Impact of the Coronavirus Pandemic on High-Risk Infant Follow-Up (HRIF) Programs: A Survey of Academic Programs
Abstract
:1. Introduction
2. Methods
- (1)
- The demographics of HRIF clinics programs;
- (2)
- The effects of the pandemic on the conduct of HRIF clinics and solutions to some common problems;
- (3)
- The effects of the pandemic on the availability of personnel in the clinic and early intervention programs;
- (4)
- Changes to reimbursements and the standardization of telemedicine visits.
3. Analysis
4. Results
4.1. Program Characteristics
4.2. Impact of the Pandemic on Conditions
4.3. Innovative Approaches to Conducting Telemedicine Visits
5. Discussion
- (1)
- Programs had to decrease the frequency of clinics due to a lack of personnel and or funding.
- (2)
- As the majority of HRIF clinics switched to either a hybrid or entirely virtual model, the access to quality and affordable internet services could be one of the reasons for decreasing show rates.
- (3)
- The delivery of care, such as the basics of vitals measurements are still limited through telemedicine services.
- (4)
- A provider or parental discomfort with telemedicine visits, as there is a lack of standardization and validity of the impact on outcomes.
- (5)
- The unclear medicolegal and state rules with regard to telemedicine visits, and future consequences.
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| HRIF | High-Risk Infant Programs |
| NICU | Neonatal Intensive Care Unit |
| SARS-CoV-2 | Severe Acute Respiratory Syndrome Coronavirus 2 |
| COVID-19 | Coronavirus disease 2019 |
| RedCAP | Research Electronic Data Capture |
| FREIDA | Fellowship and Residency Electronic Interactive Database |
| ASQs | Ages and stages questionnaires |
| DAYC | Development Assessment of young children |
| CP | Cerebral palsy |
References
- McInerny, T.A.; Campbell, D.E.; DeWitt, T.G.; Foy, J.M.; Kamat, D.M. Follow-up Care. In American Academy of Pediatrics Textbook of Pediatric Care; American Academy of Pediatrics: Elk Grove Village, IL, USA, 2017. [Google Scholar]
- Committee on Fetus and Newborn. Hospital Discharge of the High-Risk Neonate. Pediatrics 2008, 122, 1119–1126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fanaroff, A.A.; Hack, M.; Walsh, M.C. The NICHD neonatal research network: Changes in practice and outcomes during the first 15 years. Semin. Perinatol. 2003, 27, 281–287. [Google Scholar] [CrossRef]
- Ayala, L.; Winter, S.; Byrne, R.; Fehlings, D.; Gehred, A.; Letzkus, L.; Noritz, G.; Paton, M.C.; Pietruszewski, L.; Rosenberg, N.; et al. Assessments and Interventions for Spasticity in Infants With or at High Risk for Cerebral Palsy: A Systematic Review. Pediatr. Neurol. 2020, 118, 72–90. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatrics. Follow-up Care of High-Risk Infants. Pediatrics 2004, 114, 1377–1397. [Google Scholar] [CrossRef] [Green Version]
- Vohr, B.R.; O’Shea, M.; Wright, L.L. Longitudinal multicenter follow-up of high-risk infants: Why, who, when, and what to assess. Semin. Perinatol. 2003, 27, 333–342. [Google Scholar] [CrossRef]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [PubMed]
- Kim, J.-Y. Contactless Healthcare. Health Inform. Res. 2020, 26, 253–254. [Google Scholar] [CrossRef] [PubMed]
- Mann, D.M.; Chen, J.; Chunara, R.; Testa, P.; Nov, O. COVID-19 transforms health care through telemedicine: Evidence from the field. J. Am. Med. Inform. Assoc. 2020, 27, 1132–1135. [Google Scholar] [CrossRef] [PubMed]
- Education ACfGM. Program Reqruirements, Neonatal Perinatal Medicine. 2020. Available online: https://www.acgme.org/globalassets/PFAssets/ProgramRequirements/329_NeonatalPerinatalMedicine_2020.pdf?ver=2020-06-19-105945-263&ver=2020-06-19-105945-263 (accessed on 10 December 2020.).
- Gong, A.; Johnson, Y.R.; Livingston, J.; Matula, K.; Duncan, A.F. Newborn intensive care survivors: A review and a plan for collaboration in Texas. Matern. Health. Neonatol. Perinatol. 2015, 1, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuppala, V.S.; Tabangin, M.; Haberman, B.; Steichen, J.; Yolton, K. Current state of high-risk infant follow-up care in the United States: Results of a national survey of academic follow-up programs. J. Perinatol. 2012, 32, 293–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bockli, K.; Andrews, B.; Pellerite, M.; Meadow, W. Trends and challenges in United States neonatal intensive care units follow-up clinics. J. Perinatol. 2014, 34, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Maitre, N.L.; Burton, V.J.; Duncan, A.F.; Iyer, S.; Ostrander, B.; Winter, S.; Ayala, L.; Burkhardt, S.; Gerner, G.; Getachew, R.; et al. Network Implementation of Guideline for Early Detection Decreases Age at Cerebral Palsy Diagnosis. Pediatrics 2021, 145, e20192126. [Google Scholar] [CrossRef] [Green Version]
- Duncan, A.F.; Bann, C.; Maitre, N.L.; Peralta-Carcelen, M.; Hintz, S.R. Hand Function at 18–22 Months Is Associated with School-Age Manual Dexterity and Motor Performance in Children Born Extremely Preterm. J. Pediatr. 2020, 225, 51–57.e3. [Google Scholar] [CrossRef] [PubMed]
- Canadian Neonatal Network 2019 Annual Report. Available online: https://www.canadianneonatalnetwork.org/portal/Portals/0/Annual%20Reports/CNFUNreport_2019%20FINAL.pdf (accessed on 15 March 2021.).
- Albaghli, F.; Church, P.; Ballantyne, M.; Girardi, A.; Synnes, A. Neonatal follow-up programs in Canada: A national survey. Paediatr. Child Health 2019, 26, e46–e51. [Google Scholar] [CrossRef] [PubMed]



| High Risk Infant Programs Characteristics | ||||
|---|---|---|---|---|
| United States | Canada | |||
| Characteristic | N | Percentage | N | Percentage |
| (Number of respondents) | (Number of respondents) | |||
| Institutions with more than 40 NICU beds | 59 | 86% | 5 | 100 |
| (N = 51) | ||||
| Median numbers of Beds in NICU | 60 (50–81) | 5 | 65 (60–70) | |
| NICU admissions per year | ||||
| <250 | 2 | 3.20% | - | - |
| 251–500 | 7 | 11.1% | - | - |
| 501–750 | 14 | 22.2% | 1 | 20% |
| 751–1000 | 24 | 38.1% | - | - |
| >1000 | 16 | 25.4% | 4 | 80% |
| Criteria for Referral to HRIF clinic | ||||
| All discharges | 1 | 1.60% | - | 100% |
| All less than 36 weeks gestation | 57 | 90% | 5 | 100% |
| Genetic anomalies | 36 | 57% | 5 | 100% |
| HIE | 56 | 89% | 5 | 100% |
| Neurological disorder | 43 | 68% | 5 | - |
| Major Malformations | 40 | 64% | - | 30% |
| Others * | 31 | 49% | 3 | |
| Frequency of HRIF clinic pre-pandemic | ||||
| One Half-day per Week | 14 | 23% | 1 | 20% |
| One full day per week | 14 | 23% | - | - |
| Two full days per week | 10 | 18.5% | 1 | 20% |
| More than two days per week | 21 | 35.5% | 3 | 75% |
| Average Census Per HRIF clinic day | ||||
| Less than 5 patients | 8 | 14% | 1 | 20% |
| 5–10 Patients | 28 | 47% | 3 | 75% |
| 10–20 Patients | 19 | 32% | 1 | 25% |
| More than 20 Patients | 4 | 7% | - | - |
| COVID-19 Impact on HRIF Clinic Services | ||||
|---|---|---|---|---|
| Characteristic | United States | Canada | ||
| Any Cancellation of HRIF Clinic | N | Percentage | N | Percentage |
| (Number of respondents) | (Number of respondents) | |||
| No Cancellation | 19 | 30% | 1 | 20% |
| For Less than 1 month | 16 | 25% | 3 | 60% |
| 1–3 months | 24 | 38% | 1 | 20% |
| 3–5 months | 3 | 5% | - | - |
| >6 months | 1 | 1.60% | - | - |
| Change in clinic frequency | ||||
| No Change | 42 | 71% | 4 | 80% |
| Decreased | 17 | 29% | 1 | 20% |
| Change in Patient show rates | ||||
| Increased show rates | 9 | 15% | 1 | 20% |
| Decreased show rates | 25 | 42.5% | 1 | 20% |
| No change | 25 | 42.5% | 3 | 60% |
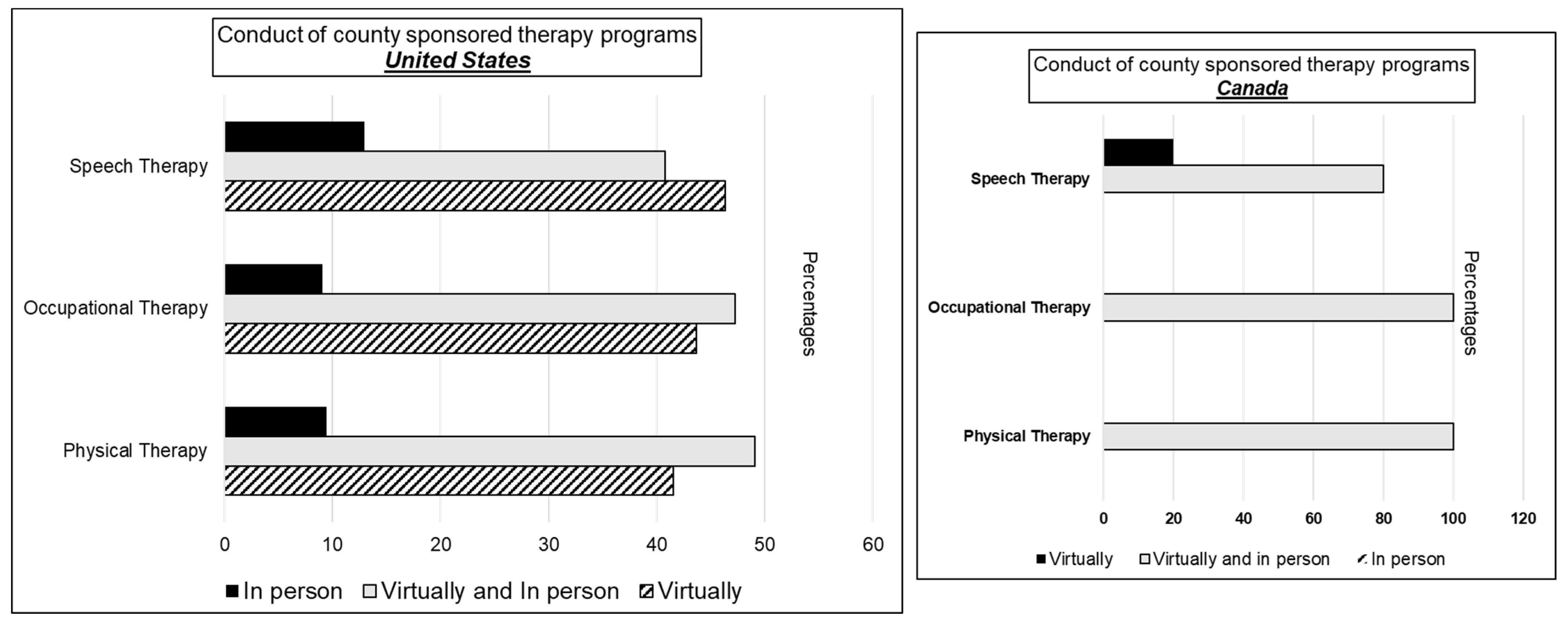
| Conduct of HRIF Clinic | ||||
| All in person visits | 9 | 14% | - | - |
| All Telemedicine | 5 | 8% | - | - |
| Both in person and telemedicine | 49 | 78% | 5 | 100% |
| Multidisciplinary Telemedicine Visits | ||||
| Yes | 18 | 45% | 5 | 100% |
| No | 15 | 37.5% | - | |
| Did not answer | 7 | 17.5% | - | |
| Standardization of telemedicine visits | ||||
| Yes | 21 | 53% | 4 | 80% |
| No | 13 | 33% | 1 | 20% |
| Did not answer | 6 | 15% | - | - |
| Reimbursement compared to in person visits | ||||
| <50% | 4 | 10% | N/A | N/A |
| 50–90% | 13 | 32.5% | ||
| 100% | 5 | 12.5% | ||
| Did not know level of reimbursements | 2 | 5% | ||
| Did not answer | 16 | 40% | ||
| Did payor policies affect decision to conduct telemedicine vs in person visits? | ||||
| Yes, It affected to conducted more tele visits | 5 | 8.50% | N/A | N/A |
| No, It did not affect | 31 | 52.5 | ||
| Did not answer | 23 | 39% | ||
| Program’s Perception of changes to HRIF clinic format. (Sliding scale) | ||||
| Mostly negative (a score of <50) | 27 | 55% | 0 | 0% |
| Mostly positive (a score of >50) | 22 | 45% | 5 | 100% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panda, S.; Somu, R.; Maitre, N.; Levin, G.; Singh, A.P. Impact of the Coronavirus Pandemic on High-Risk Infant Follow-Up (HRIF) Programs: A Survey of Academic Programs. Children 2021, 8, 889. https://doi.org/10.3390/children8100889
Panda S, Somu R, Maitre N, Levin G, Singh AP. Impact of the Coronavirus Pandemic on High-Risk Infant Follow-Up (HRIF) Programs: A Survey of Academic Programs. Children. 2021; 8(10):889. https://doi.org/10.3390/children8100889
Chicago/Turabian StylePanda, Sanjeet, Rashmi Somu, Nathalie Maitre, Garrett Levin, and Ajay Pratap Singh. 2021. "Impact of the Coronavirus Pandemic on High-Risk Infant Follow-Up (HRIF) Programs: A Survey of Academic Programs" Children 8, no. 10: 889. https://doi.org/10.3390/children8100889
APA StylePanda, S., Somu, R., Maitre, N., Levin, G., & Singh, A. P. (2021). Impact of the Coronavirus Pandemic on High-Risk Infant Follow-Up (HRIF) Programs: A Survey of Academic Programs. Children, 8(10), 889. https://doi.org/10.3390/children8100889






