nienhuijs, M.; Borstlap, W.; Loonen, T.; Hoogendoorn, B.; van Vlimmeren, L.; Maal, T. Three-dimensional stereophotogrammetry measurement of facial asymmetry in patients with congenital muscular torticollis: A non-invasive method. Int. J. Oral Maxillofac. Surg. 2020, 50, 835–842. [Google Scholar] [CrossRef]
- Crawford, S.C.; Harnsberger, H.R.; Johnson, L.; Aoki, J.R.; Giley, J. Fibromatosis Colli of infancy: CT and sonographic find ings. AJR Am. J. Roentgenol. 1988, 151, 1183–1184. [Google Scholar] [CrossRef]
- Lowry, K.C.; Estroff, J.A.; Rahbar, R. The presentation and management of fibromatosis colli. Ear Nose Throat J. 2010, 89, E4–E8. [Google Scholar] [CrossRef] [PubMed]
- Demirbilek, S.; Atayurt, H.F. Congenital muscular torticollis and sternomastoid tumor: Results of nonoperative treatment. J. Pediatric Surg. 1999, 34, 549–551. [Google Scholar] [CrossRef]
- Li, D.; Wang, K.; Zhang, W.; Wang, J. Expression of Bax/Bcl-2, TGF-β1, and Type III Collagen Fiber in Congenital Muscular Torticollis. Med. Sci. Monit. 2018, 24, 7869–7874. [Google Scholar] [CrossRef] [PubMed]




| Characteristic | n (%) | |
|---|---|---|
| Sex | Male | 80 (61.5) |
| Female | 50 (38.5) | |
| Initial diagnosis age | 0–12 months | 124 (95.4) |
| 13–24 months | 3 (2.3) | |
| After 24 months | 3 (2.3) | |
| Delivery type | Cesarean section | 38 (29.2) |
| Vaginal delivery | 92 (70.8) | |
| Range of motion | Limited | 73 (56.2) |
| Normal | 57 (43.8) | |
| Presence of fibrotic mass | Presence | 45 (34.6) |
| Absence | 85 (63.4) | |
| Plagiocephaly | Presence | 34 (26.2) |
| Absence | 96 (73.8) | |
| n (%) | |
|---|---|
| Scoliosis | 20 (15.4) |
| Pelvic malalignment syndrome (PMS) | 48 (36.9) |
| Scoliosis combined with PMS | 3 (2.3) |
| No change | 59 (45.4) |
| Total | 130 (100.0) |
| F/U Age (n) | PMS | Scoliosis | Scoliosis Combined with PMS |
|---|---|---|---|
| 24–48 months (77) | 24 (18.5) | 5 (3.8) | 1 (0.8) |
| 49–60 months (24) | 12 (9.2) | 4 (3.1) | 0 (0.0) |
| 61 months–12 year (29) | 12 (9.2) | 11 (8.5) | 2 (1.5) |
| Total (130) | 48 (36.9) | 20 (15.4) | 3 (2.3) |
| Factor | Malalignment Pelvis Group (n = 51) | Normal Pelvis Group (n = 79) | p-Value |
|---|---|---|---|
| Delivery type | 0.451 | ||
| Cesarean section | 13 (34.2) | 25 (65.8) | |
| Vaginal delivery | 38 (41.3) | 54 (58.7) | |
| Location | 0.590 | ||
| Right | 24 (36.9) | 41 (63.1) | |
| Left | 27 (41.5) | 38 (58.5) | |
| Range of motion | 0.622 | ||
| Limited | 30 (41.1) | 43 (58.9) | |
| Normal | 21 (36.8) | 36 (63.2) | |
| Presence of mass | 0.611 | ||
| Presence | 19 (42.2) | 26 (57.8) | |
| Absence | 32 (37.6) | 53 (62.8) | |
| Plagiocephaly | 0.584 | ||
| Presence | 12 (35.3) | 22 (64.7) | |
| Absence | 39 (40.6) | 57 (59.4) |
| Univariate Analysis | ||
|---|---|---|
| Variable | B (SE) | p-Value |
| Female vs. male | 0.32 (0.37) | 0.379 |
| Diagnosis age, <6 months | 0.31 (0.47) | 0.513 |
| Involved side, right vs. left | 0.19 (0.36) | 0.590 |
| Initial neck LOM | 0.23 (0.36) | 0.527 |
| Concurrent plagiocephaly | −0.28 (0.43) | 0.518 |
| Fibromatosis colli type | −0.19 (0.38) | 0.611 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.-i.; Kee, J.-H.; Choi, J.Y.; Yang, S.-s. Is Longstanding Congenital Muscular Torticollis Provoking Pelvic Malalignment Syndrome? Children 2021, 8, 735. https://doi.org/10.3390/children8090735
Park J-i, Kee J-H, Choi JY, Yang S-s. Is Longstanding Congenital Muscular Torticollis Provoking Pelvic Malalignment Syndrome? Children. 2021; 8(9):735. https://doi.org/10.3390/children8090735
Chicago/Turabian StylePark, Jun-il, Joo-Hyun Kee, Ja Young Choi, and Shin-seung Yang. 2021. "Is Longstanding Congenital Muscular Torticollis Provoking Pelvic Malalignment Syndrome?" Children 8, no. 9: 735. https://doi.org/10.3390/children8090735
APA StylePark, J.-i., Kee, J.-H., Choi, J. Y., & Yang, S.-s. (2021). Is Longstanding Congenital Muscular Torticollis Provoking Pelvic Malalignment Syndrome? Children, 8(9), 735. https://doi.org/10.3390/children8090735






