Evaluation of Cumulative Effect of Standard Triple Immunosuppression on Prevention of De Novo Donor Specific Antibodies (dnDSA) Production in Children after Kidney Transplantation—A Retrospective and Prospective Study
Abstract
1. Introduction
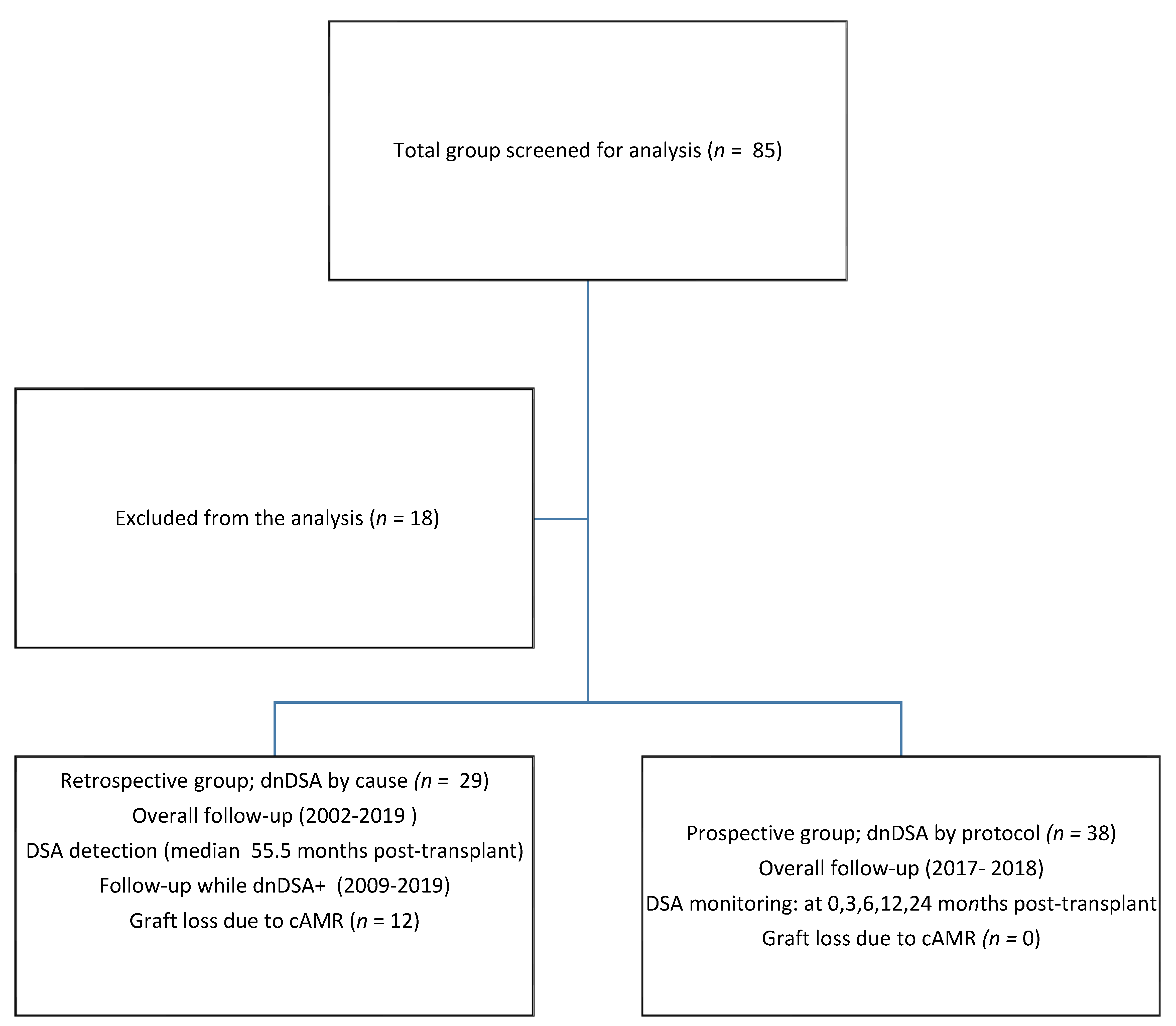
2. Materials and Methods
Statistical Analysis
3. Results
Summary of Results
- -
- The incidence of dnDSA was regularly increasing in a prospective group (DSA screening by protocol) with time after transplantation and was 8% at 3 months, 11% at 6, 16% at 14 and finally reached 21% after 2 years of follow-up;
- -
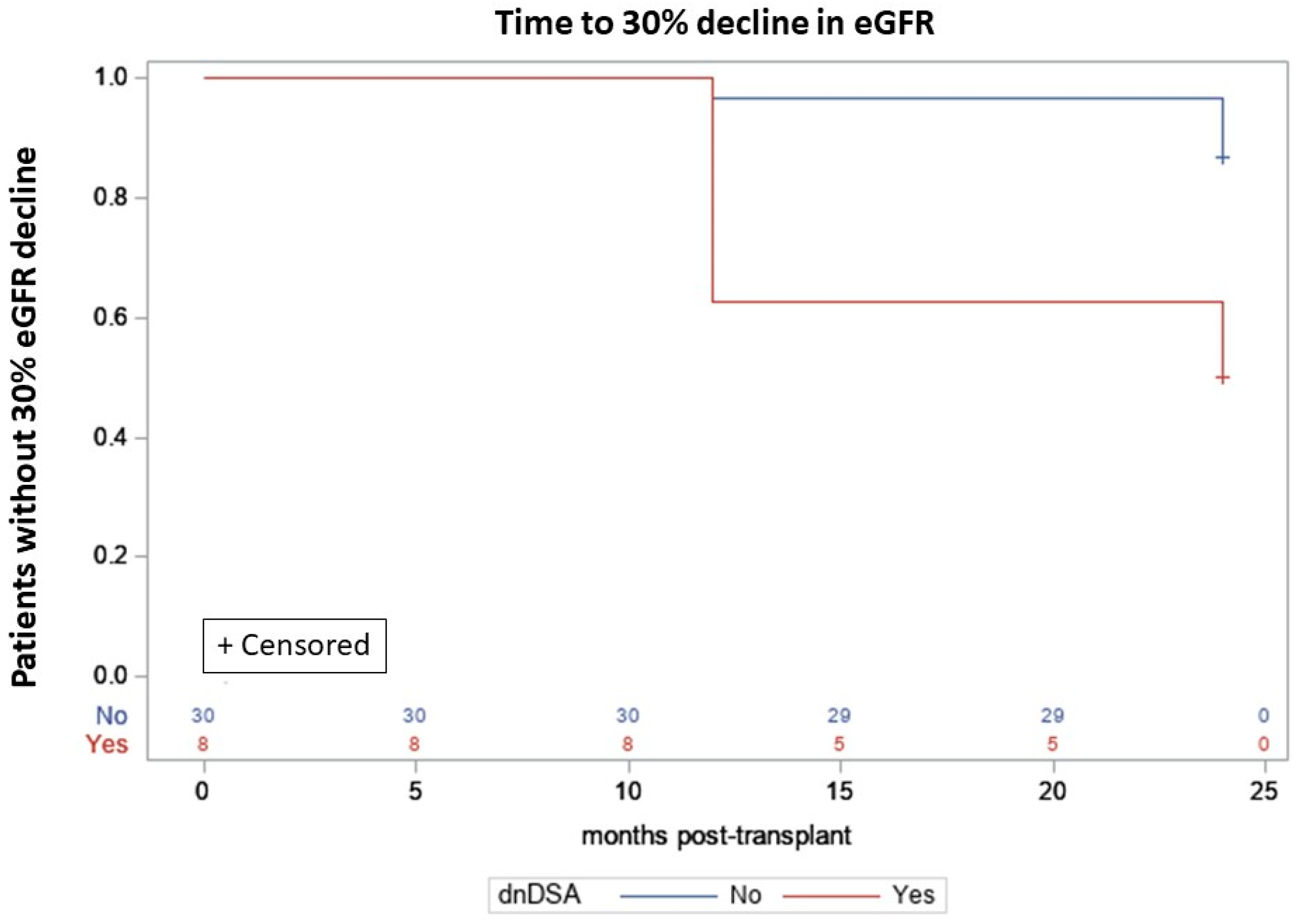
- The presence of the dnDSA in patients from the prospective group, was associated with a >4.5 higher risk of inferior graft function expressed as a chronic decrease of eGFR by ≥30% from baseline within 2-year follow-up;
- -
- A median value of all consecutive evaluations (from >1 to 24 months after transplantation) of blood TAC C0 was in the dnDSA- negative patients significantly higher than in the dnDSA- positive patients in a prospective group (7.9 ng/mL vs. 7.1 ng/mL; p = 0.0088);
- -
- dsDSA- positive and the dnDSA -negative patients did not differ significantly in terms of TAC C0 variability, evaluated during 2-year follow-up;
- -
- Vasudev score was not significantly different between the dnDSA-seronegative and dnDSA- positive patients at 1, 12 and 24 months after transplantation.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, J.J.; Balasubramanian, R.; Michaelides, G.; Wittenhagen, P.; Sebire, N.J.; Mamode, N.; Shaw, O.; Vaughan, R.; Marks, S.D. The clinical spectrum of de novo donor-specific antibodies in pediatric renal transplant recipients. Am. J. Transplant. 2014, 14, 2350–2358. [Google Scholar] [CrossRef]
- Zhang, R. Donor-Specific Antibodies in Kidney Transplant Recipients. Clin. J. Am. Soc. Nephrol. 2018, 13, 182–192. [Google Scholar] [CrossRef]
- Wiebe, C.; Gibson, I.W.; Blydt-Hansen, T.D.; Karpinski, M.; Ho, J.; Storsley, L.J.; Goldberg, A.; Birk, P.E.; Rush, D.N.; Nickerson, P.W. Evolution and clinical pathologic correlations of de novo donor-specific HLA antibody post kidney transplant. Am. J. Transplant. 2012, 12, 1157–1167. [Google Scholar] [CrossRef]
- Sellarés, J.; De Freitas, D.G.; Mengel, M.; Reeve, J.; Einecke, G.; Sis, B.; Hidalgo, L.G.; Famulski, K.; Matas, A.; Halloran, P.F. Understanding the causes of kidney transplant failure: The dominant role of antibody-mediated rejection and nonadherence. Am. J. Transplant. 2012, 12, 388–399. [Google Scholar] [CrossRef]
- Ginevri, F.; Nocera, A.; Comoli, P.; Innocente, A.; Cioni, M.; Parodi, A.; Fontana, I.; Magnasco, A.; Nocco, A.; Tagliamacco, A.; et al. Posttransplant de novo donor-specific HLA antibodies identify pediatric kidney recipients at risk for late antibody-mediated rejection. Am. J. Transplant. 2012, 12, 3355–3362. [Google Scholar] [CrossRef]
- Tait, B.D.; Süsal, C.; Gebel, H.M.; Nickerson, P.W.; Zachary, A.A.; Claas, F.H.; Reed, E.F.; Bray, R.A.; Campbell, P.; Chapman, J.R.; et al. Consensus guidelines on the testing and clinical management issues associated with HLA and non-HLA antibodies in transplantation. Transplantation 2013, 95, 19–47. [Google Scholar] [CrossRef]
- Engen, R.M.; Park, G.E.; Schumacher, C.S.; Gimferrer, I.; Warner, P.; Finn, L.S.; Weiss, N.S.; Smith, J.M. Donor-specific Antibody Surveillance and Graft Outcomes in Pediatric Kidney Transplant Recipients. Transplantation 2018, 102, 2072–2079. [Google Scholar] [CrossRef]
- O’Leary, J.G.; Samaniego, M.; Barrio, M.C.; Potena, L.; Zeevi, A.; Djamali, A.; Cozzi, E. The Influence of Immunosuppressive Agents on the Risk of De Novo Donor-Specific HLA Antibody Production in Solid Organ Transplant Recipients. Transplantation 2016, 100, 39–53. [Google Scholar] [CrossRef]
- Liefeldt, L.; Brakemeier, S.; Glander, P.; Waiser, J.; Lachmann, N. Donor-specific HLA antibodies in a cohort comparing everolimus with cyclosporine after kidney transplantation. Am. J. Transplant. 2012, 12, 1192–1198. [Google Scholar] [CrossRef]
- Pape, L. State-of-the-art immunosuppression protocols for pediatric renal transplant recipients. Pediatr. Nephrol. 2019, 34, 187–194. [Google Scholar] [CrossRef]
- Weber, L. Therapeutic drug monitoring in pediatric renal transplantation. Pediatr. Nephrol. 2015, 30, 253–265. [Google Scholar] [CrossRef]
- Todorova, E.K.; Huang, S.H.; Kobrzynski, M.C.; Filler, G. What is the intrapatient variability of mycophenolic acid trough levels? Pediatr. Transplant. 2015, 19, 669–674. [Google Scholar] [CrossRef] [PubMed]
- Forbes, N.; Schachter, A.D.; Yasin, A.; Sharma, A.P.; Filler, G. Limited sampling strategies for sirolimus after pediatric renal transplantation. Pediatr. Transplant. 2009, 13, 1020–1026. [Google Scholar] [CrossRef] [PubMed]
- Salvadori, M.; Bertoni, E. Is it time to give up with calcineurin inhibitors in kidney transplantation? World J. Transplant. 2013, 3, 7–25. [Google Scholar] [CrossRef]
- Vasudev, B.; Hariharan, S.; Hussain, S.A.; Zhu, Y.-R.; Bresnahan, B.A.; Cohen, E.P. BK virus nephritis: Risk factors, timing and outcome in renal transplant recipients. Kidney Int. 2005, 68, 1834–1839. [Google Scholar] [CrossRef] [PubMed]
- Höcker, B.; Fickenscher, H.; Delecluse, H.-J.; Böhm, S.; Küsters, U.; Schnitzler, P.; Pohl, M.; John, U.; Kemper, M.J.; Fehrenbach, H.; et al. Epidemiology and morbidity of Epstein-Barr virus infection in pediatric renal transplant recipients: A multicenter, prospective study. Clin. Infect. Dis. 2013, 56, 84–92. [Google Scholar] [CrossRef]
- Hiramitsu, T.; Tomosugi, T.; Futamura, K.; Okada, M.; Nishihira, M.; Goto, N.; Ichimori, T.; Narumi, S.; Kobayashi, T.; Uchida, K.; et al. Optimal blood levels of (extended-release) tacrolimus in living donor kidney transplantation to prevent de novo donor-specific antibody production: A retrospective cohort study. Int. Immunopharmacol. 2021, 91, 107038. [Google Scholar] [CrossRef] [PubMed]
- Pizzo, H.P.; Ettenger, R.B.; Gjertson, D.W.; Reed, E.F.; Zhang, J.; Gritsch, H.A.; Tsai, E.W. Sirolimus and tacrolimus coefficient of variation is associated with rejection, donor-specific antibodies, and nonadherence. Pediatr. Nephrol. 2016, 31, 2345–2352. [Google Scholar] [CrossRef]
- Rodrigo, E.; Segundo, D.S.; Fernández-Fresnedo, G.; López-Hoyos, M.; Benito, A.; Ruiz, J.C.; de Cos, M.A.; Arias, M. Within-Patient Variability in Tacrolimus Blood Levels Predicts Kidney Graft Loss and Donor-Specific Antibody Development. Transplantation 2016, 100, 2479–2485. [Google Scholar] [CrossRef]
- Aksoy, G.K.; Comak, E.; Koyun, M.; Akbaş, H.; Akkaya, B.; Aydınlı, B.; Uçar, F.; Akman, S. Tacrolimus Variability: A Cause of Donor-Specific Anti-HLA Antibody Formation in Children. Eur. J. Drug Metab. Pharmacokinet. 2019, 44, 539–548. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.; Colovai, A.; Del Rio, M.; Hayde, N. Tacrolimus variability is associated with de novo donor-specific antibody development in pediatric renal transplant recipients. Pediatr. Nephrol. 2020, 35, 261–270. [Google Scholar] [CrossRef]
- Hsiau, M.; Fernandez, H.; Gjertson, D.; Ettenger, R.B.; Tsai, E.W. Monitoring nonadherence and acute rejection with variation in blood immunosuppressant levels in pediatric renal transplantation. Transplantation 2011, 92, 918–922. [Google Scholar] [CrossRef]
- Schwartz, G.J.; Muñoz, A.; Schneider, M.F.; Mak, R.H.; Kaskel, F.; Warady, B.A.; Furth, S.L. New equations to estimate GFR in children with CKD. J. Am. Soc. Nephrol. 2009, 20, 629–637. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.; Lawrence, J.; Stockbridge, N. GFR decline and an end point in trials in CKD; viewpoint from FDA. Am. J. Kidney Dis. 2014, 64, 836–837. [Google Scholar] [CrossRef]
- Colombo, M.B.; Haworth, S.E.; Poli, F.; Nocco, A.; Puglisi, G.; Innocente, A.; Serafini, M.; Messa, P.; Scalamogna, M. Luminex technology for anti-HLA antibody screening: Evaluation of performance and of impact on laboratory routine. Cytom. B Clin. Cytom. 2007, 72, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Tait, B.D.; Hudson, F.; Cantwell, L.; Brewin, G.; Holdsworth, R.; Bennett, G.; Jose, M. Review article: Luminex technology for HLA antibody detection in organ transplantation. Nephrology 2009, 14, 247–254. [Google Scholar] [CrossRef]
- Haas, M.; Sis, B.; Racusen, L.C.; Solez, K.; Glotz, D.; Colvin, R.B.; Castro, M.C.R.; David, D.S.R.; Davidneto, E.; Bagnasco, S.M.; et al. Banff 2013 meeting report: Inclusion of c4d-negative antibody-mediated rejection and antibody-associated arterial lesions. Am. J. Transplant. 2014, 14, 272–283. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.C.; Reinsmoen, N.; Peng, A.; Lai, C.H.; Cao, K.; Villicana, R.; Toyoda, M.; Kahwaji, J.; Vo, A.A. Advances in diagnosing and managing antibody-mediated rejection. Pediatr. Nephrol. 2010, 25, 2035–2045. [Google Scholar] [CrossRef][Green Version]
- Magazine, D.A. Linear mixed-effects models for within-participant psychology experiments: An introductory tutorial and free, graphical user interface (LMMgui). Front. Psychol. 2015, 6, 2. [Google Scholar] [CrossRef]
- Lee, P.-C.; Zhu, L.; Terasaki, P.; Everly, M.J. HLA-specific antibodies developed in the first year posttransplant are predictive of chronic rejection and renal graft loss. Transplantation 2009, 88, 568–574. [Google Scholar] [CrossRef]
- Cioni, M.; Nocera, A.; Innocente, A.; Tagliamacco, A.; Trivelli, A.; Basso, S.; Quartuccio, G.; Fontana, I.; Magnasco, A.; Drago, F.; et al. De Novo Donor-Specific HLA Antibodies Developing Early or Late after Transplant Are Associated with the Same Risk of Graft Damage and Loss in Nonsensitized Kidney Recipients. J. Immunol. Res. 2017, 2017, 1747030. [Google Scholar] [CrossRef] [PubMed]
- Davis, S.; Gralla, J.; Klem, P.; Tong, S.; Wedermyer, G.; Freed, B.; Wiseman, A.; Cooper, J.E. Lower tacrolimus exposure and time in therapeutic range increase the risk of de novo donor-specific antibodies in the first year of kidney transplantation. Am. J. Transplant 2018, 18, 907–915. [Google Scholar] [CrossRef]
- Béland, M.-A.; Lapointe, I.; Noël, R.; Côté, I.; Wagner, E.; Riopel, J.; Latulippe, E.; Désy, O.; Béland, S.; Magee, C.N.; et al. Higher calcineurin inhibitor levels predict better kidney graft survival in patients with de novo donor-specific anti-HLA antibodies: A cohort study. Transpl. Int. 2017, 30, 502–509. [Google Scholar] [CrossRef]
- Gatault, P.; Kamar, N.; Büchler, M.; Colosio, C.; Bertrand, D.; Durrbach, A.; Albano, L.; Rivalan, J.; Le Meur, Y.; Essig, M.; et al. Reduction of Extended-Release Tacrolimus Dose in Low-Immunological-Risk Kidney Transplant Recipients Increases Risk of Rejection and Appearance of Donor-Specific Antibodies: A Randomized Study. Am. J. Transplant. 2017, 17, 1370–1379. [Google Scholar] [CrossRef] [PubMed]
- Yin, S.; Song, T.; Jiang, Y.; Li, X.; Fan, Y.; Lin, T. Tacrolimus Trough Level at the First Month May Predict Renal Transplantation Outcomes Among Living Chinese Kidney Transplant Patients: A Propensity Score-Matched Analysis. Ther. Drug Monit. 2019, 41, 308–316. [Google Scholar] [CrossRef]
- Wiebe, C.; Rush, D.N.; Nevins, T.E.; Birk, P.E.; Blydt-Hansen, T.; Gibson, I.W.; Goldberg, A.; Ho, J.; Karpinski, M.; Pochinco, D.; et al. Class II Eplet Mismatch Modulates Tacrolimus Trough Levels Required to Prevent Donor-Specific Antibody Development. J. Am. Soc. Nephrol. 2017, 28, 3353–3362. [Google Scholar] [CrossRef] [PubMed]
| Drug | Pediatric Score: Dose per Unit (mg/m2/d) | Immunosuppressive Unit |
|---|---|---|
| Tacrolimus (TAC) | 1.2 | 1 |
| Cyclosporin A (CsA) | 58 | 1 |
| Sirolimus (SRL) | 1.2 | 1 |
| Mycophenolate mofetil (MMF) | 290 | 1 |
| Azathioprine (AZA) | 58 | 1 |
| Prednisone (equivalent) | 2.9 | 1 |
| Retrospective Group (n = 29) Median (Q1–Q3) # n (%) | Prospective Group (n = 38) Median (Q1–Q3) n (%) | p | |
|---|---|---|---|
| Age, years | 8.1 (5.0–9.9) | 11.4 (8.0–14.5) | 0.002 |
| No. HLA-DR mismatches: 0/1/2 | 5/13/11 (17/45/38) | 8/25/5 (21/66/13) | 0.06 |
| No. HLA-B mismatches: 0/1/2 | 1/15/13 (3/52/45) | 2/19/17 (5/50/45) | 1 |
| No. HLA-A mismatches: 0/1/2 | 3/14/12 (10/48/41) | 4/19/15 (11/50/39) | 1 |
| HLA A+B+DR mismatches | 4 (3–5) | 4 (3–4) | 0.3 |
| Maintenance immunosuppression | |||
| TAC | 25 (86.2) | 31 (81.6) | 0.75 |
| CsA | 7 (24.1) | 7 (18.4) | 0.57 |
| MMF | 25 (86.2) | 37 (97.4) | 0.16 |
| Pred | 29 (100) | 38 (100) | N/A |
| Baseline eGFR (mL/min/1.73 m2), | 72.8 | 76.4 | 0.27 |
| No. of patients with kidney biopsies | (53.6–93.1) | (70.3–99.5) | |
| 23 (79.3) | 10 (26.3) | <0.0001 | |
| Follow-up, years | 8 (6–11) | 2 (2–2) | <0.0001 |
| Incidence of dnDSA (%) after transplantation overall | 100 | 21 | N/A |
| at 3 months | N/A | 8 | N/A |
| at 6 months | N/A | 11 | N/A |
| at 12 months | N/A | 16 | N/A |
| at 2 years | N/A | 21 | N/A |
| Variable | Group | p | |
|---|---|---|---|
| Retro Median (Q1–Q3) n (%) | Pro Median (Q1–Q3) n (%) | ||
| Incidence of dnDSA | 29 (100) | 8 (21) | <0.0001 |
| eGFR at detection of dnDSA, mL/min/1.73 m2 | 41.0 (28.7–57.2) | 85.0 (55.0–92.5) | 0.004 |
| Incidence of biopsy proven rejection | 19 (66) | 7 (18) | <0.0001 |
| Incidence of graft loss in cAMR | 12 (41) | 0 | <0.0001 |
| Parameter | dnDSA (−) | dnDSA (+) | p |
|---|---|---|---|
| TAC C0 (ng/mL), median, (Q1–Q3) | 7.9 (6.5–10.3) | 7.1 (5.9–8.5) | 0.0088 ^ |
| TAC C0 coefficient of variation (%), median (Q1–Q3) | 31 (23–39) | 29 (17–37) | 0.56 |
| Vasudev Score, Median, (Q1–Q3) | dnDSA (−) | ndDSA (+) | p |
|---|---|---|---|
| 1 month after transplantation | 10.6 (8.6–12.5) | 10.5 (8.4–11.0) | NS ^ |
| 12 months after transplantation | 6.3 (5.5–7.0) | 6.1 (5.4–6.6) | NS ^ |
| 2 years after transplantation | 5.3 (4.1–6.0) | 4.1 (3.8–5.9) | NS ^ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Urzykowska, A.; Piątosa, B.; Grycuk, U.; Kowalewski, G.; Kułaga, Z.; Grenda, R. Evaluation of Cumulative Effect of Standard Triple Immunosuppression on Prevention of De Novo Donor Specific Antibodies (dnDSA) Production in Children after Kidney Transplantation—A Retrospective and Prospective Study. Children 2021, 8, 1162. https://doi.org/10.3390/children8121162
Urzykowska A, Piątosa B, Grycuk U, Kowalewski G, Kułaga Z, Grenda R. Evaluation of Cumulative Effect of Standard Triple Immunosuppression on Prevention of De Novo Donor Specific Antibodies (dnDSA) Production in Children after Kidney Transplantation—A Retrospective and Prospective Study. Children. 2021; 8(12):1162. https://doi.org/10.3390/children8121162
Chicago/Turabian StyleUrzykowska, Agnieszka, Barbara Piątosa, Urszula Grycuk, Grzegorz Kowalewski, Zbigniew Kułaga, and Ryszard Grenda. 2021. "Evaluation of Cumulative Effect of Standard Triple Immunosuppression on Prevention of De Novo Donor Specific Antibodies (dnDSA) Production in Children after Kidney Transplantation—A Retrospective and Prospective Study" Children 8, no. 12: 1162. https://doi.org/10.3390/children8121162
APA StyleUrzykowska, A., Piątosa, B., Grycuk, U., Kowalewski, G., Kułaga, Z., & Grenda, R. (2021). Evaluation of Cumulative Effect of Standard Triple Immunosuppression on Prevention of De Novo Donor Specific Antibodies (dnDSA) Production in Children after Kidney Transplantation—A Retrospective and Prospective Study. Children, 8(12), 1162. https://doi.org/10.3390/children8121162







