Impact of Point-of-Care Decision Support Tool on Laboratory Screening for Comorbidities in Children with Obesity
Abstract
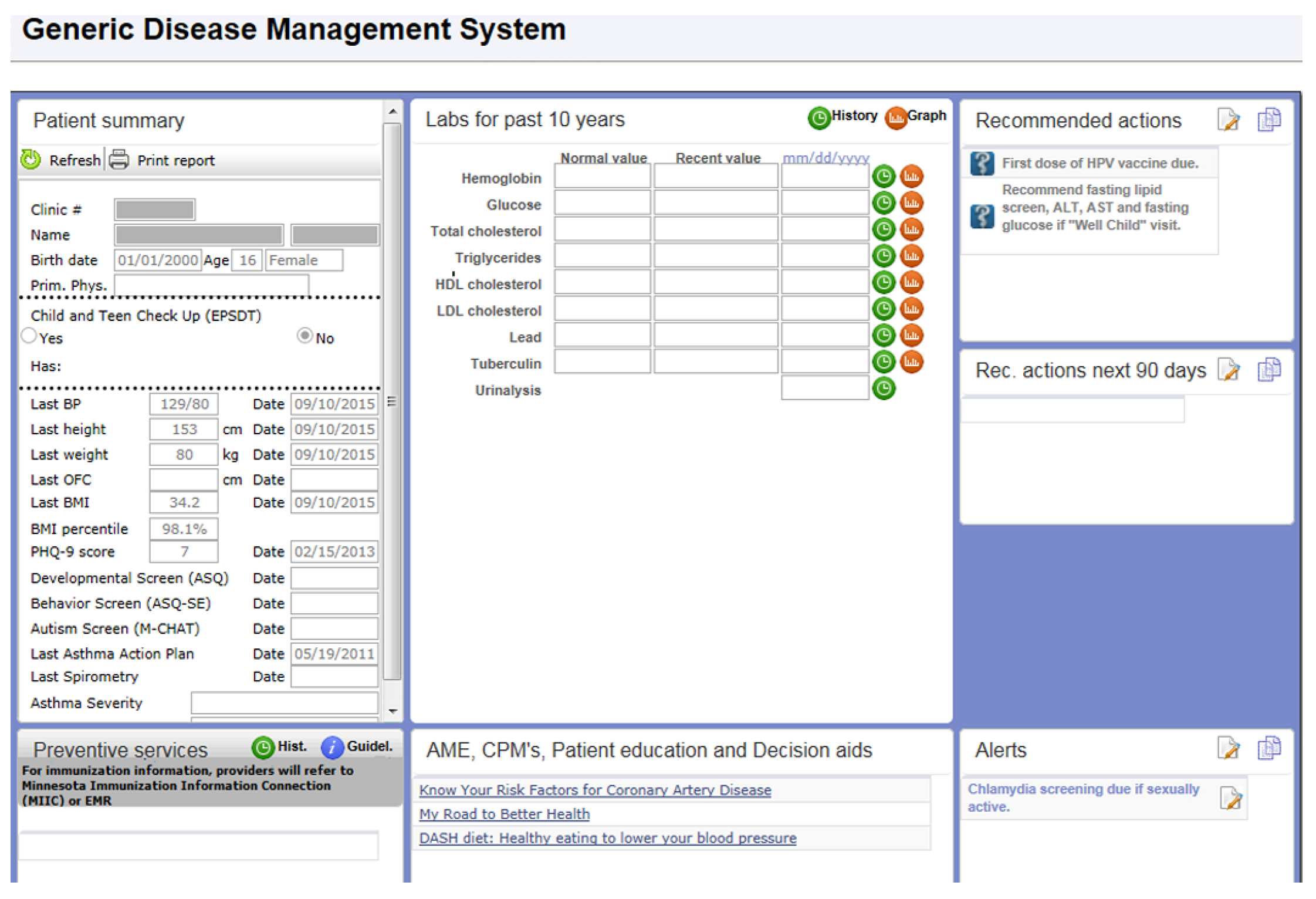
:1. Introduction
2. Methods
3. Statistical Methods
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Skinner, A.C.; Ravanbakht, S.N.; Skelton, J.A.; Perrin, E.M.; Armstrong, S.C. Prevalence of Obesity and Severe Obesity in US Children, 1999-2016. Pediatrics 2018, 141, e20173459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skinner, A.C.; Perrin, E.M.; Skelton, J.A. Cardiometabolic Risks and Obesity in the Young. N. Engl. J. Med. 2016, 374, 592–593. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Kelly, A.S. Review of Childhood Obesity: From Epidemiology, Etiology and Comorbidities to Clinical Assessment and Treatment. Mayo Clin. Proc. 2017, 92, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Mayer-Davis, E.J.; Lawrence, J.M.; Dabelea, D.; Divers, J.; Isom, S.; Dolan, L.; Imperatore, G.; Linder, B.; Marcovina, S.; Pettitt, D.J.; et al. Incidence Trends of Type 1 and Type 2 Diabetes among Youths, 2002-2012. N. Engl. J. Med. 2017, 376, 1419–1429. [Google Scholar] [CrossRef] [Green Version]
- Anderson, E.L.; Howe, L.D.; Jones, H.E.; Higgins, J.P.; Lawlor, D.A.; Fraser, A. The Prevalence of Non-Alcoholic Fatty Liver Disease in Children and Adolescents: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0140908. [Google Scholar] [CrossRef] [Green Version]
- Krebs, N.F.; Himes, J.H.; Jacobson, D.; Nicklas, T.A.; Guilday, P.; Styne, D. Assessment of Child and Adolescent Overweight and Obesity. Pediatrics 2007, 120, S193–S228. [Google Scholar] [CrossRef] [Green Version]
- American Diabetes Association 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2019. Diabetes Care 2018, 42, S13–S28. [Google Scholar] [CrossRef] [Green Version]
- Barlow, S.E. Expert Committee Expert Committee Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity: Summary Report. Pediatrics 2007, 120, S164–S192. [Google Scholar] [CrossRef] [Green Version]
- de Ferranti, S.D.; Steinberger, J.; Ameduri, R.; Baker, A.; Gooding, H.; Kelly, A.S.; Mietus-Snyder, M.; Mitsnefes, M.M.; Peterson, A.L.; St-Pierre, J.; et al. Cardiovascular Risk Reduction in High-Risk Pediatric Patients: A Scientific Statement from the American Heart Association. Circulation 2019, 139, e603–e634. [Google Scholar] [CrossRef]
- Vos, M.B.; Abrams, S.H.; Barlow, S.E.; Caprio, S.; Daniels, S.; Kohli, R.; Mouzaki, M.; Sathya, P.; Schwimmer, J.B.; Sundaram, S.S.; et al. NASPGHAN Clinical Practice Guideline for the Diagnosis and Treatment of Nonalcoholic Fatty Liver Disease in Children. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 319–334. [Google Scholar] [CrossRef] [Green Version]
- American Diabetes Association 13. Children and Adolescents: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020, 43, S163–S182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benson, L.J.; Baer, H.J.; Kaelber, D.C. Screening for obesity-related complications among obese children and adolescents: 1999–2008. Obesity 2011, 19, 1077–1082. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, M.; Rifas-Shiman, S.L.; Marshall, R.; Simon, S.R.; Gillman, M.W.; Finkelstein, J.A.; Taveras, E.M. Evaluating the Implementation of Expert Committee Recommendations for Obesity Assessment. Clin. Pediatr. 2013, 52, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Dilley, K.; Martin, L.A.; Sullivan, C.; Seshadri, R.; Binns, H.J. Pediatric Practice Research Group. Identification of Overweight Status Is Associated with Higher Rates of Screening for Comorbidities of Overweight in Pediatric Primary Care Practice. Pediatrics 2007, 119, e148–e155. [Google Scholar] [CrossRef] [PubMed]
- Nader, N.; Singhal, V.; Weaver, A.; Kumar, S.; Javed, A. Temporal Trends in the Diagnosis and Management of Childhood Obesity/Overweight in Primary Care. J. Prim. Care Community Health 2013, 5, 44–49. [Google Scholar] [CrossRef]
- Halterman, J.S.; Fisher, S.; Conn, K.M.; Fagnano, M.; Lynch, K.; Marky, A.; Szilagyi, P.G. Improved Preventive Care for Asthma. Arch. Pediatr. Adolesc. Med. 2006, 160, 1018. [Google Scholar] [CrossRef] [Green Version]
- Fiks, A.G.; Grundmeier, R.W.; Biggs, L.M.; Localio, A.R.; Alessandrini, E.A. Impact of Clinical Alerts Within an Electronic Health Record on Routine Childhood Immunization in an Urban Pediatric Population. Pediatrics 2007, 120, 707–714. [Google Scholar] [CrossRef]
- Davis, R.L.; Wright, J.; Chalmers, F.; Levenson, L.; Brown, J.C.; Lozano, P.; Christakis, A.D. A Cluster Randomized Clinical Trial to Improve Prescribing Patterns in Ambulatory Pediatrics. PLoS Clin. Trials 2007, 2, e25. [Google Scholar] [CrossRef] [Green Version]
- Rattay, K.T.; Ramakrishnan, M.; Atkinson, A.; Gilson, M.; Drayton, V. Use of an Electronic Medical Record System to Support Primary Care Recommendations to Prevent, Identify, and Manage Childhood Obesity. Pediatrics 2008, 123, S100–S107. [Google Scholar] [CrossRef] [Green Version]
- Coleman, K.J.; Hsii, A.C.; Koebnick, C.; Alpern, A.F.; Bley, B.; Yousef, M.; Shih, E.M.; Trimble-Cox, K.J.; Smith, N.; Porter, A.; et al. Implementation of Clinical Practice Guidelines for Pediatric Weight Management. J. Pediatr. 2012, 160, 918–922.e1. [Google Scholar] [CrossRef] [Green Version]
- Ayash, C.R.; Simon, S.R.; Marshall, R.; Kasper, J.; Chomitz, V.; Hacker, K.; Kleinman, K.; Taveras, E.M. Evaluating the impact of point- of-care decision support tools in improving diagnosis of obese children in primary care. Obesity 2013, 21, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, U.; Berrong, J.; Nettiksimmons, J.; Byrd, R.S. Impact of Electronic Health Record Clinical Decision Support on the Management of Pediatric Obesity. Am. J. Med Qual. 2014, 30, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Gentile, N.; Cristiani, V.; Lynch, B.A.; Wilson, P.M.; Weaver, A.L.; Rutten, L.J.; Jacobson, D.J.; Chaudhry, R.; Sriram, S.; Kumar, S. The effect of an automated point of care tool on diagnosis and management of childhood obesity in primary care. J. Eval. Clin. Pract. 2016, 22, 962–968. [Google Scholar] [CrossRef] [PubMed]
- Shojania, K.G.; Jennings, A.; Mayhew, A.; Ramsay, C.R.; Eccles, M.P.; Grimshaw, J. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database Syst. Rev. 2009, CD001096. [Google Scholar] [CrossRef]
- Force, U.P.S.T.; Bibbins-Domingo, K.; Grossman, D.C.; Curry, S.J.; Davidson, K.W.; Epling, J.W.; García, F.A.R.; Gillman, M.W.; Kemper, A.R.; Krist, A.H.; et al. Screening for Lipid Disorders in Children and Adolescents. J. Am. Med. Assoc. 2016, 316, 625–633. [Google Scholar] [CrossRef] [Green Version]
- Dryden, E.M.; Hardin, J.; McDonald, J.; Taveras, E.M.; Hacker, K. Provider Perspectives on Electronic Decision Supports for Obesity Prevention. Clin. Pediatr. 2012, 51, 490–497. [Google Scholar] [CrossRef]
- Barlow, S.E.; Dietz, W.H. Management of child and adolescent obesity: Summary and recommendations based on reports from pediatricians, pediatric nurse practitioners, and registered dietitians. Pediatrics 2002, 110, 236–238. [Google Scholar]
- Galuska, D.A.; Will, J.C.; Serdula, M.K.; Ford, E.S. Are Health Care Professionals Advising Obese Patients to Lose Weight? JAMA 1999, 282, 1576. [Google Scholar] [CrossRef] [Green Version]
- Kolagotla, L.; Adams, W. Ambulatory Management of Childhood Obesity. Obes. Res. 2004, 12, 275–283. [Google Scholar] [CrossRef] [Green Version]
- Solberg, L.I.; Brekke, M.L.; Kottke, T.E. Are Physicians Less Likely to Recommend Preventive Services to Low-SES Patients? Prev. Med. 1997, 26, 350–357. [Google Scholar] [CrossRef]
- Story, M.T.; Neumark-Stzainer, D.R.; Sherwood, N.E.; Holt, K.; Sofka, D.; Trowbridge, F.; Barlow, S.E. Management of child and adolescent obesity: Attitudes, barriers, skills, and training needs among health care professionals. Pediatrics 2002, 110, 210–214. [Google Scholar] [PubMed]
- Perrin, E.M.; Flower, K.B.; Garrett, J.; Ammerman, A.S. Preventing and Treating Obesity: Pediatricians’ Self-Efficacy, Barriers, Resources, and Advocacy. Ambul. Pediatr. 2005, 5, 150–156. [Google Scholar] [CrossRef] [PubMed]
| Total (N = 1087) | 2009 (N = 342) | 2011 (N = 366) | 2013 (N = 379) | |
|---|---|---|---|---|
| Gender | ||||
| Male | 660 (60.7%) | 202 (59.1%) | 231 (63.1%) | 227 (59.9%) |
| Female | 427 (39.3%) | 140 (40.9%) | 135 (36.9%) | 152 (40.1%) |
| Race | ||||
| Black | 77 (7.1%) | 18 (5.3%) | 23 (6.3%) | 36 (9.5%) |
| White | 850 (78.2%) | 271 (79.2%) | 288 (78.7%) | 291 (76.8%) |
| Unknown | 160 (14.7%) | 53 (15.5%) | 55 (15.0%) | 52 (13.7%) |
| Specialty | ||||
| Family Medicine | 559 (51.4%) | 171 (50.0%) | 198 (54.1%) | 190 (50.1%) |
| Pediatrics | 528 (48.6%) | 171 (50.0%) | 168 (45.9%) | 189 (49.9%) |
| Age group | ||||
| 7–10 years | 89 (8.2%) | 28 (8.2%) | 29 (7.9%) | 32 (8.4%) |
| 11–14 years | 658 (60.5%) | 202 (59.1%) | 218 (59.6%) | 238 (62.8%) |
| 15–18 years | 340 (31.3%) | 112 (32.8%) | 119 (32.5%) | 109 (28.8%) |
| Insurance | ||||
| Commercial | 877 (80.7%) | 285 (83.3%) | 293 (80.1%) | 299 (78.9%) |
| Medicaid | 176 (16.2%) | 49 (14.3%) | 60 (16.4%) | 67 (17.7%) |
| Other | 34 (3.1%) | 8 (2.3%) | 13 (3.6%) | 13 (3.4%) |
| Provider Type *† | ||||
| Nurse Practitioner | 251 (23.2%) | 54 (15.8%) | 112 (30.8%) | 85 (22.6%) |
| Resident | 224 (20.7%) | 74 (21.7%) | 73 (20.1%) | 77 (20.5%) |
| Staff | 606 (56.1%) | 213 (62.5%) | 179 (49.2%) | 214 (56.9%) |
| Obesity Status | ||||
| Non Severe | 926 (85.2%) | 297 (86.8%) | 316 (86.3%) | 313 (82.6%) |
| Severe | 161 (14.8%) | 45 (13.2%) | 50 (13.7%) | 66 (17.4%) |
| Univariate Analysis | Multiple Regression Analysis | |||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p-Value * | Odds Ratio (95% CI) | p-Value * | |
| Year | ||||
| 2009 | ref | ref | ||
| 2011 | 1.09 (0.73, 1.64) | 0.675 | 1.17 (0.75, 1.83) | 0.487 |
| 2013 | 0.82 (0.53, 1.26) | 0.362 | 0.83 (0.52, 1.33) | 0.438 |
| Gender | ||||
| Male | ref | ref | ||
| Female | 1.91 (1.35, 2.70) | 0.0002 | 1.95 (1.33, 2.87) | 0.001 |
| Race | ||||
| White | ref | ref | ||
| Black | 1.05 (0.54, 2.04) | 0.890 | 0.58 (0.25, 1.32) | 0.192 |
| Unknown | 1.17 (0.73, 1.87) | 0.518 | 1.11 (0.66, 1.87) | 0.700 |
| Specialty | ||||
| Family Medicine | ref | ref | ||
| Pediatrics | 4.14 (2.79, 6.14) | <0.001 | 5.14 (3.34, 7.92) | <0.001 |
| Age Group | ||||
| 7–10 | 0.32 (0.12, 0.90) | 0.031 | 0.21 (0.07, 0.63) | 0.005 |
| 11–14 | ref | ref | ||
| 15–18 | 1.61 (1.14, 2.30) | 0.008 | 1.93 (1.32, 2.84) | 0.001 |
| Insurance | ||||
| Commercial | ref | ref | ||
| Medicaid | 1.33 (0.87, 2.05) | 0.192 | 1.16 (0.68, 1.99) | 0.588 |
| Other | 0.17 (0.02, 1.23) | 0.080 | 0.18 (0.03, 1.29) | 0.088 |
| Provider Type | ||||
| Staff | ref | ref | ||
| NP | 1.46 (0.97, 2.19) | 0.071 | 1.32 (0.83, 2.10) | 0.234 |
| Resident | 1.32 (0.85, 2.03) | 0.213 | 1.11 (0.69, 1.78) | 0.671 |
| Obesity Status | ||||
| Moderate | ref | ref | ||
| Severe | 2.18 (1.45, 3.29) | 0.0002 | 2.54 (1.61, 4.01) | <0.001 |
| Total (N = 1087) | 2009 (N =342) | 2011 (N = 366) | 2013 (N = 379) | p-Value * | |
|---|---|---|---|---|---|
| Glucose | |||||
| Yes | 135 (12.4%) | 43 (12.6%) | 53 (14.5%) | 39 (10.3%) | 0.338 |
| No | 952 (87.6%) | 299 (87.4%) | 313 (85.5%) | 340 (89.7%) | |
| A1C | |||||
| Yes | 17 (1.6%) | 6 (1.8%) | 4 (1.1%) | 7 (1.9%) | 1.00 |
| No | 1070 (98.4%) | 336 (98.3%) | 362 (98.9%) | 372 (98.2%) | |
| ALT | |||||
| Yes | 110 (10.1%) | 35 (10.2%) | 51 (13.9%) | 24 (6.3%) | 0.073 |
| No | 977 (89.9%) | 307 (89.8%) | 315 (86.1%) | 355 (93.7%) | |
| Triglycerides | |||||
| Yes | 131 (12.1%) | 44 (12.9%) | 49 (13.4%) | 38 (10.0%) | 0.253 |
| No | 956 (88.0%) | 298 (87.1%) | 317 (86.6%) | 341 (90.1%) | |
| HDL | |||||
| Yes | 129 (11.9%) | 44 (12.9%) | 48 (13.1%) | 37 (9.8%) | 0.205 |
| No | 958 (88.1%) | 298 (87.1%) | 318 (86.9%) | 342 (90.2%) | |
| LDL | |||||
| Yes | 129 (11.9%) | 44 (12.9%) | 48 (13.1%) | 37 (9.8%) | 0.205 |
| No | 958 (88.1%) | 298 (87.1%) | 318 (86.9%) | 342 (90.2%) | |
| Any Testing Performed | |||||
| Yes | 153 (14.1%) | 50 (14.6%) | 57 (15.6%) | 46 (12.1%) | 0.335 |
| No | 934 (85.9%) | 292 (85.4%) | 309 (84.4%) | 333 (87.9%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaufman, T.K.; Gentile, N.; Kumar, S.; Halle, M.; Lynch, B.A.; Cristiani, V.; Fischer, K.; Chaudhry, R. Impact of Point-of-Care Decision Support Tool on Laboratory Screening for Comorbidities in Children with Obesity. Children 2020, 7, 67. https://doi.org/10.3390/children7070067
Kaufman TK, Gentile N, Kumar S, Halle M, Lynch BA, Cristiani V, Fischer K, Chaudhry R. Impact of Point-of-Care Decision Support Tool on Laboratory Screening for Comorbidities in Children with Obesity. Children. 2020; 7(7):67. https://doi.org/10.3390/children7070067
Chicago/Turabian StyleKaufman, Tara K., Natalie Gentile, Seema Kumar, Marian Halle, Brian A. Lynch, Valeria Cristiani, Karen Fischer, and Rajeev Chaudhry. 2020. "Impact of Point-of-Care Decision Support Tool on Laboratory Screening for Comorbidities in Children with Obesity" Children 7, no. 7: 67. https://doi.org/10.3390/children7070067
APA StyleKaufman, T. K., Gentile, N., Kumar, S., Halle, M., Lynch, B. A., Cristiani, V., Fischer, K., & Chaudhry, R. (2020). Impact of Point-of-Care Decision Support Tool on Laboratory Screening for Comorbidities in Children with Obesity. Children, 7(7), 67. https://doi.org/10.3390/children7070067






