Combined Effect of Race/Ethnicity and Type of Insurance on Reuse of Urgent Hospital-Based Services in Children Discharged with Asthma
Abstract
1. Introduction
2. Materials and Methods
2.1. Case Verification and Data Collection
2.2. Outcome Definition and Data Presentation
2.3. Statistical Analysis
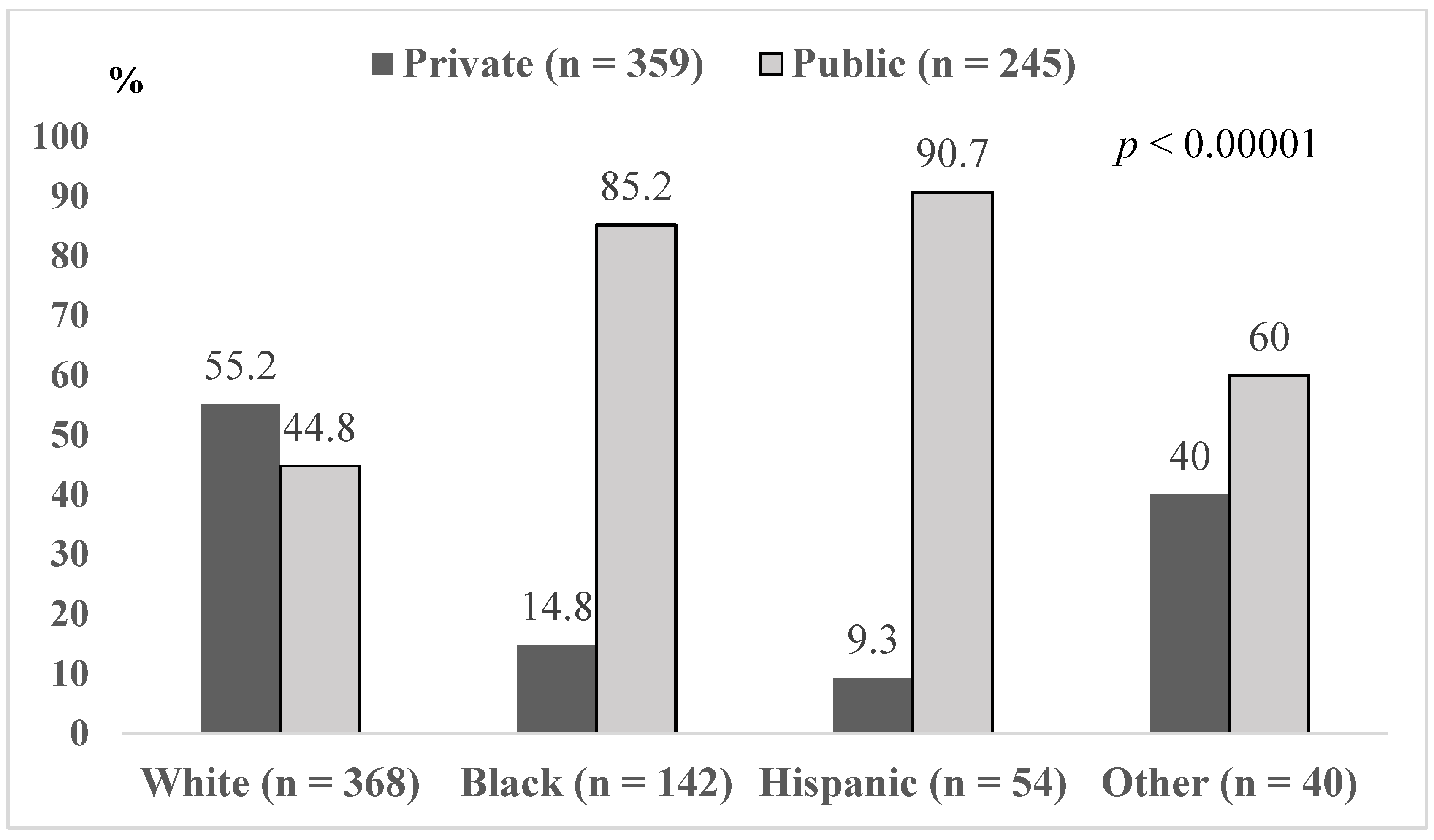
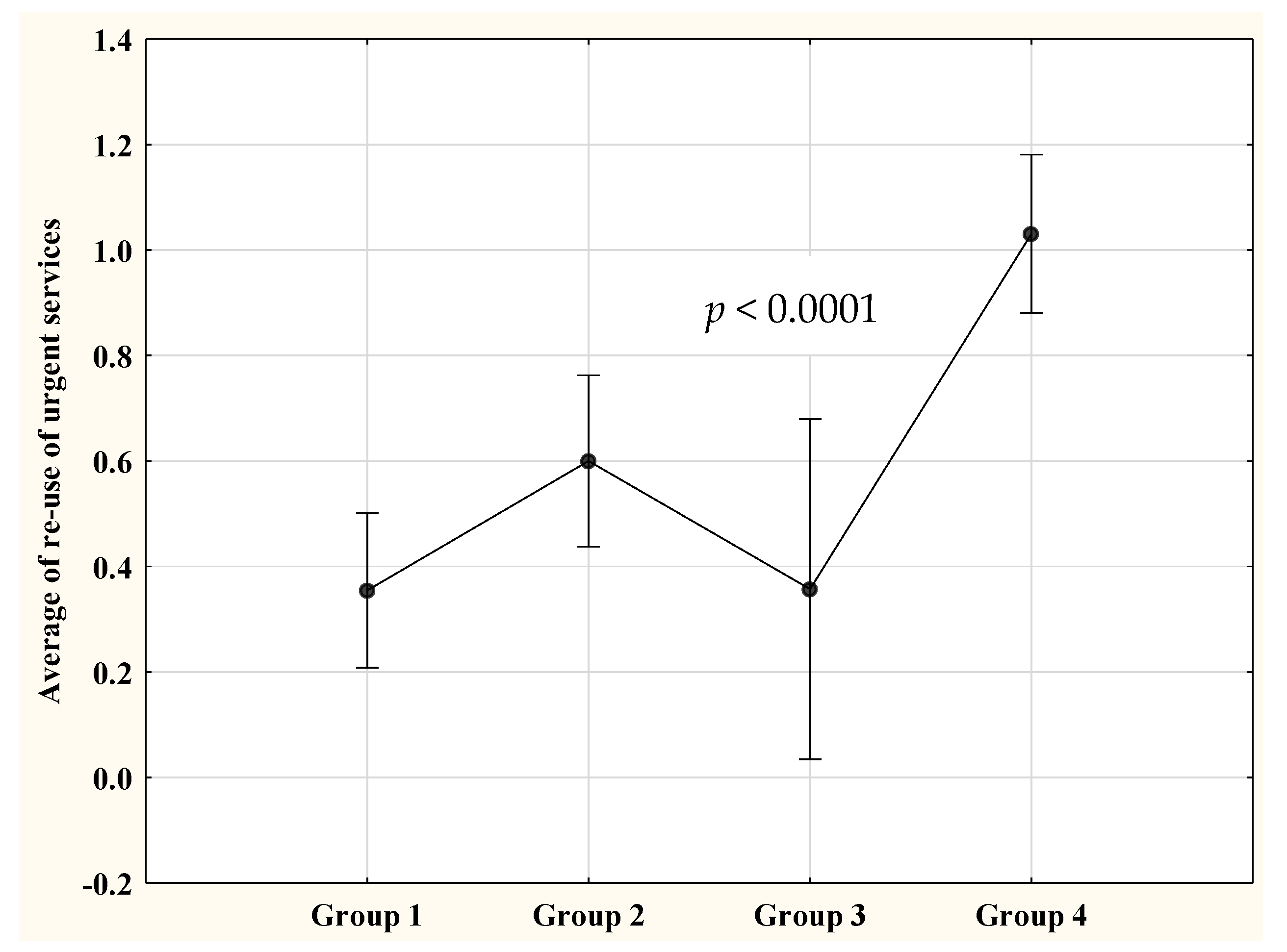
3. Results
3.1. Reuse of Hospital-Based Services for Children with Asthma
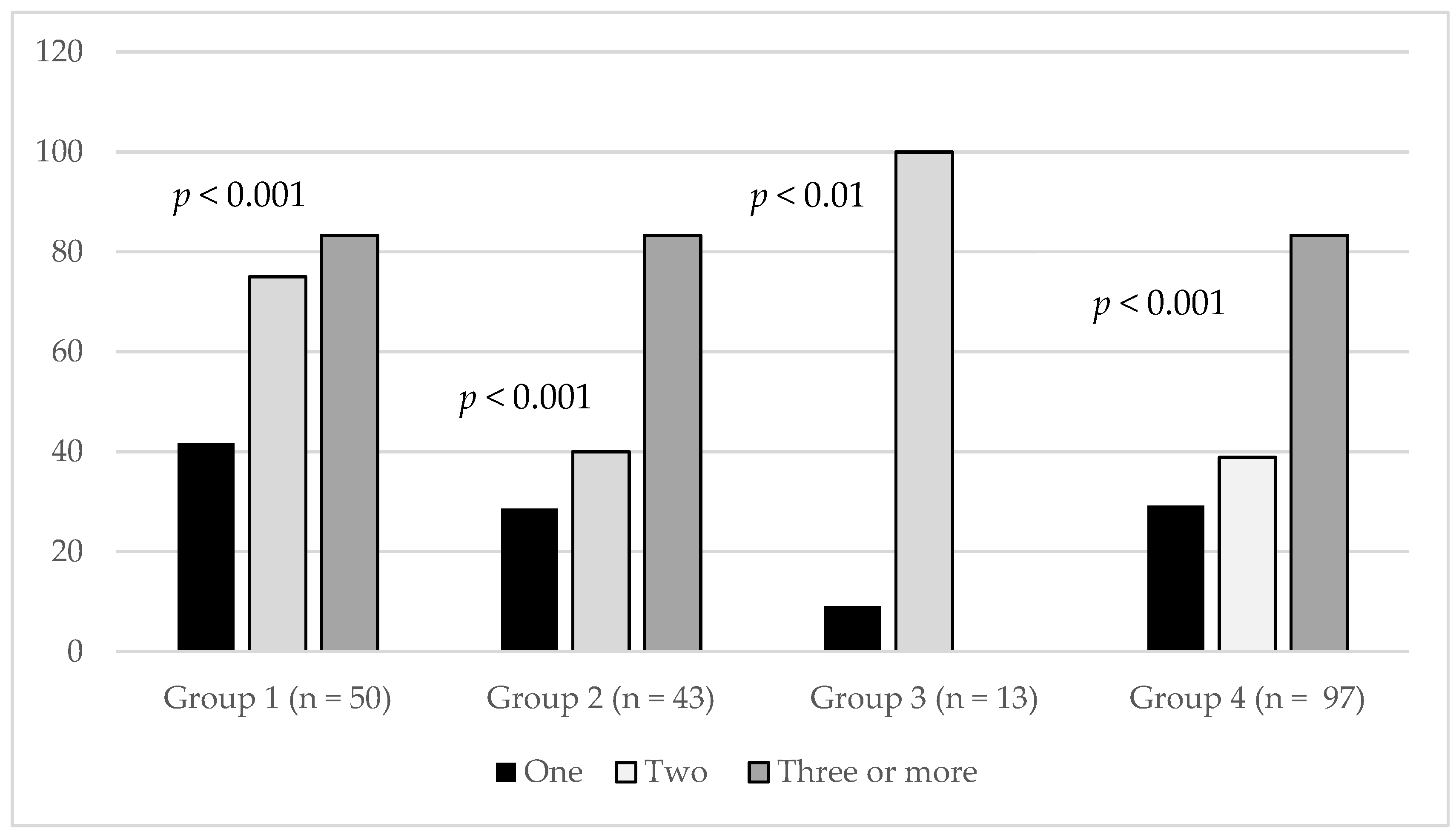
3.2. Group-Based Comparison of Hospitalization among Total Number of ED Revisitations
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gold, D.R.; Wright, R. Population disparities in asthma. Annu. Rev. Public Health 2005, 26, 89–113. [Google Scholar] [CrossRef] [PubMed]
- McDaniel, M.; Paxson, C.; Waldfogel, J. Racial Disparities in Childhood Asthma in the United States: Evidence From the National Health Interview Survey, 1997 to 2003. Pediatrics 2006, 117, 868–877. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.R.; Sternthal, M.; Wright, R.J. Social determinants: Taking the social context of asthma seriously. Pediatrics 2009, 123 (Suppl. 3), S174–S184. [Google Scholar] [CrossRef] [PubMed]
- Forno, E.; Celedón, J.C. Asthma and ethnic minorities: Socioeconomic status and beyond. Curr. Opin. Allergy Clin. Immunol. 2009, 9, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Wright, R.J.; Mitchell, H.; Visness, C.M.; Cohen, S.; Stout, J.; Evans, R.; Gold, D.R. Community Violence and Asthma Morbidity: The Inner-City Asthma Study. Am. J. Public Health 2004, 94, 625–632. [Google Scholar] [CrossRef]
- Stewart, K.A.; Higgins, P.C.; McLaughlin, C.G.; Williams, T.V.; Granger, E.; Croghan, T.W. Differences in Prevalence, Treatment, and Outcomes of Asthma Among a Diverse Population of Children With Equal Access to Care. Arch. Pediatr. Adolesc. Med. 2010, 164, 720–726. [Google Scholar] [CrossRef]
- Finkelstein, J.A.; Brown, R.W.; Schneider, L.C.; Weiss, S.T.; Quintana, J.M.; Goldmann, D.A.; Homer, C.J. Quality of care for preschool children with asthma: The role of social factors and practice setting. Pediatrics 1995, 95, 389–394. [Google Scholar]
- Beck, A.F.; Huang, B.; Simmons, J.M.; Moncrief, T.; Sauers, H.; Chen, C.; Ryan, P.H.; Newman, N.C.; Kahn, R.S. Role of Financial and Social Hardships in Asthma Racial Disparities. Pediatrics 2014, 133, 431–439. [Google Scholar] [CrossRef]
- Hill, T.D.; Graham, L.M.; Divgi, V. Racial Disparities in Pediatric Asthma: A Review of the Literature. Curr. Allergy Asthma Rep. 2010, 11, 85–90. [Google Scholar] [CrossRef]
- Liu, S.Y.; Pearlman, D.N. Hospital Readmissions for Childhood Asthma: The Role of Individual and Neighborhood Factors. Public Heal. Rep. 2009, 124, 65–78. [Google Scholar] [CrossRef]
- Crocker, D.; Brown, C.; Moolenaar, R.; Moorman, J.; Bailey, C.; Mannino, D.M.; Holguin, F. Racial and Ethnic Disparities in Asthma Medication Usage and Health-Care Utilization: Data from the National Asthma Survey. Chest 2009, 136, 1063–1071. [Google Scholar] [CrossRef] [PubMed]
- Ungar, W.J.; Paterson, J.M.; Gomes, T.; Bikangaga, P.; Gold, M.; To, T.; Kozyrskyj, A.L. Relationship of asthma management, socioeconomic status, and medication insurance characteristics to exacerbation frequency in children with asthma. Ann. Allergy Asthma Immunol. 2011, 106, 17–23. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pearlman, D.N.; Zierler, S.; Meersman, S.; Kim, H.K.; Viner-Brown, S.I.; Caron, C. Race disparities in childhood asthma: Does where you live matter? J. Natl. Med. Assoc. 2006, 98, 239–247. [Google Scholar] [PubMed]
- Wright, R.J.; Subramanian, S.V. Advancing a Multilevel Framework for Epidemiologic Research on Asthma Disparities. Chest 2007, 132 (Suppl. 5), 757S–769S. [Google Scholar] [CrossRef]
- Smith, L.A.; Hatcher-Ross, J.L.; Wertheimer, R.; Kahn, R.S. Rethinking race/ethnicity, income, and childhood asthma: Racial/ethnic disparities concentrated among the very poor. Public Health Rep. 2005, 120, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Dexheimer, J.W.; Chambers, P.; Johnson, L.H. Asthma-related emergency department use: Current perspectives. Open Access Emerg. Med. 2016, 8, 47–55. [Google Scholar] [CrossRef]
- Auger, K.A.; Kenyon, C.C.; Feudtner, C.; Davis, M.M. Pediatric hospital discharge interventions to reduce subsequent utilization: A systematic review. J. Hosp. Med. 2013, 9, 251–260. [Google Scholar] [CrossRef]
- Fassl, B.A.; Nkoy, F.L.; Stone, B.L.; Srivastava, R.; Simon, T.D.; Uchida, D.A.; Koopmeiners, K.; Greene, T.; Cook, L.J.; Maloney, C.G. The Joint Commission Children’s Asthma Care Quality Measures and Asthma Readmissions. Pediatrics 2012, 130, 482–491. [Google Scholar] [CrossRef]
- Jones, R.; Lin, S.; Munsie, J.P.; Radigan, M.; Hwang, S.-A. Racial/Ethnic Differences in Asthma-Related Emergency Department Visits and Hospitalizations among Children with Wheeze in Buffalo, New York. J. Asthma 2008, 45, 916–922. [Google Scholar] [CrossRef]
- Ferris, T.G.; Crain, E.F.; Oken, E.; Wang, L.; Clark, S.; Camargo, C.A., Jr. Insurance and quality of care for children with acute asthma. Ambul. Pediatr. 2002, 1, 267–274. [Google Scholar] [CrossRef]
- Barnett, J.C.; Berchick, E.R. Health Insurance Coverage in the United States 2016: Current Population Reports; U.S. Government Printing Office; U.S. Department of Commerce: Washington, DC, USA, 2017; pp. 60–260.
- State of New Jersey Department of Human Services. Division of Medical Assistance and Health Services, 2008. Available online: https://www.state.nj.us/humanservices/dmahs/clients/medicaid/families/ (accessed on 16 August 2020).
- Pinto, J.M.; Navallo, L.J.; Petrova, A. Does participation in the community outreach for asthma care and healthy lifestyles (COACH) program alter subsequent use of hospital services for children discharged with asthma? J. Asthma 2019. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Pneumonia Vaccine Trial Investigators’ Group. Standardization of Interpretation of Chest Radiographs for the Diagnosis of Pneumonia in Children; WHO Press: Geneva, Switzerland, 2001; p. 32. [Google Scholar]
- Ortiz-Alvarez, O.; Mikrogianakis, A.; Canadian Paediatric Society, Acute Care Committee. Managing the paediatric patient with an acute asthma exacerbation. Paediatr. Child Health 2012, 17, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention; National Center for Emerging and Zoonotic Infectious Diseases (NCEZID); Division of Global Migration and Quarantine (DGMQ). Quarantine and Isolation: Symptom Definitions; The U.S. Department of Health and Human Services: Washington, DC, USA, 2019. Available online: https://www.cdc.gov/quarantine/air/reporting-deaths-illness/definitions-symptoms-reportable-illnesses.html (accessed on 23 March 2019).
- NJ Spotlight. Explainer: Who Is Helped by New Jersey’s Charity Care Program? 2016. Available online: https://www.njspotlight.com/2016/07/16-07-04-explainer-who-is-helped-by-new-jersey-s-charity-care-program/ (accessed on 25 April 2019).
- Zhang, Q.; Lamichhane, R.; Diggs, L.A. Disparities in emergency department visits in American children with asthma: 2006–2010. J. Asthma 2016, 54, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Shields, A.E.; Comstock, C.; Weiss, K.B. Variations in asthma care by race/ethnicity among children enrolled in a state Medicaid program. Pediatrics 2004, 113, 496–504. [Google Scholar] [CrossRef]
- Assari, S.; Lankarani, M.M. Poverty Status and Childhood Asthma in White and Black Families: National Survey of Children’s Health. Healthcare 2018, 6, 62. [Google Scholar] [CrossRef]
- Grineski, S.E.; Staniswalis, J.G.; Peng, Y.; Atkinson-Palombo, C. Children’s asthma hospitalizations and relative risk due to nitrogen dioxide (NO2): Effect modification by race, ethnicity, and insurance status. Environ. Res. 2010, 110, 178–188. [Google Scholar] [CrossRef]
- Stingone, J.A.; Claudio, L. Disparities in the use of urgent health care services among asthmatic children. Ann. Allergy Asthma Immunol. 2006, 97, 244–250. [Google Scholar] [CrossRef]
- Chang, J.; Delfino, R.J.; Gillen, D.; Tjoa, T.; Nickerson, B.; Cooper, D. Repeated respiratory hospital encounters among children with asthma and residential proximity to traffic. Occup. Environ. Med. 2008, 66, 90–98. [Google Scholar] [CrossRef]
- Duckett, P.; Artiga, S. Health Coverage for the Black Population Today and under the Affordable Care Act; Kaiser Family Foundation: San Francisco, CA, USA, 2013; Available online: https://www.kff.org/disparities-policy/fact-sheet/health-coverage-for-the-black-population-today-and-under-the-affordable-care-act/ (accessed on 25 April 2019).
| Characteristics ‡ | Group 1 n = 203 | Group 2 n = 165 | Group 3 n = 42 | Group 4 n = 194 | p Value |
|---|---|---|---|---|---|
| Age (years) | 5 (3–8) | 4 (2–7) | 7 (2–11) | 4 (1.8–7) | 0.01 |
| Male sex | 129 (63.6) | 97 (58.8) | 26 (61.9) | 118 (60.8) | 0.82 |
| Prior asthma admission (s) | 77 (38.1) | 71 (43.3) | 19 (45.2) | 98 (50.8) | 0.09 |
| Prior PICU asthma admission(s) | 23 (12.3) | 23 (15.2) | 6 (15.8) | 28 (16.1) | 0.75 |
| Use of controller medication(s) | 72 (35.5) | 59 (36.0) | 17 (40.5) | 76 (39.2) | 0.82 |
| Winter season at admission | 49 (24.1) | 48 (29.1) | 11 (26.2) | 46 (23.7) | 0.98 |
| PICU hospitalization | 61 (30.2) | 48 (29.1) | 11 (26.2) | 53 (27.5) | 0.91 |
| Fever at presentation | 94 (46.3) | 89 (53.9) | 18 (42.9) | 94 (48.5) | 0.41 |
| Chest retractions | 130 (64.4) | 111 (67.3) | 21 (50.0) | 146 (75.3) | <001 |
| Oxygen supplementation | 111 (55.0) | 111 (67.3) | 16 (38.1) | 95 (49.2) | <0.001 |
| PO2 < 90% on presentation | 30 (14.9) | 29 (17.7) | 4 (9.8) | 20 (10.3) | 0.18 |
| Antibiotic treatment | 112 (55.5) | 86 (52.1) | 21 (51.2) | 106 (54.9) | 0.89 |
| Bacterial infection | 33 (16.3) | 21 (12.7) | 5 (11.9) | 28 (14.5) | 0.76 |
| Chest X-ray | 190 (94.1) | 158 (95.8) | 40 (95.2) | 184 (94.9) | 0.91 |
| Positive Chest X-ray | 23 (12.0) | 15 (9.5) | 4 (12.5) | 15 (8.2) | 0.59 |
| COACH participation | 39 (19.2) | 37 (22.4) | 7 (16.7) | 70 (36.1) | <0.001 |
| LOS (hours) | 51 (35–89.8) | 64.2 (42.5–96.8) | 52.8 (33.5–110) | 65.5 (41.1–110.8) | 0.11 |
| Group ‡ (Code) | Group 2 (1) | Group 3 (1) | Group 4 (1) | |||
|---|---|---|---|---|---|---|
| ORcrude | ORadjusted | ORcrude | ORadjusted | ORcrude | ORadjusted | |
| Group 1 (0) | 0.88 (0.64, 1.21) | 0.81 (0.64, 1.02) | 0.92 0.55,1.54) | 0.85 (0.59, 1.23) | 0.67 ** (0.49, 0.92) | 0.57 ** (0.46, 0.70) |
| Group 2 (0) | 1.05 (0.61, 1.78) | 1.07 (0.74, 1.54) | 0.77 (0.54, 1.08) | 0.71 *** (0.57, 0.88) | ||
| Group 3 (0) | 0.73 (0.43, 1.25) | 0.66 * (0.47, 0.96) | ||||
| Group † (Code) ‡ | Group 2 (1) | Group 3 (1) | Group 4 (1) |
|---|---|---|---|
| Group 1 (0) | 0.231 (0.055, 0.407) * | 0.011 (−0.011, 0.133) | 0.223 (0.148, 0.298) *** |
| Group 2 (0) | −0.235 (−0.578, 0.108) | 0.221 (0.088, 0.354) ** | |
| Group 3 (0) | 0.664 (0.209, 1.119) ** |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pinto, J.M.; Wagle, S.; Navallo, L.J.; Petrova, A. Combined Effect of Race/Ethnicity and Type of Insurance on Reuse of Urgent Hospital-Based Services in Children Discharged with Asthma. Children 2020, 7, 107. https://doi.org/10.3390/children7090107
Pinto JM, Wagle S, Navallo LJ, Petrova A. Combined Effect of Race/Ethnicity and Type of Insurance on Reuse of Urgent Hospital-Based Services in Children Discharged with Asthma. Children. 2020; 7(9):107. https://doi.org/10.3390/children7090107
Chicago/Turabian StylePinto, Jamie M., Sarita Wagle, Lauren J. Navallo, and Anna Petrova. 2020. "Combined Effect of Race/Ethnicity and Type of Insurance on Reuse of Urgent Hospital-Based Services in Children Discharged with Asthma" Children 7, no. 9: 107. https://doi.org/10.3390/children7090107
APA StylePinto, J. M., Wagle, S., Navallo, L. J., & Petrova, A. (2020). Combined Effect of Race/Ethnicity and Type of Insurance on Reuse of Urgent Hospital-Based Services in Children Discharged with Asthma. Children, 7(9), 107. https://doi.org/10.3390/children7090107





