Utilization of Parallel Resources and Sociodemographic Factors in Treating Children with Complex Chronic Diseases: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
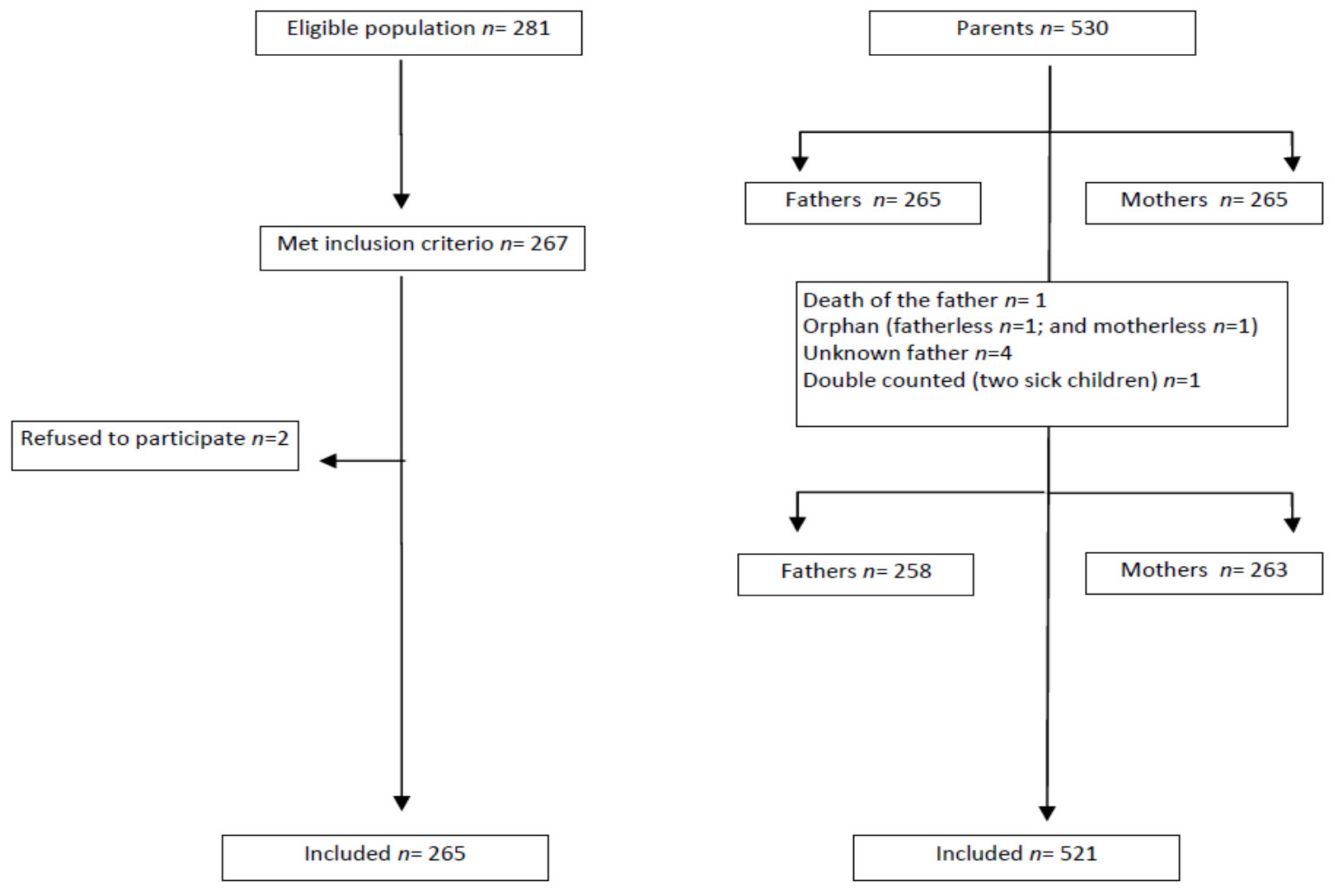
2.2. Participants
2.3. Data Collection
2.4. Analysis
3. Results
Healthcare Utilization and Sociodemographic Characteristics of the Parents
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Cohen, E.; Kuo, D.Z.; Agrawal, R.; Berry, J.G.; Bhagat, S.K.M.; Simon, T.D.; Srivastava, R. Children With Medical Complexity: An Emerging Population for Clinical and Research Initiatives. Pediatrics 2011, 127, 529–538. [Google Scholar] [CrossRef] [Green Version]
- Berry, J.G.; Hall, M.; Neff, J.M.; Goodman, D.; Cohen, E.; Agrawal, R.; Kuo, D.Z.; Feudtner, C. Children With Medical Complexity And Medicaid: Spending And Cost Savings. Health Aff. 2014, 33, 2199–2206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Looman, W.S.; Presler, E.; Erickson, M.M.; Garwick, A.W.; Cady, R.; Kelly, A.M.; Finkelstein, S.M. Care Coordination for Children With Complex Special Health Care Needs: The Value of the Advanced Practice Nurse’s Enhanced Scope of Knowledge and Practice. J. Pediatr. Health Care 2012, 27, 293–303. [Google Scholar] [CrossRef] [Green Version]
- Cady, R.G.; Belew, J.L. Parent Perspective on Care Coordination Services for Their Child with Medical Complexity. Children 2017, 4, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kingsnorth, S.; Lacombe-Duncan, A.; Keilty, K.; Bruce-Barrett, C.; Cohen, E.A. Inter-organizational partnership for children with medical complexity: The integrated complex care model. Care Health Dev. 2013, 41, 57–66. [Google Scholar] [CrossRef]
- Urbanos-Garrido, R. La desigualdad en el acceso a las prestaciones sanitarias. Propuestas para lograr la equidad. Gac. Sanit. 2016, 30, 25–30. [Google Scholar] [CrossRef] [Green Version]
- Lindly, O.J.; Chavez, A.; Zuckerman, K.E. Unmet Health Services Needs Among US Children with Developmental Disabilities: Associations with Family Impact and Child Functioning. J. Dev. Behav. Pediatr. 2016, 37, 712–723. [Google Scholar] [CrossRef]
- Bona, K.; Ms, T.M.B.; Neuberg, D.S.; Silverman, L.B.; Wolfe, J. Impact of Socioeconomic Status on Timing of Relapse and Overall Survival for Children Treated on Dana-Farber Cancer Institute ALL Consortium Protocols (2000–2010). Pediatr. Blood Cancer 2016, 63, 1012–1018. [Google Scholar] [CrossRef]
- Klitzner, T.S.; Rabbitt, L.A.; Chang, R.-K.R. Benefits of Care Coordination for Children with Complex Disease: A Pilot Medical Home Project in a Resident Teaching Clinic. J. Pediatr. 2010, 156, 1006–1010. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Vargas, P.; Tong, A.; Crowe, S.; Alexander, S.I.; Caldwell, P.; Campbell, D.E.; Couper, J.; Davidson, A.; De, S.; Fitzgerald, D.A.; et al. Research priorities for childhood chronic conditions: A workshop report. Arch. Dis. Child. 2018, 104, 237–245. [Google Scholar] [CrossRef]
- Bluebond-Langner, M.; Belasco, J.B.; Wander, M.D. “I Want to Live, Until I don’t Want to Live Anymore”: Involving Children with Life-Threatening and Life-Shortening Illnesses in Decision Making About Care and Treatment. Nurs. Clin. N. Am. 2010, 45, 329–343. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Datos de Población Municipal 2015; Observatorio de la Infancia en Andalucía (OIA): Granada, Spain, 2016.
- Junta de Andalucía. Instituto de Estadística y Cartografía de Andalucía. Sistema de Información Demográfica de Andalucía. Available online: http://www.juntadeandalucia.es/institutodeestadisticaycartografia/sid/index.htm (accessed on 31 January 2018).
- Feudtner, C.; Christakis, D.A.; Connell, F.A. Pediatric deaths attributable to complex chronic conditions: A population-based study of Washington State, 1980–1997. Pediatrics 2000, 106, 205–209. [Google Scholar]
- Domingo-Salvany, A.; Bacigalupe, A.; Carrasco, J.M.; Espelt, A.; Ferrando, J.; Borrell, C. Proposals for Social Class Classification Based on the Spanish National Classification of Occupations 2011 Using Neo-Weberian and Neo-Marxist Approaches. Gac. Sanit. 2013, 27, 263–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersen, R.M. Revisiting the Behavioral Model and Access to Medical Care: Does it Matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- De Araújo, C.A.C.; Paz-Lourido, B.; Gelabert, S.V. Tipos de apoyo a las familias con hijos con discapacidad y su influencia en la calidad de vida familiar. Ciência Saúde Coletiva 2016, 21, 3121–3130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Instituto Nacional de Estadística Encuesta Nacional de Salud. Asistencia Sanitaria. Available online: https://www.ine.es/dynt3/inebase/es/index.htm?type=pcaxis&path=/t15/p419/a2017/p02/&file=pcaxis (accessed on 28 December 2018).
- Prieto-Herraez, S.; González-Arteaga, T.; Calle, R.D.A. Public Healthcare: Citizen’s Preferences in Spain. Healthcare 2020, 8, 467. [Google Scholar] [CrossRef] [PubMed]
- Pinilla, J.; López-Valcárcel, B.G. Income and wealth as determinants of voluntary private health insurance: Empirical evidence in Spain, 2008–2014. BMC Public Health 2020, 20, 1262. [Google Scholar] [CrossRef] [PubMed]
- Al-Gharib, R.M.; Huijer, H.A.-S.; Darwish, H. Quality of care and relationships as reported by children with cancer and their parents. Ann. Palliat. Med. 2015, 4, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Bristow, S.; Jackson, D.; Shields, L.; Usher, K. The rural mother’s experience of caring for a child with a chronic health condition: An integrative review. J. Clin. Nurs. 2018, 27, 2558–2568. [Google Scholar] [CrossRef]
- Henriksson, A.; Årestedt, K. Exploring factors and caregiver outcomes associated with feelings of preparedness for caregiving in family caregivers in palliative care: A correlational, cross-sectional study. Palliat. Med. 2013, 27, 639–646. [Google Scholar] [CrossRef]
- Kearney, J.A.; Salley, C.; Muriel, A.C. Standards of Psychosocial Care for Parents of Children with Cancer. Pediatr. Blood Cancer 2015, 62, S632–S683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Law, E.F.; Fisher, E.; Fales, J.; Noel, M.; Eccleston, C. Systematic Review and Meta-Analysis of Parent and Family-Based Interventions for Children and Adolescents with Chronic Medical Conditions. J. Pediatr. Psychol. 2014, 39, 866–886. [Google Scholar] [CrossRef] [Green Version]
- López, C.G.; Escudero, M.B.; Montes, I.M.C.; Pérez, I.D. Análisis de las diferencias en la atención a la salud mental del niño y adolescente en España a través de los Planes Estratégicos de Salud Mental Autonómicos. Revista Psiquiatría Infanto-Juvenil 2019, 36, 20–30. [Google Scholar] [CrossRef]
- Jackson, A.; Liang, R.P.-T.; Frydenberg, E.; Higgins, R.O.; Murphy, B.M. Parent education programmes for special health care needs children: A systematic review. J. Clin. Nurs. 2016, 25, 1528–1547. [Google Scholar] [CrossRef]
- Dehoff, B.A.; Staten, L.K.; Rodgers, R.C.; Denne, S.C. The Role of Online Social Support in Supporting and Educating Parents of Young Children with Special Health Care Needs in the United States: A Scoping Review. J. Med. Internet Res. 2016, 18, e333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Didsbury, M.S.; Kim, S.; Medway, M.M.; Tong, A.; McTaggart, S.J.; Walker, A.M.; White, S.; Mackie, F.E.; Kara, T.; Craig, J.C.; et al. Socio-economic status and quality of life in children with chronic disease: A systematic review. J. Paediatr. Child Health 2016, 52, 1062–1069. [Google Scholar] [CrossRef]
- McClafferty, H.; Vohra, S.; Bailey, M.; Brown, M.; Esparham, A.; Gerstbacher, D.; Golianu, B.; Niemi, A.-K.; Sibinga, E.; Weydert, J.; et al. Pediatric Integrative Medicine. Pediatrics 2017, 140, e20171961. [Google Scholar] [CrossRef] [Green Version]
- Chen, S.-C.; Yu, B.Y.-M.; Suen, L.K.-P.; Yu, J.; Ho, F.Y.-Y.; Yang, J.-J.; Yeung, W.-F. Massage therapy for the treatment of attention deficit/hyperactivity disorder (ADHD) in children and adolescents: A systematic review and meta-analysis. Complement. Ther. Med. 2018, 42, 389–399. [Google Scholar] [CrossRef]
- Abdulah, D.M.; Abdulla, B.M.O. Effectiveness of group art therapy on quality of life in paediatric patients with cancer: A randomized controlled trial. Complement. Ther. Med. 2018, 41, 180–185. [Google Scholar] [CrossRef]
- Gilmer, M.J.; Baudino, M.N.; Goddard, A.T.; Vickers, D.C.; Akard, T.F. Animal-Assisted Therapy in Pediatric Palliative Care. Nurs. Clin. N. Am. 2016, 51, 381–395. [Google Scholar] [CrossRef] [PubMed]
- Gottschling, S.; Meyer, S.; Längler, A.; Ms, G.S.; Ebinger, F.; Gronwald, B. Differences in use of complementary and alternative medicine between children and adolescents with cancer in Germany: A population based survey. Pediatr. Blood Cancer 2013, 61, 488–492. [Google Scholar] [CrossRef]
- Italia, S.; Wolfenstetter, S.B.; Teuner, C.M. Patterns of Complementary and Alternative Medicine (CAM) use in children: A systematic review. Eur. J. Nucl. Med. Mol. Imaging 2014, 173, 1413–1428. [Google Scholar] [CrossRef]
- McCann, D.; Bull, R.; Winzenberg, T. The daily patterns of time use for parents of children with complex needs: A Systematic Review. J. Child Health Care 2012, 16, 26–52. [Google Scholar] [CrossRef] [PubMed]
- Marshik, P.L.; Kharat, A.A.; Jakeman, B.; Borrego, M.E.; Dodd, M.A.; Bachyrycz, A.; Anderson, J.R.; Bond, R.; Deming, P.; Mercier, R.-C.; et al. Complementary and Alternative Medicine and Therapy Use in a Diverse New Mexican Population. J. Altern. Complement. Med. 2016, 22, 45–51. [Google Scholar] [CrossRef]
- Schaible, B.; Colquitt, G.; Caciula, M.C.; Carnes, A.; Li, L.; Moreau, N. Comparing impact on the family and insurance coverage in children with cerebral palsy and children with another special healthcare need. Child: Care Health Dev. 2018, 44, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Treat, L.; Liesinger, J.; Ziegenfuss, J.Y.; Humeniuk, K.; Prasad, K.; Tilburt, J.C. Patterns of Complementary and Alternative Medicine Use in Children with Common Neurological Conditions. Glob. Adv. Health Med. 2014, 3, 18–24. [Google Scholar] [CrossRef] [Green Version]
| Children’s | Male (n = 150) | Female (n = 115) | Parent’s | Male (n = 258) | Female (n = 263) | ||
|---|---|---|---|---|---|---|---|
| Mean (SD) or n (%) | Mean (SD) or n (%) | p | Mean (SD) or n (%) | Mean (SD) or n (%) | p | ||
| Age (years) † | 7.39 (4.4) | 7.18 (4.9) | 0.714 | Parents’ age † | 44.37 (6.8) | 41.52 (6.2) | <0.001 |
| Health Recourses | Yes | None | Educational qualifications ‡ | ||||
| Private Health coverage | 32 (12.1) | 233 (87.9) | None | 13 (4.9) | 11 (4.2) | <0.001 | |
| Psychological support | 65 (24.5) | 199 (75.1) | Primary | 104 (40.3) | 88 (33.5) | ||
| Mutual support association | 78 (29.4) | 185 (69.8) | Secondary | 28 (10.6) | 26 (9.8) | ||
| Private consultations | 105 (39.6) | 160 (60.4) | University | 57 (22.1) | 78 (29.7) | ||
| Alternative therapies | 69 (26.0) | 161 (60.8) | Occupation ‡ | ||||
| Unemployed or retired | 49 (19.2) | 157 (59.7) | <0.001 | ||||
| Managerial | 36 (14.1) | 37 (14.1) | |||||
| Supervisory/intermediate level | 78 (30.6) | 37 (14.1) | |||||
| Unskilled | 92 (36.1) | 32 (12.2) | |||||
| Father (n = 258) | Mother (n = 261) | |||||
|---|---|---|---|---|---|---|
| Private Health Coverage | ||||||
| Public (n = 226) | Private (n = 32) | Public (n = 231) | Private (n = 32) | |||
| n (%) | n (%) | χ2 | n (%) | n (%) | χ2 | |
| Parent’s education background | ||||||
| -None | 13 (5.8) | 0 (0) | ** 30.987 | 11 (4.8) | 0 (0) | ** 31.903 |
| -Primary school | 99 (43.8) | 5 (15.6) | 85 (36.8) | 3 (9.4) | ||
| -Secondary school | 76 (33.6) | 8 (25) | 80 (34.6) | 6 (18.8) | ||
| -University | 38 (16.8) | 19 (59.4) | 55 (23.8) | 23 (71.9) | ||
| Parent’s Professional occupation | ||||||
| -Unemployed or retired | 48 (21.5) | 1 (3.1) | ** 37.157 | 146 (63.2) | 11 (34.4) | ** 34.296 |
| -Managers | 21 (9.4) | 15 (46.9) | 22 (9.5) | 15 (46.9) | ||
| -Intermediate occupations | 67 (30) | 11 (34.4) | 31 (13.4) | 1 (3.1) | ||
| -Unqualified occupation | 87 (39) | 5 (15.6) | ||||
| Psychological support | ||||||
| Yes (n = 194) | None (n = 64) | Yes (n = 198) | None (n = 65) | |||
| Parent’s education background | ||||||
| -None | 1 (1.6) | 12 (6.2) | * 10.242 | 10 (5,1) | 1 (1,5) | * 11.874 |
| -Primary school | 18 (28.1) | 86 (44.3) | 71 (35,9) | 17 (26,2) | ||
| -Secondary school | 24 (37.5) | 60 (30.9) | 69 (34,8) | 17 (26,2) | ||
| -University | 21 (32.8) | 36 (18.6) | 48 (24,2) | 30 (46,2) | ||
| Parent’s Professional occupation | ||||||
| -Unemployed or retired | 44 (22.9) | 5 (7.9) | ** 15.993 | 127 (64.1) | 30 (46.2) | * 8.818 |
| -Managers | 19 (9.9) | 17 (27) | 25 (12.6) | 12 (18.5) | ||
| -Intermediate occupations | 57 (29.7) | 21 (33.3) | 22 (11.1) | 15 (23.1) | ||
| -Unqualified occupation | 72 (37.5) | 20 (31.7) | 24 (12.1) | 8 (12.3) | ||
| Mutual support association | ||||||
| Yes (n = 75) | None (n = 183) | Yes (n = 77) | None (n = 186) | |||
| Parent’s education background | ||||||
| -None | 3 (4) | 10 (5.5) | 5.870 | 5 (6.5) | 6 (3.3) | * 15.052 |
| -Primary school | 23 (30.7) | 81 (44.5) | 13 (16.9) | 75 (40.8) | ||
| -Secondary school | 27 (36) | 57 (31.3) | 28 (36.4) | 56 (30.4) | ||
| -University | 22 (29.3) | 34 (18.7) | 31 (40.3) | 47 (25.5) | ||
| Parent’s Professional occupation | ||||||
| -Unemployed or retired | 9 (12.3) | 40 (22.1) | * 10.760 | 37 (48,1) | 120 (65.2) | * 15.260 |
| -Managers | 17 (23.3) | 18 (9.9) | 20 (26) | 17 (9.2) | ||
| -Intermediate occupations | 25 (34.2) | 53 (29.3) | 13 (1.9) | 22 (12) | ||
| -Unqualified occupation | 22 (30.1) | 70 (38.7) | 7 (9.1) | 25 (13.6) | ||
| Private Consultations | ||||||
| Yes (n = 104) | None (n = 154) | Yes (n = 105) | None (n = 158) | |||
| Parent’s education background | ||||||
| -None | 1 (1) | 12 (7.8) | * 12.618 | 2 (1.9) | 9 (5.7) | * 12.709 |
| -Primary school | 34 (32.7) | 70 (45.5) | 24 (22.9) | 64 (40.5) | ||
| -Secondary school | 41 (39.4) | 43 (27.9) | 41 (39) | 45 (28.5) | ||
| -University | 28 (26.9) | 29 (18.8) | 38 (36.2) | 40 (25.3) | ||
| Parent’s Professional occupation | ||||||
| -Unemployed or retired | 10 (9.6) | 39 (25.8) | * 14.705 | 56 (53.3) | 101 (63.9) | * 10.104 |
| -Managers | 20 (19.2) | 16 (10.6) | 22 (21) | 15 (9.5) | ||
| -Intermediate occupations | 39 (37.5) | 39 (25.8) | 18 (17.1) | 19 (12) | ||
| -Unqualified occupation | 35 (33.7) | 57 (37.7) | 9 (8.6) | 23 (14.6) | ||
| Alternative therapies | ||||||
| Yes (n = 67) | None (n = 158) | Yes (n = 68) | None (n = 160) | |||
| Parent’s education background | ||||||
| -None | 0 (0) | 13 (8.2) | ** 21.649 | 0 (0) | 11 (6.9) | ** 26.482 |
| -Primary school | 19 (28.4) | 75 (47.5) | 12 (17.6) | 67 (41.9) | ||
| -Secondary school | 22 (32.8) | 46 (29.1) | 23 (33.8) | 50 (31.3) | ||
| -University | 26 (38.8) | 24 (15.2) | 33 (48.5) | 32 (20) | ||
| Parent’s Professional occupation | ||||||
| -Unemployed or retired | 4 (6.1) | 41 (26.3) | ** 23.050 | 33 (48.5) | 107 (66.9) | * 8.645 |
| -Managers | 18 (27.3) | 14 (9) | 15 (22.1) | 18 (11.3) | ||
| -Intermediate occupations | 25 (37.9) | 42 (26.9) | 13 (19.1) | 18 (11.3) | ||
| -Unqualified occupation | 19 (28.8) | 59 (37.8) | 7 (10.3) | 17 (10.6) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-Ardanaz, B.; Peláez-Cantero, M.J.; González-Cano-Caballero, M.; Gutiérrez-Rodríguez, L.; Gómez-González, A.J.; Lupiáñez-Pérez, I.; Morales-Asencio, J.M.; Canca-Sánchez, J.C. Utilization of Parallel Resources and Sociodemographic Factors in Treating Children with Complex Chronic Diseases: A Cross-Sectional Study. Children 2021, 8, 973. https://doi.org/10.3390/children8110973
Pérez-Ardanaz B, Peláez-Cantero MJ, González-Cano-Caballero M, Gutiérrez-Rodríguez L, Gómez-González AJ, Lupiáñez-Pérez I, Morales-Asencio JM, Canca-Sánchez JC. Utilization of Parallel Resources and Sociodemographic Factors in Treating Children with Complex Chronic Diseases: A Cross-Sectional Study. Children. 2021; 8(11):973. https://doi.org/10.3390/children8110973
Chicago/Turabian StylePérez-Ardanaz, Bibiana, María José Peláez-Cantero, María González-Cano-Caballero, Laura Gutiérrez-Rodríguez, Alberto José Gómez-González, Inmaculada Lupiáñez-Pérez, José Miguel Morales-Asencio, and José Carlos Canca-Sánchez. 2021. "Utilization of Parallel Resources and Sociodemographic Factors in Treating Children with Complex Chronic Diseases: A Cross-Sectional Study" Children 8, no. 11: 973. https://doi.org/10.3390/children8110973
APA StylePérez-Ardanaz, B., Peláez-Cantero, M. J., González-Cano-Caballero, M., Gutiérrez-Rodríguez, L., Gómez-González, A. J., Lupiáñez-Pérez, I., Morales-Asencio, J. M., & Canca-Sánchez, J. C. (2021). Utilization of Parallel Resources and Sociodemographic Factors in Treating Children with Complex Chronic Diseases: A Cross-Sectional Study. Children, 8(11), 973. https://doi.org/10.3390/children8110973







