Evaluating a Standardized Transition of Care Process for Pediatric Inflammatory Bowel Disease Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Clinic Development and Description
2.2. Transition Readiness Assessment
2.3. Depression Screen
2.4. Disease Activity
2.5. Data Source
2.6. Statistical Analysis
3. Results
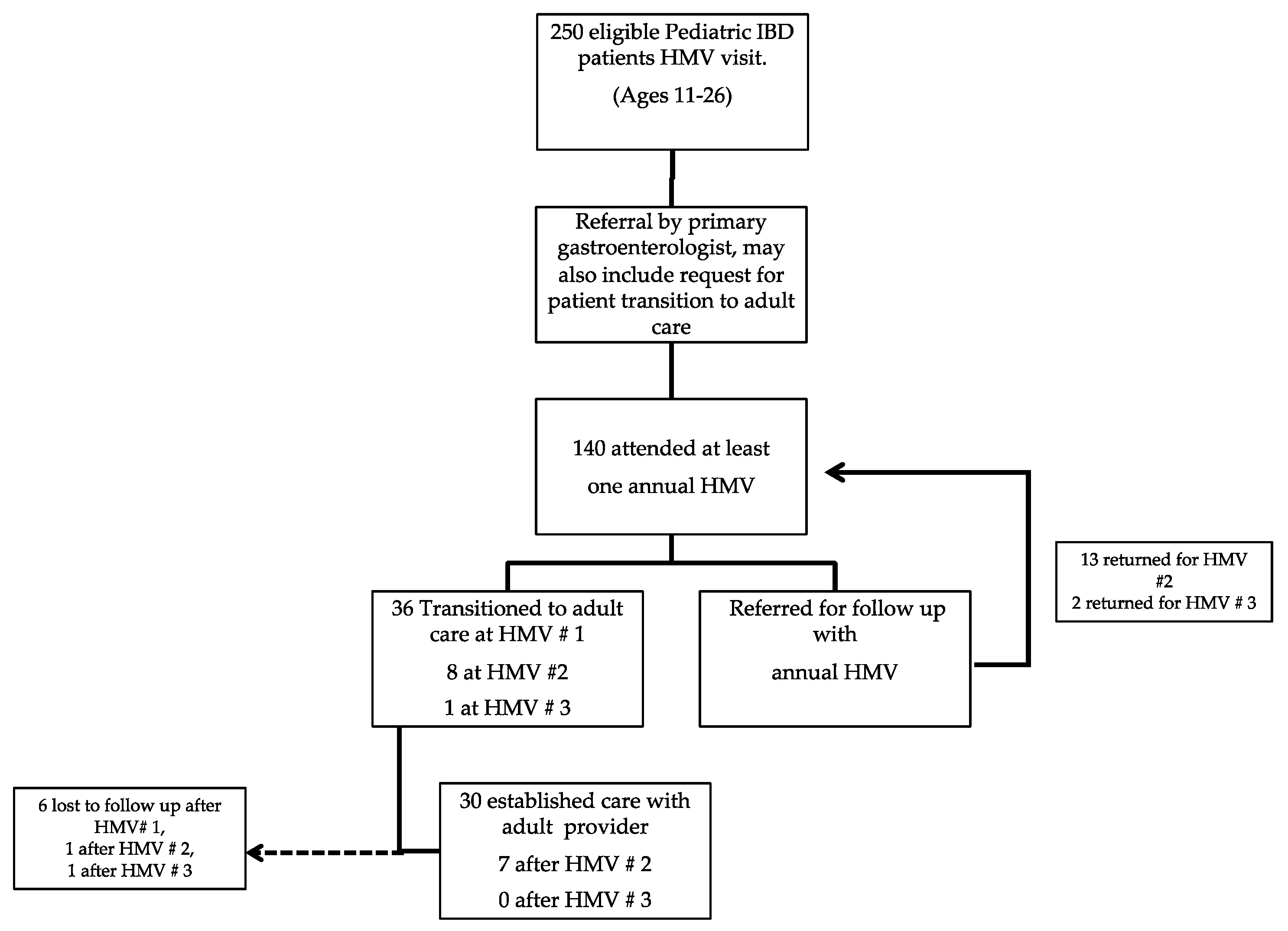
3.1. Patient Characteristics
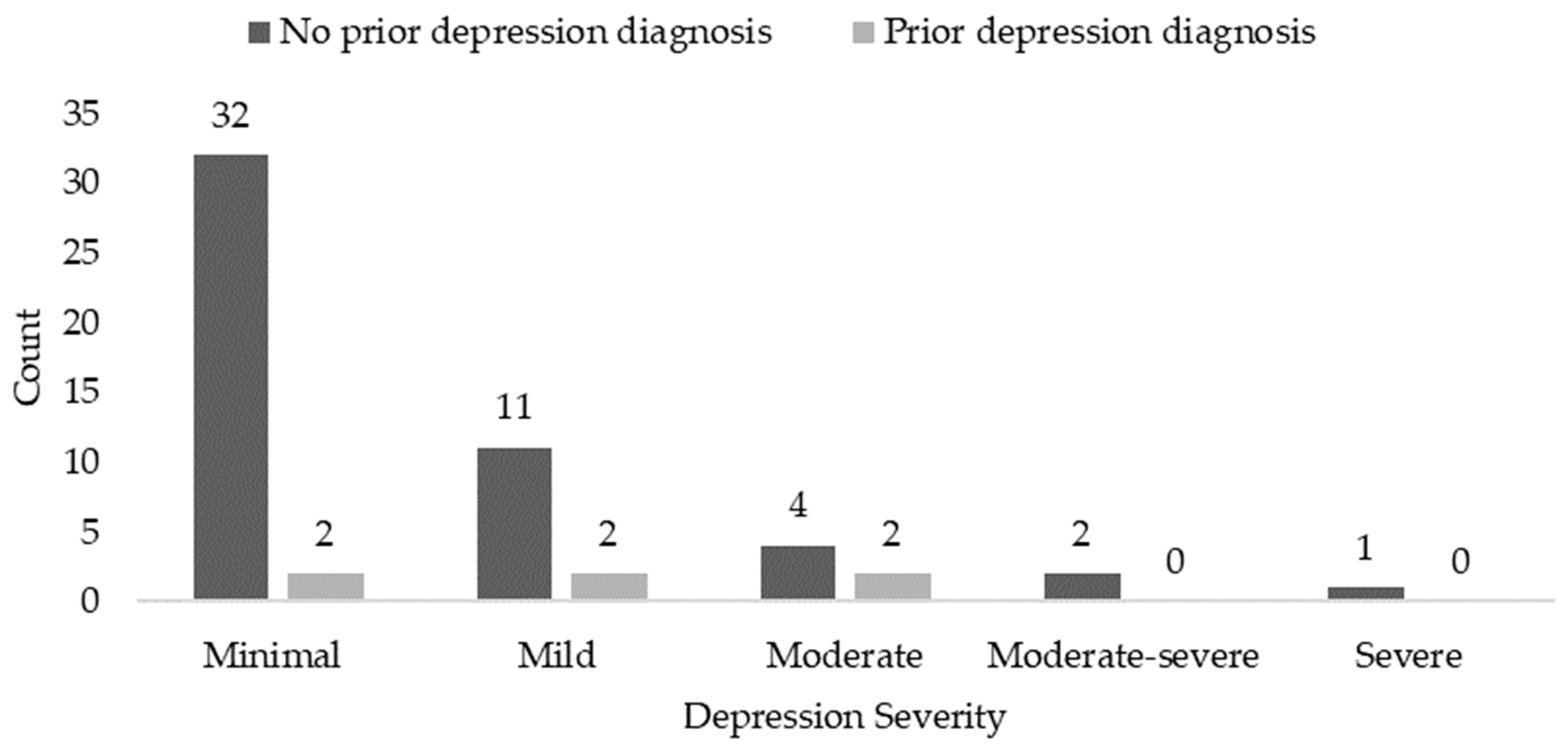
3.2. PHQ-9 Depression Screen
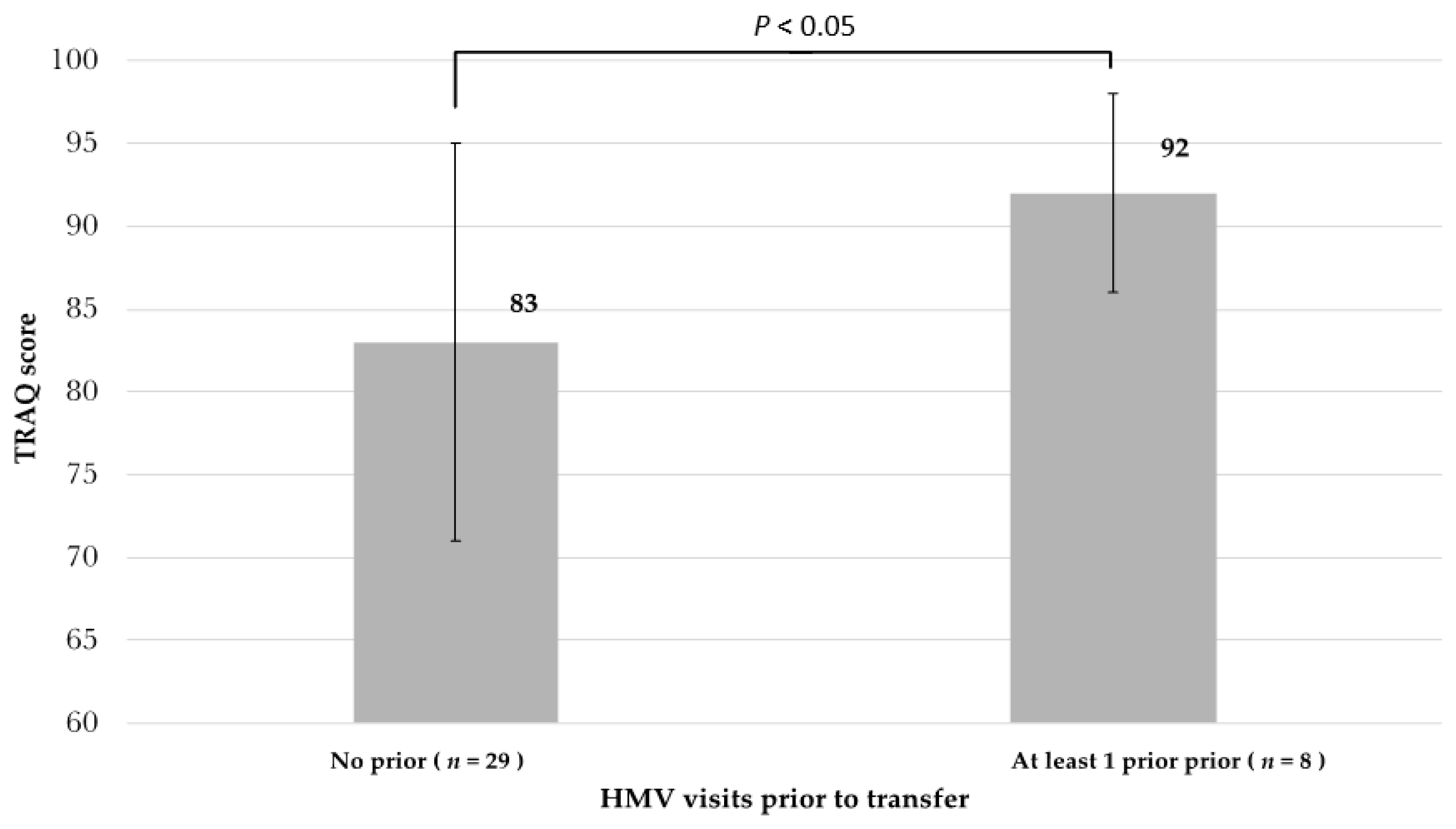
3.3. Transition Readiness Assessment
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Sýkora, J.; Pomahačová, R.; Kreslová, M.; Cvalínová, D.; Štych, P.; Schwarz, J. Current global trends in the incidence of pediatric-onset inflammatory bowel disease. World J. Gastroenterol. 2018, 24, 2741–2763. [Google Scholar] [CrossRef] [PubMed]
- M’Koma, A.E. Inflammatory Bowel Disease: An Expanding Global Health Problem. Clin. Med. Insights Gastroenterol. 2013, 6, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Rosen, M.J.; Dhawan, A.; Saeed, S.A. Inflammatory Bowel Disease in Children and Adolescents. JAMA Pediatr. 2015, 169, 1053–1060. [Google Scholar] [CrossRef] [PubMed]
- Szigethy, E.; Youk, A.O.; Benhayon, D.; Fairclough, D.L.; Newara, M.C.; Kirshner, M.A.; Bujoreanu, S.I.; Mrakotsky, C.; Bousvaros, A.; Srinath, A.I.; et al. Depression Subtypes in Pediatric Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 574–581. [Google Scholar] [CrossRef] [PubMed]
- Szigethy, E.; Levy-Warren, A.; Whitton, S.; Bousvaros, A.; Gauvreau, K.; Leichtner, A.M.; Beardslee, W.R. Depressive Symptoms and Inflammatory Bowel Disease in Children and Adolescents: A Cross-Sectional Study. J. Pediatr. Gastroenterol. Nutr. 2004, 39, 395–403. [Google Scholar] [CrossRef]
- Walter, J.G.; Kahn, S.A.; Noe, J.D.; Schurman, J.V.; Miller, S.A.; Greenley, R.N. Feeling Fine. Inflamm. Bowel Dis. 2016, 22, 402–408. [Google Scholar] [CrossRef]
- Hommel, K.A.; Odell, S.; Sander, E.; Baldassano, R.N.; Barg, F.K. Treatment adherence in paediatric inflammatory bowel disease: Perceptions from adolescent patients and their families. Heal. Soc. Care Community 2010, 19, 80–88. [Google Scholar] [CrossRef]
- Blum, R.W.; Garell, D.; Hodgman, C.H.; Jorissen, T.W.; Okinow, N.A.; Orr, D.P.; Slap, G.B. Transition from child-entered to adult health-care systems for adolescents with chornic conditions. A position paper of the Society for Adolescent Medicine. J. Adolesc. Health 1993, 14, 570–576. [Google Scholar] [CrossRef]
- Menon, T.; Afzali, A. Inflammatory Bowel Disease: A Practical Path to Transitioning from Pediatric to Adult Care. Am. J. Gastroenterol. 2019, 114, 1432–1440. [Google Scholar] [CrossRef]
- Trivedi, I.; Keefer, L. The Emerging Adult with Inflammatory Bowel Disease: Challenges and Recommendations for the Adult Gastroenterologist. Gastroenterol. Res. Pr. 2015, 2015, 1–11. [Google Scholar] [CrossRef]
- Sebastian, S.; Jenkins, H.; McCartney, S.; Ahmad, T.; Arnott, I.; Croft, N.; Russell, R.; Lindsay, J.O. The requirements and barriers to successful transition of adolescents with inflammatory bowel disease: Differing perceptions from a survey of adult and paediatric gastroenterologists. J. Crohns Coliti 2012, 6, 830–844. [Google Scholar] [CrossRef] [PubMed]
- Gray, W.N.; Denson, L.A.; Baldassano, R.N.; Hommel, K.A. Treatment Adherence in Adolescents with Inflammatory Bowel Disease: The Collective Impact of Barriers to Adherence and Anxiety/Depressive Symptoms. J. Pediatr. Psychol. 2012, 37, 282–291. [Google Scholar] [CrossRef] [PubMed]
- De Silva, P.S.A.; Fishman, L.N. Transition of the Patient with IBD from Pediatric toAdult Care—An Assessment of Current Evidence. Inflamm. Bowel Dis. 2014, 20, 1458–1464. [Google Scholar] [CrossRef]
- Wood, D.L.; Sawicki, G.; Miller, M.D.; Smotherman, C.; Lukens-Bull, K.; Livingood, W.C.; Ferris, M.; Kraemer, D.F. The Transition Readiness Assessment Questionnaire (TRAQ): Its Factor Structure, Reliability, and Validity. Acad. Pediatr. 2014, 14, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Kappelman, M.D.; Crandall, W.V.; Colletti, R.B.; Goudie, A.; Leibowitz, I.H.; Duffy, L.; Milov, D.E.; Kim, S.C.; Schoen, B.T.; Patel, A.S.; et al. Short pediatric Crohnʼs disease activity index for quality improvement and observational research. Inflamm. Bowel Dis. 2011, 17, 112–117. [Google Scholar] [CrossRef]
- Turner, D.; Otley, A.R.; Mack, D.; Hyams, J.; De Bruijne, J.; Uusoue, K.; Walters, T.D.; Zachos, M.; Mamula, P.; Beaton, D.E.; et al. Development, Validation, and Evaluation of a Pediatric Ulcerative Colitis Activity Index: A Prospective Multicenter Study. Gastroenterology 2007, 133, 423–432. [Google Scholar] [CrossRef]
- Hyams, J.S.; Ferry, G.D.; Mandel, F.S.; Gryboski, J.D.; Kibort, P.M.; Kirschner, B.S.; Griffiths, A.M.; Katz, A.J.; Grand, R.J.; Boyle, J.T.; et al. Development and validation of a pediatric Crohn’s disease activity index. J. Pediatr. Gastroenterol. Nutr. 1991, 12, 439–447. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Keefer, L.; Kane, S.V. Considering the Bidirectional Pathways between Depression and IBD: Recommendations for Comprehensive IBD Care. Gastroenterol. Hepatol. 2017, 13, 164–169. [Google Scholar]
- Gray, W.N.; Holbrook, E.; Morgan, P.J.; Saeed, S.A.; Denson, L.A.; Hommel, K.A. Transition Readiness Skill Acquistition in Adolscets and Adults with Inflammatory Bowel Disease: Findings from Integrating Assessment into Clinical Practice. Inflamm. Bowel Dis. 2015, 21, 1125–1131. [Google Scholar] [CrossRef] [PubMed]
- Graff, L.A.; Walker, J.R.; Bernstein, C.N. Depression and anxiety in inflammatory bowel disease: A review of comorbidity and management. Inflamm. Bowel Dis. 2009, 15, 1105–1118. [Google Scholar] [CrossRef] [PubMed]
- Neuendorf, R.; Harding, A.; Stello, N.; Hanes, D.; Wahbeh, H. Depression and anxiety in patients with Inflammatory Bowel Disease: A systematic review. J. Psychosom. Res. 2016, 87, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Sabbagh, S.; Ronis, T.; White, P.H. Pediatric rheumatology: Addressing the transition to adult-orientated health care. Open Access Rheumatol. Res. Rev. 2018, 10, 83–95. [Google Scholar] [CrossRef] [PubMed]
- Beal, S.J.; Nye, A.; Marraccini, A.; Biro, F.M. Evaluation of readiness to transfer to adult healthcare: What about the well adolescent? Health 2014, 2, 225–231. [Google Scholar] [CrossRef] [PubMed]
| Demographics | n = 140 |
|---|---|
| Age (years) at Initial HMV | 18 ± 2 |
| Age (years) at Diagnosis | 13 ± 2 |
| White [n (%)] | 112 (80) |
| Male [n (%)] | 83 (59) |
| Primary Diagnosis | |
| Crohn’s Disease | 103 (75) |
| Ulcerative Colitis | 29 (21) |
| Unclassified | 6 (4.3) |
| Secondary Diagnosis | |
| At Least One Secondary Diagnosis * | 56 (40) |
| Anxiety/Depression | 30 (21) |
| GERD | 15 (11) |
| Other | 44 (31) |
| None | 83 (60) |
| Recommended Follow Up Course | |
| Transitioned to Adult | 36 (26) |
| Return annual HMV | 114 (74) |
| both diagnoses) | |
| HMV = Health Maintenance Visit | |
| GERD = gastroenterology reflux disease | |
| Data are number (percent) of patients or mean ± SD | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shearer, J.L.; Perry, S.; Lidyard, N.; Apperson-Hensen, C.; DeLozier, S.; Burkhart, K.; Katz, J.; Moses, J. Evaluating a Standardized Transition of Care Process for Pediatric Inflammatory Bowel Disease Patients. Children 2020, 7, 271. https://doi.org/10.3390/children7120271
Shearer JL, Perry S, Lidyard N, Apperson-Hensen C, DeLozier S, Burkhart K, Katz J, Moses J. Evaluating a Standardized Transition of Care Process for Pediatric Inflammatory Bowel Disease Patients. Children. 2020; 7(12):271. https://doi.org/10.3390/children7120271
Chicago/Turabian StyleShearer, Jennifer Lynne, Sharon Perry, Nicole Lidyard, Carolyn Apperson-Hensen, Sarah DeLozier, Kimberly Burkhart, Jeffry Katz, and Jonathan Moses. 2020. "Evaluating a Standardized Transition of Care Process for Pediatric Inflammatory Bowel Disease Patients" Children 7, no. 12: 271. https://doi.org/10.3390/children7120271
APA StyleShearer, J. L., Perry, S., Lidyard, N., Apperson-Hensen, C., DeLozier, S., Burkhart, K., Katz, J., & Moses, J. (2020). Evaluating a Standardized Transition of Care Process for Pediatric Inflammatory Bowel Disease Patients. Children, 7(12), 271. https://doi.org/10.3390/children7120271







