Mental Health and Wellbeing at Schools: Health Promotion in Primary Schools with the Use of Digital Methods
Abstract
1. Introduction
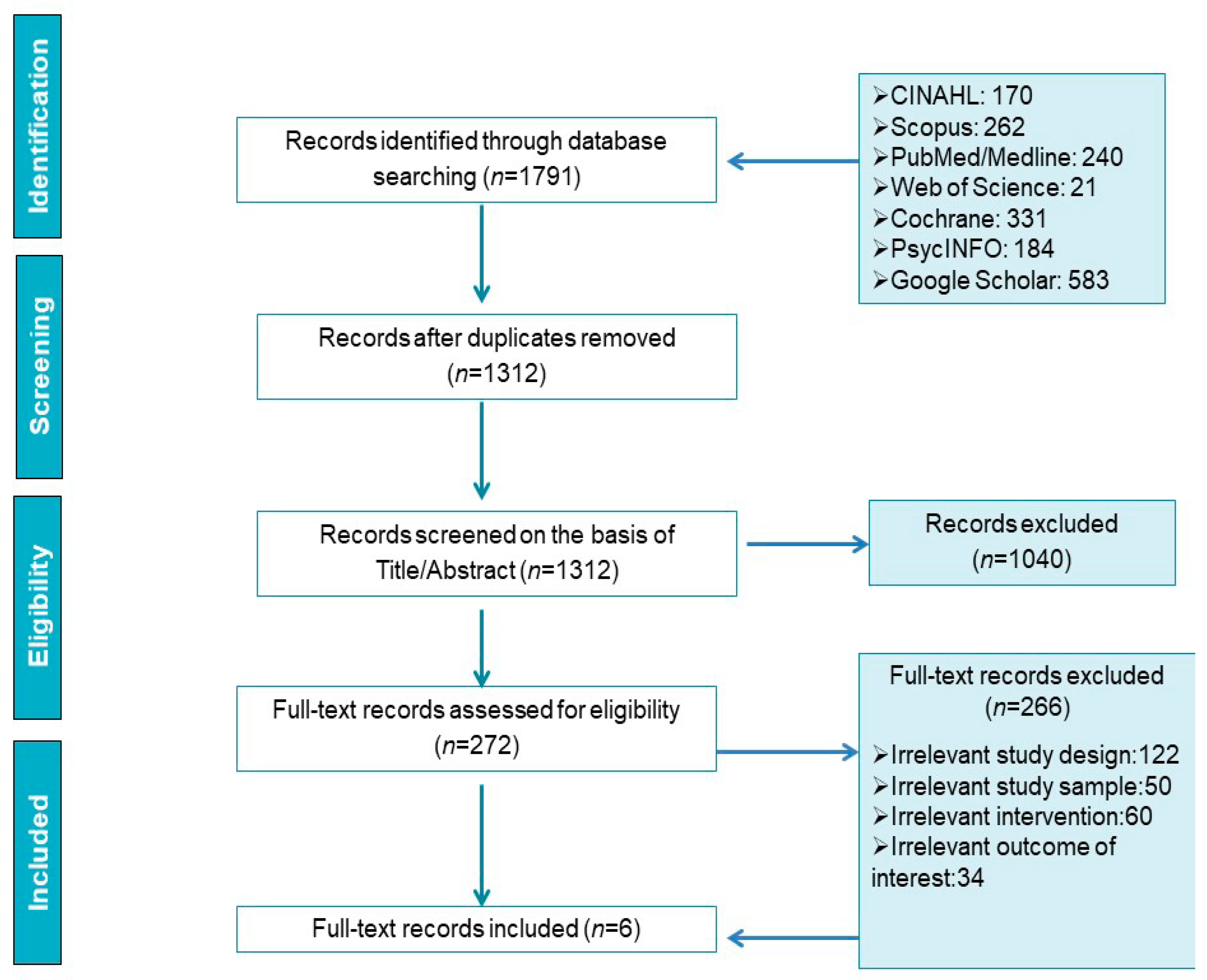
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Literature Search
2.3. Data Analysis
3. Results
3.1. Aims of the Studies
3.2. Interventions
3.3. Evaluation Tools
3.4. Intervention Outcomes
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Erskine, H.E.; Moffitt, T.E.; Copeland, W.E.; Costello, E.J.; Ferrari, A.J.; Patton, G.; Degenhardt, L.; Vos, T.; Whiteford, H.A.; Scott, J.G. A heavy burden on young minds: The global burden of mental and substance use disorders in children and youth. Psychol. Med. 2015, 45, 1551–1563. [Google Scholar] [CrossRef]
- Essau, C.A. Frequency and patterns of mental health services utilization among adolescents with anxiety and depressive disorders. Depress. Anxiety 2005, 22, 130–137. [Google Scholar] [CrossRef]
- Kizaur, L. Barriers in Accessing Child Mental Health Services for Parents and Caregivers; 2016 Retrieved from Sophia, the St. Catherine University Repository. Available online: https://sophia.stkate.edu/msw_papers/616 (accessed on 1 February 2021).
- OECD. Mental Health Problems Costing Europe Heavily. 2018. Available online: https://www.oecd.org/health/mental-health-problems-costing-europe-heavily.htm (accessed on 1 February 2021).
- Kessler, R.C.; Angermeyer, M.; Anthony, J.C.; de Graaf, R.; Demyttenaere, K.; Gasquet, I.; de Girolamo, G.; Gluzman, S.; Gureje, O.; Haro, J.M.; et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 2007, 6, 168–176. [Google Scholar] [PubMed]
- McGorry, P.D.; Purcell, R.; Goldstone, S.; Amminger, G.P. Age of onset and timing of treatment for mental and substance use disorders: Implications for preventive intervention strategies and models of care. Curr. Opin. Psychiatry 2011, 24, 301–306. [Google Scholar] [CrossRef]
- De Girolamo, G.; Dagani, J.; Purcell, R.; Cocchi, A.; McGorry, P.D. Age of onset of mental disorders and use of mental health services: Needs, opportunities and obstacles. Epidemiol. Psychiatr. Sci. 2012, 21, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Whiteford, H.A.; Degenhardt, L.; Rehm, J.; Baxter, A.J.; Ferrari, A.J.; Erskine, H.E.; Charlson, F.J.; Norman, R.E.; Flaxman, A.D.; Johns, N.; et al. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet 2013, 382, 1575–1586. [Google Scholar] [CrossRef]
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- National Health System (NHS). Mental Health of Children and Young People in England. 2017. Available online: https://files.digital.nhs.uk/9B/6F123E/MHCYP%202017%20Summary.pdf (accessed on 2 February 2021).
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef]
- Colman, I.; Murray, J.; Abbott, R.A.; Maughan, B.; Kuh, D.; Croudace, T.J.; Jones, P.B. Outcomes of conduct problems in adolescence: 40 year follow-up of national cohort. BMJ 2009, 338, a2981. [Google Scholar] [CrossRef]
- European Union. Joint Action on Mental Health and Well-Being. Mental Health and Schools. 2017. Available online: https://ec.europa.eu/health/sites/health/files/mental_health/docs/2017_mh_schools_en.pdf (accessed on 5 February 2021).
- Lima-Serrano, M.; Lima-Rodríguez, J.S. Impact of school-based health promotion interventions aimed at different behavioral domains: A systematic review. Gac. Sanit. Sep. Oct. 2014, 28, 411–417. [Google Scholar] [CrossRef][Green Version]
- World Health Organisation (WHO). Health Promoting School: An Effective Approach for Early Action on NCD Risk Factors. Available online: http://www.who.int/healthpromotion/publications/health-promotion-school/en/ (accessed on 18 February 2021).
- Singh, A.; Bassi, S.; Nazar, G.P.; Saluja, K.; Park, M.; Kinra, S.; Arora, M. Impact of school policies on non-communicable disease risk factors—A systematic review. BMC Public Health 2017, 17, 1–19. [Google Scholar] [CrossRef] [PubMed]
- UNICEF Data: Monitoring the Situation of Children and Women. Primary Education. 2019. Available online: https://data.unicef.org/topic/education/primary-education/ (accessed on 18 February 2021).
- Demetriou, Y.; Sudeck, G.; Thiel, A.; Höner, O. The Effects of School-Based Physical Activity Interventions on Students’ Health-Related Fitness Knowledge: A systematic review. Educ. Res. Rev. 2015, 16, 19–40. [Google Scholar] [CrossRef]
- Schüller, I.; Demetriou, Y. Physical activity interventions promoting social competence at school: A systematic review. Educ. Res. Rev. 2018, 25, 39–55. [Google Scholar] [CrossRef]
- Racey, M.; O’Brien, C.; Douglas, S.; Marquez, O.; Hendrie, G.; Newton, G. Systematic Review of School-Based Interventions to Modify Dietary Behavior: Does Intervention Intensity Impact Effectiveness? J. Sch. Health 2016, 86, 452–463. [Google Scholar] [CrossRef]
- Carney, T.; Myers, B.J.; Louw, J.; Okwundu, C.I. Brief school-based interventions and behavioural outcomes for substance-using adolescents. Cochrane Database Syst. Rev. 2016, 1, CD008969. [Google Scholar] [CrossRef] [PubMed]
- Champion, K.E.; Newton, N.C.; Barrett, E.L.; Teesson, M. A systematic review of school-based alcohol and other drug prevention programs facilitated by computers or the Internet. Drug Alcohol Rev. 2012, 32, 115–123. [Google Scholar] [CrossRef]
- Salerno, J.P. Effectiveness of Universal School-Based Mental Health Awareness Programs among Youth in the United States: A Systematic Review. J. Sch. Health 2016, 86, 922–931. [Google Scholar] [CrossRef]
- Kutcher, S.; Wei, Y.; Gilberds, H.; Ubuguyu, O.; Njau, T.; Brown, A.; Sabuni, N.; Magimba, A.; Perkins, K. A school mental health literacy curriculum resource training approach: Effects on Tanzanian teachers’ mental health knowledge, stigma and help-seeking efficacy. Int. J. Ment. Health Syst. 2016, 10, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Teesson, M.; Newton, N.C.; Slade, T.; Chapman, C.; Birrell, L.; Mewton, L.; Mather, M.; Hides, L.; McBride, N.; Allsop, S.; et al. Combined prevention for substance use, depression, and anxiety in adolescence: A cluster-randomised controlled trial of a digital online intervention. Lancet Digit. Health 2020, 2, e74–e84. [Google Scholar] [CrossRef]
- Gonsalves, P.P.; Hodgson, E.S.; Kumar, A.; Aurora, T.; Chandak, Y.; Sharma, R.; Michelson, D.; Patel, V. Design and Development of the “POD Adventures” Smartphone Game: A Blended Problem-Solving Intervention for Adolescent Mental Health in India. Front. Public Health 2019, 7, 238. [Google Scholar] [CrossRef]
- Peiris-John, R.; Dizon, L.; Sutcliffe, K.; Kang, K.; Fleming, T. Co-creating a large-scale adolescent health survey integrated with access to digital health interventions. Digit. Health 2020, 6, 1–13. [Google Scholar] [CrossRef]
- Osborn, T.L.; Rodriguez, M.; Wasil, A.R.; Venturo-Conerly, K.E.; Gan, J.; Alemu, R.G.; Roe, E.; Arango, G.S.; Otieno, B.H.; Wasanga, C.M.; et al. Single-session digital intervention for adolescent depression, anxiety, and well-being: Outcomes of a randomized controlled trial with Kenyan adolescents. J. Consult. Clin. Psychol. 2020, 88, 657–668. [Google Scholar] [CrossRef]
- Maloney, C.A.; Abel, W.D.; McLeod, H.J. Jamaican adolescents’ receptiveness to digital mental health services: A cross-sectional survey from rural and urban communities. Internet Interv. 2020, 21, 100325. [Google Scholar] [CrossRef]
- Huen, J.M.; Lai, E.S.; Shum, A.K.; So, S.W.; Chan, M.K.; Wong, P.W.; Law, Y.W.; Yip, P.S. Evaluation of a Digital Game-Based Learning Program for Enhancing Youth Mental Health: A Structural Equation Modeling of the Program Effectiveness. JMIR. Ment. Health 2016, 3, e46. [Google Scholar] [CrossRef] [PubMed]
- Moeini, B.; Bashirian, S.; Soltanian, A.R.; Ghaleiha, A.; Taheri, M. Examining the Effectiveness of a Web-Based Intervention for Depressive Symptoms in Female Adolescents: Applying Social Cognitive Theory. J. Res. Health Sci 2019, 19, e00454. [Google Scholar] [PubMed]
- Clarke, A.M.; Kuosmanen, T.; Barry, M.M. A Systematic Review of Online Youth Mental Health Promotion and Prevention Interventions. J. Youth Adolesc. 2015, 44, 90–113. [Google Scholar] [CrossRef]
- Payton, J.; Weissberg, R.P.; Durlak, J.A.; Dymnicki, A.B.; Taylor, R.D.; Schellinger, K.B.; Pachan, M. The Positive Impact of Social and Emotional Learning for Kindergarten to Eighth-Grade Students: Findings from Three Scientific Reviews; Collaborative for Academic, Social, and Emotional Learning: Chicago, IL, USA, 2008. Available online: https://files.eric.ed.gov/fulltext/ED505370.pdf (accessed on 19 February 2021).
- Fazel, M.; Hoagwood, K.; Stephan, S.; Ford, T. Mental health interventions in schools in high-income countries. Lancet Psychiatry 2014, 1, 377–387. [Google Scholar] [CrossRef]
- World Health Organization Regional Office for Europe (WHO Europe). Health Literacy. The Solid Facts. Available online: https://apps.who.int/iris/bitstream/handle/10665/128703/e96854.pdf (accessed on 17 May 2020).
- Glasziou, P.; Irwig, L.; Bain, C.; Colditz, G. Systematic Reviews in Health Care. A Practical Guide; Cambridge University Press: Cambridge, UK, 2004. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Long, M.W.; Albright, G.; McMillan, J.; Shockley, K.M.; Price, O.A. Enhancing Educator Engagement in School Mental Health Care Through Digital Simulation Professional Development. J. Sch. Health 2018, 88, 651–659. [Google Scholar] [CrossRef] [PubMed]
- Pereira, C.A.; Wen, C.L.; Miguel, E.C.; Polanczyk, G.V. A randomised controlled trial of a web-based educational program in child mental health for schoolteachers. Eur. Child Adolesc. Psychiatry 2014, 24, 931–940. [Google Scholar] [CrossRef] [PubMed]
- Barnett, B.; Corkum, P.; Elik, N. A web-based intervention for elementary school teachers of students with attention-deficit/hyperactivity disorder (ADHD). Psychol. Serv. 2012, 9, 227–230. [Google Scholar] [CrossRef]
- Shum, A.K.; Lai, E.S.; Leung, W.G.; Cheng, M.N.; Wong, H.K.; So, S.W.; Law, Y.W.; Yip, P.S.; Amresh, A.; Katz, D.; et al. A Digital Game and School-Based Intervention for Students in Hong Kong: Quasi-Experimental Design. J. Med. Internet Res. 2019, 21, e12003. [Google Scholar] [CrossRef]
- Sanders, S.; Lane, J.J.; Losinski, M.; Nelson, J.; Asiri, A.; Holloway, S.M.K.; Rogers, E. An Implementation of a Computerized Cognitive Behavioral Treatment Program to Address Student Mental Health Needs: A Pilot Study in an After-School Program. Prof. Sch. Couns. 2018, 22, 1–9. [Google Scholar] [CrossRef]
- Attwood, M.; Meadows, S.; Stallard, P.; Richardson, T. Universal and targeted computerised cognitive behavioural therapy (Think, Feel, Do) for emotional health in schools: Results from two exploratory studies. Child Adolesc. Ment. Health 2012, 17, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Costello, E.J.; Mustillo, S.; Erkanli, A.; Keeler, G.; Angold, A. Prevalence and Development of Psychiatric Disorders in Childhood and Adolescence. Arch. Gen. Psychiatry 2003, 60, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Sutan, R.; Ezdiani, N.M.; Muhammad, A.A.R.; Diyana, M.M.; Mokhtar, D.; Rahman, R.A.; Johani, F.H.; Bin Abd Majid, M.S.; Mohd Fauzi, M.F.; Haneef Azme, M.; et al. Systematic Review of School-Based Mental Health Intervention among Primary School Children. J. Community Med. Health Educ. 2018, 8, 589. [Google Scholar]
- Bevan Jones, R.; Stallard, P.; Agha, S.S.; Rice, S.; Werner-Seidler, A.; Stasiak, K.; Kahn, J.; Simpson, S.A.; Alvarez-Jimenez, M.; Rice, F.; et al. Simpson Mario Alvarez-Jimenez Frances Rice et al. Practitioner review: Co-design of digital mental health technologies with children and young people. J Child Psychol. Psychiatry 2020, 61, 928–940. [Google Scholar] [CrossRef]
- Knitzer, J.; Cooper, J. Beyond Integration: Challenges for Children’s Mental Health. Health Aff. 2006, 25, 670–679. [Google Scholar] [CrossRef]
- Hollis, C.; Falconer, C.J.; Martin, J.L.; Whittington, C.; Stockton, S.; Glazebrook, C.; Davies, E.B. Annual Research Review: Digital health interventions for children and young people with mental health problems—A systematic and meta-review. J. Child Psychol. Psychiatry 2017, 58, 474–503. [Google Scholar] [CrossRef] [PubMed]
- Kollins, S.H.; DeLoss, D.J.; Cañadas, E.; Lutz, J.; Findling, R.L.; Keefe, R.S.E.; Epstein, J.N.; Cutler, A.J.; Faraone, S.V. A novel digital intervention for actively reducing severity of paediatric ADHD (STARS-ADHD): A randomised controlled trial. Lancet Digit. Health 2020, 2, e168–e178. [Google Scholar] [CrossRef]
- Podina, I.R.; Mogoase, C.; David, D.; Szentagotai, A.; Dobrean, A. A Meta-Analysis on the Efficacy of Technology Mediated CBT for Anxious Children and Adolescents. J. Ration. Cogn. Ther. 2016, 34, 31–50. [Google Scholar] [CrossRef]
- Vigerland, S.; Ljótsson, B.; Thulin, U.; Öst, L.-G.; Andersson, G.; Serlachius, E. Internet-delivered cognitive behavioural therapy for children with anxiety disorders: A randomised controlled trial. Behav. Res. Ther. 2016, 76, 47–56. [Google Scholar] [CrossRef]
- Storch, E.A.; Salloum, A.; King, M.A.; Crawford, E.A.; Andel, R.; McBride, N.M.; Lewin, A.B. A randomized controlled trial in community mental health centers of computer-assisted cognitive behavioral therapy versus treatment as usual for children with anxiety. Depress. Anxiety 2015, 32, 843–852. [Google Scholar] [CrossRef]
- Ebert, D.D.; Zarski, A.-C.; Christensen, H.; Stikkelbroek, Y.; Cuijpers, P.; Berking, M.; Riper, H. Internet and Computer-Based Cognitive Behavioral Therapy for Anxiety and Depression in Youth: A Meta-Analysis of Randomized Controlled Outcome Trials. PLoS ONE 2015, 10, e0119895. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Bapuji, S.B.; Winters, S.E.; Struthers, A.; Raynard, M.; Metge, C.; Kreindler, S.A.; Charette, C.J.; Lemaire, J.A.; Synyshyn, M.; et al. Effectiveness of internet-based interventions for children, youth, and young adults with anxiety and/or depression: A systematic review and meta-analysis. BMC Health Serv. Res. 2014, 14, 313. [Google Scholar] [CrossRef] [PubMed]
- Van Vliet, H.; Andrews, G. Internet-Based Course for the Management of Stress for Junior High Schools. Aust. N. Z. J. Psychiatry 2009, 43, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Parisod, H.; Pakarinen, A.; Kauhanen, L.; Aromaa, M.; Leppänen, V.; Liukkonen, T.N.; Smed, J.; Salanterä, S. Promoting children’s health with digital games: A review of reviews. Games Health J. 2014, 3, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Charlier, N.; Zupancic, N.; Fieuws, S.; Denhaerynck, K.; Zaman, B.; Moons, P. Serious games for improving knowledge and self-management in young people with chronic conditions: A systematic review and meta-analysis. J. Am. Med. Inform. Assoc. 2016, 23, 230–239. [Google Scholar] [CrossRef]
- Tark, R.; Metelitsa, M.; Akkermann, K.; Saks, K.; Mikkel, S.; Haljas, K. Usability, Acceptability, Feasibility, and Effectiveness of a Gamified Mobile Health Intervention (Triumf) for Pediatric Patients: Qualitative Study. JMIR Serious Games 2019, 7, e13776. [Google Scholar] [CrossRef]
- Bergin, A.D.; Vallejos, E.P.; Davies, E.B.; Daley, D.; Ford, T.; Harold, G.; Hetrick, S.; Kidner, M.; Long, Y.; Merry, S.; et al. Preventive digital mental health interventions for children and young people: A review of the design and reporting of research. NPJ Digit. Med. 2020, 3, 1–9. [Google Scholar] [CrossRef]
| Inclusion Criteria |
| 1. Articles written in English language |
| 2. Empirical studies |
| 3. Dissertations and/or case reports |
| 4. Organizational reports and guidelines |
| 5. Intervention studies |
| 6. Conducted in primary school settings |
| 7. Participants were any staff members and/or students of primary schools |
| Exclusion Criteria |
| 1. Systematic and meta-analyses articles |
| 2. Not intervention studies |
| 3. Did not use digital mental health interventions |
| 4. Editorials and/or commentaries |
| 5. Book reviews and/or letters |
| 6. Articles not focused on mental health and wellbeing of primary school children |
| 7. Study protocols |
| Author/Year | Country | Study Aim | Number of Participants | Content of Intervention | Duration of Intervention | Evaluation Tools/Test Timing | Intervention Outcomes |
|---|---|---|---|---|---|---|---|
| Sanders et al., 2019 | USA | To address the feasibility and effectiveness of an abbreviated cCBT software program, “Camp Cope-A-Lot” (CCAL), for elementary students at risk for anxiety and other behavioral problems. | 26 students (7–11 years) -Treatment group (n = 11) -Control group (n = 15) | The abbreviated cCBT software program, Camp Cope-A-Lot (CCAL) | 6 sessions lasting 20–30 min for 4 weeks | -Beck Anxiety Inventory for Youth (BAI-Y) -BASC—Behavioral -Emotional Screening System (BASC-3 BESS -Children’s Usage Rating Profile (CURP) -Usage Rating Profile–Intervention Revised (URP-IR) All administered at the end of the CCAL program. | Successful impact to ease the internalizing symptoms of students in an after-school setting. |
| Shum et al., 2019 | Hong Kong—China | To examine the effectiveness of a school-based digital game-based intervention program “DoReMiFa” with the combination of a CBT and positive psychology model. | 459 children (8 to 12 years) -Intervention group (n = 264) -Control group (n = 195) | -The Adventures of DoReMiFa, a digital game–based lesson -School-based lesson | 11 digital game-based lessons lasting around 25 to 60 min/lesson | -The Screen for Child Anxiety-Related Emotional Disorders -Mental Health Knowledge Checklist -Children’s Automatic Thoughts Scale-Negative or Positive -Interpersonal Reactivity Index -Rosenberg Self-Esteem Scale Administered at: -preintervention stage -2 weeks after completion of -6-month follow-up | Effective results in the mental health knowledge even 6 months after the intervention. |
| Long et al., 2018 | U.S.A. | To evaluate the impact of the “At-Risk for Elementary School Educators” online mental health role-play simulation for elementary school teachers to confront students with psychological distress. | 18,896 elementary school teachers (mean age 41 years). -Intervention group (n = 9427) -Control group (n = 9469). | At-Risk for Elementary School Educators, a self-paced online simulation. | A 45 to 90 min online role-play simulation | The Gatekeeper Behavior Scale: -at baseline -post-test -3-month follow-up | Effective results in teacher’s preparedness, likelihood, and self-efficacy to perform positive gatekeeping behaviors for students with psychological distress. |
| Pereira and Wen, 2015 | Brazil | To develop a web-based program, to educate primary school teachers on child mental disorders and to test its effectiveness compared with other methods delivered or with no intervention. | 115 teachers (mean age 40.3) -Web-based interactive education (WBIE) group (n = 52) -Text- and video-based education (TVBE) group (n = 32) -Waiting list (WL, no intervention) (n = 31). | -Educational videos -Website tutorial -Internet discussion forum -Web conference -Written support text | 9 h of training (three-hour session/week for 3 weeks) | Questionnaires assessing knowledge, beliefs and attitudes: -at the preintervention stage- immediately after the intervention | -Τhe WBIE group showed greater gains in knowledge than other groups. -The WL group gained more knowledge than did those trained with the text- and video-based program. |
| Attwood et al., 2012 | UK | To evaluate the computerized CBT program “Think, Feel, Do” in two studies: Study 1: a universal study Study 2: targeted at children with mild/ moderate emotional problems of anxiety or low mood. | -Study 1: 13 boys (10 and 12 years). -Study 2: 12 children (9 boys and 3 girls) (10 to 16 yr) | -Study 1: Boys were assigned to either cCBT or a matched computer time (gaming) condition. -Study 2: The cCBT was delivered by the school nurse. “Think, Feel, Do” consisted of quizzes, practical exercises, video clips, music and animation was delivered. Online games were also used. | 6 sessions lasting 45 min/week or every 2 weeks, during class time. | -Spence Children’s Anxiety Scale Child and Parent Version (SCAS) -Adolescent Well-Being Scale (AWS) -Rosenberg Self Esteem Inventory (RSEI) -Schema Questionnaire for Children (SQC) Assessments were completed within two weeks after the completion of the intervention | The cCBT “Think, Feel, Do” can have positive effects on anxiety and low mood symptoms |
| Barnett et al., 2012 | Canada | To determine whether a web-based medium is an effective tool for supporting knowledge, attitude, and behavior changes in teachers of elementary school children with ADHD. | 19 elementary school teachers (mean age 36.9 years) | -Discussion Board -Intrasystem email -Web links | 7 sessions: 1 session/week | Self-report measures after the intervention | Increased knowledge on managing ADHD in the classroom was documented. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sakellari, E.; Notara, V.; Lagiou, A.; Fatkulina, N.; Ivanova, S.; Korhonen, J.; Kregar Velikonja, N.; Lalova, V.; Laaksonen, C.; Petrova, G.; et al. Mental Health and Wellbeing at Schools: Health Promotion in Primary Schools with the Use of Digital Methods. Children 2021, 8, 345. https://doi.org/10.3390/children8050345
Sakellari E, Notara V, Lagiou A, Fatkulina N, Ivanova S, Korhonen J, Kregar Velikonja N, Lalova V, Laaksonen C, Petrova G, et al. Mental Health and Wellbeing at Schools: Health Promotion in Primary Schools with the Use of Digital Methods. Children. 2021; 8(5):345. https://doi.org/10.3390/children8050345
Chicago/Turabian StyleSakellari, Evanthia, Venetia Notara, Areti Lagiou, Natalja Fatkulina, Svetla Ivanova, Joonas Korhonen, Nevenka Kregar Velikonja, Valentina Lalova, Camilla Laaksonen, Gergana Petrova, and et al. 2021. "Mental Health and Wellbeing at Schools: Health Promotion in Primary Schools with the Use of Digital Methods" Children 8, no. 5: 345. https://doi.org/10.3390/children8050345
APA StyleSakellari, E., Notara, V., Lagiou, A., Fatkulina, N., Ivanova, S., Korhonen, J., Kregar Velikonja, N., Lalova, V., Laaksonen, C., Petrova, G., & Lahti, M. (2021). Mental Health and Wellbeing at Schools: Health Promotion in Primary Schools with the Use of Digital Methods. Children, 8(5), 345. https://doi.org/10.3390/children8050345








