Venous Malformations and Blood Coagulation in Children
Abstract
1. Introduction
2. Materials and Methods
Statistics
3. Results
3.1. Patient Characteristics
3.2. Blood Cell Count
3.3. Coagulation Screening Tests and D-Dimer
3.4. Coagulation Factors and Antithrombin
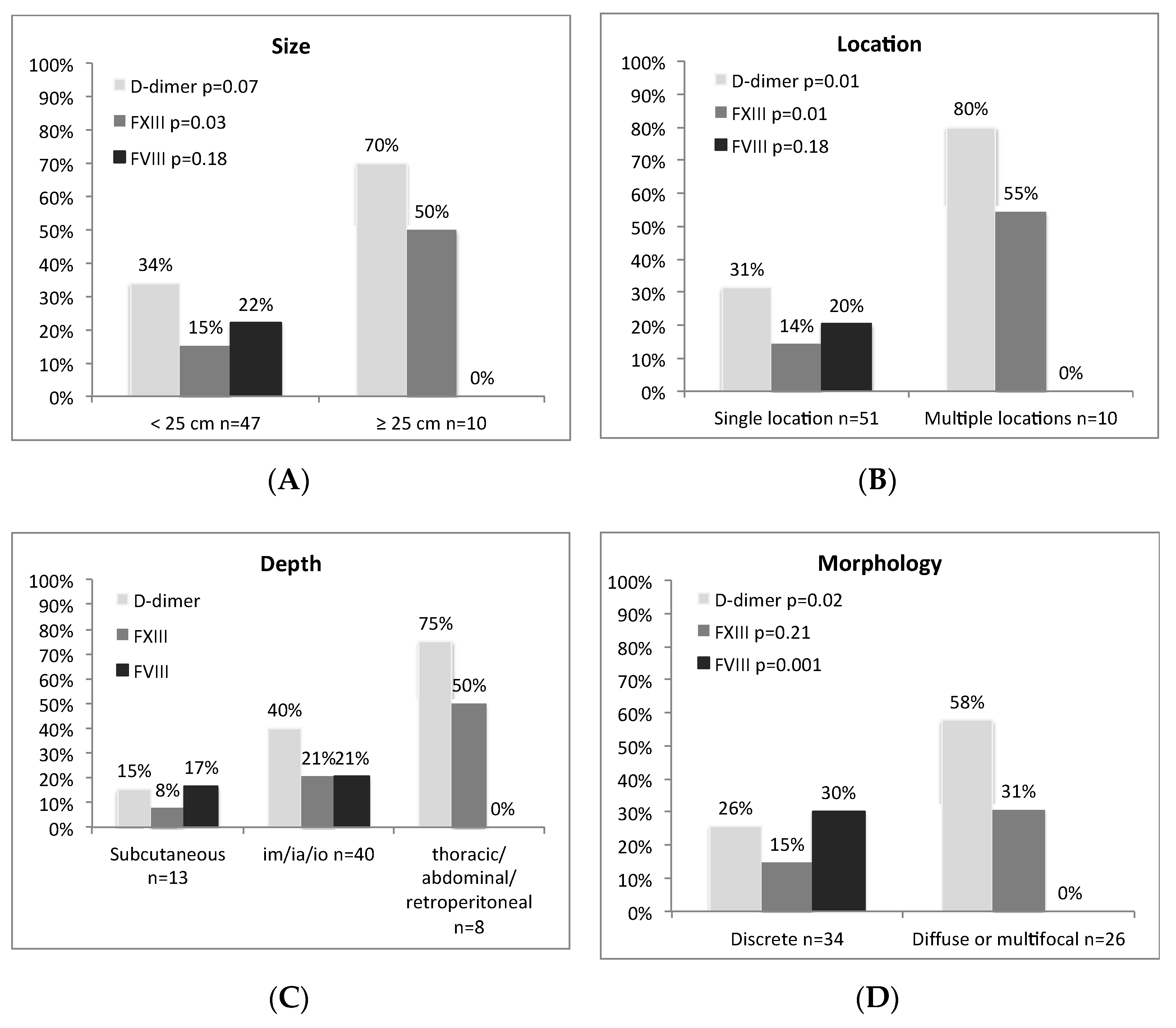
3.5. Associations with the Clinical Features of Malformations
3.6. Complications
3.7. Anticoagulant Therapy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Dasgupta, R.; Fishman, S.J. ISSVA classification. Semin. Pediatr. Surg. 2014, 23, 158–161. [Google Scholar] [CrossRef]
- Dompmartin, A.; Ballieux, F.; Thibon, P.; Lequerrec, A.; Hermans, C.; Clapuyt, P.; Barrellier, M.-T.; Hammer, F.; Labbé, D.; Vikkula, M.; et al. Elevated D-dimer level in the differential diagnosis of venous malformations. Arch. Dermatol. 2009, 145, 1239–1244. [Google Scholar] [CrossRef]
- Leung, M.W.Y.; Liu, C.S.W.; Fung, D.H.S.; Poon, W.L.; Yam, F.S.D.; Leung, Y.C.L.; Chung, K.L.Y.; Tang, P.M.Y.; Chao, N.S.Y.; Liu, K.K.W.; et al. Venous malformation and localized intravascular coagulopathy in children. Eur. J. Pediatr. Surg. 2016, 27, 181–184. [Google Scholar] [CrossRef] [PubMed]
- Dompmartin, A.; Acher, A.; Thibon, P.; Tourbach, S.; Hermans, C.; Deneys, V.; Pocock, B.; Lequerrec, A.; Labbé, D.; Barrellier, M.-T.; et al. Association of localized intravascular coagulopathy with venous malformations. Arch. Dermatol. 2008, 144, 873–877. [Google Scholar] [CrossRef] [PubMed]
- Mazoyer, E.; Enjolras, O.; Bisdorff, A.; Perdu, J.; Wassef, M.; Drouet, L. Coagulation disorders in patients with venous malformation of the limbs and trunk. Arch. Dermatol. 2008, 144, 861–867. [Google Scholar] [CrossRef]
- Mazereeuw-Hautier, J.; Syed, S.; Leisner, R.; Harper, J. Extensive venous/lymphatic malformations causing life-threatening haematological complications. Br. J. Dermatol. 2007, 157, 558–563. [Google Scholar] [CrossRef] [PubMed]
- Adams, D.M. Special considerations in vascular anomalies: Hematologic management. Clin. Plast. Surg. 2011, 38, 153–160. [Google Scholar] [CrossRef]
- Aronniemi, J.; Castrén, E.; Lappalainen, K.; Vuola, P.; Salminen, P.; Pitkäranta, A.; Pekkola, J. Sclerotherapy complications of peripheral venous malformations. Phlebol. J. Venous Dis. 2016, 31, 712–722. [Google Scholar] [CrossRef]
- Zhuo, K.Y.; Russell, S.; Wargon, O.; Adams, S. Localised intravascular coagulation complicating venous malformations in children: Associations and therapeutic options. J. Paediatr. Child Health 2017, 53, 737–741. [Google Scholar] [CrossRef]
- Griffin, C.T.; Srinivasan, Y.; Zheng, Y.-W.; Huang, W.; Coughlin, S.R. A role for thrombin receptor signaling in endothelial cells during embryonic development. Science 2001, 293, 1666–1670. [Google Scholar] [CrossRef]
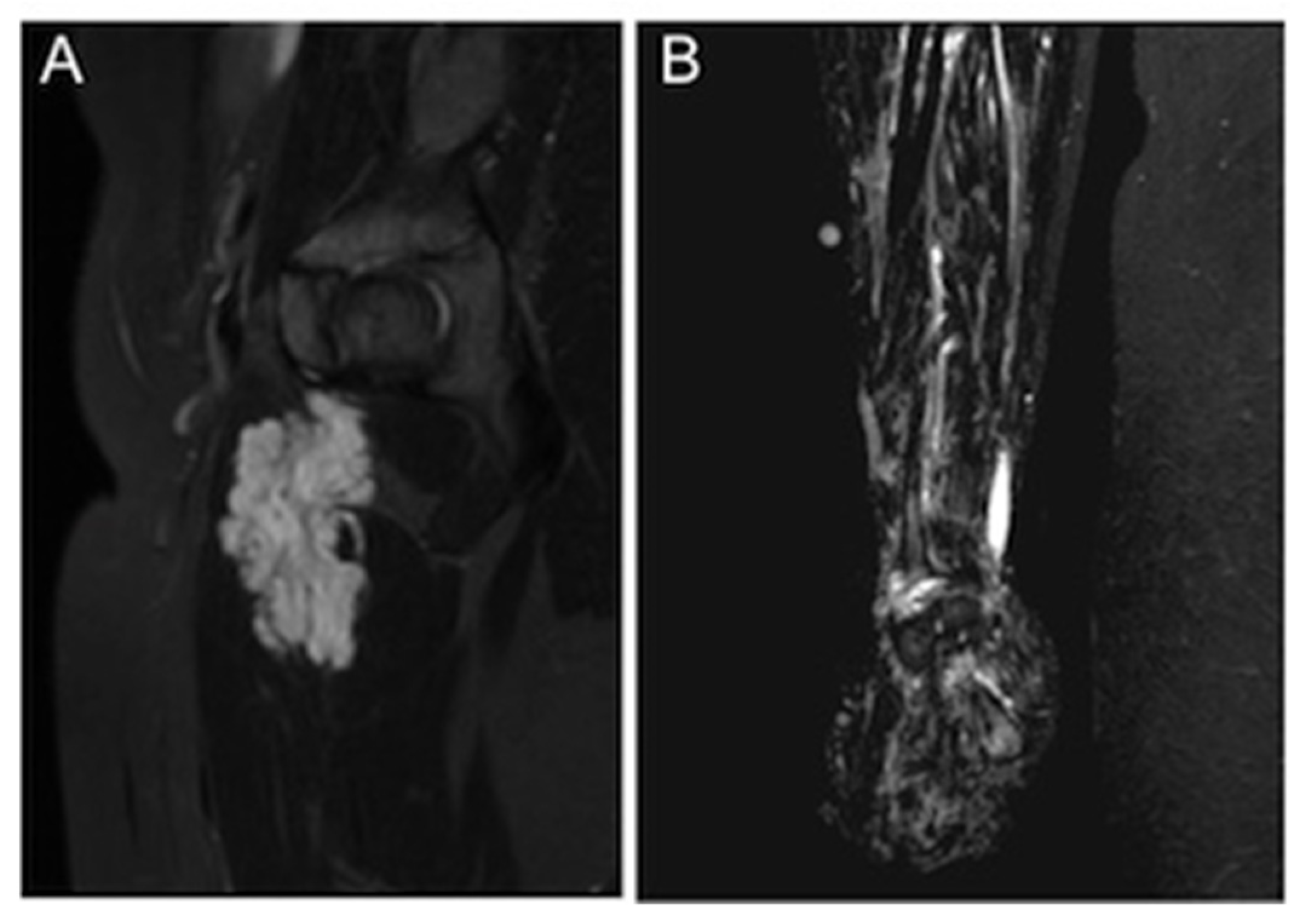
- Koo, K.S.H.; Dowd, C.F.; Mathes, E.F.; Rosbe, K.W.; Hoffman, W.Y.; Frieden, I.J.; Hess, C.P. MRI phenotypes of localized intravascular coagulopathy in venous malformations. Pediatr. Radiol. 2015, 45, 1690–1695. [Google Scholar] [CrossRef]
- Jenkins, P.V.; Rawley, O.; Smith, O.P.; O’Donnell, J.S. Elevated factor VIII levels and risk of venous thrombosis. Br. J. Haematol. 2012, 157, 653–663. [Google Scholar] [CrossRef] [PubMed]
- Bank, I.; Libourel, E.J.; Middeldorp, S.; Hamulyak, K.; Van Pampus, E.C.M.; Koopman, M.M.W.; Prins, M.H.; Van Der Meer, J.; Buller, H.R. Elevated levels of FVIII:C within families are associated with an increased risk for venous and arterial thrombosis. J. Thromb. Haemost. 2005, 3, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, G.E.; Sims, P.J.; Wiedmer, T.; Furie, B.; Furie, B.C.; Shattil, S.J. Platelet-derived Microparticles Express High Affinity Receptors for Factor VIII*. J. Biol. Chem. 1991, 266, 17261–17268. [Google Scholar] [CrossRef]
- Randi, A.M.; Laffan, M.A. Von Willebrand factor and angiogenesis: Basic and applied issues. J. Thromb. Haemost. 2017, 15, 13–20. [Google Scholar] [CrossRef]
- Hethershaw, E.L.; La Corte, A.L.C.; Duval, C.; Ali, M.; Grant, P.J.; Ariëns, R.A.S.; Philippou, H. The effect of blood coagulation factor XIII on fibrin clot structure and fibrinolysis. J. Thromb. Haemost. 2014, 12, 197–205. [Google Scholar] [CrossRef]
- Kattula, S.; Byrnes, J.R.; Wolberg, A.S. Fibrinogen and fibrin in hemostasis and thrombosis. Arter. Thromb. Vasc. Biol. 2017, 37, e13–e21. [Google Scholar] [CrossRef] [PubMed]
- Pitkänen, H.H.; Jouppila, A.; Lemponen, M.; Ilmakunnas, M.; Ahonen, J.; Lassila, R. Factor XIII deficiency enhances thrombin generation due to impaired fibrin polymerization—An effect corrected by Factor XIII replacement. Thromb. Res. 2017, 149, 56–61. [Google Scholar] [CrossRef][Green Version]
- Nguyen, H.-L.; Boon, L.M.; Vikkula, M. Genetics of vascular malformations. Semin. Pediatr. Surg. 2014, 23, 221–226. [Google Scholar] [CrossRef]
- Nätynki, M.; Kangas, J.; Miinalainen, I.; Sormunen, R.; Pietilä, R.; Soblet, J.; Boon, L.M.; Vikkula, M.; Limaye, N.; Eklund, L. Common and specific effects of TIE2 mutations causing venous malformations. Hum. Mol. Genet. 2015, 24, 6374–6389. [Google Scholar] [CrossRef]
- Appel, I.M.; Grimminck, B.; Geerts, J.; Stigter, R.; Cnossen, M.H.; Beishuizen, A. Age dependency of coagulation parameters during childhood and puberty. J. Thromb. Haemost. 2012, 10, 2254–2263. [Google Scholar] [CrossRef]
- Mammen, E. Antithrombin: Its physiological importance and role in DIC. Semin. Thromb. Hemost. 1998, 24, 19–25. [Google Scholar] [CrossRef]
- Aird, W. Vascular bed-specific thrombosis. J. Thromb. Haemost. 2014, 5, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Toulon, P.; Berruyer, M.; Brionne-François, M.; Grand, F.; Lasne, D.; Telion, C.; Arcizet, J.; Giacomello, R.; De Pooter, N. Age dependency for coagulation parameters in paediatric populations. Thromb. Haemost. 2016, 116, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Toulon, P. Developmental hemostasis: Laboratory and clinical implications. Int. J. Lab. Hematol. 2016, 38, 66–77. [Google Scholar] [CrossRef] [PubMed]
- Di Blasio, L.; Puliafito, A.; Gagliardi, P.A.; Comunanza, V.; Somale, D.; Chiaverina, G.; Bussolino, F.; Primo, L. PI3K/mTOR inhibition promotes the regression of experimental vascular malformations driven by PIK3CA-activating mutations. Cell Death Dis. 2018, 9, 45. [Google Scholar] [CrossRef]


| N (%) or Median (Range) | |
|---|---|
| Patients | 62 |
| Male | 27 (44) |
| Female | 35 (56) |
| Age | 11.4 (1.1–19.4) |
| Lesion size (cm) (excluding multifocal lesions) | |
| <5 | 15 (24.2) |
| 5–10 | 18 (29) |
| 10–25 | 14 (22.6) |
| >25 | 10 (16.1) |
| Lesion morphology | |
| Multifocal | 5 (8.1) |
| Diffuse, infiltrating | 22 (35.5) |
| Discrete, well-demarcated | 35 (56.5) |
| Lesion location | |
| Head and neck | 2 (3.2) |
| Trunk | 5 (8.1) |
| Extremities | 44 (71.0) |
| Multiple locations | 11 (17.7) |
| Lesion depth | |
| Subcutaneous only | 13 (21.0) |
| ia/io/im component | 40 (64.5) |
| abd./retroperit./thoracic | 9 (14.5) |
| Diagnosis | |
| VM | 55 (88.7) |
| Combined: | 7 (11.3) |
| LVM | 4 (6.5) |
| CVM | 2 (3.2) |
| LCVM | 1 (1.6) |
| Biomarker | Reference Limit | N | Median | Range | Values below Reference Range N (%) | Values above Reference Range N (%) |
|---|---|---|---|---|---|---|
| Leukocytes (E9/L) | 5–14 | 57 | 5.8 | 2.8–14.9 | 19 (33.3) | 1 (1.8) |
| FV (IU/dL) | 79–128 | 61 | 102 | 56–136 | 6 (9.8) | 2 (3.3) |
| FVIII (IU/dL) | 52–148 | 60 | 119.5 | 75–206 | 0 | 10 (16.7) |
| FXIII (IU/dL) | 76–156 | 60 | 95.5 | 53–141 | 12 (20.0) | 0 |
| Antithrombin (%) | 84–108 | 62 | 110.0 | 84–134 | 0 | 34 (54.8) |
| D-dimer (mg/L) | <0.5 | 61 | 0.3 | 0.1–15.1 | 0 | 24 (39.3) |
| Fibrinogen (g/L) | 1.7–4 | 60 | 2.85 | 0.0–5.2 | 1 (1.7) | 6 (10.0) |
| VWF:RCo (%) | 44–183 | 53 | 82.0 | 44–220 | 0 | 2 (3.8) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aronniemi, J.; Långström, S.; Mattila, K.A.; Mäkipernaa, A.; Salminen, P.; Pitkäranta, A.; Pekkola, J.; Lassila, R. Venous Malformations and Blood Coagulation in Children. Children 2021, 8, 312. https://doi.org/10.3390/children8040312
Aronniemi J, Långström S, Mattila KA, Mäkipernaa A, Salminen P, Pitkäranta A, Pekkola J, Lassila R. Venous Malformations and Blood Coagulation in Children. Children. 2021; 8(4):312. https://doi.org/10.3390/children8040312
Chicago/Turabian StyleAronniemi, Johanna, Satu Långström, Katariina A. Mattila, Anne Mäkipernaa, Päivi Salminen, Anne Pitkäranta, Johanna Pekkola, and Riitta Lassila. 2021. "Venous Malformations and Blood Coagulation in Children" Children 8, no. 4: 312. https://doi.org/10.3390/children8040312
APA StyleAronniemi, J., Långström, S., Mattila, K. A., Mäkipernaa, A., Salminen, P., Pitkäranta, A., Pekkola, J., & Lassila, R. (2021). Venous Malformations and Blood Coagulation in Children. Children, 8(4), 312. https://doi.org/10.3390/children8040312





