Evolving Cognitive Dysfunction in Children with Neurologically Stable Opsoclonus–Myoclonus Syndrome
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Pang, K.K.; de Sousa, C.; Lang, B.; Pike, M.G. A prospective study of the presentation and management of dancing eye syndrome/opsoclonus–myoclonus syndrome in the United Kingdom. Eur. J. Paediatr. Neurol. 2010, 14, 156–161. [Google Scholar] [CrossRef]
- Gorman, M.P. Update on diagnosis, treatment, and prognosis in opsoclonus–myoclonus–ataxia syndrome. Curr. Opin. Pediatr. 2010, 22, 745–750. [Google Scholar] [CrossRef]
- Berridge, G.; Menassa, D.A.; Moloney, T.; Waters, P.J.; Welding, I.; Thomsen, S.; Zuberi, S.; Fischer, R.; Aricescu, A.R.; Pike, M.; et al. Glutamate receptor δ2 serum antibodies in pediatric opsoclonus myoclonus ataxia syndrome. Neurology 2018, 91, e714–e723. [Google Scholar] [CrossRef] [PubMed]
- Hayward, K.; Jeremy, R.J.; Jenkins, S.; Barkovich, A.J.; Gultekin, S.H.; Kramer, J.; Crittenden, M.; Matthay, K.K. Long-term neurobehavioral outcomes in children with neuroblastoma and opsoclonus-myoclonus-ataxia syndrome: Relationship to MRI findings and anti-neuronal antibodies. J. Pediatr. 2001, 139, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, W.G.; Davalos-Gonzalez, Y.; Brumm, V.L.; Aller, S.K.; Burger, E.; Turkel, S.B.; Borchert, M.S.; Hollar, S.; Padilla, S. Opsoclonus-ataxia caused by childhood neuroblastoma: Developmental and neurologic sequelae. Pediatrics 2002, 109, 86–98. [Google Scholar] [PubMed]
- Mitchell, W.G.; Brumm, V.L.; Azen, C.G.; Patterson, K.E.; Aller, S.K.; Rodriguez, J. Longitudinal neurodevelopmental evaluation of children with opsoclonus-ataxia. Pediatrics 2005, 116, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Tate, E.D.; Allison, T.J.; Pranzate, M.R.; Verhu, S.J. Neuroepidemiologic trends in 105 US cases of pediatric opsoclonus-myoclonus syndrome. J. Pediatr. Oncol. Nurs. 2005, 22, 8–19. [Google Scholar] [CrossRef] [PubMed]
- Brunklaus, A.; Pohl, K.; Zuberi, S.M.; de Sousa, C. Outcome and prognostic features in opsoclonus-myoclonus syndrome from infancy to adult life. Pediatrics 2011, 128, e388–e394. [Google Scholar] [CrossRef] [PubMed]
- Anand, G.; Bridge, H.; Rackstraw, P.; Chekroud, A.M.; Yong, J.; Stagg, C.J.; Pike, M. Cerebellar and cortical abnormalities in paediatric opsoclonus-myoclonus syndrome. Dev. Med. Child Neurol. 2015, 57, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Pranzatelli, M.R.; Travelstead, A.L.; Tate, E.D.; Allison, T.J.; Moticka, E.J.; Franz, D.N.; Nigro, M.A.; Parke, J.T.; Stumpf, D.A.; Verhulst, S.J. B- and T-cell markers in opsoclonus-myoclonus syndrome: Immunophenotyping of CSF lymphocytes. Neurology 2004, 62, 1526–1532. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials. Opsoclonus Myoclonus Syndrome/Dancing Eye Syndrome (OMS/DES) in Children with and without Neuroblastoma; Identifier: NCT01868269; National Library of Medicine: Bethesda, MD, USA, 2019.
- Sheridan, A.; Kapur, K.; Pinard, F.; Dietrich Alber, F.; Camposano, S.; Pike, M.G.; Klein, A.; Gorman, M.P. Predictors of Intelligence Quotient (IQ) in a multinational study of 81 patients with pediatric opsoclonus myoclonus ataxia syndrome. Dev. Med. Child Neurol. 2020. In press. [Google Scholar] [CrossRef] [PubMed]
- Ekmekci, O. Pediatric Multiple Sclerosis and Cognition: A Review of Clinical, Neuropsychologic, and Neuroradiologic Features. Behav. Neurol. 2017, 2017, 1463570. [Google Scholar] [CrossRef] [PubMed]
- Anderson, V.; Spencer-Smith, M.; Wood, A. Do children really recover better? Neurobehavioural plasticity after early brain insult. Brain 2011, 134, 2197–2221. [Google Scholar] [CrossRef] [PubMed]
- Nomura, Y.; Halperin, J.M.; Newcorn, J.H.; Davey, C.; Fifer, W.P.; Savitz, D.A.; Brooks-Gunn, J. The risk for impaired learning-related abilities in childhood and educational attainment among adults born near-term. J. Pediatr. Psychol. 2009, 34, 406–418. [Google Scholar] [CrossRef] [PubMed]
- Schendel, D.; Bhasin, T.K. Birth weight and gestational age characteristics of children with autism, including a comparison with other developmental disabilities. Pediatrics 2008, 121, 1155–1164. [Google Scholar] [CrossRef]
- Hillemeier, M.M.; Farkas, G.; Morgan, P.L.; Martin, M.A.; Maczuga, S.A. Disparities in the prevalence of cognitive delay: How early do they appear? Paediatr. Perinat. Epidemiol. 2009, 23, 186–198. [Google Scholar] [CrossRef] [PubMed]
- Allotey, J.; Zamora, J.; Cheong-See, F.; Kalidindi, M.; Arroyo-Manzano, D.; Asztalos, E.; van der Post, J.A.M.; Mol, B.W.; Moore, D.; Birtles, D.; et al. Cognitive, motor, behavioural and academic performances of children born preterm: A meta-analysis and systematic review involving 64 061 children. BJOG An Int. J. Obstet. Gynaecol. 2018, 125, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Park, D.C.; Reuter-Lorenz, P. The adaptive brain: Aging and neurocognitive scaffolding. Annu. Rev. Psychol. 2009, 60, 173–196. [Google Scholar] [CrossRef] [PubMed]
- Eckert, M.A. Slowing down: Age-related neurobiological predictors of processing speed. Front. Neurosci. 2011, 5, 25. [Google Scholar] [CrossRef]
- Olsson, I.T.; Perrin, S.; Lundgren, J.; Hjorth, L.; Johanson, A. Long-term cognitive sequelae after pediatric brain tumor related to medical risk factors, age, and sex. Pediatr. Neurol. 2014, 51, 515–521. [Google Scholar] [CrossRef]
| Case | Gender | Age at Onset | Age at Diagnosis | Clinical Features at Presentation | OMS Score at Diagnosis | Presence of Neuroblastoma | Treatment | Response | Age at Last Follow-Up |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | 23 months | 25 months | Unsteady gait, abnormal eye movements, opsoclonus, titubation, intention tremor and ataxia | 8/15 | No | Prednisolone IVIG | Good | 13 years |
| 2 | Female | 30 months | 34 months | Unsteady gait, vomiting, opsoclonus and regression in language | 12/15 | No | Dexamethasone | Good | 7 years 6 months |
| 3 | Female | 17 months | 17 months | Limb tremors, ataxia, loss of lower limb and truncal control and loss of speech | 11/15 | Yes | Surgical resection of neuroblastoma Dexamethasone Cyclophosphamide | Good | 7 years 8 months |
| Case | Age | Intellectual Functioning | Other Domains Tested |
|---|---|---|---|
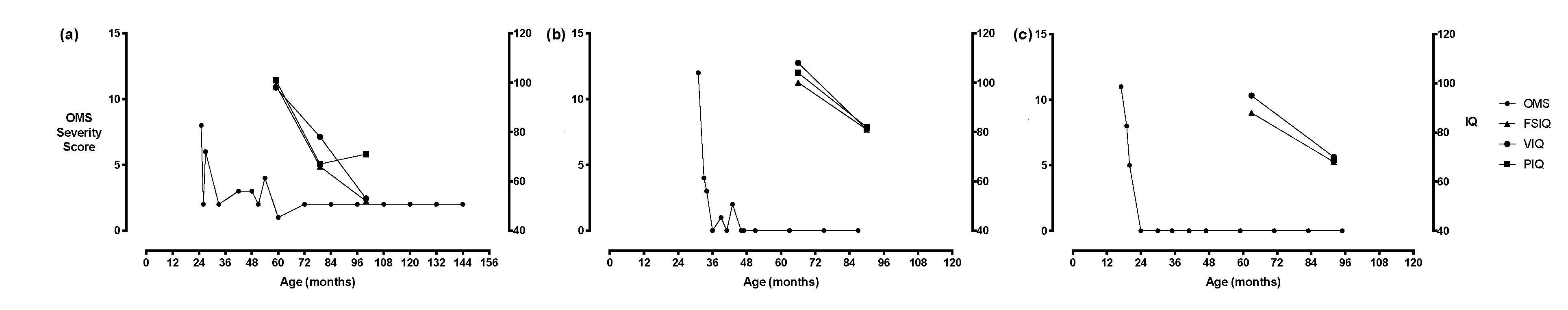
| 1 | 4 years 11 months | FSIQ: 99 VIQ: 98 PIQ: 101 | Attention (selective): – Visuospatial skills: ++ Language (receptive): – Language (expressive): – |
| 6 years 7 months | FSIQ: 66 VIQ: 78 PIQ: 67 | Processing speed: ++ Language (receptive): – Language (expressive): – | |
| 8 years 4 months | FSIQ: 5 VIQ: 53 PIQ: 71 | Attention (working memory): ++ Processing speed: ++ Visuospatial skills: ++ Language (receptive): ++ Language (expressive): ++ Academic (reading): ++ Academic (spelling): ++ | |
| 2 | 5 years 6 months | FSIQ: 100 VIQ: 108 PIQ: 104 | Attention (sustained): – Attention (working memory): – Processing speed: – Visuospatial skills: + Memory (new learning): – Memory (delayed recall): – |
| 7 years 6 months | FSIQ: 81 VIQ: 81 PIQ: 82 | Attention (sustained): ++ Attention (working memory): – Processing speed: – Visuospatial skills: + Language (receptive): – Memory (new learning): – Memory (delayed recall): – Academic (reading): – Academic (spelling): – | |
| 3 | 5 years 3 months | FSIQ: 81 VIQ: 95 | Not tested |
| 7 years 8 months | FSIQ: 68 VIQ: 70 PIQ: 69 | Attention (sustained): ++ Processing speed: ++ Language (receptive): ++ Language (expressive): – Memory (new learning): – Memory (delayed recall): – Academic (reading): – Academic (spelling): – |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goh, E.L.; Scarff, K.; Satariano, S.; Lim, M.; Anand, G. Evolving Cognitive Dysfunction in Children with Neurologically Stable Opsoclonus–Myoclonus Syndrome. Children 2020, 7, 103. https://doi.org/10.3390/children7090103
Goh EL, Scarff K, Satariano S, Lim M, Anand G. Evolving Cognitive Dysfunction in Children with Neurologically Stable Opsoclonus–Myoclonus Syndrome. Children. 2020; 7(9):103. https://doi.org/10.3390/children7090103
Chicago/Turabian StyleGoh, En Lin, Kate Scarff, Stephanie Satariano, Ming Lim, and Geetha Anand. 2020. "Evolving Cognitive Dysfunction in Children with Neurologically Stable Opsoclonus–Myoclonus Syndrome" Children 7, no. 9: 103. https://doi.org/10.3390/children7090103
APA StyleGoh, E. L., Scarff, K., Satariano, S., Lim, M., & Anand, G. (2020). Evolving Cognitive Dysfunction in Children with Neurologically Stable Opsoclonus–Myoclonus Syndrome. Children, 7(9), 103. https://doi.org/10.3390/children7090103






